Abstract
Over the past two decades, video-assisted thoracoscopic surgery (VATS) has evolved from a diagnostic procedure to a treatment for complex lung cancer cases. VATS is now accepted as a feasible, safe, and effective surgical technique for the treatment of lung cancer [1]. In fact, in current practice guidelines, thoracoscopic surgery is the suggested approach for the treatment of early-stage lung cancer [2, 3]. Decreased blood loss, reduced pain, shorter length of hospital stay, and fewer overall complications are just a few of the many potential benefits of this minimally invasive approach [4]. High-volume centers have not only evolved VATS techniques by performing more complex surgeries using VATS, but have also developed a new approach decreasing the number of incisions to one—the uniportal technique [5–7].
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Uniportal
- Single port
- Lobectomy
- Thoracoscopy
- Lung cancer
- Video-assisted thoracoscopic surgery
- Minimally invasive surgical procedures
Introduction
Over the past two decades, video-assisted thoracoscopic surgery (VATS) has evolved from a diagnostic procedure to a treatment for complex lung cancer cases. VATS is now accepted as a feasible, safe, and effective surgical technique for the treatment of lung cancer [1]. In fact, in current practice guidelines, thoracoscopic surgery is the suggested approach for the treatment of early-stage lung cancer [2, 3]. Decreased blood loss, reduced pain, shorter length of hospital stay, and fewer overall complications are just a few of the many potential benefits of this minimally invasive approach [4]. High-volume centers have not only evolved VATS techniques by performing more complex surgeries using VATS, but have also developed a new approach decreasing the number of incisions to one—the uniportal technique [5,6,7].
VATS Evolution: From Multiportal to Uniportal
In the early 1990s, video-assisted thoracic procedures were mainly performed through three or more ports. McKenna and colleagues published a series of 1100 VATS lobectomy cases using 3–4 ports with excellent technical results [8]. This paper was considered a landmark for the inclusion of VATS in the thoracic surgery arena. Pushing the boundaries, surgeons from major centers then developed VATS techniques with fewer incisions (fewer ports). D’Amico and colleagues demonstrated the feasibility and safety of VATS using two incisions (one 10-mm port and a working incision of approximately 4 cm) in a series of 500 patients who underwent lobectomy for lung cancer [9]. In 2004, Rocco and colleagues introduced the single-port (uniportal) approach for simple procedures, such as wedge pulmonary resections for the diagnosis of interstitial lung diseases and for the treatment of spontaneous pneumothorax [10]. In 2011, Gonzalez-Rivas and colleagues reported the first lobectomy performed using a uniportal VATS technique [11].
Over the last 5 years, the single-port approach has rapidly gained popularity across Europe and Asia [12]. Li, Akter, and their colleagues demonstrated shorter hospital stays and reduced chest tube drainage with the uniportal technique [13, 14]. However, contradictory results were recently presented in a report from Perna and colleagues, which failed to demonstrate any superiority of the uniportal approach versus a multiple-port approach with regards to postoperative pain, duration of chest tube drainage, length of hospital stay, or the incidence of postoperative complications [15]. Although the methodology of Perna’s study has been questioned, it is notable as the first randomized trial to analyze postoperative outcomes according to the number of VATS incisions [16].
Minimally invasive thoracic surgery demands extremely precise movements, a profound knowledge of anatomy, and comfort with specialized equipment to avoid technical complications, especially vascular accidents. Some surgeons believe that it is safer and easier to perform lung surgery through multiple ports; however, there is no data that validates this impression. Because vision is the predominant sense used during a VATS procedure, we believe that the uniportal technique offers a safer approach because the straight, frontal view of the pulmonary hilum elements facilitates a secure dissection. For this reason, the uniportal approach has been our standard VATS approach since January 2014 [7].
The learning curve for proficiency with any VATS procedure can vary according to the complexity of the case, the technical skills of the surgeon, and the surgical volume of both the surgeon and the surgeon’s institution. Ideally, the surgeon should be able to perform all types of lobectomy and be able to manage an incomplete fissure and pulmonary adhesions. The surgeon’s operating time should reach a steady and reasonable duration (for example, less than 3 h). The rate of conversion to thoracotomy should match that seen in the majority of studies in the literature, and intraoperative complications should be comparable with complications that occur using the surgeon’s thoracotomy technique. Using VATS lobectomy, even standard cases are technically demanding and have the potential risk of uncontrollable pulmonary hemorrhage. High-volume centers have demonstrated very low rates of complications and conversion to thoracotomy [8, 9]. In our series of 250 uniportal VATS procedures, which included early-stage lung cancer and complex lung resection cases, we converted to thoracotomy in 6.1% of cases [7]. However, when only early-stage lung cancer cases were analyzed, the conversion rate was 2.2% [7].
Indications for Uniportal Lobectomy
Indications for the uniportal lobectomy are the same as those for multiportal VATS. Indications include early-stage (stages I and II) non-small cell lung cancer (NSCLC), infectious disease that results in the destruction or loss of function of a lobe, and pulmonary sequestration.
Contraindications for Uniportal Lobectomy
The contraindications for uniportal lobectomy are mostly relative. With the development of different types of articulated staplers and the experience gained with time, most complex lung resections have been described using uniportal techniques including bronchoplasty, pneumonectomy and arterioplasty [7, 17,18,19]. The safety of the patient and the comfort of the surgeon must always be the leading factors in determining the surgical approach.
In general, as for any VATS technique, the most common relative contraindication is locally advanced lung cancer. Central tumors invading the pulmonary hilum, tumors invading the chest wall, and tumors invading adjacent structures (such as the vena cava, atrium and aorta) are some examples. Complex pleural adhesions, calcified lymph nodes, and anatomic malformations may also demand the use of more ports or a prophylactic conversion to thoracotomy [20].
Preoperative Planning
Patients should be evaluated regarding their operability and the resectability of their disease. The patient’s clinical status determines their operability. Functional evaluation is performed with spirometry to measure preoperative FEV1 (forced expiratory volume in 1 s) and DLCO (diffusion capacity of the lung for carbon monoxide). Patients with borderline lung function should undergo a cardiopulmonary exercise test to measure peak VO2 (ventilatory oxygen uptake) and assess possible postoperative complications [2]. Other cardiac exams may be requested depending on the clinical scenario and type of lung resection.
In patients with NSCLC, a complete lung cancer staging is performed with chest computed tomography (CT) scan, positron emission tomography (PET) scan, endobronchial ultrasound (EBUS) or mediastinoscopy, and magnetic resonance imaging (MRI) of the brain [2]. A CT scan with intravenous contrast is extremely useful to evaluate the vascular anatomy, mediastinal and hilar lymph nodes, and the position of the tumor relative to adjacent organs. PET scan is used to evaluate distant and lymph nodal metastasis as well as to identify the metabolic activity of the tumor. EBUS or mediastinoscopy is performed for invasive mediastinal staging [2].
Uniportal Right Upper Lobe Technique for Lung Cancer
Patient Positioning, Uniportal Access, and Lobectomy Overview
We initiate single-lung ventilation under general anesthesia in all our patients. We position the patient in a full lateral decubitus with a breakpoint just above the iliac crest for a hyperextension of the chest. This will enlarge the intercostal spaces facilitating the access to the pleural cavity (Fig. 1). The surgeon and the assistant position themselves in front of the patient, so they will have the same viewing angle, which allows a better coordination of movements inside the chest cavity.
Conventional and dedicated VATS instruments are used along with a 5-mm, 30o camera. A single 3–4 cm incision is made in the fourth intercostal space between the anterior axillary and the median axillary line. In women, we take care to avoid the breast. Access to the pleural cavity is easier when a wound protector is used.
The right upper lobectomy begins with the inspection of the pleural space to ensure resectability of the tumor and the absence of metastatic disease. Subsequently, the following steps are taken to perform the lobectomy through the single port:
-
1.
Ligation of the anterior trunk of the pulmonary artery
-
2.
Transection of right upper lobe bronchus
-
3.
Ligation of right upper lobe pulmonary vein
-
4.
Completion of the fissure
-
5.
Lymphadenectomy
Ligation of the Pulmonary Artery Anterior Trunk
We position the right upper lobe (RUL) towards the posterior chest wall to expose the anterior and the superior portions of the pulmonary hilum. The mediastinal pleura is opened from the superior pulmonary vein (SPV) towards the posterior portion of the airway. Care is taken to identify the phrenic nerve and the proper plane of dissection between the azygos vein and the superior structures of the pulmonary hilum. The pleura must be dissected all the way to the back wall of the bronchus intermedius (BI), so the carina between the right upper lobe bronchus (RULB) and BI can be identified. This posterior dissection will allow the RUL to be more mobile and allow the RULB to be easily encircled. The dissection can be performed bluntly or with the help of scissors, an electrocautery, or an ultrasonic scalpel. We avoid blunt dissection to decrease bleeding. Repeating the dissection from the SPV towards the airway will progressively expose the SPV, the anterior trunk (AT) of the pulmonary artery and the airway.
With a thoracoscopic dissection instrument, we liberate all adhesions between the SPV and the AT, as well as adhesions between the AT and the airway. It is important to avoid pressure over the artery to prevent hematomas and tearing of the wall of the artery while safely encircling the AT. Hilar and lobar lymph nodes (#10 and #11) can be removed during the vascular dissection and sent for frozen-section analyses. When stapling the AT, only one instrument should be used to apply cranial traction to the lobe. This will result in upright placement of the AT, and the staple device will easily and safely slide behind the artery (Fig. 2). Due to the straight view of the artery afforded by the uniportal approach, it is rarely necessary to articulate the staple device.
Dissection of the Right Upper Lobe Bronchus
The RULB is behind and lateral to the AT. Without changing the position of the instruments, you can proceed with its dissection after the transection of the AT is completed. The RULB can be bluntly dissected with an instrument protecting the pulmonary artery. An interlobar lymph node will be identified at the carina between the RULB and BI. Once this lymph node is removed, the dissection around the bronchus is straightforward, especially if the posterior pleura has been liberated. We apply continuous pressure at the carina of the RULB, towards the posterior chest wall, with a long thoracoscopic blunt dissector. Once we are able to go around the RULB, we release as much of the lung as possible and release the artery from the RULB, so that a staple device can be safely introduced. We usually perform a ventilation test to ensure proper stapling. After we transect the RULB, we like to dissect from the bronchial stump towards the BI. This will later facilitate the completion of the fissure (Fig. 3).
Dissection of Right Upper Lobe Vein
Once the AT and the RULB are divided, we reposition the lobe for an anterior dissection. With some posterior traction over the RUL, the superior and inferior pulmonary veins must be identified. In general, the SPV receives the middle lobe vein(s) and the upper lobe vein(s). It is important to identify the proper level of dissection between those two veins to develop the plane that will allow full release the right upper lobe vein (RULV). At the other margin of the RULV, the release must be more delicate because of the proximity between the RULV and the pulmonary artery. Once both borders of the RULV are free, we always pass a vessel loop around the RULV to fully liberate the vein (Fig. 4). Stapling the RULV is the most demanding step of this operation, not only because the vein is directly in front of the working incision, but also because the pulmonary artery is directly behind the vein, which makes it dangerous to pass the staple device around the vein. However, when the vein is largely released from all its adhesions, it becomes mobile and flexible allowing anterior traction with the blade of the staple device for a safe passage around the vein, distant from the artery.
Completion of the Fissure
Once the hilar elements of the lobe have been dissected, the superior lobe should be placed in its anatomic position to allow identification of the fissure. Usually, there is an outline of the fissure between the lobes, but in the absence of this sign, the middle lobe vein is an important landmark. After placing a couple of staple loads in the minor fissure, the limit between upper and middle lobes will be clearly identified at the pulmonary hilum. We section the parenchyma along the fissure, towards the major fissure, taking care to ensure that the RULB stump stays within the surgical specimen (Fig. 5). It is possible to transect one or two arterial branches (e.g. the posterior ascending artery) along with the fissure (the “fissureless technique”). Alternatively, those vessels can be independently ligated with vascular staples.
Lymphadenectomy
We routinely perform hilar and mediastinal lymphadenectomy. We resect the hilar and interlobar lymph nodes when dissecting the hilum and complete the mediastinal lymphadenectomy after the lobectomy. All lymph nodes are sent for frozen-section analysis. When positive lymph nodes are found, we extend the lymphadenectomy.
Final Steps
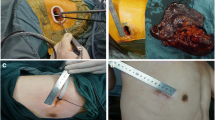
The lobe can be removed through the uniportal incision if the tumor is smaller than 3 cm, does not infiltrate the visceral pleura, and if a wound protector is used. Otherwise, the resected lobe should be placed inside a disposable bag to avoid contact with the incision or tearing and spillage during removal. We perform an intercostal nerve block intrapleurally from the first to the seventh intercostal space with bupivacaine (0.25%, 3 mL per space) (Fig. 6). Before closing the incision, we insert a 24 F chest tube through the working incision and maintain it in a water seal (Fig. 7). A routine postoperative bronchoscopy is done for airway toilette while the patient is still intubated.
Postoperative Care
Early ambulation after surgery, efficient analgesia, and respiratory exercises are key steps for the patient’s proper recovery. The drain is removed in the absence of an air leak and if the drainage is less than 300 mL in 24 h.
References
Swanson SJ, Herndon JE, D’Amico TA, Demmy TL, McKenna RJ, Green MR, et al. Video-assisted thoracic surgery lobectomy: report of CALGB 39802 – a prospective, multi-institution feasibility study. J Clin Oncol. 2007;25:4993–7.
National Comprehensive Cancer Network (NCCN). NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®). Non-small cell lung cancer. Version 4.2016. Jan 12, 2016. Abstract available at http://www.ncc.org/professionals/physician_gls/pdf/nscl.pdf.
Howington JA, Blum MG, Chang AC, Balekian AA, Murthy SC. Treatment of stage I and II non-small cell lung cancer: diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2013;143(Suppl 5):e278S–313S.
Scott WJ, Allen MS, Darling G, Meyers B, Decker PA, Putnam JB, McKenna RW, Landrenau RJ, Jones DR, Inculet RI, Malthaner RA. Video-assisted thoracic surgery versus open lobectomy for lung cancer: a secondary analysis of data from the American College of Surgeons Oncology Group Z0030 randomized clinical trial. J Thorac Cardiovasc Surg. 2010;139(4):976–83.
Kara HV, Balderson SS, D’Amico TA. Modified uniportal video-assisted thoracoscopic lobectomy: Duke approach. Ann Thorac Surg. 2014;98:2239–41.
Battoo A, Jahan A, Yang Z, Nwogu CE, Yendamuri SS, Dexter EU, Hennon MW, Picone AL, Demmy TL. Thoracoscopic pneumonectomy: an 11-year experience. Chest. 2014;146:1300–9.
Drevet G, Ugalde Figueroa P. Uniportal video-assisted thoracoscopic surgery: safety, efficacy and learning curve during the first 250 cases in Quebec, Canada. Ann Cardiothorac Surg. 2016;5(2):100–6.
RJ MK Jr, Houck W, Fuller CB. Video-assisted thoracic surgery lobectomy: experience with 1,100 cases. Ann Thorac Surg. 2006;81(2):421–5.
Onaitis MW, Petersen RP, Balderson SS, Toloza E, Burfeind WR, Harpole DH Jr, D’Amico TA. Thoracoscopic lobectomy is a safe and versatile procedure: experience with 500 consecutive patients. Ann Surg. 2006;244(3):420–5.
Rocco G, Martin Ucar A, Passera E. Uniportal VATS wedge pulmonary resections. Ann Thorac Surg. 2004;77:726–8.
Gonzalez D, Paradela M, Garcia J, de la Torre M. Single-port video-assisted thoracoscopic lobectomy. Interact Cardiovasc Thorac Surg. 2011;12:514–5.
Gonzalez-Rivas D. VATS lobectomy: surgical evolution from conventional VATS to uniportal approach. Sci World J. 2012;2012:780842.
Li C, Ma H, He J, Ni B, Xu C, Zhao J. Clinical analysis of thoracoscopic lobectomy in the treatment of peripheral lung cancer with single utility port. Chin J Lung Cancer. 2013;16:487–91.
Akter F, Routledge T, Toufektzian L, Attia R. In minor and major thoracic procedures is uniport superior to multiport video-assisted thoracoscopic surgery? Interact Cardiovasc Thorac Surg. 2015;20(4):550–5.
Perna V, Carvajal AF, Torrecilla JA, Gigirey O. Uniportal video-assisted thoracoscopic lobectomy versus other video-assisted thoracoscopic lobectomy techniques: a randomized study. Eur J Cardiothorac Surg. 2016;50:411–5.
Gonzalez-Rivas D, D’Amico T, Jiang G, Sihoe A. Uniportal video-assisted thoracic surgery: a call for better evidence, not just more evidence. Eur J Cardiothorac Surg. 2016;50(3):416–7.
Gonzalez-Rivas D, Fernandez R, Fieira E, et al. Uniportal video-assisted thoracoscopic bronchial sleeve lobectomy: first report. J Thorac Cardiovasc Surg. 2013;145:1676–7.
Gonzalez-Rivas D, Delgado M, Fieira E, et al. Double sleeve uniportal video-assisted thoracoscopic lobectomy for non-small cell lung cancer. Ann Cardiothorac Surg. 2014;3:E2.
Gonzalez-Rivas D, Delgado M, Fieira E, et al. Uniportal video-assisted thoracoscopic pneumonectomy. J Thorac Dis. 2013;5(Suppl 3):S246–52.
D’Amico TA. Operative techniques in early-stage lung cancer. J Natl Compr Cancer Netw. 2010;8:807–13.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Electronic Supplementary Material
(MP4 493595 kb)
Rights and permissions
Copyright information
© 2019 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Andrade, H., Vieira, A., Figueroa, P.U. (2019). Uniportal Right Upper Lobectomy. In: Gonzalez-Rivas, D., Ng, C., Rocco, G., D’Amico, T. (eds) Atlas of Uniportal Video Assisted Thoracic Surgery. Springer, Singapore. https://doi.org/10.1007/978-981-13-2604-2_21
Download citation
DOI: https://doi.org/10.1007/978-981-13-2604-2_21
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-13-2603-5
Online ISBN: 978-981-13-2604-2
eBook Packages: MedicineMedicine (R0)