Abstract
Cholelithiasis and cholecystitis represent common causes of upper abdominal pain in adult population. Imaging of the gallbladder has changed dramatically in recent decades; US still represents the method of choice for detection of gallstones for its high sensitivity and wide availability; however, CT and MR can allow an accurate, noninvasive imaging especially in patients with severe symptoms and suspected complications.
The characteristic US finding of gallstones is a highly reflective echo from the anterior surface of gallstones with a marked posterior acoustic shadowing.
CT is less sensitive than US in the detection of stones but is better able to demonstrate severe complications of acute cholecystitis.
MRI, including MR cholangiopancreatography (MRCP), can be a valuable complement in patients with severe symptoms, especially when US and CT findings are inconclusive, allowing a detailed evaluation of the biliary tract with the advantages of improved stone detection and absence of ionizing radiation.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Gallbladder disease
- Gallstones
- Choledocholithiasis
- Acute cholecystitis
- Computed tomography
- MR cholangiopancreatography
13.1 Introduction
Gallbladder disease is one of the most common conditions that affects a significant portion of the worldwide population, and symptomatic cholelithiasis is responsible of a significant percentage of emergency department visit for abdominal pain.
The epidemiology and risk factors of cholelithiasis have been widely investigated over the last several decades. Gallstones formation is the result of a complex interaction of multiple factors, including increasing age, hormonal effects (female gender, parity, exogenous oestrogens) metabolic disorders (obesity, diabetes mellitus, dyslipidaemia), dietary factors (high cholesterol diets), liver disease (cirrhosis, HCV infection), gallbladder stasis (long-term parental nutrition, low physical activity), and also genetics factors [1].
Crystalline deposits in the gallbladder are classified by chemical composition: cholesterol stones (>70% of cholesterol content), the most common type in the Western world, formed by supersaturation of cholesterol and associated with a decrease in the quantity of bile salt and lecithin, and mixed stones (from 30 to 70% of cholesterol content) and pigmented stones (cholesterol <30%), further distinguished into black and brown stones. Black stones are formed from polymerized calcium bilirubinate and are associated with hemolytic disorders and cirrhosis; brown pigment stones are composed of unpolymerized calcium bilirubinate, are most common in Oriental population, and are correlated with recurrent pyogenic cholangitis and biliary parasite infections [2,3,4].
As well as their cause, the types of gallstone vary by the measures attempted to prevent their formation, their response to dissolution therapy, and their appearance on imaging procedures [5].
The prevalence of cholelithiasis in the developed countries varies between 5 and 25%, and most patients are asymptomatic. It was calculated that each year approximately 2–4% of people with gallstones develop symptoms [5, 6] with biliary colic being the most common symptom.
13.2 Biliary Tract Obstruction
13.2.1 Cholelithiasis and Biliary Colic
Biliary colic is typically steady in quality rather than “colicky” as the name implies, and it is described as a constant, dull right upper quadrant abdominal pain, sometimes radiating to the right back or the shoulder and not relieved or exacerbated by movement, position, or bowel function. Typically, pain will last more than 30 min with the maximum time being 6 h [7, 8].
It results from gallbladder distention after acute and usually transient obstruction of the cystic duct by stones or sludge. When the stone falls back into the gallbladder or migrates into the common bile duct (CBD), the pain usually subsides; otherwise, gallstones can obstruct the cystic duct or gallbladder neck with an irritation of the gallbladder mucosa, a subsequent release of several inflammatory mediators, and progressive gallbladder wall inflammation, typically leading to an acute cholecystitis.
The presence of biliary stones into the choledochus defines the condition of choledocholithiasis.
This pathological entity is classified as primary or secondary according to stone origin: the primary form refers to stones formed directly within the biliary tree, while the secondary refers to stones ejected from the gallbladder. Primary choledocholithiasis is generally composed of brown stones and is rare in Western populations, while secondary choledocholithiasis is characterized by a stone composition analogous to that of cholelithiasis, with cholesterol as the most common type [9].
Once in the CBD, stones may reach the duodenum following the bile flow; otherwise, also owing to the smaller diameter of the distal duct caliber at the Vater papilla, they may remain in the choledochus. In this latter case, gallstones may be mostly asymptomatic or cause a variety of bile flow problems, including complete obstruction and jaundice. Bile stasis may be also responsible for bile infection and consequent ascending cholangitis, whereas bile/pancreatic juice flow obstruction may potentially trigger the intrapancreatic activation of pancreatic enzymes, causing acute biliary pancreatitis. Hepatic abscesses may also be a rarer infectious complication of choledocholithiasis, whereas chronic CBD obstruction may also cause biliary cirrhosis.
Extremely rarer is the condition of an obstruction of the common hepatic duct due to extrinsic compression by an impacted gallstone in the gallbladder neck, known as Mirizzi syndrome. Patients typically present with fever, right upper quadrant pain, and obstructive jaundice. Repeated bouts of recurrent cystic duct stone impaction and inflammation may lead to a cholecystobiliary fistula [10].
13.2.1.1 Imaging of Primary Condition
Since its advent in 1968, the endoscopic retrograde cholangiopancreatography (ERCP) has become the gold standard in the setting of biliary obstruction. It is an invasive procedure technique for the examination and intervention of the biliary tract, with a reported complication rate of 1 to 9% and a mortality rate from 0.2 to 0.5% [11].
Advances in biliary radiology with US, CT, and MRI technology have allowed an accurate, noninvasive imaging of the biliary tree and pancreas, in the setting of biliary obstruction and in the investigation of its causes and severity. In some cases, a multimodality imaging approach may be necessary.
13.2.1.1.1 US
Abdominal ultrasonography is the imaging of choice in patients with upper abdominal quadrant pain and is widely recommended as the initial imaging test in case of suspicion of biliary colic because of its high sensitivity and accuracy, noninvasiveness, lack of ionizing radiations, relatively low cost, and widely available.
Its accuracy for detecting gallbladder stones is more than 95%, and its sensitivity is comparable to that of MR cholangiopancreatography (MRCP) (97.7%), although it is less sensitive for the detection of microlithiasis and biliary sludge [12].
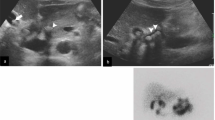
The characteristic findings of gallstones at US are a highly reflective echo from the anterior wall of the gallstone, gravitational mobility of the gallstone on repositioning the patient, and marked posterior acoustic shadowing (Fig. 13.1). This latter finding is extremely important in regard to the specificity of the technique and furthermore for the differential diagnosis of a gallbladder mass seen at US, because non-shadowing structures are considerably less likely than shadowing structures to represent gallstones.
When the gallbladder is completely filled with stones, the resulting appearance is termed the wall-echo-shadow sign (Fig. 13.2): the anterior gallbladder wall is echogenic; a thin layer of bile immediately underneath the anterior wall is usually seen as a dark line; finally, the most superficial stones are seen as a highly echogenic layer beneath the bile with associated intense shadowing that obscures the deeper stones and the posterior gallbladder wall [12].
Even though US has a high specificity for choledocholithiasis, its sensitivity ranges from 22 to 33% for detecting CBD stones [13, 14].
The major limitation for US in detecting CBD stones is mostly represented by the presence of intestinal gas, which often obscures the distal common duct and the ampulla of Vater.
Operator experience also plays a major role: when the examination is performed by an expert operator, sensitivity is nearly double (77–90%) than that of an operator with little experience (37–47%) [15].
US, however, is able to detect indirect signs of obstruction, in particular the subsequent dilatation of the CBD and even of the intrahepatic biliary tree. Biliary dilatation greater than 6 mm in patients with an intact gallbladder and than 10 mm postcholecystectomy is suspected of biliary obstruction.
13.2.1.1.2 CT
Although ultrasonography (US) is the most useful imaging modality for initial evaluation of the biliary system, multidetector computed tomography (CT) is often ordered in the emergency department for patients who present with nonspecific abdominal complaints or in cases where US findings are equivocal.
The sensitivity of CT for detecting choledocholithiasis varies between 72 and 88%; however, sensitivities for direct depiction (excluding indirect signs like ductal dilatation from criteria) of CBD stones have not exceeded 75% [16,17,18].
The appearance of gallstones on CT imaging varies with their chemical composition; stones may be heterogeneous in appearance, ranging from being heavily calcified and radiopaque to being slightly less radiopaque than bile due to cholesterol and to having gas attenuation due to locules of nitrogen gas, and may vary in appearance even within the same patient [19] (Fig. 13.3).
Nitrogen gas accumulation within gallstone fissures is sometimes observed in a star-shaped pattern on CT, termed the “Mercedes-Benz” sign [12, 20].
Approximately 10 to 20% of gallstones is composed of pure cholesterol, which are low in density, and they appear isoattenuating with bile, resulting in being hard to see on CT images.
Detection of biliary stones depends in part on technologic factors and in part on the care taken by the interpreting physician.
In general, CBD stones at CT may be better evaluated using thin sections and multiplanar reconstructions; unenhanced CT to establish a baseline helps identify biliary stones and confirm their lack of contrast enhancement. The use of narrow window settings can accentuate the attenuation difference between the stone and adjacent bile or soft tissue, improving their detection [18] (Fig. 13.4).
A 66-year-old woman with choledocholithiasis. Axial (a) non-enhanced CT image with narrow window setting shows hyperdense sludge within the iuxtapapillary choledochus (empty arrow). Coronal (b) contrast-enhanced CT image confirm a dilated CBD with intraluminal sludge seen as mildly increased density (white arrow) in hypoattenuating bile
Baron has recommended using the highest kilovoltage setting (140 kVp) to increase the chances of distinguishing stones from the bile [21].
A portal venous phase image, obtained through the abdomen 70–80 s after the intravenous injection of a 100–150-mL bolus of contrast material with a high iodine concentration (300–400 mg of iodine per millimeter), is required [17].
Traditionally, the presence or absence of bile duct stones can be determined through the criteria previously described by Baron, who illustrated the appearance of stones depending on a slice of examination [22]. In particular, the stone can be seen as a central density surrounded by hypoattenuating bile or ampullary soft tissue (target sign); otherwise, a faint rim of increased density can be visible along peripheral margin of low-density calculus (rim sign). Again, a calculus with increased density that is surrounded by a crescent of hypoattenuating bile is suggestive of the crescent sign.
When visible on CT images, biliary stones have a lamellated appearance and are angulated and geometric in shape and tend to be in a dependent posterior location in the biliary tract, with a crescent of bile outlining the anterior portion of the stone. Furthermore, signs of inflammation such as periductal edema, biliary epithelial thickening, and mural enhancement may point to local irritation caused by stones or to associated cholangitis or cholecystitis. However, mural enhancement has been reported to be frequently seen with malignancy and should prompt careful investigation [17].
A particular kind of CT imaging helpful for patients with suspected choledocholithiasis is the CT cholangiography, which provides a noninvasive opacification of the biliary tract and can be achieved with the administration of intravenous positive contrast materials, such as iopanoic acid, which are excreted into the bile. CT cholangiography is helpful for patients with suspected choledocholithiasis (sensitivity 86–93%, specificity 100%). It has also been shown to have sensitivity in diagnosing bile duct stones comparable with magnetic resonance cholangiography (>90%) and higher than unenhanced helical CT [23, 24].
However, this technique has some disadvantages that limit its use: a pre-imaging medication with antihistaminic drugs is required to prevent potentially life-threatening allergic reactions; a higher dose of radiation is needed, compared with conventional helical CT; and furthermore, the excretion of currently available biliary contrast materials is variable and is influenced by poorly understood factors. In particular, patients with liver insufficiency and high serum bilirubin levels (levels >3 mg/dl) often have CT cholangiographic images with insufficient opacification of bile ducts [25].
Definitely, CT imaging is better able to accurately demonstrate the location (97%) and cause (94%) of biliary obstruction, compared with US, but US is still more sensitive, specific, and accurate for diagnosis of cholelithiasis and has been shown to have a much higher positive predictive value (75% vs 50% for CT) and negative predictive value (97% vs 89% for CT) for diagnosing acute biliary disease [26].
13.2.1.1.3 MRI
In acute biliary disorders, MR imaging, including MR cholangiopancreatography (MRCP), can be a valuable complement to other imaging strategies in patients with severe symptoms and those suspected of having serious complications, especially when US and CT findings are inconclusive.
About 15–30% of patients who have acute biliary disorders are estimated to require MR imaging.
Because of its very high tissue contrast, multisequence MR imaging can provide a more comprehensive and detailed evaluation of the biliary tree and pancreatic duct, and because of its noninvasiveness and for the absence of the morbidity and mortality risk associated with ERCP, it has been widely adopted in the work-up of biliary obstruction [27].
On T1-weighted images, pigment gallstones appear to be hyperintense, while cholesterol gallstones are hypointense on the T1-weighted images; the reason of hyperintensity of pigment gallstones on T1-weighted images is in their composition, in particular in their metal ion content [28].
Gallstones are well depicted on MRCP, regardless of their location, and appear on T2-weighted images as foci of low signal intensity surrounded by bright bile (Fig. 13.5 and Fig. 13.6). Several studies have demonstrated that the sensitivity and specificity for MRCP in diagnosing choledocholithiasis are high (85–92% and 93–97%), with generally better results when sections with a thickness of 3 mm or less are acquired [29].
(a) Axial T2-weighted MR image shows a distended gallbladder with several small stones layered in the lumen. (b) MR cholangiopancreatogram confirms the presence of numerous tiny stones in the gallbladder; the main bile duct and intrahepatic branches are dilated, but non-stones are clearly present in the lumen
However, one important pitfall is represented by the reduced accuracy of MR cholangiography in the detection of small stones. Even with thin-section 3D imaging techniques, the sensitivity for stones that are 3 mm or smaller is substantially less than for larger calculi and may be less than 50%.
Additional limitations have also been reported, such as mistaking multiple impacted stones (with minimal surrounding bile) for a stricture or misidentifying pneumobilia, which manifests as signal voids with all sequences, for an intrabiliary stone [30].
When stones are not identified despite a high level of clinical suspicion, more invasive studies such as ERCP or endoscopic US may be pursued.
In particular, EUS is considered to have high sensitivity, especially for small CBD stones, seeming to be superior in the detection of CBD stones than 5 mm in diameter, compared to MRCP.
Endoscopic retrograde cholangiopancreatography (ERCP), despite its small but not negligible risk of complications, represents the most accurate diagnostic procedure for detecting CBD stones and also allowing their removal [31].
13.2.1.2 Imaging of Complications
The most frequent complications of choledocholithiasis are acute cholangitis and gallstone pancreatitis.
Acute cholangitis is a potentially life-threatening condition caused by partial or complete obstruction of the biliary tree with biliary stasis and increased intrabiliary pressure, which predisposes to bacterial overgrowth and ascending infection. Acute suppurative cholangitis refers to pus in the biliary tract, a condition that can lead to increased intraluminal pressure and precipitate biliary sepsis. Independent risk factors for this severe form of acute cholangitis include patient age older than 70 years, current smoker status, and an impacted biliary stone [32, 33].
The classical presentation is the “Charcot triad” of fever, right upper quadrant abdominal pain, and jaundice, which has however been reported to be present in 56–70% of patients. Patients can also present with “Reynold pentad”, which is Charcot triad with shock and altered mental status [34].
The most common bacteria isolated in infected bile without prior instrumentation are E. coli (31%), Klebsiella pneumoniae (17%), Enterococcus faecalis (17%), and Streptococcus species (17%) [35].
Complications of acute cholangitis include pyogenic hepatic abscesses, portal vein thrombosis, and biliary peritonitis (Fig. 13.7).
Choledocholithiasis with acute cholangitis, gallbladder perforation, and hepatic abscess. Coronal contrast-enhanced CT image (a) shows obstructive gallstones in the distal CBD with marked proximal intra- and extrahepatic biliary ductal dilatation and a hydropic gallbladder with dependent stones, focal disruptions of the wall, and multiple loculated pericholecystic fluid collections. Axial (b) contrast-enhanced CT image shows an intrahepatic abscess, represented by a low-attenuation lesion with subtle peripheral enhancement in the left liver lobe (white arrow)
The most common CT finding of acute cholangitis is biliary obstruction, with a diffuse and concentric thickening of the extrahepatic biliary duct with enhancement. Purulent bile may have increased CT attenuation. Transient hepatic attenuation differences (THADs), which appear as patchy, wedge-shaped, or geographic inhomogeneous hepatic parenchymal enhancement during the hepatic arterial phase on the CT, have been reported to be common in patients with acute cholangitis [36].
A recently described CT scoring system based on the extent of transient hepatic attenuation differences, degree of biliary dilatation, and presence of an obstructive lesion is highly sensitive (84–90%) and specific (84%) for the diagnosis of acute cholangitis [37].
There are no specific studies comparing multidetector CT with MR imaging in the setting of cholangitis. However, MR imaging seems to be more helpful than multidetector CT because of the higher signal-to-noise and contrast-to-noise ratios [38].
Enhancement of intrahepatic biliary duct walls is a common finding, reported in up to 92% of cases investigated with MR imaging, and it is best seen with gadolinium-enhanced delayed-phase fat-suppressed sequences.
Liver parenchymal changes, caused by an extension of the inflammatory process into the periportal tissues, with a dilatation of the peribiliary venous plexus and an increasing arterial flow, are seen in MR imaging as a high signal intensity on T2-weighted images and an inhomogeneous contrast enhancement with a wedge-shaped (72%), peripheral patchy (14%), or peribiliary (14%) pattern distribution [39].
Another potential complication of choledocholithiasis is represented by biliary pancreatitis.
Gallstone or biliary sludge impaction at the ampulla of Vater may cause ampullary spasm, pancreatico-biliary reflux, and obstruction of the common and pancreatic ducts, leading to acute pancreatitis (Fig. 13.8). Alternatively, biliary sludge may cause cholestasis or irritate the sphincter of Oddi, causing edema and biliopancreatic outflow obstruction. Anatomic variations such as a common pancreatico-biliary channel or pancreas divisum also raise the risk of acute pancreatitis [40, 41].
Most patients presenting with this complication present typical symptoms of pancreatitis, and fewer may also provide a history of biliary colic. The most common complaint is sudden-onset epigastric or right upper quadrant abdominal pain that is unrelenting and in 50% of cases radiates to the back [42].
Upper abdominal pain with amylase or lipase three times the upper normal limit is diagnostic of acute pancreatitis in many cases, and the addition of choledocholithiasis on imaging may sufficiently identify the cause as biliary. However, as previously said, ultrasonography may fail to detect stones smaller than 4 mm, and small stones are a known risk factor for biliary pancreatitis.
CT is often not an essential study in mild gallstone pancreatitis but provides more useful information in moderate to severe cases. The use of CT for stratification of severity and to direct management requires appropriate timing and technique because pancreatic involvement is best visualized on CT at a few days after the onset of symptoms. If an initial CT was obtained during diagnosis, it may need to be repeated if the patient’s pain is persistent and laboratory values fail to trend toward normal.
Findings at contrast-enhanced CT include an obstructive stone in a dilated CBD, associated with an edematous hypoattenuating pancreas with surrounding peripancreatic inflammation and fluid. Severe cases of pancreatitis may include findings of pseudocyst formation and parenchymal necrosis.
13.3 Cholecystitis
13.3.1 Acute Cholecystitis
Acute cholecystitis is defined as inflammation of the gallbladder, generally caused by obstruction of the cystic duct. The most common causes of cystic duct obstruction are gallstones or biliary sludge (acute calculous cholecystitis), which represent over 90% of cases. Cholecystitis can also occur in the absence of gallstones and is known as acalculous cholecystitis, a much rarer condition which occurs in critically ill or injured patients (trauma, burns, sepsis), and it is generally the result of biliary stasis and/or gallbladder ischemia [43].
According to the World Society of Emergency Surgery (WSES) guidelines 2016, there is no single clinical or laboratory finding with sufficient diagnostic accuracy to establish or exclude acute cholecystitis (Level IIB); combination of detailed history, complete clinical examination, and laboratory tests may strongly support the diagnosis of acute cholecystitis (Level IVC) [44].
13.3.1.1 Imaging of Primary Condition
13.3.1.1.1 US
US exam is the first imaging modality performed in the suspect of acute cholecystitis according to guidelines [44], because of its high sensibility, sensitivity, and availability. US detects the presence of gallstones and the signs of acute cholecystitis and assesses the positivity of Murphy sign.
Typical findings of acute cholecystitis on US exam are distention of gallbladder (defined as diameter greater than 5 cm on axial scan and greater than 8 cm in longitudinal scan) due to cystic duct obstruction and homogeneous wall thickening (defined as thickness > than 4 mm), finding that must be differentiated from gallbladder wall thickening related to other causes (Table 13.1). Other typical findings are stratified aspect of gallbladder wall related to submucosal edema (Fig. 13.9) and the presence of pericholecystic fluid. On Power Doppler hyperemia of the gallbladder wall could be demonstrated.
The detection of single or multiple obstructive stones or endoluminal sludge (Fig. 13.10) eventually confirms the underlying cause even though diagnostic performance of US in the diagnosis of inflammation of the gallbladder is not as good as its performance in the diagnosis of gallstones, as indicated in a recent meta-analysis [45]; moreover, it also presents several limitations related to body habitus.
13.3.1.1.2 CT
As previously said, the main limitations of CT exam performed in patients with clinical suspicion of acute biliary disorders are represented by the detection of stones, which could be difficult to recognize—especially if they are small in size—and the radiation exposure. For these reasons, its use is limited to patients with atypical symptoms and signs or when complications are suspected.
Similarly to US exam, CT findings of acute cholecystitis include gallbladder distension with inhomogeneous bile attenuation and gallbladder wall thickening, with intense mucosal enhancement after endovenous injection of contrast media and ipo-attenuating submucosal edema (Fig. 13.11). In addition, the presence of pericholecystic fat stranding, pericholecystic fluid, and hyper-enhancement of liver parenchyma adjoining to gallbladder fossa (CT rim sign) could be detected [46].
13.3.1.1.3 MRI
When findings in previous exams are ambiguous, MR imaging may be helpful in detecting stones, especially in particular sites like gallbladder neck and cystic duct and the associated gallbladder wall abnormalities [47].
On T2-weighted images, the gallbladder wall may show increased signal intensity and thickening. Pericholecystic fluid collections and edema of the surrounding liver tissue may be found. Periportal hyperintensity, although a nonspecific finding, may be observed on T2-weighted images. Although an inflammation-related increase in bile protein content may result in variable signal intensity of the bile on T1-weighted images, the bile usually appears markedly hypointense on T1-weighted sequences due to the impairment of gallbladder concentrating capability, a typical finding of the acute inflammatory phase. After administration of contrast media, gallbladder wall and surrounding fat show increased enhancement (Fig. 13.12). Similarly to CT exam, adjacent liver parenchyma can also show enhancement; this finding is due to a hyperemic response of the liver parenchyma related to acute inflammation of the gallbladder.
Axial T1-weighted MR image before (a) and after gadolinium administration (b) in a 61-year-old man with persistent jaundice and biliary stent implantation. Gallbladder appears over-distended with a hyper-enhanced wall thickening and an intraluminal air-fluid level with hyperintense small stones in dependent position
13.3.1.2 Complications
13.3.1.2.1 Emphysematous Cholecystitis
Emphysematous cholecystitis is a surgical emergency, prevalent in women and in diabetic population, and can occur as a complication of acalculous cholecystitis [48]. It is favored by hypoperfusion of cystic artery, and it carries a five times greater risk of perforation compared with uncomplicated acute cholecystitis [18].
It is typically caused by secondary infection of the gallbladder wall by gas-forming bacteria that infect the gallbladder wall producing intramural and intraluminal gas, such as Clostridium welchii, C. perfringens, E. coli, and Bacteroides fragilis.
On US exam it appears as inhomogeneous wall thickening, in which multiple hyperechoic, highly reflecting intramural spots can be detected (“dirty” shadowing). A more specific, though less common finding consists of small, non-shadowing echogenic foci rising up from the dependent portions of the gallbladder lumen, similar to effervescing bubbles in a glass of champagne (“champagne sign”). Also air in biliary ducts can be detected. The main limitations of ultrasound evaluation are represented by artifacts related to presence of gas within parietal wall or in the lumen of the gallbladder. For these reason CT (Fig. 13.13) is considered the most sensitive and specific imaging modality for identifying mural gas and for identifying complication like visceral perforation [49].
MR imaging has a supplementary role in providing information on intramural necrosis as well as intraluminal gas (Fig. 13.14). Gas in the gallbladder lumen and wall appears as signal void area, but it could be difficult to differentiate intramural gas from intramural stone. Susceptibility artifact at the air-tissue interface generates larger signal voids on fat-suppressed T1-w, fat-suppressed T2-w, and black blood T2-w spin-echo echo-planar images than on heavily T2-w, because heavily T2-w images are less affected by susceptibility. This finding could help distinguish intramural gas from an intramural stone [27].
Emphysematous cholecystitis in an 86-year-old woman: axial T2 fat-suppressed (a), T1 weighted out of phase (b), and contrast-enhanced (c). MR axial images show a marked gallbladder wall thickening with intense contrast enhancement. Inhomogeneous intraluminal material and void of signal areas due to air bubbles are also detected
13.3.1.2.2 Gangrenous Cholecystitis
Gangrenous cholecystitis occurs in up to 39% of patients with acute calculous cholecystitis [50] as a consequence of ischemic injury of gallbladder wall related to inflammatory processes. The presence of focal mural defect can evolve into visceral perforation leading to loculated or freely flowing intraperitoneal bile [46], pericholecystic or intrahepatic abscess, and peritonitis, depending on the site of perforation [50].
Compared to not complicated cholecystitis, on US exam gangrenous cholecystitis appears as inhomogeneous, irregular hypoechoic wall thickening of gallbladder wall with hypoperfused areas on Doppler corresponding to necrosis with laminated intraluminal membrane.
Findings on CT exam are similar to US; in particular poorly enhancing wall with focal hypoattenuating defects in the gallbladder mucosa or sloughed intraluminal membranes suggests gangrene [46]. Pericholecystic abscesses, appearing as hypoattenuating areas rounded by tiny rim enhancement (Fig. 13.15), have been described in cases of gangrenous cholecystitis with specificity close to 90% [51].
Gangrenous cholecystitis in a 64-year-old woman with leukocytosis and abdominal pain and a clinical history of pancreatic adenocarcinoma. Axial (a) and coronal (b) contrast-enhanced CT images show gallbladder wall thickening with focal mucosal defects (arrow) without frank perforation and pericholecystic inflammation with multiple loculated fluid collections (arrow head)
On MRI, the “interrupted rim sign” (patchy enhancement of the gallbladder mucosa) represents areas of necrosis. Gangrenous cholecystitis may be suggested by asymmetric gallbladder wall thickening due to intramural microabscesses, intramural hemorrhage, and complex pericholecystic fluid collections containing debris.
13.3.1.2.3 Hemorrhagic Cholecystitis
Hemorrhagic cholecystitis is more prevalent in patients with alytiasic cholecystitis than lytiasic one. It can clinically present with hemobilia as a consequence of necrosis of the wall with subsequent rupture of small parietal vessels or bleeding of pseudoaneurysm of cystic artery.
In addition to the signs of acute inflammation, gallbladder appears distended by inhomogeneous hyperechoic finely corpusculated material suspended in the lumen or stratified in the declive position. Gallbladder wall can present irregular thickening with focal hypoechoic and hyperechoic areas related to underlying necrotic processes and focal hemorrhagic areas, respectively.
On CT exam, the gallbladder appears distended by hyperdense endoluminal material rounded by irregular thickening of the wall, which has patchy density before and after contrast media administration due to coexisting ischemic and hemorrhagic areas. Blood breakdown products in the gallbladder wall and lumen can be clearly identified on pre-contrast MRI sequences, detecting, according to their specific intensity of signal, the age of the hemorrhage [52].
13.3.1.2.4 Suppurative Cholecystitis
Suppurative cholecystitis (gallbladder empyema) typically occurs in diabetic patients as a consequence of infection by suppurative bacteria (Fig. 13.16). In addition to findings of acute noncomplicated cholecystitis, gallbladder appears distended by corpusculated material that appears hyperechoic on US and hyperattenuating of CT exam, resembling sludge and without findings specific for empyema. At MRI imaging heavily T2-weighted imaging is sensitive enough to demonstrate purulent bile, which is dependent and has lower signal intensity. On other types of MR images, pus or purulent bile is difficult to demonstrate [27]. Only clinical signs and symptoms and percutaneous needle aspiration of the gallbladder can establish the diagnosis of empyema.
Acute suppurative cholecystitis in a diabetic patient with abdominal pain and fever. Non-enhanced axial CT image (a) shows a distended gallbladder with moderate hypodense wall thickening and intraluminal high-attenuating corpusculated material resembling sludge. The MR images performed 1 week later (b and c) show gallbladder wall fissurations with multiple pericholecystic fluid collections. Percutaneous cholecystostomy was subsequently performed and purulent material was drained
13.3.1.2.5 Cholecysto-Enteric Fistulas and Gallstones Ileus
Cholecysto-enteric fistulas are abnormal communications between gallbladder and gastrointestinal lumen via their wall and usually follow several episodes of acute or subacute cholecystitis.
Fistulas can occur between gallbladder and duodenum, in small bowel loops, or in colon (cholecysto-colic). When a gallstone greater than 2.5 cm in diameter passes through a fistula between the gallbladder and small bowel, the impacted gallstone on the ileocecal valve leads to a mechanical small bowel obstruction (gallstones ileus). Classical findings are defined in the “Rigler’s triad”: sign of small bowel mechanical obstruction, presence of gas in the lumen of gallbladder and/or in biliary tree (pneumobilia), and ectopic gallstone (usually in the right iliac fossa) (Fig. 13.17). The presence of two of the three signs of the Rigler’s triad is considered diagnostic, and CT represents the imaging study of choice [53].
Gallbladder perforation with an entero-biliary fistula in a 73-year-old woman with abdominal pain and high fever. Coronal (a) and axial (b) contrast-enhanced CT images show a collapsed gallbladder with an irregular wall thickening and inhomogeneous intense enhancement and a fistulous communication between the gallbladder wall and duodenum (black arrow). Axial and coronal CT images of the same patient (c–d) show dilated loops of small bowel up to the level of an obstructive gallstone, showing a hyperdense calcific core and a radiolucent peripheral component (white arrow)
Bouveret syndrome consists in a gastric outlet obstruction produced by a gallstone impacted in the pylorus or proximal duodenum; it can be considered a very proximal form of gallstone ileus [54].
13.3.1.2.6 Pseudoaneurysms of Cholecystic Artery
Pseudoaneurysms of cholecystic artery are among the worst complications of acute cholecystitis because of their high risk of bleeding, and they are due to parietal artery damage as a consequence of acute inflammation. They could be asymptomatic when detected as incidental findings or can present as acute, massive upper abdomen bleeding. CT is the best effective instrument to detect the presence of pseudoaneurysms and to plan their best treatment.
References
Stinton LM, Shaffer EA. Epidemiology of gallbladder disease: cholelithiasis and cancer. Gut Liver. 2012;6:172–87.
Portincasa P, Moschetta A, Palasciano G. Cholesterol gallstone disease. Lancet. 2006;368:230–9.
Qiao T, Ma RH, Luo XB, Yang LQ, Luo ZL, Zheng PM. The systematic classification of gallbladder stones. PLoS One. 2013;8(10):e74887.
O’Connell K, Brasel K. Bile metabolism and lithogenesis. Surg Clin N Am. 2014;94:361–75.
Gurusamy KS, Davidson BR. Gallstones. BMJ. 2014;348:g2669.
Shaffer EA. Epidemiology of gallbladder stone disease. Best Pract Res Clin Gastroenterol. 2006;20(6):981–96.
Diehl AK, Sugarek NJ, Todd KH. Clinical evaluation for gallstone disease: usefulness of symptoms and signs in diagnosis. Am J Med. 1990;89(1):29–33.
Portincasa P, Moschetta A, Petruzzelli M, Palasciano G, Di Ciaula A, Pezzolla A. Symptoms and diagnosis of gallbladder stones. Best Pract Res Clin Gastroenterol. 2006;20:1017–29.
Molvar C, Glaenzer B. Choledocholithiasis: evaluation, treatment, and outcomes. Semin Intervent Radiol. 2016;33(4):268–76.
Csendes A, Diaz JC, Burdiles P, Maluenda F, Nava O. Mirizzi syndrome and cholecystobiliary fistula: a unifying classification. Br J Surg. 1989;76(11):1139–43.
Mallery JS, Baron TH, Dominitz JA, et al. Complications of ERCP. Gastrointest Endosc. 2003;57(6):633–8.
Bortoff GA, Chen MYM, Ott DJ, Wolfman NT, Routh WD. Gallbladder stones: imaging and intervention. Radiographics. 2000;20(3):751–66.
Einstein DM, Lapin SA, Ralls RW, Halls JM. The insensitivity of sonography in the detection of choledocholithiasis. Am J Roentgenol. 1984;142(4):725–8.
Blackbourne LH, Earnhardt RC, Sistrom CL, Abbitt P, Jones RS. The sensitivity and role of ultrasound in the evaluation of biliary obstruction. Am Surg. 1994;60(9):683–90.
Gandolfi L,v Torresan F, Solmi L, Puccetti A. The role of ultrasound in biliary and pancreatic diseases. Eur J Ultrasound. 2003;16:141–59.
Miller FH, Hwang CM, Gabriel H, Goodhartz LA, Omar AJ, Parsons WG. Contrast-enhanced helical CT of choledocholithiasis. Am J Roentgenol. 2003;181(1):125–30.
Yeh BM, Liu PS, Soto JA, Corvera CA, Hussain HK. MR imaging and CT of the biliary tract. Radiographics. 2009;29(6):1669–88.
Patel NB, Oto A, Thomas S. Multidetector CT of emergent biliary pathologic conditions. Radiographics. 2013;33(7):1867–88.
Chan WC, Joe BN, Coakley FV, Prien EL, Gould RG, Prevrhal S, et al. Gallstone detection at CT in vitro: effect of peak voltage setting. Radiology. 2006;241(2):546–53.
O’Connor OJ, Maher MM. Imaging of cholecystitis. Am J Roentgenol. 2011;196:W367–74.
Baron RL. Gallstone characterization: the role of imaging. Semin Roentgen. 1991;26:216–25.
Baron RL. Computed tomography of the bile ducts. Semin Roentgenol. 1997;32(3):172–87.
Soto JA, Velez SM, Guzmán J. Choledocholithiasis: diagnosis with oral-contrast-enhanced CT cholangiography. Am J Roentgenol. 1999;172(4):943–8.
Soto JA, Alvarez O, Munera F, Velez SM, Valencia J, Ramirez N. Diagnosing bile duct stones: comparison of unenhanced helical CT, oral contrast-enhanced CT cholangiography, and MR cholangiography. Am J Roentgenol. 2000;175(4):1127–34.
Cabada Giadás T, De Toledo LSO, Martínez-Berganza Asensio MT, Cozcolluela Cabrejas R, Alberdi Ibáñez I, Alvarez López A, et al. Helical CT cholangiography in the evaluation of the biliary tract: application to the diagnosis of choledocholithiasis. Abdom Imaging. 2002;27(1):61–70.
Hou LA, Van Dam J. Pre-ERCP imaging of the bile duct and gallbladder. Gastrointest Endosc Clin N Am. 2013;23:185–97.
Watanabe Y, Nagayama M, Okumura A, Amoh Y, Katsube T, Suga T, et al. MR imaging of acute biliary disorders. Radiographics. 2007;27(2):477–95.
Hong-Ming T, Xi-Zhang L, Chiung-Yu C, Pin-Wen L, Jui-Che L. MRI of gallstones with different compositions. AJR Am J Roentgenol. 2004;182(6):1513–9.
Verma D, Kapadia A, Eisen GM, Adler DG. EUS vs MRCP for detection of choledocholithiasis. Gastrointest Endosc. 2006;64(2):248–54.
Irie H, Honda H, Kuroiwa T, Yoshimitsu K, Aibe H, Shinozaki K, et al. Pitfalls in MR cholangiopancreatographic interpretation. Radiographics. 2001;21:23–37.
Kondo S, Isayama H, Akahane M, Toda N, Sasahira N, Nakai Y, et al. Detection of common bile duct stones: comparison between endoscopic ultrasonography, magnetic resonance cholangiography, and helical-computed-tomographic cholangiography. Eur J Radiol. 2005;54:271–5.
Boey JH, Way LW. Acute cholangitis. Ann Surg. 1980;191(3):264–70.
Tsujino T, Sugita R, Yoshida H, Yagioka H, Kogure H, Sasaki T, et al. Risk factors for acute suppurative cholangitis caused by bile duct stones. Eur J Gastroenterol Hepatol. 2007;19(7):585–8.
Wada K, Takada T, Kawarada Y, Nimura Y, Miura F, Yoshida M, et al. Diagnostic criteria and severity assessment of acute cholangitis: Tokyo guidelines. J Hepato-Biliary-Pancreat Surg. 2007;14(1):52–8.
Flores C, Maguilnik I, Hadlich E, Goldani LZ. Microbiology of choledochal bile in patients with choledocholithiasis admitted to a tertiary hospital. J Gastroenterol Hepatol. 2003;18(3):333–6.
Pradella S, Centi N, La Villa G, Mazza E, Colagrande S. Transient hepatic attenuation difference (THAD) in biliary duct disease. Abdom Imaging. 2009;34(5):626–33.
Kim SW, Shin HC, Kim HC, Hong MJ, Kim IY. Diagnostic performance of multidetector CT for acute cholangitis: evaluation of a CT scoring method. Br J Radiol. 2012;85(1014):770–7.
Catalano O, Sahani DV, Forcione DG, Czermak B, Liu C-H, Soricelli A, et al. Biliary infections: spectrum of imaging findings and management. Radiographics. 2009;29(7):2059–80.
Bader TR, Braga L, Beavers KL, Semelka RC. MR imaging findings of infectious cholangitis. Magn Reson Imaging. 2001;19(6):781–8.
Testoni PA. Acute recurrent pancreatitis: etiopathogenesis, diagnosis and treatment. World J Gastroenterol. 2014;20:16891–901.
Cucher D, Kulvatunyou N, Green DJ, Jie T, Ong ES. Gallstone Pancreatitis. A review. Surg Clin N Am. 2014;94:257–80.
Attasaranya S, Fogel EL, Lehman GA. Choledocholithiasis, ascending cholangitis, and gallstone pancreatitis. Med Clin N Am. 2008;92:925–60.
Knab LM, Boller A-M, Mahvi DM. Cholecystitis. Surg Clin North Am. 2014;94(2):455–70.
Ansaloni L, Pisano M, Coccolini F, Peitzmann AB, Fingerhut A, Catena F, et al. WSES guidelines on acute calculous cholecystitis. World J Emerg Surg. 2016;11(16):2016.
Kiewiet JJS, Leeuwenburgh MMN, Bipat S, Bossuyt PMM, Stoker J, Boermeester MA. A systematic review and meta-analysis of diagnostic performance of imaging in acute cholecystitis. Radiology. 2012;264(3):708–20.
Shakespear JS, Shaaban AM, Rezvani M. CT findings of acute cholecystitis and its complications. AJR Am J Roentgenol. 2010;194(6):1523–9.
Catalano OA, Sahani DV, Kalva SP, Cushing MS, Hahn PF, Brown JJ, et al. MR imaging of the gallbladder: a pictorial essay. Radiographics. 2008;28(1):135–55.
Tellez LGS, Rodriguez-Montes JA, De Lis SF, Martin LGS. Acute emphysematous cholecystitis. Report of twenty cases. Hepatogastroenterology. 1999;46(28):2144–8.
Grayson DE, Abbott RM, Levy AD, Sherman PM. Emphysematous infections of the abdomen and pelvis: a pictorial review. Radiographics. 2002;22(3):543–61.
Chawla A, Bosco JI, Lim TC, Srinivasan S, Teh HS, Shenoy JN. Imaging of acute cholecystitis and cholecystitis-associated complications in the emergency setting. Singap Med J. 2015;56(8):438–44.
Bennett GL, Rusinek H, Lisi V, Israel GM, Krinsky GA, Slywotzky CM, et al. CT findings in acute gangrenous cholecystitis. Am J Roentgenol. 2002;178(2):275–81.
Elsayes KM, Oliveira EP, Narra VR, EL-Merhi FM, Brown JJ. Magnetic resonance imaging of the gallbladder: spectrum of abnormalities. Acta Radiol. 2007;48(5):476–82.
Ploneda-Valencia CF, Gallo-Morales M, Rinchon C, Navarro-Muñiz E, Bautista-López CA, de la Cerda-Trujillo LF, et al. Gallstone ileus: an overview of the literature. Rev Gastroenterol México (English Ed.) 2017;82(3):248–54.
Brennan GB, Rosenberg RD, Arora S. Bouveret syndrome. Radiographics. 2004;24:1171–5.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
13.1 Electronic Supplementary Material
Contrast-enhanced CT images show a voluminous mixed gallstone consisting in hypodense core and calcified shell with tiny peripheral gas collections. (MP4 23024 kb)
A 66-year-old woman with choledocholithiasis. CT images show hyperdense sludge within the iuxtapapillary choledochus. (MP4 10853 kb)
MR images show a distended gallbladder with several small stones layered in the lumen. The main bile duct and intrahepatic branches are dilated, but non-stones are clearly present in the lumen. (MP4 1816 kb)
MR images show a distended gallbladder with several small stones layered in the lumen. The main bile duct and intrahepatic branches are dilated, but non-stones are clearly present in the lumen. (MP4 941 kb)
Choledocholithiasis. MR images show multiple filling defects in the CBD, related to numerous calculi. (MP4 2822 kb)
Choledocholithiasis. MR images show multiple filling defects in the CBD, related to numerous calculi. (MP4 1500 kb)
Choledocholithiasis with acute cholangitis, gallbladder perforation, and hepatic abscess. Obstructive gallstones in the distal CBD with marked proximal intra- and extrahepatic biliary ductal dilatation and a hydropic gallbladder with dependent stones, focal disruptions of the wall, and multiple loculated pericholecystic fluid collections. In left liver lobe also an intrahepatic abscess is demonstrated. (MP4 12027 kb)
Contrast-enhanced CT images show a diffuse pancreatic swelling with peripancreatic and retroperitoneal edema and fat stranding, extending to the pararenal space (thickened Gerota’s fascia). Small calcified gallstones are present into the gallbladder lumen. (MP4 9960 kb)
Acute cholecystitis in a 51-year-old man with upper abdominal pain and fever, already treated by cholecystostomy. Contrastenhanced CT image show a gallbladder wall thickening, with intense mucosal enhancement and hypoattenuating submucosal edema. (MP4 14998 kb)
T1 MR image before and after gadolinium administration in a 61-year-old man with persistent jaundice and biliary stent implantation. Gallbladder appears over-distended with a hyper-enhanced wall thickening and an intraluminal air-fluid level with hyperintense small stones in dependent position. (MP4 17923 kb)
Emphysematous cholecystitis in an 86-year-old woman with upper abdominal pain and fever. Contrast-enhanced CT images show an over-distended gallbladder and an important wall thickening with intraluminal and intramural air. (MP4 8816 kb)
Emphysematous cholecystitis in an 86-year-old woman. MR images show a marked gallbladder wall thickening with intense contrast enhancement. Inhomogeneous intraluminal material and void of signal areas due to air bubbles are also detected. (MP4 1093 kb)
Emphysematous cholecystitis in an 86-year-old woman. MR images show a marked gallbladder wall thickening with intense contrast enhancement. Inhomogeneous intraluminal material and void of signal areas due to air bubbles are also detected. (MP4 1516 kb)
Emphysematous cholecystitis in an 86-year-old woman. MR images show a marked gallbladder wall thickening with intense contrast enhancement. Inhomogeneous intraluminal material and void of signal areas due to air bubbles are also detected. (MP4 14876 kb)
Gangrenous cholecystitis in a 64-year-old woman with leukocytosis and abdominal pain and a clinical history of pancreatic adenocarcinoma. Contrast-enhanced CT images show gallbladder wall thickening with focal mucosal defects without frank perforation and pericholecystic inflammation with multiple loculated fluid collections. (MP4 4396 kb)
Acute suppurative cholecystitis in a diabetic patient with abdominal pain and fever. CT images show a distended gallbladder with moderate hypodense wall thickening and intraluminal high-attenuating corpusculated material resembling sludge. (MP4 19822 kb)
Acute suppurative cholecystitis in a diabetic patient with abdominal pain and fever. The MR images performed 1 week later show gallbladder wall fissurations with multiple pericholecystic fluid collections. (MP4 2747 kb)
Acute suppurative cholecystitis in a diabetic patient with abdominal pain and fever. The MR images performed 1 week later show gallbladder wall fissurations with multiple pericholecystic fluid collections. (MP4 2429 kb)
Gallbladder perforation with an entero-biliary fistula in a 73-year-old woman with abdominal pain and high fever. Contrastenhanced CT images show a collapsed gallbladder with an irregular wall thickening and inhomogeneous intense enhancement and a fistulous communication between the gallbladder wall and duodenum. CT images also show dilated loops of small bowel up to the level of an obstructive gallstone, with hyperdense calcific core and a radiolucent peripheral component. (MP4 23740 kb)
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Veronica, B., Francesca, C., Luigi, L., De Gaetano, A.M., Riccardo, M. (2019). Imaging of Biliary Colic and Cholecystitis. In: Cova, M., Stacul, F. (eds) Pain Imaging. Springer, Cham. https://doi.org/10.1007/978-3-319-99822-0_13
Download citation
DOI: https://doi.org/10.1007/978-3-319-99822-0_13
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-99821-3
Online ISBN: 978-3-319-99822-0
eBook Packages: MedicineMedicine (R0)