Abstract
The concept of autoinflammation arose from the recognition of monogenic disorders with seemingly unprovoked inflammation without the high-titer autoantibodies or antigen-specific T cells seen in classic autoimmune diseases. During the first decade of the ‘autoinflammatory era’, a clear connection was established between autoinflammatory disease and the innate immune system, with targeted therapies providing a powerful affirmation of mechanistic hypotheses. Although the ‘inflammasomopathies’, which are associated with marked interleukin (IL)-1β production, were some of the earliest recognized autoinflammatory diseases, it soon became clear that autoinflammation can be caused by a variety of genetic lesions affecting a range of innate immune pathways, including nuclear factor kappa B (NF-κB) activation and type I interferon production. The advent of next-generation sequencing has resulted in the discovery of multiple new diseases, genes, and pathways, while genome-wide association studies (GWAS) have shed light on the pathogenesis of genetically complex autoinflammatory diseases, such as Behçet disease. During the next decade, the universe of autoinflammatory diseases will continue to expand, but it is likely that distinctions between clinical disease and normal variation will blur, and that treatments developed for autoinflammation will be applied to a much broader range of human illnesses.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Autoinflammation
- Innate immunity
- Inflammasome
- Interleukin (IL)-1β
- Type I interferon
- Next-generation sequencing
- Genome-wide association study (GWAS)
- Mosaicism
- Nomenclature
- Targeted therapy
- Aphthous ulcers
-
The autoinflammatory diseases were initially recognized for seemingly unprovoked inflammation, but were soon discovered to be disorders of innate immunity
-
Next-generation sequencing has led to an explosion of discovery of monogenic autoinflammatory diseases and newly recognized innate immune pathways
-
Genome-wide association studies (GWAS) provide insight into the etiology of genetically complex autoinflammatory diseases
-
In addition to continued discovery of new diseases, genes, and pathways, the next decade promises to draw connections between autoinflammatory diseases and the ‘range of normal’ phenotypes, and to apply the treatments developed for autoinflammatory diseases to a broad spectrum of illnesses
1 ‘Ancient’ History
For over a century, medical science has been fascinated with the questions of if, when, and how the immune system might turn against its host. At the beginning of the twentieth century, the Nobel Prize-winning immunologist Paul Ehrlich proposed the concept of horror autotoxicus to argue that the consequences of autoimmunity would be so dire that an organism would have multiple mechanisms in place to prevent self-reactivity from ever happening [1]. However, the subsequent decades provided ample evidence that there are in fact numerous human illnesses in which such safeguards break down, giving rise to either systemic or organ-specific autoimmunity. Self-reactive antibodies and T lymphocytes have been implicated in the pathogenesis of many of these disorders.
By the latter half of the twentieth century there remained a group of illnesses characterized by episodes of seemingly unprovoked systemic or localized inflammation, without the apparent involvement of high-titer autoantibodies or antigen-specific T lymphocytes. Astute clinicians recognized that for several of these illnesses, recurrent fevers were a prominent feature, and that they appeared to be hereditary. These included familial Mediterranean fever (FMF), familial Hibernian fever , hyperimmunoglobulinemia D with periodic fever syndrome (HIDS), Muckle-Wells syndrome (MWS), and familial cold urticaria. The advent of the Human Genome Project provided the tools to search for the underlying genes in a hypothesis-neutral, comprehensive fashion known as positional cloning , enabling the discovery of previously unknown regulators of immunity gone awry in these illnesses (see Chap. 2).
1.1 First Discoveries: The Birth of Autoinflammation
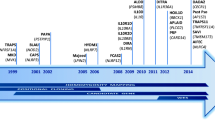
Owing both to its relatively well-defined phenotype and to the availability of the large numbers of families needed for high-resolution genetic mapping, FMF was the first of the recurrent fever syndromes to be analyzed in this way. In the summer of 1997 two independent consortia discovered recessive mutations in the causative gene, MEFV, which encodes what was then a novel protein denoted pyrin (or marenostrin) ([2, 3]; see Chap. 16). Although not known at the time, pyrin forms the nucleus of a macromolecular complex (denoted the pyrin inflammasome) that activates interleukin-(IL)1β, IL-18, and the executioner protein gasdermin D in response to certain bacterial toxins ([4, 5]; see Chap. 5). FMF-associated mutations in pyrin lower the threshold for activation. The ~90 N-terminal residues of pyrin constitute a motif that is the prototype for a cognate interaction domain (the PYRIN domain) found in some 20 immune-related human proteins. The discovery of MEFV not only fulfilled the promise of positional cloning, but also allowed the unequivocal determination that certain other periodic fever syndromes were not FMF, thus opening up a new area of clinical investigation. In 1999, mutations in TNFRSF1A, encoding the 55 kDa tumor necrosis factor receptor, were shown to define a recurrent fever syndrome now called the tumor necrosis factor (TNF) receptor-associated periodic syndrome (TRAPS), which subsumed familial Hibernian fever and several other dominantly-inherited fever syndromes seen in multiple ethnicities ([6]; see Chap. 18).
The authors of the paper describing TRAPS proposed the term ‘autoinflammatory’ to denote what appeared to be an emerging family of illnesses characterized by seemingly unprovoked systemic or localized inflammation, but without the cardinal features of autoimmunity. A year later the concept was refined and extended, with the proposal of a classification scheme that included the recurrent fever syndromes, certain complement disorders (such as hereditary angioedema), familial urticarial syndromes (familial cold urticaria, MWS—see Chap. 19), granulomatous disorders (Blau syndrome—see Chap. 20), metabolic disorders (crystalline arthropathies—see Chap. 34), storage diseases (Gaucher disease, Hermansky-Pudlak syndrome), fibrosing disorders, and Behçet disease ([7]; see Chap. 35). Recognizing the heterogeneity of human disease, this analysis included both monogenic and genetically complex illnesses. However, at this early stage the schema was based solely on the whimsical notion of a family of diseases manifesting unprovoked inflammation without high-titer autoantibodies or antigen-specific T cells, in the absence of more detailed genetic or functional insight.
2 The ‘Eureka’ Decade
During the next decade, two independent lines of investigation converged to corroborate the concept of autoinflammation. On the one hand, the field of human genetics accelerated the discovery of genes underlying the newly recognized autoinflammatory diseases. On the other hand, advances in basic immunology firmly established the role of the innate immune system in host defense [8]. Whereas the adaptive immune system is mediated by lymphocytes with membrane receptors encoded by genes that somatically rearrange and mutate, the evolutionarily more ancient innate immune system utilizes myeloid effector cells with both extracellular and intracellular receptors that are ‘hard-wired’ in the genome to recognize ‘pathogen-associated molecular patterns’ (see Chap. 4). Genetics and immunobiology advanced hand-in-hand, with the growing realization that many of the disorders defined clinically as ‘autoinflammatory’ are caused by genetic mutations that perturb the innate immune system. Disease-gene discoveries provided clinical relevance for innate immunity, and advances in immunology explained newly recognized autoinflammatory illnesses. Highly successful trials of therapies predicted to target the relevant pathways were the heady affirmation of an emerging understanding of a new field of medicine ([9,10,11]; see Chaps. 41 and 42).
Nowhere was this paradigm more evident than in the elucidation of the cryopyrin-associated periodic syndromes (CAPS). In 2001 Hal Hoffman and his colleagues discovered dominantly-inherited mutations in the gene encoding a PYRIN domain-containing protein (denoted cryopyrin) as the cause of both familial cold autoinflammatory syndrome (formerly familial cold urticaria) and MWS ([12]; see Chap. 19). Within a year, two other groups discovered mutations in the same gene as the cause of neonatal-onset multisystem inflammatory disorder (NOMID; also called (mainly in Europe) chronic infantile neurologic cutaneous and articular [CINCA] syndrome) , a devastating disorder manifesting chronic aseptic meningitis [13, 14]. All of these diseases are collectively denoted CAPS. Independently and nearly simultaneously, other groups discovered a role for cryopyrin (alternatively termed ‘PYPAF1,’ ‘NALP3,’ and now ‘NLRP3’) in the activation of IL-1β [15, 16]. The late Jürg Tschopp and his colleagues proposed a macromolecular complex they termed the inflammasome, one variant of which includes nucleotide-binding domain, leucine-rich repeat (NLR) family, pyrin domain containing 3 (NLRP3), that leads to the autocatalysis of caspase-1 and the release of biologically active IL-1β from leukocytes ([17]; see Chap. 5). CAPS-associated mutations were soon found to cause constitutive activation of the NLRP3 inflammasome, thus suggesting a possible role for IL-1 inhibition in the treatment of CAPS. The life-altering effects of IL-1 inhibition in CAPS have been a triumph of molecular medicine and a true vindication of the importance of IL-1 in human immunobiology [9,10,11].
2.1 Expanding the Discovery of Diseases Caused by Genetic Mutations
The early years of the ‘autoinflammatory era’ witnessed the discovery of several new disease-causing genes (Table 1.1), the deepening of our understanding of innate immune pathways, and further therapeutic advances. Given the genomic technologies of the time, the new disease gene discoveries were the result of either positional cloning or candidate gene approaches, sometimes suggesting extensions of known innate immune pathways (see Chap. 2). For example, the discovery of loss-of-function mutations in IL1RN, encoding the endogenous IL-1 receptor antagonist (a recombinant form of which is anakinra, a biologic used in the treatment of CAPS), causing the disease deficiency of IL-1 receptor antagonist (DIRA), highlighted the need for tight IL-1 regulation in normal homeostasis ([18, 19]; see Chap. 25). The discovery of dominantly inherited mutations in PSTPIP1, which encodes a pyrin-binding protein also involved in regulating the cytoskeleton, in pyogenic arthritis, pyoderma gangrenosum and acne (PAPA) syndrome [20, 21], suggested a connection between innate immunity and the cytoskeleton that is still under active investigation (see Chap. 22). The discovery of autoinflammatory phenotypes associated with CARD15/NOD2 (see Chap. 20) and NLRP12 (see Chap. 29) expanded the spectrum of disorders associated with this large family of NACHT-domain-containing proteins, raising the possibility of even more [22,23,24]. The discovery of mevalonate kinase (MVK) mutations in HIDS [25, 26], now called mevalonate kinase deficiency (MKD) due to this discovery, established a link between metabolism and autoinflammation that has only recently been explained.
2.2 Early Thoughts on Pathophysiologic Mechanisms
During this first decade, many of the advances in disease mechanism and treatment centered on IL-1β and related proteins, leading some to suggest an equivalence of autoinflammation with IL-1-mediated disease (see Chaps. 5 and 10). Evidence emerged that the prototypic autoinflammatory disease, FMF, is driven by IL-1β [27], and that uric acid crystals activate the NLRP3 inflammasome, thus supporting the hypothesis that gout, a genetically complex disorder, is also autoinflammatory and driven by IL-1β ([28]; see Chap. 34). Nevertheless, even during this early era there was mounting evidence for other molecular mechanisms, such as nuclear factor kappa B (NF-κB) activation in Blau syndrome ([29]; see Chap. 20). This is not surprising, given the broad scope of innate immune sensing and signaling. As was noted a decade ago, the autoinflammatory diseases are a sampling from the universe of natural variation in the innate immune system that is severe enough to cause illness, but not so severe to be embryonic lethal [30]. The ensuing decade has given us a glimpse of just how diverse a universe this is.
3 Horror Autoinflammaticus: The Golden Age of Autoinflammation
The second decade of the autoinflammatory era began in 2009 with the publication of ‘Horror Autoinflammaticus: The Molecular Pathophysiology of Autoinflammatory Disease,’ a comprehensive review of the field that proposed a classification scheme based on molecular insights garnered to that point ([30]; see Chap. 10). Autoinflammation had come of age. Building on this foundation, the last decade has witnessed a genomic explosion, catalyzed in large part by a revolution in next-generation sequencing technology that has led to drastic reductions in costs and a concomitant boom in the availability of whole-exome and now whole-genome sequencing (see Chap. 2). The number of monogenic autoinflammatory diseases has gone up dramatically, shedding light on new innate immune pathways and disease mechanisms. While the cases have become ever rarer, they are ‘experiments of nature’ by which, as Sir William Harvey noted four centuries ago, “Nature is nowhere [more] accustomed to display her secret mysteries than in cases where she shows traces of her workings apart from the beaten path” [31].
3.1 New Discoveries of Rare Mongenic Autoinflammatory Diseases
Some of the newly recognized disease-causing genes encode known innate immune sensors for which a monogenic human disease had not already been discovered. NLRC4 encodes the lynchpin of an inflammasome that senses bacterial flagellin; gain-of-function mutations have now been shown to cause colitis, a CAPS-like spectrum, and an increased risk of macrophage activation syndrome (MAS) ([32, 33]; see Chap. 29). NLRP1 encodes a protein that nucleates the main inflammasome in the skin; activating mutations were shown to cause dyskeratosis with or without arthritis ([34, 35]; see Chap. 29). TMEM173 encodes the stimulator of interferon genes (STING), a major sensor of intracellular double-stranded DNA; de novo gain-of-function mutations are now known to cause vasculopathy, peripheral gangrene, and interstitial fibrosis (STING-associated vasculopathy with onset in infancy, SAVI) ([36]; see Chap. 24). MEFV encodes pyrin, the protein mutated in FMF; mutations in a critical phosphorylation site have been shown to cause a dominantly-inherited chronic neutrophilic dermatosis termed pyrin-associated autoinflammation with neutrophilic dermatosis (PAAND) ([37]; see Chap. 29).
In other cases, next-generation sequencing has led to the identification of genes defining entirely new mechanisms of innate immune regulation. WDR1 encodes a protein that regulates the actin cytoskeleton; loss-of-function mutations lead to activation of the pyrin inflammasome and increased IL-18 production ([38]; see Chap. 28). ADA2 (formerly CECR1) encodes what is thought to be a growth factor expressed in myeloid cells; loss-of-function mutations cause recurrent fevers, early-onset strokes, vasculopathy, and sometimes bone marrow failure and immunodeficiency ([39, 40]; see Chap. 23). PSMB8 encodes a component of the immunoproteasome that degrades K48-ubiquitinated proteins; biallelic loss-of-function mutations cause a syndrome of fevers, panniculitis, and lipodystrophy ([41,42,43,44]; see Chap. 24). TNFAIP3, OTULIN, HOIL-1, and HOIP encode proteins that regulate ubiquitination, a major form of post-translational protein modification. Haploinsufficiency of TNFAIP3 or biallelic loss-of-function mutations at the other three loci cause a spectrum of autoinflammatory phenotypes ([45,46,47,48]; see Chap. 29). PLCG2 encodes a signaling molecule expressed in hematopoietic cells; heterozygous gain-of-function missense mutations cause an autoinflammatory syndrome of rash, ocular inflammation, mild immunodeficiency, and interstitial lung disease ([49]; see Chap. 28). ADGRE2 encodes a membrane mechanosensor expressed on mast cells; heterozygous loss-of-function mutations in an autoinhibitory domain cause vibratory urticaria [50]. LACC1 encodes a key regulator of metabolism in macrophages; biallelic loss-of-function mutations cause a monogenic form of systemic juvenile idiopathic arthritis ([51]; see Chap. 32). Perhaps most surprising of all, TRNT1 encodes a ubiquitously expressed enzyme that adds the 3-nt CCA sequence to the 3′ ends of all tRNA molecules. Biallelic hypomorphic mutations cause an autoinflammatory syndrome denoted sideroblastic anemia with immunodeficiency , fevers, and developmental delay (SIFD) ([52]; see Chap. 28).
3.2 Expanded Understanding of Disease Pathophysiology Related to the Innate Immune System and Novel Genetic Mechanisms
Over the last decade there have also been substantial advances in our understanding of the biology of innate immunity and in targeted therapies, although, not surprisingly, these have not kept pace with new disease gene discoveries. It is no secret that the timeline for functional and mechanistic analysis is much slower than for monogenic disease gene discovery, especially in the world of next-generation sequencing and large clinics dedicated to undiagnosed autoinflammatory patients. As a case in point, it took almost 20 years to understand the role of pyrin in the sensing of bacterial toxins that inactivate RhoA and the pathway by which the pyrin inflammasome is activated [4, 53]. It took an even longer time to discover gasdermin D and its role in IL-1β release from leukocytes [54,55,56]. Nevertheless, the advances of the last decade have made it abundantly clear that, notwithstanding the great importance of IL-1 in human biology, there is much more to autoinflammation than this cytokine. For example, the type I interferons play a central role in the pathogenesis of several autoinflammatory diseases, such as SAVI and PRAAS [36, 57], and targeted therapies with JAK inhibitors show great promise in a number of these disorders ([58]; see Chap. 24).
The last decade has witnessed not only a dizzying expansion in the quantity of monogenic diseases and innate immune pathways, but new qualitative insights into broader mechanisms of human disease, driven by the study of autoinflammation. Of extraordinary potential impact is the careful documentation of somatic mosaicism (see Chaps. 2 and 12) not only in infantile-onset forms of NOMID/CINCA [59] but also in adult-onset CAPS and Schnitzler syndrome ([60, 61]; see Chap. 37). We simply do not know how many adult-onset cases of (nonmalignant) unexplained recurrent fever and/or autoinflammation are due to somatic mutations, but the precedent of cancer teaches us that such events are not rare. Of similar general import is the recent documentation of digenic inheritance (see Chap. 12) in the proteasome-associated autoinflammatory syndromes (PRAAS) [57]. Consideration of the multi-molecular proteasome complex gave rise to the hypothesis of digenic inheritance in unexplained cases of PRAAS, but it is eminently possible that similar gene-gene interactions are operative in other multistep pathways, offering potential explanations for unsolved cases (see Chap. 24). Finally, and not surprisingly, with the discovery of ever more genes underlying monogenic autoinflammation, there are now an increasing number of cases in which there is an overlap among autoinflammation, autoimmunity, and immunodeficiency ([47, 48]; see Chaps. 28 and 38). In the case of the ubiquitination disorders, this has been shown to be due to the differential effects of regulatory events in multiple cell types. It would be absurd to believe that such overlaps would not be found.
3.3 Expansion of Autoinflammation to Non-monogenic and Common Diseases
Nearly since the outset, it has been clear that not all of the illnesses that fit under the autoinflammatory rubric are monogenic . As noted above, some are now known to exhibit a digenic mode of inheritance, but still others are genetically complex. The latter include Behçet disease (see Chap. 35), systemic juvenile idiopathic arthritis, adult-onset Still disease (see Chap. 32), chronic non-bacterial osteomyelitis (CNO), previously called chronic recurrent multifocal osteomyelitis (CRMO) (see Chap. 31), the syndrome of periodic fever with aphthous stomatitis, pharyngitis, and cervical adenitis (PFAPA) (see Chap. 30), the crystalline arthropathies (see Chap. 34), sarcoidosis, fibrosing diseases, and, by some definitions, atherosclerosis, type 2 diabetes, cancer, and neurodegenerative diseases (see Chap. 39). Probably the best-studied is Behçet disease, which presents with the classic triad of painful oral ulcers, ocular inflammation, and genital ulcers. Advances in genotyping chips have begun to shape our understanding of genetically complex autoinflammatory diseases. Through the careful collection of well-phenotyped patients and ethnically-matched controls, combined with genome-wide association studies (GWAS) and targeted deep-resequencing, a total of 17 susceptibility loci for Behçet disease have been identified: HLA-B*51, ERAP1, IL10, IL23R, STAT4, CCR1-CCR3, KLRC4, CEBPB-PTPN1, ADO-EGR2, IRF8, RIPK2, LACC1, FUT2, IL12A, MEFV-p.Met694Val, IL1A-IL1B, and TNFAIP3 [62,63,64,65,66]. Although it often has been observed that most GWAS ‘hits’ confer relatively little risk to disease susceptibility in any given individual, there nevertheless is a remarkable convergence among GWAS studies in immune diseases, suggesting commonalities in pathogenesis among disorders, and the possibility of targeted therapies. GWAS studies of Behçet disease indicate a role for adaptive immunity (given the remarkable epistasis between HLA-B*51 and ERAP1), shared pathogenesis with spondyloarthropathies and certain infectious diseases, and the possibility of therapies targeting the IL-23 axis (see Chap. 38). As noted below, GWAS also draws a shocking but totally logical connection between Behçet disease and everyday life.
4 Nomenclature of the Autoinflammatory Diseases
As a consequence of the burgeoning list of autoinflammatory diseases , there are now vigorous discussions about nomenclature and nosology. Since language is very much a matter of convention, it would be presumptuous for one individual to impose any specific naming scheme. In any area of discourse, history matters, and thus it would be difficult to advocate against terms like ‘familial Mediterranean fever,’ regardless of whether all cases are familial, or Mediterranean, or exhibit fever, simply because FMF is thoroughly entrenched in our lexicon. For similar reasons, it is sometimes difficult to dislodge firmly established eponyms. Nevertheless, going forward I do subscribe to the view that eponyms should be avoided, so as not to torment our junior colleagues with a litany of people who didn’t actually have the diseases attached to their names. Instead, I favor disease names and classification schemes that reflect the underlying biology, whether that is best reflected in a gene name or the name of its encoded protein – or even a pathway (‘inflammasomopathy,’ ‘interferonopathy’)—rather than a string of clinical manifestations that spell out a memorable acronym. Just as we classify and name infectious diseases by their causative microorganisms, so too should we classify and name autoinflammatory diseases according to their underlying etiology. Such a schema shapes our thinking, stimulates hypotheses, and suggests targeted therapies. As noted above, as we learn more there will be an inevitable blurring of the boundaries between autoinflammatory and autoimmune or immunodeficiency (see Chaps. 28 and 38). That is simply the nature of nature, and any useful schema will need to deal with it. The responsibility for establishing naming conventions should rest with the community that uses them most. In this particular case, that is probably the International Society for Systemic Autoinflammatory Diseases (ISSAID) or its designees.
5 Quō vādis? Autoinflammation and the Human Condition
The third decade of the autoinflammatory era will begin auspiciously with the publication of this, the first medical text on autoinflammation. Anticipating what is in store for this next decade, it is fitting to recall the observation of the twentieth century American ‘philosopher’, the baseball player Yogi Berra: “It’s tough to make predictions, especially about the future.” Nevertheless, the developments of the last 10 years likely foreshadow the next ten, and so it would be reasonably safe to predict more disease genes, more pathways, more biology, and more targeted therapies. There has been no evidence that we are approaching an asymptote in new discoveries in this arena, and it is likely that as we peel the onion we will be greeted with successive layers of regulatory complexity. There is nothing wrong in prognosticating ‘more of the same’ for the next decade. And it would be grand.
However, two recent advances augur additional more profound tectonic shifts. The first is an abstract presented by the direct-to-consumer genomic testing company 23andMe at the 2017 annual meeting of the American Society of Human Genetics [67]. This abstract presented a GWAS of canker sores/aphthous ulcers in 178,409 affected individuals and 66,609 controls. Individuals were scored as affected through their response to a questionnaire (“Have you ever had a canker sore [an open sore on the soft tissue inside the mouth]? Yes/No/Not sure”). There was no medical or dental examination, no review of medical records. Remarkably, 47 loci reached genome-wide significance, including 8 loci known to be associated with Behçet disease (IL10, STAT4, CCR3, IL12A, RIPK2, NOD2, IRF8, CEBPB). Whereas the 23andMe study had very large numbers of subjects but little opportunity for clinical observation, the studies of Behçet disease were roughly 100 times smaller, but relied on meticulous phenotyping. The fact that there was significant overlap between the two studies suggests that, at least for some phenotypes, a yes-no questionnaire applied to many subjects may reach the same conclusions as a careful clinical study of a much smaller number of subjects. The overlap between the two GWAS studies also suggests that some of the same loci that confer susceptibility to severe diseases may also confer susceptibility to more common, ‘every day’ problems like canker sores. It is tempting to speculate that the loci that were not in common between the two studies (such as HLA-B*51, ERAP1, and IL23R), determine who gets Behçet disease rather than simple canker sores. It is also possible that other disorders manifesting with oral ulcers may share some of these susceptibility loci, and that the knowledge of these loci will eventually lead to targeted therapies for aphthae.
With the increasing dissemination of genomic sequencing and genotyping across the population, and the advent of large cohort studies such as the All of Us Research Program, it will be increasingly possible to connect genes and loci associated with autoinflammatory diseases with phenotypes that we would consider in the range of normal experience. While the experience to date with targeted therapies for rare autoinflammatory diseases could certainly be considered to be personalized or precision medicine, the more universal approach will take the field to an entirely new level.
A second advance was the publication, in August 2017, of two papers summarizing the initial results of a randomized, double-blind, placebo-controlled trial of canakinumab (a human monoclonal anti-IL-1β antibody) in 10,061 subjects with a previous myocardial infarction and an elevated C-reactive protein level of 2 mg or more per liter. In a paper published in the New England Journal of Medicine, canakinumab at a dose of 150 mg given every 3 months significantly lowered the rate of recurrent cardiovascular events, relative to placebo, regardless of lipid-level lowering ([68]; see Chap. 39). The same research group simultaneously published a paper in The Lancet demonstrating reductions in lung cancer and total cancer mortality among subjects treated with canakinumab in the same clinical protocol ([69]; see Chap. 39). Together, these papers suggest an important role for inflammation in both cardiovascular disease and cancer, and the possibility of therapies targeting innate immunity in preventing or treating these common illnesses.
These two advances promise a much greater role for autoinflammation in the general human condition. Not only will the boundaries blur between autoinflammation and autoimmunity or immunodeficiency, but the boundaries between health and disease will also blur.
6 Questions for the Next Decade
There also remain a number of questions for the field to address in the next decade. Ten of those I consider of primary importance are listed below:
-
1.
What accounts for the intermittent nature of many of the autoinflammatory diseases?
-
2.
What is the molecular basis of phenotypic heterogeneity among individuals with the same or similar genotypes?
-
3.
What is the penetrance of monogenic autoinflammatory variants in the general population?
-
4.
To what extent does somatic mutation explain late-onset autoinflammatory disease (see Chaps. 2 and 12)?
-
5.
What is the role of the microbiome in autoinflammatory disease?
-
6.
To what extent do epigenetic factors (see Chap. 3) influence the course of monogenic and genetically complex autoinflammatory disorders?
-
7.
How do the various inflammasomes differ in their processing of IL-1β, IL-18, and gasdermin D, and how do these differences correlate with disease phenotype (see Chaps. 5 and 6)?
-
8.
To what extent do monogenic diseases inform our understanding of genetically complex autoinflammatory diseases (see Chap. 38)?
-
9.
How will disease discovery evolve with new technologies, such as whole genome sequencing (see Chap. 2) and metabolomics?
-
10.
What will be the relative roles of biologics, small molecules, and bone marrow transplantation in the therapy of these illnesses (see Chap. 42)?
It is an exciting time to be working in the field of autoinflammation. This textbook offers a multidisciplinary approach to a maturing discipline that truly transcends the arenas of internal medicine, pediatrics, genetics and genomics, clinical and basic immunology, and cell biology, and I expect that practitioners and trainees from all of these fields will derive great benefit from its comprehensive and systematic approach. I hope that you, too, will find yourself as captivated as I am, and that this text will be your passport to an exhilarating journey in autoinflammation.
Dan Kastner, MD, PhD
Bethesda, Maryland
July 1, 2018
Abbreviations
- CAPS:
-
Cryopyrin-associated periodic syndromes
- CINCA:
-
Chronic infantile neurologic cutaneous and articular syndrome
- CNO:
-
Chronic non-bacterial osteomyelitis
- CRMO:
-
Chronic recurrent multifocal osteomyelitis
- DIRA:
-
Deficiency of interleukin-1 receptor antagonist
- FMF:
-
Familial Mediterranean fever
- GWAS:
-
Genome-wide association studies
- HIDS:
-
Hyperimmunoglobulinemia D with periodic fever syndrome
- IL:
-
Interleukin
- ISSAID:
-
International Society for Systemic Autoinflammatory Diseases
- MKD:
-
Mevalonate kinase deficiency
- MWS:
-
Muckle-Wells syndrome
- NF-κB:
-
Nuclear factor kappa B
- NLR:
-
Nucleotide-binding domain, leucine-rich repeat
- NLRP3:
-
NLR family, pyrin domain containing 3
- NOMID:
-
Neonatal-onset multisystem inflammatory disorder
- PAAND:
-
Pyrin-associated autoinflammation with neutrophilic dermatosis
- PAPA:
-
Pyogenic arthritis, pyoderma gangrenosum and acne
- PFAPA:
-
Periodic fever, aphthous stomatitis, pharyngitis, cervical adenitis
- SAVI:
-
STING-associated vasculopathy with onset in infancy
- SIFD :
-
Sideroblastic anemia with immunodeficiency, fevers, and developmental delay
- STING:
-
Stimulator of interferon genes
- TNF:
-
Tumor necrosis factor
- TRAPS:
-
TNF receptor-associated periodic syndrome
References
Silverstein AM. Autoimmunity versus horror autotoxicus: the struggle for recognition. Nat Immunol. 2001;2:279–81.
International FMF Consortium. Ancient missense mutations in a new member of the RoRet gene family are likely to cause familial Mediterranean fever. Cell. 1997;90:797–807.
French FMF Consortium. A candidate gene for familial Mediterranean fever. Nat Genet. 1997;17:25–31.
Park YH, Wood G, Kastner DL, Chae JJ. Pyrin inflammasome activation and RhoA signaling in the autoinflammatory disease FMF and HIDS. Nat Immunol. 2016;17:914–21.
Manthiram K, Zhou Q, Aksentijevich I, Kastner DL. The monogenic autoinflammatory diseases define new pathways in human innate immunity and inflammation. Nat Immunol. 2017;18:832–42.
McDermott MF, Aksenitijevich I, Galon J, et al. Germline mutations in the extracellular domains of the 55 kDA TNF receptor, TNFR1, define a family of dominantly inherited autoinflammatory syndromes. Cell. 1999;97:133–44.
Galon J, Aksentijevich I, McDermott MF, O’Shea JJ, Kastner DL. TNFRSF1A mutations and autoinflammatory syndromes. Curr Opin Immunol. 2000;12:479–86.
Medzhitov R, Janeway C Jr. Innate immunity. N Engl J Med. 2000;343:338–44.
Hoffman HM, Rosengren S, Boyle DL, et al. Prevention of cold-associated acute inflammation in familial cold autoinflammatory syndrome by interleukin-1 receptor antagonist. Lancet. 2004;364:1779–85.
Goldbach-Mansky R, Dailey NJ, Canna SW, et al. Neonatal-onset multisystem inflammatory disease responsive to interleukin-1β inhibition. N Engl J Med. 2006;355:581–92.
Lachmann HJ, Kone-Paut I, Kuemmerle-Deschner JB, et al. Use of canakinumab in the cryopyrin-associated periodic syndrome. N Engl J Med. 2009;360:2416–25.
Hoffman HM, Mueller JL, Broide DH, Wandere AA, Koldner RD. Mutation of a new gene encoding a putative pyrin-like protein causes familial cold autoinflammatory syndrome and Muckle-Wells syndrome. Nat Genet. 2001;29:301–5.
Feldmann J, Prieur AM, Quartier P, et al. Chronic infantile neurological cutaneous and articular syndrome is caused by mutations in CIAS1, a gene highly expressed in polymorphonuclear cells and chondrocytes. Am J Hum Genet. 2002;71:198–203.
Aksentijevich I, Nowak M, Mallah M, et al. De novo CIAS1 mutations, cytokine activation, and evidence for genetic heterogeneity in patients with neonatal-onset multisystem inflammatory disease (NOMID): a new member of the expanding family of pyrin-associated autoinflammatory diseases. Arthritis Rheum. 2002;46:3340–8.
Wang L, Manji GA, Grenier JM, et al. PYPAF7, a novel PYRIN-containing Apaf1-like protein that regulates activation of NF-kappa B and caspase-1-dependent cytokine processing. J Biol Chem. 2002;277:29874–80.
Agostini L, Martinon F, Burns K, McDermott MF, Hawkins PN, Tschopp J. NALP3 forms an IL-1β-processing inflammasome with increased activity in Muckle-Wells autoinflammatory disorder. Immunity. 2004;20:319–25.
Tschopp J, Martinon F, Burns K. NALPS: a novel protein family involved in inflammation. Nat Rev Mol Cell Biol. 2003;4:95–104.
Aksentijevich I, Masters SL, Ferguson PJ, et al. An autoinflammatory disease with deficiency of the interleukin-1-receptor antagonist. N Engl J Med. 2009;360:2426–37.
Reddy S, Jia S, Geoffrey R, et al. An autoinflammatory disease due to homozygous deletion of the IL1RN locus. N Engl J Med. 2009;360:2438–44.
Wise CA, Gillum JD, Seidman CE, et al. Mutations in CD2BP1 disrupt binding to PTP PEST and are responsible for PAPA syndrome, an autoinflammatory disorder. Hum Mol Genet. 2002;11:961–9.
Shoham NG, Genola M, Mansfield E, et al. Pyrin binds the PSTPIP1/CD2BP1 protein, defining familial Mediterranean fever and PAPA syndrome as disorders in the same pathway. Proc Natl Acad Sci U S A. 2003;100:13501–6.
Hugot JP, Chamaillard M, Zouali H, et al. Association of NOD2 leucine-rich repeat variants with susceptibility to Crohn’s disease. Nature. 2001;411:599–603.
Miceli-Richard C, Lesage S, Rybojad M, et al. CARD15 mutations in Blau syndrome. Nat Genet. 2001;29:19–20.
Jeru I, Duquesnoy P, Fernandes-Alnemri T, et al. Mutations in NALP12 cause hereditary periodic fever syndromes. Proc Natl Acad Sci U S A. 2008;105:1614–9.
Houten SM, Kulis W, Duran M, et al. Mutations in MVK, encoding mevalonate kinase, cause hyperimmunoglobulinaemia D and periodic fever syndrome. Nat Genet. 1999;22:175–7.
Drenth JPH, Cuisset L, Grateau G, et al. Mutations in the gene encoding mevalonate kinase cause hyper-IgD and periodic fever syndrome. Nat Genet. 1999;22:178–81.
Chae JJ, Komarow HD, Cheng J, et al. Targeted disruption of pyrin, the FMF protein, causes heightened sensitivity to endotoxin and a defect in macrophage apoptosis. Mol Cell. 2003;11:591–604.
Martinon F, Pétrilli V, Mayor A, Tardivel A, Tschopp J. Gout-associated uric acid crystals activate the NALP3 inflammasome. Nature. 2006;440:237–41.
Kanazawa N, Okafuji I, Kambe N, et al. Early-onset sarcoidosis and CARD15 mutations with constitutive nuclear factor-κB activation: common genetic etiology with Blau syndrome. Blood. 2005;105:1195–7.
Masters SL, Simon A, Aksentijevich I, Kastner DL. Horror Autoinflammaticus: the molecular pathophysiology of autoinflammatory disease. Annu Rev Immunol. 2009;27:621–68.
Szentivanyi A, Friedman H. The immunologic revolution: facts and witnesses. Boca Raton: CRC Press; 1993. p. 107.
Romberg N, Al Moussawi K, Nelson-Williams C, et al. Mutation of NLRC4 causes a syndrome of enterocolitis and autoinflammation. Nat Genet. 2014;46:1135–9.
Canna SW, de Jesus AA, Gouni S, et al. An activating NLRC4 inflammasome mutation causes autoinflammation with recurrent macrophage activation syndrome. Nat Genet. 2014;46:1140–6.
Zhong FL, Mamai O, Sborgi L, et al. Germline NLRP1 mutations cause skin inflammatory and cancer susceptibility syndromes via inflammasome activation. Cell. 2016;167:187–202.
Grandemange S, Sanchez E, Louis-Plence P, et al. A new autoinflammatory and autoimmune syndrome associated with NLRP1 mutations: NAIAD (NLRP1-assocaited autoinflammation with arthritis and dyskeratosis). Ann Rheum Dis. 2017;76:1191–8.
Liu Y, Jesus AA, Marrero B, et al. Activated STING in a vascular and pulmonary syndrome. N Engl J Med. 2014;371:507–18.
Masters SL, Lagou V, Jéru I, et al. Familial autoinflammation with neutrophilic dermatosis reveals a regulatory mechanism of pyrin activation. Sci Transl Med. 2016;8:332ra45.
Standing AS, Malinova D, Hong Y, et al. Autoinflammatory periodic fever, immunodeficiency, and thrombocytopenia (PFIT) caused by mutation in actin-regulatory gene WDR1. J Exp Med. 2017;214:59–71.
Zhou Q, Yang D, Ombrello AK, et al. Early-onset stroke and vasculopathy associated with mutations in ADA2. N Engl J Med. 2014;370:911–20.
Navon Elkan P, Pierce SB, Segel R, et al. Mutant adenosine deaminase 2 in a polyarteritis nodosa vasculopathy. N Engl J Med. 2014;370:921–31.
Agarwal AK, Xing C, DeMartino GN, et al. PSMB8 encoding the β5i proteasome subunit is mutated in joint contractures, muscle atrophy, microcytic anemia, and panniculitis-induced lipodystrophy syndrome. Am J Hum Genet. 2010;87:866–72.
Arima K, Kinoshita A, Mishima H, et al. Proteasome assembly defect due to a proteasome subunit beta type 8 (PSMB8) mutation causes the autoinflammatory disorder, Nakajo-Nishimura syndrome. Proc Natl Acad Sci U S A. 2011;108:14914–9.
Kitamura A, Maekawa Y, Uehara H, et al. A mutation in the immunoproteasome subunit PSMB8 causes autoinflammation and lipodystrophy in humans. J Clin Invest. 2011;121:4150–60.
Liu Y, Ramot Y, Torrelo A, et al. Mutations in proteasome subunit β type 8 cause chronic atypical neutrophilic dermatosis with lipodystrophy and elevated temperature with evidence of genetic and phenotypic heterogeneity. Arthritis Rheum. 2012;64:895–907.
Zhou Q, Wang H, Schwartz DM, et al. Loss-of-function mutations in TNFAIP3 leading to A20 haploinsufficiency cause an early-onset autoinflammatory disease. Nat Genet. 2016;48:67–73.
Zhou Q, Yu X, Demirkaya E, et al. Biallelic hypomorphic mutations in a linear deubiquitinase define otulipenia, an early-onset autoinflammatory disease. Proc Natl Acad Sci U S A. 2016;113:10127–32.
Boisson B, Laplantine E, Prando C, et al. Immunodeficiency, autoinflammation and amylopectinosis in humans with inherited HOIL-1 and LUBAC deficiency. Nat Immunol. 2012;13:1178–86.
Boisson B, Laplantine E, Dobbs K, et al. Human HOIP and LUBAC deficiency underlies autoinflammation, immunodeficiency, amylopectinosis, and lymphangiectasia. J Exp Med. 2015;212:939–51.
Zhou Q, Lee G-S, Brady J, et al. A hypermorphic missense mutation in PLCG2, encoding phospholipase Cy2, causes a dominantly inherited autoinflammatory disease with immunodeficiency. Am J Hum Genet. 2012;91:713–20.
Boyden SE, Desai A, Cruse G, et al. Vibratory urticaria associated with a missense variant in ADGRE2. N Engl J Med. 2016;374:656–63.
Wakil SM, Monies DM, Aboulhoda M, et al. Association of a mutation in LACC1 with a monogenic form of systemic juvenile idiopathic arthritis. Arthritis Rheumatol. 2015;67:288–95.
Giannelou A, Wang H, Zhou Q, et al. Aberrant tRNA processing causes an autoinflammatory syndrome responsive to TNF inhibitors. Ann Rheum Dis. 2018;77:612–9.
Xu H, Yang J, Gao W, et al. Innate immune sensing of bacterial modifications of Rho GTPases by the pyrin inflammasome. Nature. 2014;513:237–41.
Shi J, Zhao Y, Wang K, et al. Cleavage of GSDMD by inflammatory caspases determines pyroptotic cell death. Nature. 2015;526:660–5.
Kayagaki N, Stowe IB, Lee BL, et al. Caspase-11 cleaves gasdermin D for non-canonical inflammasome signaling. Nature. 2015;526:666–71.
Liu X, Zhang Z, Ruan J, et al. Inflammasome-activated gasdermin D causes pyroptosis by forming membrane pores. Nature. 2016;535:153–8.
Brehm A, Liu Y, Sheikh A, et al. Additive loss-of-function proteasome subunit mutation in CANDLE/PRAAS patients promote type I IFN production. J Clin Invest. 2015;125:4196–211.
Sanchez GAM, Reinhardt A, Ramsey S, et al. JAK 1/2 inhibition with baricitinib in the treatment of autoinflammatory interferonopathies. J Clin Invest. 2018;128:3041–52.
Tanaka N, Izawa K, Saito MK, et al. High incidence of NLRP3 somatic mosaicism in patients with chronic infantile neurologic, cutaneous, articular syndrome: results of an International Multicenter Collaborative Study. Arthritis Rheum. 2011;63:3625–32.
Zhou Q, Aksentijevich I, Wood GM, et al. Cryopyrin-associated periodic syndrome caused by a myeloid-restricted somatic NLRP3 mutation. Arthritis Rheumatol. 2015;67:2482–6.
de Koning HD, van Gijn ME, Stoffels M, et al. Myeloid lineage-restricted somatic mosaicism of NLRP3 mutations in patients with variant Schnitzler syndrome. J Allergy Clin Immunol. 2015;135:561–4.
Remmers EF, Cosan F, Kirino Y, et al. Genome-wide association study identifies variants in the MHC class I, IL10, and IL23R-IL12RB2 regions associated with Behçet’s disease. Nat Genet. 2010;42:698–702.
Kirino Y, Bertsias G, Ishigatsubo Y, et al. Genome-wide association analysis identifies new susceptibility loci for Behçet’s disease and epistasis between HLA-B*51 and ERAP1. Nat Genet. 2013;45:202–7.
Kirino Y, Zhou Q, Ishigatsubo Y, et al. Targeted resequencing implicates the familial Mediterranean fever gene MEFV and the toll-like receptor 4 gene TLR4 in Behçet’s disease. Proc Natl Acad Sci U S A. 2013;110:8134–9.
Ombrello MJ, Kirino Y, de Bakker PIW, Gül A, Kastner DL, Remmers EF. Behçet disease-associated MHC class I residues implicate antigen binding and regulation of cell-mediated cytotoxicity. Proc Natl Acad Sci U S A. 2014;111:8867–72.
Takeuchi M, Mizuki N, Megure A, et al. Dense genotyping of immune-related loci implicates host responses to microbial exposure in Behçet’s disease susceptibility. Nat Genet. 2017;49:438–43.
Sathirapongsasuti F. GWAS of canker sores implicates Th-1 pathway and shared genetic architecture with immune-mediated disease. 23andMe, Inc. ASHG’17. https://research.23andme.com/wp-content/uploads/2018/03/Fah_Canker_Sores_ASHG17.pdf
Ridker PM, Everett BM, Thuren T, et al. Antiinflammatory therapy with canakinumab for atherosclerotic disease. N Engl J Med. 2017;377:1119–31.
Ridker PM, MacFadyen JJ, Thuren T, et al. Effect of interleukin-1β inhibition with canakinumab on incident lung cancer in patients with atherosclerosis: exploratory results from a randomized, double-blind, placebo-controlled trial. Lancet. 2017;390:1833–42.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Kastner, D.L. (2019). Autoinflammation: Past, Present, and Future. In: Hashkes, P., Laxer, R., Simon, A. (eds) Textbook of Autoinflammation. Springer, Cham. https://doi.org/10.1007/978-3-319-98605-0_1
Download citation
DOI: https://doi.org/10.1007/978-3-319-98605-0_1
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-98604-3
Online ISBN: 978-3-319-98605-0
eBook Packages: MedicineMedicine (R0)