Abstract
Children with neurodevelopmental disabilities are at increased risk for physical inactivity and obesity. Inactive or obese children are more likely to become inactive or obese adults, resulting in increased risk for developing several chronic conditions. The literature has documented a strong relationship between exercise, weight, and sleep in adults and typically developing children, but this is much less clear in children with neurodevelopmental disabilities. Understanding the impact that physical activity and weight can have on sleep disorders may help develop interventions that target modifiable behaviors to treat sleep disorders in children with neurodevelopmental disabilities.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
FormalPara Case VignetteHenry is an 11 year 6 month old boy with a history of sleep disturbance, autism spectrum disorder (ASD), mixed receptive-expressive language disorder, ADHD, and anxiety disorder. He has difficulty falling asleep and becomes anxious when he can’t fall asleep. He does not use electronics around bedtime. Generally, he falls asleep between 10 PM and 12:30 AM, although sometimes he stays up until 2 AM. He stares at the ceiling, frustrated because he can’t fall asleep. Even after falling asleep, Henry wakes in the middle of the night and has difficulty falling back to sleep. He always falls asleep in the car and also during reading class at school before midday. He has had snoring and no witnessed apneas. There is no history of parasomnias. Henry does not exercise regularly and spends most of his free time playing video games or on his tablet. His diet is very limited: he prefers fast food and convenience foods, and he won’t eat vegetables. He drinks sweetened beverages such as soda and juice daily. His most recent growth parameters are as follows:
Weight (kg) | %ile | Z score | Height (cm) | %ile | Z score | BMI | %ile | Z score |
|---|---|---|---|---|---|---|---|---|
80.1 | >99 | 2.76 | 162.5 | 98.0 | 2.16 | 30.3 | 99.0 | 2.3 |
Evidence Base
Exercise
The Physical Activity Guidelines for Americans indicate that youth should have 60 minutes of physical activity a day, most days of the week [1]. Participation in play, sports, and recreation helps build and maintain healthy bones, muscles, and joints [2]. Regular physical activity benefits youth physiologically and psychosocially, improving bone density, muscle tissue, and maintenance of body weight and also reducing depression and social isolation [3].
Studies show that children and adolescents with intellectual disabilities have lower levels of physical fitness when compared with their typical peers [4,5,6]. Others indicate that children with ASD fail to meet the recommended amount of moderate-to-vigorous physical activity [7, 8]. This decrease in activity may be due to cognitive, physical, or social limitations [9]. Weak social and communication skills can impede participation in various physical activities [4]. Parents of children with ASD report barriers to physical activity participation: their child may require too much supervision; adult coaches lack skills needed to include their child; their child has few friends; and other children exclude their child [10]. Some communities offer fitness programs specially tailored to children with special needs; however, many communities do not have the resources to offer such programing [11], while others do not have the resources to match demand. Despite efforts to improve physical activity accessibility for this population, children with disabilities have lower levels of cardiorespiratory fitness and muscular endurance, and higher rates of obesity, than their typically developing peers [12]. Must et al. emphasize the need for physical activity programs designed to meet the needs of children with neurodevelopmental disabilities [13]. Until these needs are met, children with neurodevelopmental disabilities may continue to experience decreased physical fitness measures, potentially increasing their risk of developing cardiovascular disease in the future.
Case Vignette
Henry’s parents have tried signing him up for several team sports like soccer, baseball, and lacrosse over the years, but these did not go well. Henry had a hard time grasping the rules of the game. Socially, he did not interact or fit in with his teammates and he needed more supervision than was available in order to participate in programs [14]. Over time, Henry’s parents gave up and allowed him to pursue his preferred, sedentary activities such that he does not engage in regular physical activity.
Exercise and Sleep
A strong relationship between exercise and sleep in adults has been documented. Studies show an association between self-reported exercise and better sleep in adults [15,16,17,18]. Positive effects of exercise on sleep such as shorter sleep-onset time and more total sleep time have been found in older adults with mild sleep problems [19, 20]. Wang and Youngstedt found that sleep quality in older women improved the night following an aerobic exercise session [21]. Among children, researchers have found that intense daytime physical activity might promote good sleep quality in typically developing 6–10 year olds [22]. Likewise, typically developing children who are more physically active tend to have healthier, more consistent sleep patterns than those who exercise minimally [22]. This relationship carries over to the limited information available about children with neurodevelopmental disabilities, showing that preschool children with ASD benefit from a high level of morning and afternoon physical activity with earlier sleep onset [23].
Regular physical activity has been found to reduce the risk of developing any type of sleep disorder in adult men and women [17]. Exercise training in adults can reduce the severity of obstructive sleep apnea even with minimal changes in body weight [24]. In a cross-sectional study, Peppard and Young also found decreased apneic events with increased physical activity even after adjusting for body mass index [25]. Exercise training also reduces daytime sleepiness and improves sleep efficiency in adults with obstructive sleep apnea [17].
As noted elsewhere in this book, children with ASD frequently experience sleep disruption [26]. Wachob and Lorenzi found that activity levels were significantly related to sleep patterns in children ages 9–16 with ASD: more physically active children had better sleep quality [27].
Not only can physical activity result in better sleep, but good sleep promotes better physical activity as seen from studies on sleep timing. Evans et al. found that typically developing children with obstructive sleep apnea have limited ability to perform exercise due to reduced cardiac output and oxygen consumption at peak exercise capacity independent of their weight status [28]. Also, lack of sleep impairs a person’s ability to exercise and increases the risk of exercise-induced injuries [16].
Sleep timing and circadian rhythms may also impact exercise. Typically developing children who wake up later in the day are found to be less active [29]. Similar results have been found in adults with intellectual disabilities: Mikulovic et al. found that adults with intellectual disability who woke up early are more physically active than those who wake up late and those who wake up later tend to participate in more sedentary activities throughout the day [30]. Likewise, adolescents with intellectual disabilities who wake up early were more active than those who wake up late [31].
Research has shown that children with ASD spend significantly more time in sedentary activities – particularly those involving screens such as television, movies and video games –compared to typically developing children [10, 14, 32, 33]. The American Academy of Pediatrics suggests that children less than 2 years of age not use any screen media and preschoolers 2–5 years limit screen media to less than 1 h daily [34]. Yet children with ASD have spent 62% more time watching television and more hours per day playing video games than their typically developing siblings [32]. Also, the age at which children begin their television viewing is earlier in children with ASD compared to typically developing children [33]. Furthermore, children with ASD or ADHD with access to bedroom media spend less time sleeping each night [35].
There are several potential mechanisms by which exercise can promote sleep. First, exercise reduces anxiety [36]. Anxiety is a common factor in reduced sleep among children; therefore, minimizing anxiety through exercise may result in improved sleep. Sleep usually begins when the core temperature changes and body heat loss is maximal. Regular exercise promotes an increase in body temperature. As body temperature returns to normal, the resulting downregulation is associated with sleepiness [37]. Depression reduces sleep in adults; exercise may improve sleep in adults with depression [20].
The effects of exercise on sleep in children with neurodevelopmental disabilities have not been extensively studied. Nevertheless, patients like Henry could benefit significantly from regular exercise. For example, regular daily exercise may reduce the anxiety he experiences when trying to fall asleep or by increasing his sleepiness at bedtime by promoting a reduction in core temperature. Exercise for children can include participating in physical education class, participating in dance class or sports team practice, playing at recess, and active play at home or outdoors. Henry’s family should look for opportunities to incorporate more physical activity into his daily routine. They can assign Henry active daily chores such as taking out the garbage, sweeping the kitchen floor, or walking the dog. Also, Henry can walk around the block to and from the bus stop on school days. Adding small increments of physical activity throughout Henry’s day can form healthy habits on which he can build. With time and encouragement, these small increments can grow to longer periods of physical activity.
Obesity Prevalence
The prevalence of childhood obesity, a significant public health concern, has tripled in the past three decades [38]. Data from the 2011 to 2014 National Health and Nutrition Examination Survey, a nationally representative sample, indicates that 17.0% of children in the United States are obese [38]. Data from the 2011 National Survey of Children’s Health suggest that 28.9% of children with intellectual disability between the ages 10 and 17 were obese [39]. Other literature documents that children with neurodevelopmental disabilities are disproportionately affected by obesity [40,41,42,42]. Findings from 2009 to 2010 NHANES data show no significant change in obesity prevalence since 2003–2004 [43]. In short, there has been no significant improvement in childhood obesity prevalence in the past decade.
Weight and Sleep
The relationship between weight and sleep has been an area of active study in adults and typically developing children but less so in children with neurodevelopmental disabilities. A recent review of multiple longitudinal studies with adults noted that all found an association between short sleep duration and increased weight [44]. Many studies have described a relationship between short sleep duration and obesity in youth [45,46,47,47]. Iglayreger et al. created a composite cardiometabolic risk score and found sleep duration inversely predicts cardiometabolic risk, even after controlling for physical activity, in obese adolescents [48]. However, studies with adolescents show mixed results, most likely due to variations in methodology. A recent study found an association between short sleep and adiposity for both 10-year-old boys and girls [49]; however, a longitudinal study of 9–11-year-olds found an association between short sleep and BMI only in girls [50].
Some studies indicate that the time at which a child goes to bed is a better predictor of obesity than sleep duration [28, 51, 52], and late bedtimes were associated with adiposity independent of sleep duration [52, 53]. Vanhelst et al. documented that certain patterns of sleep behavior were more closely associated with overweight and obesity in adolescents with intellectual disability. Subjects were categorized into four sleep patterns: early bed/early rise, early bed/late rise, late bed/late rise, and late bed/early rise. Subjects in either of the late-bed groups were more likely to be overweight or obese [30]. Late bedtime seems to be a unique contributor to obesity risk.
Recent research suggests a bidirectional relationship between childhood obesity and sleep dysfunction. Obesity is a risk factor for developing obstructive sleep apnea. An obese child is four to five times more likely to develop obstructive sleep apnea than a nonobese child [54]. Conversely, typically developing children with sleep-disordered breathing have increased odds of becoming overweight [55]. In addition, children are more likely to develop obesity if they sleep less than 9 h per night [56].
The Centers for Disease Control and Prevention (CDC) defines childhood obesity as those whose body mass index percentile is at or above the 95th percentile relative to children the same age and gender [57]. Henry’s growth parameters indicate that he is obese. Gradual weight loss is appropriate and should be achieved by modifying his diet and exercise habits. His parents have worked with a nutritionist in the past; but did not agree with some of the specific recommendations. For example, the nutritionist recommended that Henry eliminate all sweetened beverages from his diet and his parents felt this was unrealistic for a child. They stopped working with the nutritionist after one visit and only followed the provided recommendations for 2 weeks before returning to previous habits.
Several mechanisms may underlie the sleep-obesity association. Hunger and satiety hormones, ghrelin and leptin, are affected by sleep deprivation [58]. Ghrelin, a peptide hormone, is secreted primarily in the stomach. When the stomach is empty, ghrelin is secreted, triggering hunger and appetite. When the stomach stretches, ghrelin secretion stops, decreasing feelings of hunger. Ghrelin’s receptor, the ghrelin/growth hormone secretagogue receptor, is found in the same cells as the receptor for leptin, also a peptide hormone, which functions to inhibit hunger. Therefore, leptin levels are suppressed prior to eating and elevated after eating (Fig. 30.1). Both hormones are affected by alterations in sleep. Sleep deprivation drives leptin levels down, resulting in decreased satisfaction after eating. Lack of sleep also causes ghrelin levels to rise, resulting in increased appetite. Simply put, inadequate sleep affects an individual’s appetite regulatory system, increasing appetite and leading to overeating and weight gain. A fair amount of research examines the effects of sleep on leptin levels in children [59, 60]. When compared with children who sleep less, children who sleep more report decreased caloric intake and lower fasting leptin levels. These children also weigh less [59].
It is possible that children with neurodevelopmental disabilities increase their overall energy intake with sleep deprivation through increased total calorie consumption. Such a relationship has been found in adults [61,62,63,63]. Lack of sleep is associated with decreased physical activity resulting from fatigue and lack of energy to exercise. In addition, Golley found that typically developing children who went to bed late and woke up late ate fewer fruits, vegetables, and dairy and more “empty-calorie” snack foods independent of sleep duration [52]. In a study of Australian children with ADHD, parents reported increased sleep disturbance in children who had a higher intake of carbohydrates, fats, and sugar [64]. Long-term consumption of poorer diet quality can promote weight gain. In addition, children with neurodevelopmental disabilities often eat a less varied diet with calorie dense foods which may affect weight [65, 66]. Also, sleep deprivation is associated with a slight decrease in thermoregulation due to a reduction in core body temperature results. Over time, this slight decrease in calorie expenditure may result in weight gain.
Psychotropic medications are often used to treat children with neurodevelopmental disabilities. These medications can alter appetite, change food preferences, induce fluid retention, and change hormone production [67]. The atypical antipsychotics, in particular, are associated with weight gain, which can be substantial.
Physical activity and weight are important factors affecting sleep in children with neurodevelopmental disabilities. All three variables have reciprocal relationships, each potentially affecting the other. Henry has risk factors which attribute to his lack of sleep. He is physically active far less than the 60 daily minutes prescribed in the Physical Activity Guidelines for Americans. In addition, he is obese. Henry’s lack of sleep may in turn hamper his ability to exercise and may contribute to excess weight gain. Physical activity and weight are two important behavioral factors which are modifiable and could offer a non-pharmacologic means to treat sleep disorders in children with neurodevelopmental disabilities.
Many children with neurodevelopmental disabilities and sleep disorders stand to benefit from modifying behavior in order to achieve a healthy weight and to improve exercise habits. Childhood weight management programs aim to improve weight and physical activity and have been developed for typically developing children who are obese. However, few centers have developed weight management programs specifically for children with neurodevelopmental disabilities. A 10-week school-based program was developed for children with intellectual disabilities or autism in Australia. Evaluation of its participants indicate improvements in a 6-min walk test – a standard measure to measure endurance and walking speed – and a decrease in candy and chocolate consumption [4]. The Wake Forest School of Medicine, in conjunction with the Brenner FIT Program, provided a multidisciplinary intervention for children with obesity and found those with cognitive disabilities demonstrated greater decreases in BMI z-score when compared to their obese typically developing peers who also received the intervention [68]. Z-scores indicate the number of standard deviations from the mean value. In this case, measuring changes in z-score values can indicate shifts in BMI percentile toward the mean even without actual changes in BMI percentile. These programs utilized the unique strengths of each individual patient and family unit.
In creating a weight management program for children with neurodevelopmental disabilities, it is important to incorporate the expertise of several disciplines including specialists in nutrition, exercise, and behavior. These professionals should be experienced in working with children with neurodevelopmental disabilities in order to address their unique needs. A participant in the group may need on-the-spot modifications to any exercise or educational lesson, which an experienced professional can provide. An ideal weight management program should provide initial weekly sessions for 2–3 months [4]. This frequency of intervention provides a base for children to establish new exercise and eating habits. The exercise, nutrition, and behavior specialists coordinate sessions to build strength, endurance, and nutrition knowledge. For example, the nutrition professional may create a nutrition lesson plan that incorporates multiple learning modalities such as visual, auditory, tactile, and kinesthetic. The behavior specialist may then work with parents to help address barriers to maintaining healthy eating and exercise habits at home. Incentives such as trips to the park or a new jump rope may be used to motivate children to meet their goals. After the period of weekly sessions, group participants should be followed at regular intervals to ensure they are maintaining healthy habits. A successful program will demonstrate positive changes in endurance and strength measures as well as changes in eating habits.
Case Vignette: Recommendations and Treatment
It has been 2 years since Henry’s family took him to a nutritionist. His sleep, weight, and inactivity continue to be an issue. The sleep specialist recommended behavior modification efforts again and working with a nutritionist who specializes in weight management for children with disabilities. That initial nutrition clinic interview revealed that Henry drinks soda and juice daily. He eats no vegetables. His family relies on fast food and convenience food items often. He uses a tablet most of his time away from school, and he does not engage in regular physical activity. After assessing his diet, the nutritionist had several recommendations in mind; however, during the interview, Henry’s mother made several comments indicating she did not yet appreciate the importance of changing Henry’s eating and exercise habits. Knowing that weight loss efforts are more successful for children when parents are committed to making similar healthy lifestyle changes [70–72], the nutritionist decided to implement some motivational interviewing techniques. Motivational interviewing is a method that aims to engage intrinsic motivation within a client, in this case a parent, in order to change behavior. Motivational interviewing is a patient-centered style which guides people to explore their ambivalence about changing behavior. The nutritionist asked Henry’s mother “What do you think will happen to Henry if he does not change his eating patterns?” and also “Why do you think the sleep specialist is concerned about Henry’s weight?” After discussing responses to these questions, Henry’s mother was able to identify three key healthy changes to eating with which she agreed: (1) decrease Henry’s sweetened beverage consumption to 0.5 cup juice per day, (2) provide fruit at breakfast, and (3) have Henry eat three bites of vegetable at dinner. His mother endorsed that she believed making these changes was reasonable and could potentially be helpful for Henry.
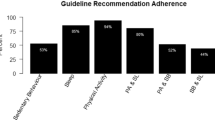
In 2015, the American Academy of Pediatrics’ most recent guidelines for treating overweight or obese children were released [72]. This publication provided comprehensive guidelines for the treatment of childhood obesity. Among the recommendations were guidelines for dietary, physical activity, and sedentary activity behavior designed to help reduce childhood obesity. Evidence supports recommendations which include the following: limiting sweetened beverage consumption; encouraging adequate consumption of fruits and vegetables; limiting screen time; eating breakfast daily; encouraging healthy choices while eating out, especially at fast-food restaurants; encouraging family meals; limiting food portion sizes; and encouraging at least 60 min of physical activity daily [72]. These recommendations do not specifically address individual needs of children with neurodevelopmental disabilities; however, it is appropriate for providers to use these target behaviors as a guide when creating treatment plans. The primary goal of obesity treatment is to improve a child’s health in the long term through establishing healthy lifestyle habits.
Target behaviors for patients and families to adopt to prevent excessive weight gain [73] |
|---|
Encourage consumption of diets with recommended quantities of fruits and vegetables |
Limit television and other screen time |
Eat breakfast daily |
Limit eating out at restaurants, particularly fast-food restaurants |
Encourage family meals |
Limit portion size |
Encourage adequate daily physical activity |
Limit consumption of sugar-sweetened beverages |
Treating a child who has developed obesity is very challenging. Therefore, targeting primary obesity prevention within the family, school, and community environments is critical. Parents should offer regularly scheduled, balanced, varied meals and snacks for their children while limiting empty-calorie foods, high-fat meats, and dairy products. Parents should also promote physical activity and active play and limit screen time and sedentary activities. Schools should provide a healthy food environment, which limits using food as a reward and parties that serve primarily sweets.
Case Vignette: Follow-Up
At follow-up, Henry had maintained his weight from his previous visit. This was deemed successful since Henry had been gaining 1–2 kg monthly for the previous 8 months. His mother shared her challenges and successes in making healthy behavior changes. She found she was able to limit Henry’s juice and soda consumption when they ate at home but not when they ate out. Henry was successful with eating fruit at breakfast. She reported that initially Henry was reluctant to eat three bites of vegetables at dinner. However, both parents have been consistent in requiring this of Henry. Although Henry does not enjoy eating vegetables, he is indeed eating three bites without complaint. Mostly his mother felt positive and was motivated to make further efforts to support weight loss for Henry. A short-term weight loss goal was discussed and established for Henry based on recommendations provided by the American Academy of Pediatrics’ guidelines in treating overweight or obese children (Table 30.1). At this visit, the nutritionist recommended Henry be evaluated by a physical therapist to help develop a home exercise program.
Maintaining regular exercise and a healthy weight is beneficial for the overall health of children with neurodevelopmental disabilities and may improve sleep irregularities. Yet as discussed earlier in this chapter, meeting these recommendations poses many challenges for children with neurodevelopmental disabilities. Physicians may prescribe exercise to children; however, there are several factors to consider when creating a formal prescription for physical activity in children with neurodevelopmental disabilities [74]. First, it is important to obtain current health and fitness status to identify any reasons to restrict or modify activity. This also provides a baseline for tracking improvement. Next, physicians should maintain regular follow-up visits to monitor health and fitness progress and identify potential problems such as musculoskeletal issues.
Listed below are some useful tips to help incorporate physical activity into children’s routines. Additionally, some communities have recreation programs geared for children with neurodevelopmental disabilities. Those communities without specialized programs should evaluate creating opportunities for physical activity for this population, such as sports programming.
Incorporating physical activity into daily routines |
|---|
Help your kids participate in a variety of age-appropriate activities For preschoolers, play duck, duck goose, follow the leader, or freeze dance Older children may enjoy yoga, martial arts, or dance class Keep a variety of sports equipment on hand such as balls, hula hoops, or jump ropes |
Establish a regular schedule for physical activity Schedule physical activity on a calendar or set reminders on phone to remind your child it is time to get active Play outside for 15 min before going inside the house after school 10 min push-ups, sit-ups, etc. before dinner |
Incorporate activity into daily routines Take the stairs instead of the elevator Walk to school or walk around the block after being dropped off by school bus |
Embrace a healthier lifestyle yourself, so you’ll be a positive role model for your family Eat vegetables Try new foods Drink water instead of soda |
Keep it fun, so you can count on your kids to come back for more |
Case Vignette
When Henry returned to the nutritionist for his third visit, he had already seen the physical therapist that had helped his family develop an appropriate physical activity plan. They found that several short periods of exercise throughout the day were most effective for Henry. These 5–10-min exercise sessions were added as part of his family’s daily routine. By this visit Henry had lost 4 lbs over the previous 3 months, and his mother felt confident they could continue their new healthy lifestyle behaviors. Henry will continue to be followed every 3 months to ensure ongoing progress.
Further Research and Future Directions
The relationship between sleep duration, sleep timing, physical activity, and weight should be established in children with neurodevelopmental disabilities. Weight and physical activity are factors which can be modified by behavioral interventions. If the relationships between weight, physical activity, and sleep are clarified among children with neurodevelopmental disabilities, medical providers could have noninvasive interventions to promote for treatment of sleep disorders in this population. Further research may be able to establish specific physical activity type and duration recommendations to promote improved sleep onset and duration while limiting wakefulness. Similarly, best practices in treating obese children with neurodevelopmental disabilities should be established. Understanding specific techniques or teaching modalities which convey nutrition messages and motivate adherence to healthy eating habits can be helpful in promoting healthy weight in children with neurodevelopmental disabilities. Clarifying these relationships would help establish standards of practice for practitioners working with children with neurodevelopmental disabilities and sleep disorders.
References
U.S. Department of Health and Human Services. Physical activity guidelines for Americans. Washington, DC: U.S. Department of Health and Human Services; 2008.
King G, Law M, King S, Rosenbaum P, Kertoy MK, Young NL. A conceptual model of the factors affecting the recreation and leisure participation of children with disabilities. Phys Ther Occup Ther Pediatr. 2003;23:63–90.
Burgeson CR, Wechsler H, Brener ND, Young JC, Spain CG. Physical education and activity: results from the School Health Policies and Programs Study 2000. J of Sch Health. 2001;71:279–93.
Hinckson EA, Dickinson A, Water T, Sands M, Penman L. Physical activity, dietary habits and overall health in overweight and obese children and youth with intellectual disability or autism. Res Dev Disabil. 2013;34:1170–8.
Salaun L, Berthouze-Aranda SE. Physical fitness and fatness in adolescents with intellectual disabilities. J Appl Res Intellect Disabil. 2012;25:231–9.
Kim J, Mutyala B, Agiovlasitis S, Fernhall B. Health behaviors and obesity among US children with attention deficit hyperactivity disorder by gender and medication use. Prev Med. 2011;52:218–22.
Pan CY, Frey GC. Physical activity patterns in youth with autism spectrum disorders. J Autism Dev Disord. 2006;36:597–606.
Macdonald M, Esposito P, Ulrich D. The physical activity patterns of children with autism. BMC Res Notes. 2011;4:422.
Rimmer JA, Rowland JL. Physical activity for youth with disabilities: a critical need in an underserved population. Dev Neurorehabil. 2008;11:141–8.
Must A, Phillips S, Curtin C, Bandini LG. Barriers to physical activity in children with autism spectrum disorders: relationship to physical activity and screen time. J Phys Act Health. 2015;12:529–34.
Newacheck PW, Strickland B, Shonkoff JP. An epidemiologic profile of children with special health care needs. Pediatrics. 1998;102:117–23.
Chen AY, Kim SE, Houtrow AJ, Newacheck PW. Prevalence of obesity among children with chronic conditions. Obesity. 2010;18:210–3.
Must A, Phillips SM, Curtin C, Anderson SE, Maslin M, Lividini K, et al. Comparison of sedentary behaviors between children with autism spectrum disorders and typically developing children. Autism. 2014;18:376–84.
Feehan K, O’Neil ME, Abdalla D, Fragala-Pinkham M, Kondrad M, Berhane Z, et al. Factors influencing physical activity in children and youth with special health care needs: a pilot study. Int J Pediatr. 2012;2012:583249.
Kim K, Uchiyama M, Okawa M, Liu X, Ogihara R. An epidemiological study of insomnia among the Japanese general population. Sleep. 2000;23:41–7.
Chennaoui M, Arnal PJ, Sauvet F, Leger D. Sleep and exercise: a reciprocal issue? Sleep Med Rev. 2015;20:59–72.
Sherrill DL, Kotchou K, Quan SF. Association of physical activity and human sleep disorders. Arch Intern Med. 1998;158:1894–8.
Liu X, Uchiyama M, Kim K, Okawa M, Shibui K, Kidu Y, et al. Sleep loss and daytime sleepiness in the general adult population of Japan. Psychiatry Res. 2000;93:1–11.
King AC, Oman RF, Brassington GS, Bliwise DL, Haskell WL. Moderate-intensity exercise and self-rated quality of sleep in older adults: a randomized controlled trial. JAMA. 1997;277:32–7.
Singh NA, Clements KM, Fiatarone MA. A randomized controlled trial of the effect of exercise on sleep. Sleep. 1997;20:95–101.
Wang X, Youngstedt SD. Sleep quality improved following a single session of moderate-intensity aeromic exercise in older women: results from a pilot study. J Sport Health Sci. 2014;3:338–42.
Ekstedt M, Nyberg G, Ingre M, Ekblom O, Marcus C. Sleep, physical activity and BMI in six to ten year-old children measured by accelerometry: a cross –sectional study. Int J Behav Nutr Phys Act. 2013;10:82–91.
Tatsumi Y, Mohri I, Shimizu S, Tachibana M, Ohno Y, Tanike M. Daytime physical activity and sleep in pre-schoolers with developmental disorders. J Pediatr Child Health. 2015;51:396–402.
Iftikhar IH, Kline CE, Youngstedt SD. Effects of exercise training on sleep apnea: a meta-analysis. Lung. 2014;192:175–84.
Peeppard PE, Young T. Exercise and sleep-disordered breathing: an association independent of body habits. Sleep. 2004;27:480–4.
Williams P, Sears L, Allard A. Sleep problems in children with autism. J Sleep Res. 2004;13:265–8.
Wachob D, Lorenzi DG. Brief report: influence of physical activity on sleep quality in children with autism. J Autism Dev Disord. 2015;45:2641–6.
Evans CA, Selvadurai H, Baur LA, Waters KA. Effects of obstructive sleep apnea and obesity on exercise function in children. Sleep. 2014;37:1103–10.
Olds TS, Maher CA, Matricciani L. Sleep duration or bedtime? Exploring the relationship between sleep habits and weight status and activity patterns. Sleep. 2011;34:1299–307.
Mikulovic J, Dieu O, Fardy PS, Bui-Xuan G, Vanhelst J. Influence of sleep timing behavior on weight status and activity patterns in adults with intellectual disabilities. Res Dev Disabil. 2014;35:3254–9.
Vanhelst J, Bui-Xuan G, Fardy PS, Mikulovic J. Relationship between sleep habits, anthropometric characteristics and lifestyle habits in adolescents with intellectual disabilities. Res Dev Disabil. 2013;34:2614–20.
Mazurek MO, Wenstrup C. Television, video game and social media use among children with ASD and typically developing siblings. J Autism Dev Disord. 2013;43:1258–71.
Chonchaiya W, Nutnarumit P, Pruksananonda C. Comparison of television viewing between children with autism spectrum disorder and controls. Acta Paediatr. 2011;100:1033–7.
Council on Communications and Media. Media and young minds. Pediatrics. 2016;138:e20162591.
Engelhardt CR, Mazurek MO, Sohl K. Media use and sleep among boys with autism spectrum disorder, ADHD, or typical development. Pediatrics. 2013;132:1081–9.
O’Connor PJ, Raglin JS, Martinsen EW. Physical activity, anxiety and anxiety disorders. Int J Sport Psychol. 2000;31:136–55.
Murphy PJ, Campbell SS. Nighttime drop in body temperature: a physiological trigger for sleep onset? Sleep. 1997;20:255–64.
Ogden CL, Carroll MD, Lawman HG, Fryar CD, Kruszon-Moran D, Kit BK, Flegal KM. Trends in obesity prevalence among children and adolescents in the United States, 1988–1994 through 2013–2014. JAMA. 2016;315:2292–9.
Segal M, Eliasziw M, Phillips S, Bandini L, Curtin C, Kral TV, Sherwood NE, Sikich L, Stanish H, Must A. Intellectual disability is associated with increased risk for obesity in a nationally representative sample of U.S. children. Disabil Health J. 2016;9:392–8.
Rimmer JH, Yamaki K, Brienne MD, Wang E, Vogel LC. Obesity and overweight prevalence among adolescents with disabilities. Prev Chronic Dis. 2011;8:A41. Epub 2011 Feb 15
Bandini LG, Curtin C, Hamad C, Tybor DJ, Must A. Prevalence of overweight in children with developmental disorders in the continuous National Health and Nutrition Examination Survey (NHANES) 1999–2002. BMC Pediatr. 2010;10:11. https://doi.org/10.1186/1471-2431-10-11.
Egan AM, Dreyer ML, Odar C, Beckwith M, Garrison CB. Obesity in young children with autism spectrum disorders: prevalence and associated factors. Child Obes. 2013;9:125–31.
Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2009–2010. NCHS Data Brief. 2012;82:1–8.
Patel SR, Hu FB. Short sleep duration and weight gain: a systematic review. Obesity. 2008;16:643–53.
Cappuccio FP, Taggart FM, Kandala NB, Currie A, Peile E, Stranges S, et al. Meta-analysis of short sleep duration and obesity in children and adults. Sleep. 2008;31:619–26.
Knutson KL. Sex differences in the association between sleep and body mass index in adolescents. J Pediatr. 2005;147:830–934.
Van Cauter E, Spiegel K, Tasali E, Leproult R. Metabolic consequences of sleep and sleep loss. Sleep Med. 2008;9(supplement 1):S23–8.
Iglayreger HB, Peterson MD, Liu D, Parker CA, Woolford SJ, Sallinen Gafka BJ, Hassan F, Gordon PM. Sleep duration predicts cardiometabolic risk in obese adolescents. J Pediatr. 2014;164:1085–90.
Pileggi C, Lotito F, Bianco A, Nobile CG, Pavia M. Relationship between chronic short sleep duration and childhood body mass index: a school-based cross-sectional study. PLoS One. 2013;8(6):e66680.
El-Sheikh M, Bagley EJ, Keiley MK, Erath SA. Growth in body mass index from childhood into adolescence: the role of sleep duration and quality. J Early Adolesc. 2014;132:1145–66.
Schubert E, Randler C. Association between chronotype and the constructs of the three-factor-eating-questionnaire. Appetite. 2008;51:501–5.
Golley RK, Maher CA, Matricciani L, Olds TS. Sleep duration or bedtime? Exploring the association between sleep timing behaviour, diet and BMI in children and adolescents. Int J Obes. 2013;37:546–51.
Jarrin DC, McGrath JJ, Drake CL. Beyond sleep duration: distinct sleep dimensions are associated with obesity in children and adolescents. Int J Obes. 2013;37:552–8.
Redline S, Tishler PV, Schluchter M, Aylor J, Clark K, Graham G. Risk factors for sleep-disordered breathing in children. Associations with obesity, race and respiratory problems. Am J Respir Crit Care Med. 1999;159:1527–32.
Bonuck K, Chervin RD, Howe LD. Seep-disordered breathing, sleep duration and childhood overweight: a longitudinal cohort study. J Pediatr. 2015;166:632–9.
Shi Z, Taylor AW, Gill TK, Tuckerman J, Adams R, Martin J. Short sleep duration and obesity among Australian children. BMC Public Health. 2010;10:609.
Centers for Disease Control and Prevention. http://www.cdc.gov/healthyweight/assessing/bmi/childrens_bmi/about_childrens_bmi.html.
Morselli L, Leproult R, Balbo M, Spiegel K. Role of sleep duration in the regulation of glucose metabolism and appetite. Best Pract Res Clin Endocrinol Metab. 2010;24:687–702.
Hart CN, Carskadon MA, Considine RV, Fava JL, Lawton J, Raynor HA, et al. Changes in children’s sleep duration on food intake, weight and leptin. Pediatrics. 2013;132(6):e1473–80.
Boeke CE, Storfer-Isser A, Redline S, Taveras E. Childhood sleep duration and quality in relation to leptin concentration in two cohort studies. Sleep. 2014;37:613–20.
St-Onge MP. The role of sleep duration in the regulation of energy balance: effects on energy intakes and expenditure. J Clin Sleep Med. 2013;9:73–80.
Chaput JP, St-Onge MP. Increased food intake by insufficient sleep in humans: are we jumping the gun on the hormonal explanation? Front Endocrinol. 2014;5:116.
Calvin AD, Carter RE, Adachi T, Macedo PG, Alburquerue FN, van der Walt C, et al. Effects of experimental sleep restriction on caloric intake and activity energy expenditure. Chest. 2013;144:79–86.
Blunden SL, Milte CM, Sinn N. Diet and sleep in children with attention deficit hyperactivity disorder: preliminary data in Australian children. J Child Health Care. 2011;15:14–24.
Kral TV, Eriksen WT, Souders MC, Pinto-Martin JA. Eating behaviors, diet quality, and gastrointestinal symptoms in children with autism spectrum disorders: a brief review. J Pediatr Nurs. 2013;28:548–56.
Kral TV, Souders MC, Tompkins VH, Remiker AM, Eriksen WT, Pinto-Martin JA. Child eating behaviors and caregiver feeding practices in children with autism spectrum disorders. Public Health Nurs. 2015;32(5):488–97.
Correll CU. Weight gain and metabolic effects of mood stabilizers and antipsychotics in pediatric bipolar disorder: a systematic review and pooled analysis of short-term trials. J Am Acad Child Adolesc Psychiatry. 2007;46:687–700.
Brown CL, Irby MB, Houle TT, Skelton JA. Family-based obesity treatment in children with disabilities. Acad Pediatr. 2015;15:197–203.
Epstein LH, Valoski A, Wing RR, McCurley J. Ten-year outcomes of behavioral family-based treatment for childhood obesity. Health Psychol. 1994;13:373–83.
Golan M, Crow S. Targeting parents exclusively in the treatment of childhood obesity: long-term results. Obes Res. 2004;12:357–61.
Golan M, Weizman A, Apter A, Fainaru M. Parents as the exclusive agents of change in the treamtnet of childhood obesity. Am J Clin Nutr. 1998;67:1130–5.
Daniels SR, Hasink SG, Committee on Nutrition. The role of the pediatrician in primary prevention of obesity. Pediatrics. 2015;136:e275–92.
Barlow SE. Expert committee recommendations regarding the prevention, assessment and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120(Suppl 4):S164–92.
Sullivan MG. http://www.mdedge.com/pediatricnews/article/46296/pediatrics/rev-obese-kids-exercise-prescriptions. 2011. Accessed 26 Oct 2017.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Heyman, A. (2019). Exercise, Weight, and Sleep. In: Accardo, J. (eds) Sleep in Children with Neurodevelopmental Disabilities. Springer, Cham. https://doi.org/10.1007/978-3-319-98414-8_30
Download citation
DOI: https://doi.org/10.1007/978-3-319-98414-8_30
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-98412-4
Online ISBN: 978-3-319-98414-8
eBook Packages: MedicineMedicine (R0)