Abstract
Diseases of the gallbladder and biliary tree are conditions that physicians routinely encounter, and they can present multiple diagnostic and treatment dilemmas. Cholelithiasis, choledocholithiasis, and acute cholecystitis are only some of the many potential diagnoses. Recent advances in imaging modalities have provided numerous options to aid clinicians in confirming or clarifying a particular diagnosis. For most cases of acute cholecystitis, ultrasound remains the initial diagnostic imaging of choice. It is inexpensive, readily available, and easily repeatable. HIDA scans also can be helpful, especially if an initial ultrasound is equivocal. These scans also have a role in the post-operative setting to evaluate for biliary leaks. MRI and MRCP provide high-resolution images of the hepatobiliary system with excellent tissue contrast. Currently, this modality is especially useful in the evaluation choledocholithiasis, and it will likely play an increasing role in the diagnosis of acute cholecystitis as MRI technology improves and becomes more widely available. CT scans are available to most patients, but have the downside of delivering ionizing radiation. They are most useful when the clinical picture is unclear or when there are additional symptoms outside of the right upper quadrant. By tailoring the selection of radiographic images to the individual patient scenario, clinicians can maximize diagnostic utility and mitigate unnecessary costs and radiation exposure.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Acute cholecystitis
- Acute calculous cholecystitis
- Acalculous cholecystitis
- Gangrenous cholecystitis
- Ultrasonography
- Cholescintigraphy
- HIDA scan
- Magnetic resonance imaging
- Magnetic resonance cholangiopancreatography
- Computed tomography
- Cholangiography
- Cholecystostomy
- Endoscopic ultrasound
Introduction
Diseases of the gallbladder and biliary tree are frequently encountered problems in the medical community. Acute calculous and acalculous cholecystitis, symptomatic cholelithiasis, choledocholithiasis, gallbladder polyps, gallbladder wall calcifications, and gallbladder malignancies can all present unique diagnostic and treatment dilemmas.
In the United States, gallstones affect approximately 20–25 million adults [1]. Fortunately, most individuals do not become symptomatic from their cholelithiasis [2]. Despite this fact, gallstones are one of the most expensive digestive disorders with an estimated annual cost of approximately $6 billion [3]. Due to the prevalence of gallstones and the advent of laparoscopy, cholecystectomies have become one of the most commonly performed abdominal operations with over 750,000 completed annually [4]. It is notable that only 15–17 % of laparoscopic cholecystectomies are performed for acute cholecystitis [5, 6].
Like many of the aforementioned conditions, acute cholecystitis can present many diagnostic difficulties for physicians, and there is an array of imaging modalities to help to confirm the findings of the history and physical exam. As it is not always clear which radiographic test is best for a particular clinical situation, the recently published Tokyo Guidelines have outlined severity criteria for acute cholecystitis and key imaging findings across different modalities to confirm the diagnosis [7].
Ultrasound
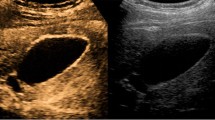
The initial test for the diagnosis of acute cholecystitis is currently abdominal ultrasound. This study has the advantage of being an inexpensive, widely available imaging modality that does not deliver any ionizing radiation. Structures of varying depth can be analyzed depending on the frequency of probe that is used. Additionally, its Doppler technology can provide information on vascular flow in the area of interest. Ultrasound’s accuracy in diagnosing the presence of gallstones (Fig. 4.1) has been consistently reported to be greater than 90 % [8]. Imaging findings that suggest acute cholecystitis include: gallbladder wall thickening greater than 4 mm, pericholecystic fluid, cholelithiasis, sludge, and a sonographic Murphy’s sign (Fig. 4.2).
Gray-scale ultrasound of the gallbladder with related abnormal findings. (a) Cholelithiasis and gallbladder wall thickening up to 8 mm. (b) Gallstone lodged in the gallbladder neck with associated wall thickening. (c) Cholelithiasis, thickened gallbladder wall, and pericholecystic fluid. (d) Cholelithiasis, sludge, pericholecystic edema, and mild gallbladder wall thickening
Despite all of these advantages, there are still some drawbacks to using ultrasound as a diagnostic imaging technique. Importantly, the acquisition of images is operator dependent. Moreover, a number of patient and anatomical factors can obscure the signal and result in poor image quality. Two main issues are obesity and bowel/bone between the gallbladder and the transducer on abdominal wall. As with all imaging, findings must be placed in the appropriate clinical context. For example, gallbladder wall thickening is not unique to acute cholecystitis and can be seen in cases of cirrhosis and hepatitis [9]. Furthermore, gallstones can have a similar appearance to gallbladder polyps (Fig. 4.3). However, gallstones are mobile, whereas polyps are fixed structures. By simply rotating the patient and acquiring additional images, important clinical information can be obtained.
Depending on the series, the reported sensitivity and specificity of ultrasound for the diagnosis of acute cholecystitis have varied greatly [10–14]. However, a recent systematic review and meta-analysis reported them to be 81 % (95 % Confidence Interval (CI): 75–87 %) and 83 % (95 % CI: 74–89 %), respectively [15]. In a prospective study that analyzed the ultrasound findings of 497 patients suspected of having acute cholecystitis, the positive predictive value of gallstones in combination with a thickened gallbladder wall and/or a positive sonographic Murphy’s sign ranged from 92 to 95 % [10].
Color Doppler can provide another potential information source to aid in clinical decision-making. One study showed that all patients with histologically proven acute cholecystitis had increased vascular flow in the distal two-thirds of the thickened gallbladder wall [16].
There is some controversy regarding which imaging modality is best for acute acalculous cholecystitis, as it can be difficult to clearly and definitively diagnose. Affected patients are often severely ill due to trauma, burns, sepsis, shock, or other postoperative complications. They cannot reliably participate in a physical examination and their laboratories values may be altered for other reasons. Compared to acute calculous cholecystitis, the pathology in these patients is likely a result of bile stasis and/or mucosal ischemia [17]. Ultrasound is easy to use, portable, and easily repeatable which minimizes logistical problems when dealing with critically ill patients. Therefore, ultrasound may make the most sense as the initial imaging modality for patients that cannot be easily transported to the radiology department.
Gallbladder wall thickness has been shown to be useful in diagnosing acute acalculous cholecystitis, with a wall thickness of greater than 3.5 mm having a specificity of 98.5 % [18]. Other criteria such as sludge, hydrops, and gallbladder distension have been cited as diagnostic criteria, but it is important to note that many intensive care unit patients have “abnormal” findings on ultrasound without having a diagnosis of acute acalculous cholecystitis [19, 20]. Multiple studies have shown a specificity of greater than 90 % for the diagnosis of acute acalculous cholecystitis by ultrasound, but the sensitivities have varied more widely and have been reported as low as 30 % [21–23].
In summary, due to its low cost, ease of use, and availability in many clinics and emergency rooms, the vast majority of patients with suspected acute cholecystitis undergo ultrasound as their initial imaging modality [11]. For clinical situations where the diagnosis is not entirely clear, it may be useful or necessary to pursue additional imaging studies.
Cholescintigraphy
Cholescintigraphy using technetium-99 m (99mTc) labeled hepatobiliary iminodiacetic acid (HIDA) is another commonly used imaging technique to confirm the diagnosis of acute cholecystitis. The radiolabeled agent is given intravenously after which it is extracted by the hepatocytes in the liver, secreted into the bile canaliculi, flows through the bile ducts and into the gallbladder, and then passes into the intestines [24]. The gallbladder usually begins to fill approximately 10 min into the study and is often completely filled by 30–40 min; however, up to 60 min is considered normal [25].
The classic finding of acute cholecystitis on a HIDA scan is persistent non-filling of the gallbladder, even on delayed imaging (Fig. 4.4) [25]. Additionally, increased radiotracer uptake in the liver parenchyma adjacent to the gallbladder fossa, known as the “rim sign,” has been shown to be a predictor of acute cholecystitis [26, 27]. False-positive test results do occur and are frequently seen in individuals who have been fasting for a prolonged time period (greater than 24 h) or who have received parenteral nutrition [28, 29].
Morphine (which stimulates contraction of the sphincter of Oddi and increases pressure in the biliary tree) augmented cholescintigraphy has been touted as a way to decrease the false-positive rate and improve diagnostic accuracy [30]. Cholecystokinin, with its ability to stimulate gallbladder contraction and lower sphincter of Oddi pressure, has been used to increase the diagnostic accuracy as well [31].
Cholescintigraphy has been consistently reported to have a higher sensitivity and specificity than ultrasound for the diagnosis of acute cholecystitis. In the aforementioned systematic review and meta-analysis, the sensitivity and specificity were 96 % (95 % CI: 94–97 %) and 90 % (95 % CI: 86–93 %), respectively [15]. While cholescintigraphy may have a higher diagnostic accuracy compared to ultrasound, the modality does have some limitations that have historically precluded its adoption as the initial imaging study of choice in patients with suspected acute cholecystitis. These issues are mostly logistical as nuclear medicine personnel are typically unavailable to perform the study on evenings and weekends. Comparatively, in many larger centers, ultrasound technicians are present 24 h per day, including weekends. Additionally, a HIDA scan takes longer than an ultrasound to complete, provides information limited to the biliary system, and exposes the patient to radiation, thereby limiting its attractiveness in pregnant patients.
As mentioned previously, the diagnosis of acute acalculous cholecystitis is a difficult clinical problem. While ultrasound often may be the preferred modality, cholescintigraphy should not be overlooked as a valuable tool to aid in the diagnosis. Some authors even have advocated its role as the initial imaging modality [32]. Reported sensitivities have ranged from 67 to 100 %, and specificities have been reported from 38 to 100 % [21–23, 33]. There have been concerns of increased false-positive rates in critically ill patients, but morphine augmentation has helped to alleviate this issue [23, 33].
HIDA scans are also useful in the postoperative setting to aid in the diagnosis of complications. Following cholecystectomy, there is an approximately 0.5 % risk of bile duct injury [34, 35]. For clinically significant bile leaks that go unrecognized at the time of surgery, patients are often discharged shortly thereafter and then present days later. Their symptoms can include abdominal pain and/or distension, nausea, vomiting, and possibly fevers. Initial imaging studies such as an ultrasound may demonstrate a fluid collection in the gallbladder fossa. HIDA scans are a useful and sensitive tool for determining if the fluid is biliary in nature (Fig. 4.5) [36, 37]. Additionally, obtaining delayed views are crucial to avoid missing bile leaks, especially when the initial images appear normal [38]. Furthermore, complete absence of emptying of the tracer from the liver may indicate a complete biliary obstruction as present with an inadvertently ligated common bile duct. Importantly, this study lacks the ability to pinpoint the exact site of the bile leak.
HIDA scan demonstrating a post-operative biliary leak following cholecystectomy. Shown from left to right are the images acquired at 5, 15, 30, and 60 min following radiotracer injection. By the final time point, there continues to be evidence of tracer uptake at the level of the liver which extends down into the right paracolic gutter
Consequently, cholescintigraphy is a useful imaging tool that can provide valuable information in multiple clinical settings related to biliary tract disease. However, the ability to perform the study may be limited by the availability of qualified personnel and the time necessary to acquire images.
Magnetic Resonance Imaging
Magnetic resonance imaging (MRI) technology has advanced greatly in recent years. However, MRI is still not considered a routine initial imaging study for patients with suspected acute cholecystitis. MRI is a costly exam that is less readily available when compared to ultrasound. The study time is also greater in length, although there have been reports of protocols for acute abdomen imaging that are as quick as 15 min [39, 40].
One clear benefit of MRI is that it does not deliver any ionizing radiation, which makes it a particularly useful tool in the evaluation of pregnant patients with right upper quadrant pain (Fig. 4.6) [41]. Additionally, MRI’s excellent tissue contrast provides high-resolution images of the biliary anatomy which allows for improved recognition of choledocholithiasis when compared to other imaging modalities (Fig. 4.7) [42].
Imaging findings on MRI that are suggestive of acute cholecystitis include: pericholecystic high signal, a thickened gallbladder wall, and an enlarged gallbladder [43, 44]. Multiple studies have demonstrated that MRI is equivalent to or slightly better than ultrasound in diagnosing acute cholecystitis [44, 45]. One study used the HASTE sequence (ultrafast protocol for image acquisition) with no additional contrast material to analyze the pericholecystic signal, and found that it yielded a diagnostic accuracy of 89 % [46]. While there are certainly fewer studies available to analyze MRI’s role in diagnosing acute cholecystitis, a recent meta-analysis demonstrated a sensitivity of 85 % (95 % CI: 66–95 %) and a specificity of 81 % (95 % CI: 69–90 %) [15].
Magnetic resonance cholangiopancreatography (MRCP) has become one of the main diagnostic imaging modalities for the investigation of the biliary tree and pancreatic ducts, as well as the body and tail of the pancreas. This study is useful for investigating biliary obstruction (due to choledocholithiasis, stricture, or malignancy), anatomic variants of the biliary anatomy, the pancreatic ducts, and potential postoperative complications following hepatobiliary surgery [47–49]. Some studies have even suggested MRCP is equivalent to endoscopic retrograde cholangiopancreatography (ERCP) for the diagnosis of choledocholithiasis [50, 51]. MRCP has been demonstrated to have a sensitivity of 84 %, a specificity of 94 %, a positive predictive value of 91 %, and a negative predictive value of 93 % for the diagnosis of choledocholithiasis [52].
Therefore, while MRI has been shown to effectively diagnose acute cholecystitis, its cost, time consumption, and limited availability have prevented its widespread adoption as a first-line imaging modality for that disease process. However, with improved MRI technology and the advent of MRCP, high-resolution images of the hepatobiliary system greatly assist clinicians in the diagnosis and treatment complex biliary and pancreatic pathology.
Computed Tomography
Computed tomography (CT) has become one of the most widely used imaging modalities in modern medicine. This technology is readily available and of moderate cost, but does have the downside of exposure to ionizing radiation. Also, CT scans are less accurate than ultrasound at diagnosing cholelithiasis with a reported accuracy of just under 90 % and a sensitivity of 79 % [53].
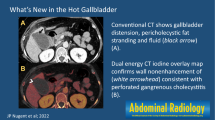
Signs of acute cholecystitis on CT scans include: gallbladder distension, wall thickening, pericholecystic fluid and fat stranding, and mucosal hyperenhancement (Fig. 4.8) [54]. Reactive hyperemia resulting in enhancement of the area of liver parenchyma adjacent to the gallbladder fossa may be present as well [54, 55]. Additionally, a tensile gallbladder fundus which displaces the abdominal wall may be a useful imaging sign to diagnose acute cholecystitis, especially in the disease’s early stages (Fig. 4.9) [56].
For the diagnosis of acute cholecystitis, CT scans have been shown to have a range of sensitivities from 39 to 92 % and a specificity range of 93–99 % [57, 58]. One study reported a positive predictive value of 50 %, and a negative predictive value of 89 % [57]. In more complex clinical situations, CT scans have been shown to have a sensitivity of 96 % for the diagnosis of acute gangrenous cholecystitis, and key imaging findings include an irregular or absent gallbladder wall, gas in the wall or lumen, intraluminal membranes, or a pericholecystic abscess (Fig. 4.10) [58]. Also, CT is the most sensitive and specific imaging modality for identifying gas within the gallbladder lumen or wall [59] and has been reported to have up to a 100 % sensitivity for diagnosing emphysematous cholecystitis [60].
CT scan demonstrating gangrenous cholecystitis. (a) Coronal image demonstrating focal mucosal loss of the gallbladder fundus with associated abscess extending into the liver parenchyma. (b) Axial image showing gallbladder wall thickening, pericholecystic fluid, and the area of focal gallbladder wall disruption
Given the accessibility of this technology, there has been some evidence to suggest an overuse of CT scans in evaluating patients with gallbladder disease, especially with presentation during off-hours [61]. However, it should be noted that CT imaging can provide important information when the clinical situation is unclear or a more complex diagnosis is being considered. CT scans are widely available and are most useful for patients with atypical presentations or when symptoms include areas of the abdomen outside of the right upper quadrant.
Intraoperative Cholangiography
Intraoperative cholangiography (Fig. 4.11) is performed in approximately 30 % of all cholecystectomies [62]. Clear preoperative indications for the procedure include: jaundice, elevated liver function tests and/or pancreatic enzyme levels, and ductal dilatation or choledocholithiasis seen on imaging studies [63]. There has been a great debate in the literature regarding the use of routine intraoperative cholangiography. Those surgeons in favor of this practice have argued that it results in a lower rate of biliary tract injury during cholecystectomy, an increased degree of intraoperative detection of common bile duct stones that can be treated at the time of initial surgery, and is a tool for surgical education [64]. Many other surgeons perform cholangiography only in select patient scenarios. Recent studies have suggested that there is limited, if any, benefit to performing routine intraoperative cholangiography with every cholecystectomy [65, 66]. There have even been reports of higher rates of bile duct injuries for surgeons who routinely perform cholangiography as compared to those who only do so selectively [67]. While this debate is likely to continue, the fact remains that intraoperative cholangiography can provide critical information about biliary anatomy that can be used to guide surgical therapy.
Percutaneous Cholecystostomy
The complication rate associated with performing a laparoscopic cholecystectomy for acute cholecystitis increases with the severity of the episode as well as the age of the patient. In patients who are poor surgical candidates, percutaneous placement of a cholecystostomy tube has been advocated as a temporary measure (until cholecystectomy can be performed) or as a definitive procedure [68]. It is performed under ultrasound or CT guidance, and it can be done by either a transabdominal or a transhepatic approach. The data on percutaneous cholecystostomy tubes are mixed with some studies suggesting their ability to be used as a first-line treatment for acute cholecystitis without interval cholecystectomy and others suggesting a role only when there are prohibitive operative risks [69–72]. In either case, percutaneous cholecystostomy tube placement will continue to be one treatment option for patients who are precluded from undergoing surgery on account of other medical comorbidities.
Endoscopic Drainage
Advances in endoscopy have allowed for increased access to the biliary tree and gallbladder for a variety of diagnostic and therapeutic procedures. Over the recent years, endoscopic approaches to gallbladder drainage have been reported with increasing frequency. These types of approaches are particularly useful in patients who are poor surgical candidates and who may have a contraindication to a percutaneous procedure. One option is to access the gallbladder through the transpapillary route and leave either a nasobiliary tube or a stent in place (Fig. 4.12). Alternatively, there are reports of transmural drainage through the distal antrum or the duodenum (Fig. 4.13).
Transpapillary gallbladder drainage in a 40-year-old male with a history of end-stage liver disease who presented with acute cholecystitis. (a) During ERCP, there was evidence of a cystic duct obstruction due to a gallstone. (b) Dilation of the cystic duct using a 4 mm balloon catheter. (c) Successful placement of a transpapillary ten French stent
Transduodenal gallbladder stent in a 70-year-old male with metastatic colon cancer who while receiving palliative chemotherapy developed acute cholecystitis. (a) Endoscopic ultrasound-guided transduodenal needle puncture with wire placement and subsequent balloon dilation of the tract. (b) Balloon dilation of the stent lumen. (c) Transduodenal lumen apposing covered metal stent within the gallbladder. Note: A common bile duct stent was also placed due to a biliary stricture
A systematic review combined data from multiple retrospective studies on naso-gallbladder drainage to achieve a pooled technical success rate of 81 % and a clinical response rate of 75 % [73]. Similarly, for endoscopic transpapillary gallbladder stenting, the technical success rate was 96 % and the clinical response rate was 88 % [73]. A recent prospective, randomized controlled trial (designed as a non-inferiority study) demonstrated that the technical and clinical success of endoscopic guided transmural gallbladder drainage was comparable to that of percutaneous transhepatic gallbladder drainage [74].
Endoscopic approaches for biliary tree access have undergone numerous advances in recent years and serve as an excellent therapeutic option for patients who are not able to undergo a surgical procedure.
Conclusion
Cholelithiasis and acute cholecystitis are common conditions that clinicians and surgeons encounter daily in practice. The recent advances in diagnostic imaging have provided numerous options to aid in the delivery of patient care. For most instances of acute cholecystitis, ultrasound still remains the initial diagnostic imaging of choice. HIDA scans play an important role in diagnosis, especially when the initial ultrasound is equivocal. Additionally, they are useful in the postoperative setting to investigate biliary leaks. MRI and MRCP provide high-resolution images of the hepatobiliary system with excellent tissue contrast. As MRI scanning becomes more ubiquitous and less expensive, this modality may have an increased role in the diagnosis of acute cholecystitis. CT scans are most helpful when the diagnosis of acute cholecystitis is unclear, or when there are additional symptoms outside of the right upper quadrant. CT scanning also has clinical utility when there is concern for complications of cholecystitis such intra-abominal abscess, gallbladder perforation, and gangrenous or emphysematous cholecystitis. By tailoring the selection of radiographic images to the individual patient scenario, clinicians can maximize diagnostic utility and mitigate unnecessary costs and radiation exposure.
References
Shaffer EA. Gallstone disease: epidemiology of gallbladder stone disease. Best Pract Res Clin Gastroenterol. 2006;20(6):981–96.
Halldestam I, Enell EL, Kullman E, Borch K. Development of symptoms and complications in individuals with asymptomatic gallstones. Br J Surg. 2004;91(6):734–8.
Everhart JE, Ruhl CE. Burden of digestive diseases in the United States part I: overall and upper gastrointestinal diseases. Gastroenterology. 2009;136(2):376–86.
Stinton LM, Myers RP, Shaffer EA. Epidemiology of gallstones. Gastroenterol Clin North Am. 2010;39(2):157–69. vii.
Steiner CA, Bass EB, Talamini MA, Pitt HA, Steinberg EP. Surgical rates and operative mortality for open and laparoscopic cholecystectomy in Maryland. N Engl J Med. 1994;330(6):403–8.
Orlando 3rd R, Russell JC, Lynch J, Mattie A. Laparoscopic cholecystectomy. A statewide experience The Connecticut Laparoscopic Cholecystectomy registry. Arch Surg. 1993;128(5):494–8; discussion 498–9.
Hirota M, Takada T, Kawarada Y, Nimura Y, Miura F, Hirata K, Mayumi T, Yoshida M, Strasberg S, Pitt H, et al. Diagnostic criteria and severity assessment of acute cholecystitis: Tokyo Guidelines. J Hepatobiliary Pancreat Surg. 2007;14(1):78–82.
Hessler PC, Hill DS, Deforie FM, Rocco AF. High accuracy sonographic recognition of gallstones. AJR Am J Roentgenol. 1981;136(3):517–20.
Ralls PW, Quinn MF, Juttner HU, Halls JM, Boswell WD. Gallbladder wall thickening: patients without intrinsic gallbladder disease. AJR Am J Roentgenol. 1981;137(1):65–8.
Ralls PW, Colletti PM, Lapin SA, Chandrasoma P, Boswell Jr WD, Ngo C, Radin DR, Halls JM. Real-time sonography in suspected acute cholecystitis. Prospective evaluation of primary and secondary signs. Radiology. 1985;155(3):767–71.
Alobaidi M, Gupta R, Jafri SZ, Fink-Bennet DM. Current trends in imaging evaluation of acute cholecystitis. Emerg Radiol. 2004;10(5):256–8.
Kalimi R, Gecelter GR, Caplin D, Brickman M, Tronco GT, Love C, Yao J, Simms HH, Marini CP. Diagnosis of acute cholecystitis: sensitivity of sonography, cholescintigraphy, and combined sonography-cholescintigraphy. J Am Coll Surg. 2001;193(6):609–13.
Chatziioannou SN, Moore WH, Ford PV, Dhekne RD. Hepatobiliary scintigraphy is superior to abdominal ultrasonography in suspected acute cholecystitis. Surgery. 2000;127(6):609–13.
Summers SM, Scruggs W, Menchine MD, Lahham S, Anderson C, Amr O, Lotfipour S, Cusick SS, Fox JC. A prospective evaluation of emergency department bedside ultrasonography for the detection of acute cholecystitis. Ann Emerg Med. 2010;56(2):114–22.
Kiewiet JJ, Leeuwenburgh MM, Bipat S, Bossuyt PM, Stoker J, Boermeester MA. A systematic review and meta-analysis of diagnostic performance of imaging in acute cholecystitis. Radiology. 2012;264(3):708–20.
Schiller VL, Turner RR, Sarti DA. Color doppler imaging of the gallbladder wall in acute cholecystitis: sonographic-pathologic correlation. Abdom Imaging. 1996;21(3):233–7.
Huffman JL, Schenker S. Acute acalculous cholecystitis: a review. Clin Gastroenterol Hepatol. 2010;8(1):15–22.
Deitch EA, Engel JM. Acute acalculous cholecystitis. Ultrasonic diagnosis. Am J Surg. 1981;142(2):290–2.
Molenat F, Boussuges A, Valantin V, Sainty JM. Gallbladder abnormalities in medical ICU patients: an ultrasonographic study. Intensive Care Med. 1996;22(4):356–8.
Boland GW, Slater G, Lu DS, Eisenberg P, Lee MJ, Mueller PR. Prevalence and significance of gallbladder abnormalities seen on sonography in intensive care unit patients. AJR Am J Roentgenol. 2000;174(4):973–7.
Mirvis SE, Vainright JR, Nelson AW, Johnston GS, Shorr R, Rodriguez A, Whitley NO. The diagnosis of acute acalculous cholecystitis: a comparison of sonography, scintigraphy, and CT. AJR Am J Roentgenol. 1986;147(6):1171–5.
Puc MM, Tran HS, Wry PW, Ross SE. Ultrasound is not a useful screening tool for acute acalculous cholecystitis in critically ill trauma patients. Am Surg. 2002;68(1):65–9.
Prevot N, Mariat G, Mahul P, Granjon D, Cuilleron M, Tiffet O, De Filipis JP, Jospe R, Auboyer C, Dubois F. Contribution of cholescintigraphy to the early diagnosis of acute acalculous cholecystitis in intensive-care-unit patients. Eur J Nucl Med. 1999;26(10):1317–25.
Doo E, Krishnamurthy GT, Eklem MJ, Gilbert S, Brown PH. Quantification of hepatobiliary function as an integral part of imaging with technetium-99m-mebrofenin in health and disease. J Nucl Med. 1991;32(1):48–57.
Lambie H, Cook AM, Scarsbrook AF, Lodge JP, Robinson PJ, Chowdhury FU. Tc99m-hepatobiliary iminodiacetic acid (HIDA) scintigraphy in clinical practice. Clin Radiol. 2011;66(11):1094–105.
Bushnell DL, Perlman SB, Wilson MA, Polcyn RE. The rim sign: association with acute cholecystitis. J Nucl Med. 1986;27(3):353–6.
Cawthon MA, Brown DM, Hartshorne MF, Karl Jr RD, Bauman JM, Howard 3rd WH, Bunker SR. Biliary scintigraphy. The “hot rim” sign. Clin Nucl Med. 1984;9(11):619–21.
Shuman WP, Gibbs P, Rudd TG, Mack LA. PIPIDA scintigraphy for cholecystitis: false positives in alcoholism and total parenteral nutrition. AJR Am J Roentgenol. 1982;138(1):1–5.
Larsen MJ, Klingensmith 3rd WC, Kuni CC. Radionuclide hepatobiliary imaging: nonvisualization of the gallbladder secondary to prolonged fasting. J Nucl Med. 1982;23(11):1003–5.
Flancbaum L, Choban PS, Sinha R, Jonasson O. Morphine cholescintigraphy in the evaluation of hospitalized patients with suspected acute cholecystitis. Ann Surg. 1994;220(1):25–31.
Eikman EA, Cameron JL, Colman M, Natarajan TK, Dugal P, Wagner Jr HN. A test for patency of the cystic duct in acute cholecystitis. Ann Intern Med. 1975;82(3):318–22.
Weissmann HS, Berkowitz D, Fox MS, Gliedman ML, Rosenblatt R, Sugarman LA, Freeman LM. The role of technetium-99m iminodiacetic acid (IDA) cholescintigraphy in acute acalculous cholecystitis. Radiology. 1983;146(1):177–80.
Mariat G, Mahul P, Prévôt N, De Filippis JP, Cuilleron M, Dubois F, Auboyer C. Contribution of ultrasonography and cholescintigraphy to the diagnosis of acute acalculous cholecystitis in intensive care unit patients. Intensive Care Med. 2000;26(11):1658–63.
Flum DR, Cheadle A, Prela C, Dellinger EP, Chan L. Bile duct injury during cholecystectomy and survival in medicare beneficiaries. JAMA. 2003;290(16):2168–73.
Nuzzo G, Giuliante F, Giovannini I, Ardito F, D’Acapito F, Vellone M, Murazio M, Capelli G. Bile duct injury during laparoscopic cholecystectomy: results of an Italian national survey on 56 591 cholecystectomies. Arch Surg. 2005;140(10):986–92.
Walker AT, Shapiro AW, Brooks DC, Braver JM, Tumeh SS. Bile duct disruption and biloma after laparoscopic cholecystectomy: imaging evaluation. AJR Am J Roentgenol. 1992;158(4):785–9.
Peters JH, Ollila D, Nichols KE, Gibbons GD, Davanzo MA, Miller J, Front ME, Innes JT, Ellison EC. Diagnosis and management of bile leaks following laparoscopic cholecystectomy. Surg Laparosc Endosc. 1994;4(3):163–70.
Weissmann HS, Gliedman ML, Wilk PJ, Sugarman LA, Badia J, Guglielmo K, Freeman LM. Evaluation of the postoperative patient with 99mTc-IDA cholescintigraphy. Semin Nucl Med. 1982;12(1):27–52.
Stoker J. Magnetic resonance imaging and the acute abdomen. Br J Surg. 2008;95(10):1193–4.
Tonolini M, Ravelli A, Villa C, Bianco R. Urgent MRI with MR cholangiopancreatography (MRCP) of acute cholecystitis and related complications: diagnostic role and spectrum of imaging findings. Emerg Radiol. 2012;19(4):341–8.
Oto A, Ernst RD, Ghulmiyyah LM, Nishino TK, Hughes D, Chaljub G, Saade G. MR imaging in the triage of pregnant patients with acute abdominal and pelvic pain. Abdom Imaging. 2009;34(2):243–50.
Wong HP, Chiu YL, Shiu BH, Ho LC. Preoperative MRCP to detect choledocholithiasis in acute calculous cholecystitis. J Hepatobiliary Pancreat Sci. 2012;19(4):458–64.
Altun E, Semelka RC, Elias Jr J, Braga L, Voultsinos V, Patel J, Balci NC, Woosley JT. Acute cholecystitis: MR findings and differentiation from chronic cholecystitis. Radiology. 2007;244(1):174–83.
Hakansson K, Leander P, Ekberg O, Hakansson HO. MR imaging in clinically suspected acute cholecystitis. A comparison with ultrasonography. Acta Radiol. 2000;41(4):322–8.
Oh KY, Gilfeather M, Kennedy A, Glastonbury C, Green D, Brant W, Yoon HC. Limited abdominal MRI in the evaluation of acute right upper quadrant pain. Abdom Imaging. 2003;28(5):643–51.
Regan F, Schaefer DC, Smith DP, Petronis JD, Bohlman ME, Magnuson TH. The diagnostic utility of HASTE MRI in the evaluation of acute cholecystitis. Half-Fourier acquisition single-shot turbo SE. J Comput Assist Tomogr. 1998;22(4):638–42.
Taourel P, Bret PM, Reinhold C, Barkun AN, Atri M. Anatomic variants of the biliary tree: diagnosis with MR cholangiopancreatography. Radiology. 1996;199(2):521–7.
Prabhakar PD, Prabhakar AM, Prabhakar HB, Sahani D. Magnetic resonance cholangiopancreatography of benign disorders of the biliary system. Magn Reson Imaging Clin N Am. 2010;18(3):497–514. xi.
Griffin N, Yu D, Alexander Grant L. Magnetic resonance cholangiopancreatography: pearls, pitfalls, and pathology. Semin Ultrasound CT MR. 2013;34(1):32–43.
Chan YL, Chan AC, Lam WW, Lee DW, Chung SS, Sung JJ, Cheung HS, Li AK, Metreweli C. Choledocholithiasis: comparison of MR cholangiography and endoscopic retrograde cholangiography. Radiology. 1996;200(1):85–9.
Guibaud L, Bret PM, Reinhold C, Atri M, Barkun AN. Bile duct obstruction and choledocholithiasis: diagnosis with MR cholangiography. Radiology. 1995;197(1):109–15.
Griffin N, Wastle ML, Dunn WK, Ryder SD, Beckingham IJ. Magnetic resonance cholangiopancreatography versus endoscopic retrograde cholangiopancreatography in the diagnosis of choledocholithiasis. Eur J Gastroenterol Hepatol. 2003;15(7):809–13.
Barakos JA, Ralls PW, Lapin SA, Johnson MB, Radin DR, Colletti PM, Boswell Jr WD, Halls JM. Cholelithiasis: evaluation with CT. Radiology. 1987;162(2):415–8.
Shakespear JS, Shaaban AM, Rezvani M. CT findings of acute cholecystitis and its complications. AJR Am J Roentgenol. 2010;194(6):1523–9.
Yamashita K, Jin MJ, Hirose Y, Morikawa M, Sumioka H, Itoh K, Konish J. CT finding of transient focal increased attenuation of the liver adjacent to the gallbladder in acute cholecystitis. AJR Am J Roentgenol. 1995;164(2):343–6.
An C, Park S, Ko S, Park MS, Kim MJ, Kim KW. Usefulness of the tensile gallbladder fundus sign in the diagnosis of early acute cholecystitis. AJR Am J Roentgenol. 2013;201(2):340–6.
Harvey RT, Miller Jr WT. Acute biliary disease: initial CT and follow-up US versus initial US and follow-up CT. Radiology. 1999;213(3):831–6.
Bennett GL, Rusinek H, Lisi V, Israel GM, Krinsky GA, Slywotzky CM, Megibow A. CT findings in acute gangrenous cholecystitis. AJR Am J Roentgenol. 2002;178(2):275–81.
Grayson DE, Abbott RM, Levy AD, Sherman PM. Emphysematous infections of the abdomen and pelvis: a pictorial review. Radiographics. 2002;22(3):543–61.
Revzin MV, Scoutt L, Smitaman E, Israel GM. The gallbladder: uncommon gallbladder conditions and unusual presentations of the common gallbladder pathological processes. Abdom Imaging. 2015;40(2):385–99.
Benarroch-Gampel J, Boyd CA, Sheffield KM, Townsend Jr CM, Riall TS. Overuse of CT in patients with complicated gallstone disease. J Am Coll Surg. 2011;213(4):524–30.
Livingston EH, Miller JA, Coan B, Rege RV. Costs and utilization of intraoperative cholangiography. J Gastrointest Surg. 2007;11(9):1162–7.
Orenstein SB, Marks JM, Hardacre JM. Technical aspects of bile duct evaluation and exploration. Surg Clin North Am. 2014;94(2):281–96.
Buddingh KT, Weersma RK, Savenije RA, van Dam GM, Nieuwenhuijs VB. Lower rate of major bile duct injury and increased intraoperative management of common bile duct stones after implementation of routine intraoperative cholangiography. J Am Coll Surg. 2011;213(2):267–74.
Sheffield KM, Riall TS, Han Y, Kuo YF, Townsend Jr CM, Goodwin JS. Association between cholecystectomy with vs without intraoperative cholangiography and risk of common duct injury. JAMA. 2013;310(8):812–20.
Giger U, Ouaissi M, Schmitz SF, Krahenbuhl S, Krahenbuhl L. Bile duct injury and use of cholangiography during laparoscopic cholecystectomy. Br J Surg. 2011;98(3):391–6.
Ragulin-Coyne E, Witkowski ER, Chau Z, Ng SC, Santry HP, Callery MP, Shah SA, Tseng JF. Is routine intraoperative cholangiogram necessary in the twenty-first century? A national view. J Gastrointest Surg. 2013;17(3):434–42.
Sanjay P, Mittapalli D, Marioud A, White RD, Ram R, Alijani A. Clinical outcomes of a percutaneous cholecystostomy for acute cholecystitis: a multicentre analysis. HPB (Oxford). 2013;15(7):511–6.
Simorov A, Ranade A, Parcells J, Shaligram A, Shostrom V, Boilesen E, Goede M, Oleynikov D. Emergent cholecystostomy is superior to open cholecystectomy in extremely ill patients with acalculous cholecystitis: a large multicenter outcome study. Am J Surg. 2013;206(6):935–40; discussion 940–1.
Anderson JE, Inui T, Talamini MA, Chang DC. Cholecystostomy offers no survival benefit in patients with acute acalculous cholecystitis and severe sepsis and shock. J Surg Res. 2014;190(2):517–21.
Abi-Haidar Y, Sanchez V, Williams SA, Itani KM. Revisiting percutaneous cholecystostomy for acute cholecystitis based on a 10-year experience. Arch Surg. 2012;147(5):416–22.
Chang YR, Ahn YJ, Jang JY, Kang MJ, Kwon W, Jung WH, Kim SW. Percutaneous cholecystostomy for acute cholecystitis in patients with high comorbidity and re-evaluation of treatment efficacy. Surgery. 2014;155(4):615–22.
Itoi T, Coelho-Prabhu N, Baron TH. Endoscopic gallbladder drainage for management of acute cholecystitis. Gastrointest Endosc. 2010;71(6):1038–45.
Jang JW, Lee SS, Song TJ, Hyun YS, Park do H, Seo DW, Lee SK, Kim MH, Yun SC. Endoscopic ultrasound-guided transmural and percutaneous transhepatic gallbladder drainage are comparable for acute cholecystitis. Gastroenterology. 2012;142(4):805–11.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
LaRocca, C.J., Hoskuldsson, T., Beilman, G.J. (2015). The Use of Imaging in Gallbladder Disease. In: Eachempati, S., Reed, II, R. (eds) Acute Cholecystitis. Springer, Cham. https://doi.org/10.1007/978-3-319-14824-3_4
Download citation
DOI: https://doi.org/10.1007/978-3-319-14824-3_4
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-14823-6
Online ISBN: 978-3-319-14824-3
eBook Packages: MedicineMedicine (R0)