Abstract
The purpose of this study was to examine age-related physical activity patterns in youth with autism spectrum disorders (ASD). Thirty youth, aged 10–19 years, were divided into three groups: elementary (n=9), middle (n=9) and high (n=12) school. Participants wore an accelerometer and completed an activity questionnaire for seven consecutive days. The main findings were that (a) elementary youth are more active than the other groups, regardless type of day or time period, and (b) there are no consistent patterns in physical activity of youth with ASD according to day or time period. Findings emphasize that interventions for this population should address increasing extracurricular physical activity options during adolescence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Youth with autistic spectrum disorders (ASD) may be at risk for inactivity due to social and behavioral deficits often associated with the condition, such as difficulties understanding social cues, making eye contact, playing imaginative and social games, engaging in sharing/turn-taking and reciprocal conversation, and making friends (Autism Society of America, 2002). Social and behavioral deficits could limit opportunities for these individuals to participate in physical activity, because most youth are physically activity with peers (Fox & Riddoch, 2000). However, data regarding physical activity patterns in youth with ASD are apparently lacking and there are few published physical activity studies that have included this population. Levinson and Reid (1991) examined physical activity in youth with a variety of disabilities, including ASD, using parent reports and found that youth with disabilities are essentially inactive, but participants with ASD were not specifically discussed. It is clear that people with ASD have been excluded from the physical activity literature.
The lack of information on this topic in those with ASD is regrettable because the importance of physical activity to overall health for all individuals has been well-documented and increasing physical activity among youth is a critical, national health objective (U.S. Department of Health and Human Services (USDHHS), 2000). Regular physical activity participation reduces risk for morbidity and mortality associated with chronic diseases such as cardiovascular disease, certain cancers, diabetes, and obesity (USDHHS, 2002), and multiple cardiovascular disease risk factors have been observed in youth (Berenson & Srnivasan, 2005). Physical activity also leads to positive self-esteem, behavior, happiness, and intellectual, and social outcomes in youth (Biddle, Sallis, & Cavill, 1998; Strauss, Rodzilsky, Burack, & Colin, 2001). The only related research in youth with ASD has been the use of exercise to decrease self-stimulating or maladaptive behavior, although no long-term studies on this topic exist (Celiberti, Bobo, Kelly, Harris, & Handleman, 1997; Elliott, Dobbin, Rose, & Soper, 1994). Despite a lack of research, it is reasonable to assume that the general physical and mental health benefits of physical activity would also extend to youth with ASD. Related literature is focused on prevention or treatment of primary and associated conditions and there appear to be no studies that have addressed healthy living in this population. This is a concern for two reasons: (a) as previously mentioned, autistic traits might predispose youth with ASD to be inactive; and (b) weight gain is a common side effect of medications used to treat autistic symptoms (Scahill & Koenig, 1999), both of which could negatively affect healthy living. Research is needed to understand the risk for developing chronic disease associated with inactivity in youth with ASD.
Current physical activity recommendations based on youth without disabilities are generally that: (a) children should engage in at least 60 min or more of age and developmentally appropriate physical activity on all or most days of the week and (b) adolescents should be active every day, including 20 min bouts of continuous moderate to vigorous physical activity (MVPA) three or more times per week (USDHHS, 2002). These guidelines should also apply to youth with ASD, but it is not clear if they are meeting these minimum standards. The paucity of similar research on youth with other disabilities indicates that those with mental retardation (Suzuki et al., 1991), physical disabilities, sensory impairments, and other health impairments (Longmuir & Bar-Or, 2000) do not meet these guidelines and are generally more sedentary than peers without disabilities. Disability is a primary physical activity determinant and students with conditions perceived as less physically or cognitively restrictive (e.g., hearing impairments) are more active than those with mental or physical disabilities (Longmuir & Bar-Or, 2000; Suzuki et al., 1991). Therefore, reports on this topic cannot be generalized across disabling conditions. Research is needed to determine if the unique characteristics associated with ASD present a greater risk for inactivity compared to other types of disabilities and those without disabilities.
Beyond overall physical activity levels, it is also important to examine physical activity patterns in this population. It is documented that physical activity significantly decreases during adolescence and varies according to day of week and time of day, although there is no consensus regarding optimal times for youth to be active (Gavarry, Giacomoni, Bernard, Seymat, & Falgairette, 2003; Mota, Santos, Guerra, Ribeiro, & Duarte, 2003). The observed decline in physical activity with adolescence is partially due to a reduction in school time devoted to physical education and recess with age (USDHHS, 2000). This might be particularly important for youth with ASD because this group acquires a significant portion of daily MVPA during recess (Rosser & Frey, 2005). In addition, youth with ASD have few opportunities for extracurricular physical activity. The competitive focus of community-based programs often prohibits successful participation and these individuals are typically ineligible for segregated programs such as Paralympics or Special Olympics, because, depending on the severity of the condition, diagnostic criteria are not always met. Essentially, youth with ASD are in an indeterminate state regarding physical activity participation. There are few segregated programs that can address the special needs of those with ASD, but because of these special needs this group is likely to be excluded or unsuccessful in integrated activities. As a result, physical activity patterns in youth with ASD are probably different from peers who are afforded greater opportunities to be active.
Physical activity in youth with ASD can be explained to some extent by the social model of disability (Llewellyn & Hogan, 2000). The majority of theoretical approaches used to examine physical activity in youth are based on social–cognitive models. In general, these theories operate on an assumption of reciprocity between the individual and the environment (Taylor, Baranowski, & Sallis, 1994), which is difficult to apply to those with disabilities because this population has less control over and accessibility to the environment than the general population. Youth without disabilities have access to physical activity programs, but choices to engage in activity are determined by social, cognitive or cultural variables. Youth with ASD often do not have basic access to physical activity opportunities for various reasons related to the disability and consequently are not afforded the same choices to be active. For example, an individual with ASD might be prohibited from joining an after-school program due to concerns expressed by staff regarding behavior. According to the social model of disability, physical activity patterns of youth with ASD are more affected by social constraints than the actual impairment (Llewellyn & Hogan, 2000).
Therefore, this research project was undertaken for two main reasons: (a) physical activity is important to overall health and well-being; and (b) there is little information on physical activity in youth with ASD. Physical activity was objectively examined in a sample of these individuals according to day of week (weekday vs. weekend) and within day-time period [in school (9:00 a.m. to 2:00 p.m.) vs. after school (3:00–6:00 p.m.)] to determine if clear physical activity patterns existed. Based on the social model of disability, it was hypothesized that youth with ASD would not engage in regular physical activity regardless of day or time period.
Method
Participants
Data were collected on 35 youth, but 5 were excluded due to incomplete data or equipment malfunction. The final sample consisted of 30 (boys, n=27; girls, n=3) youth, ages 10–19 years (M age=13.2 years, SD=2.1). Participants were recruited within a 130 mile radius of the main research site, through a university-based physical activity program for youth with disabilities, an autism resource center, local autism support groups, a local summer camp for youth with ASD, and available media (direct contact, e-mail announcement, autism listserves). In an effort to obtain a homogenous sample, recruitment was restricted to participants rated as high-functioning on the autism spectrum, according to parent reports. Individuals with mental retardation as a co-occurring condition, as well as those with severe behavior problems that required formal intervention, were excluded. All received varying levels of special education services under the category of autism, except those who were home-schooled (Table 1). Participants were at least 6-years post-diagnosis (M=7.08, SD=2.92), and diagnoses included Autism (boys, n=12; girls, n=2), Asperger’s syndrome (boys, n=11; girls, n=1), and Pervasive Developmental Disorder-Not Otherwise Specified (PDD-NOS) (boys, n=4). Most exhibited various stereotypes, primarily rocking or pacing, but this was not controlled due to difficulty in obtaining reliable assessments without direct observation. Parents indicated these movements were not severe and did not warrant behavior modification. All but six manifested associated conditions such as anxiety (n=6), obsessive-compulsive disorder (n=3), mental health problems (n=2), attention deficit and/or hyperactivity (n=5), seizures (n=3), Tourette’s syndrome or tic disorers (n=3), fine or gross motor delays (n=5), mild physical conditions (n=3), or general health problems (e.g. asthma, allergies) (n=9), and many had multiple co-occurring conditions. Twenty-two participants were on medications to relieve symptoms associated with ASD and many were on multiple medications. General language skills included nonverbal (n=4), a few sentences (n=3), and normal speech patterns (n=23), as based on parent reports and researcher interaction with participants. Twenty-eight resided in urban settings and two in rural settings. Twenty-eight lived in a two-parent household and 12 (ES, ne=3; MS, n=6; HS, n=3) were enrolled in a segregated community-based physical activity programs, such as adapted martial arts or adapted aquatics. One participant was 19-years-old and attended college courses full-time, but lived at home. Since there were no differences in physical activity variables between HS participants and the individual in college, these data were combined in the analysis. Additional participant demographics are presented in Table 1.
Procedures
The study protocol was approved by the university review board for the protection of human subjects. Study objectives and methods were individually explained to and written consent and assent obtained from parents and youth, respectively. Height and weight measures were collected in a private setting with all youth dressed in light clothing and shoes removed for calculation of body mass index (kg/m2). Since youth physical activity is difficult to measure in field settings, two assessment methods were used to increase measurement accuracy (Kohl, Fulton, & Caspersen, 2000).
Accelerometry
The Manufacturing Technologies Inc. (MTI) 7164 uniaxial accelerometer (Shalimar, Florida) is a small (5.1×4.1×1.5 cm), light weight (42.5 g) single channel device designed to measure and record acceleration ranging in magnitude from .05 to 2.00 G with frequency response from .25 to 2.50 Hz. The filtered acceleration signal is digitized and the magnitude is summed over a user-specified period of time. At the end of each epoch, the summed value is stored in memory and the numerical integrator is reset. A large signal or count represents high levels of physical activity. At the end of data collection accelerometers were downloaded and data organized using associated software.
The MTI accelerometer is considered valid for use in field-based studies of physical activity in youth (Trost et al., 1998). Rosser and Frey (2005) also found that children with ASD can tolerate the instrument. Consistent with previous studies, the accelerometer was placed in a small nylon pouch and worn over the right hip either with a clip or with an elastic belt (Trost et al., 2002). Prior to data collection, all participants engaged in practice trials wearing the device. Verbal and written instructions on how to wear and care for the device were provided. A time sheet was also provided to record when the accelerometer was worn. All participants wore the device during waking hours, except bathing or water activities, for 7 consecutive days (2 weekends and 5 weekdays) between the months of September and November. This represented a period of mild weather in the region where participants resided.
Accelerometers were programmed to collect data in 1-min intervals. Activity counts were analyzed to determine total movement counts, counts per minute (CPM), and time spent in light (<3 MET), moderate (3–5.9 MET), vigorous (6–8.9 MET), and very vigorous (≥9 MET) physical activity using age-specific count cutoffs corresponding to each specified intensity level (Freedson, Melanson, & Sirard, 1998; Trost, Pate, Freedson, Sallis, & Taylor 2000). For example, physical activity at a moderate intensity value ranged between 1017 CPM for 10-year-olds and 2274 CPM for 18-year-olds. The frequency of continuous 5-, 10-, and 20-min MVPA at an intensity greater than or equal to 3 METs was also calculated. Continuous MVPA was established: (a) 5-min MVPA=minutes ≥5 but <10 min, (b) 10-min MVPA=minutes ≥10 but <20 min, and (c) 20-min MVPA=minutes ≥20.
Pilot work indicated that youth would tolerate about 8 h of monitor wear and parents indicated that this was representative of the child’s highest physical activity levels. This time period is slightly less than that previously used (Mota et al., 2003), but there are no guidelines regarding specific time periods that are representative of the entire day’s physical activity (Trost et al., 2000). Therefore, participants were asked to wear the accelerometer for no less than 8 h a day during data collection. Four days of monitoring have been shown to achieve reliable physical activity estimates in youth (Trost et al., 2000) and participants with less than 8 h of monitoring data on each day or less than 4 days (including 1 weekend day) of completed monitoring were excluded from the analyses.
Accelerometer data were also divided according to two time periods during school days: in school (9:00 am to 2:00 pm) and after school (3:00 to 6:00 pm). A 1 h gap between 2:00 and 3:00 pm was used to control for individual differences at the finish of the school day. The after-school time period (3:00 to 6:00 pm) was chosen because few youth in the present study wore the accelerometers beyond 6:00 pm during school days and this has been identified as the after school period when youth are most active (Mota et al., 2003).
Questionnaire
The Child/Adolescent Activity Log (CAAL) is a 21-item questionnaire designed to measure daily physical activity. It was chosen because (a) it is a valid and reliable measure of physical activity in children/adolescents, and (b) it is easy to administer (Garcia, George, Coviak, Antonakos, & Pender, 1997). For the purposes of this study, the CAAL was used to qualify activity patterns, rather than as an assessment tool per se because of the inherent difficulties associated with self-reports in youth (Dale, Welk, & Matthews, 2002). It was pilot tested with five parents of youth with disabilities to ensure if the format, words, and activities needed to be adapted to fit this population. Based on parent input it was decided that if youth with ASD could not independently fill out the questionnaire, parents could assist with this task. None of the activity items were changed from the original questionnaire after pilot testing.
The CAAL was completed daily during the same period the monitor was worn. Youth recalled the activities they participated in each day (all day for the weekends and only after school (3:00 pm to bedtime) during weekdays) and circled the total number of minutes of participation for each activity that day. The amount of time spent watching television and playing computer games was also estimated over the week, and expressed on a daily basis (all day for the weekends and only after school (3:00 pm to bedtime) during weekdays). All participants were asked to take a packet of logs home and the researcher provided telephone call reminders to complete the log, as needed. Questionnaires were reviewed with both participants and parents upon return to verify responses.
Statistical Analysis
Participants were divided into three groups according to school level: ES (n=9), MS (n=9), and HS (n=12) to address potential differences in activity opportunities (e.g., no recess in MS and HS). Physical activity variables were examined separately at each school level for the fit between distributions and assumptions of normality and homoscedasticity. All cases remained for further analysis because assumptions were met and no multivariate outliers were identified. Gender differences in the physical activity variables were tested using independent t-tests. Results revealed no difference between girls and boys, and genders were combined for further analysis. Pilot work revealed little participation in vigorous or very vigorous physical activity, so these categories were combined with moderate physical activity and reported as MVPA.
Intraclass correlation coefficients and 95% confidence intervals were calculated to investigate the intra- and inter-individual variation in activity scores across different days of assessment (2 weekends and 5 school days). School level and day of week differences were analyzed using a two-way ANOVA (school level×day of week) with repeated measures on one factor (day of week: weekday versus weekend). Least significant difference (LSD) posthoc tests were undertaken if significant difference or interaction between factors were observed. If there was a difference between school levels, a two-way ANOVA (school level×school day time period) with repeated measures on one factor (school day time period) was used to analyze youth group and school day time period differences. If there was no difference between youth groups, paired-sample t-tests were used to examine whether the physical activity variables differed significantly between two different time periods during school days (9:00 am to 2:00 pm versus 3:00 to 6:00 pm) for all participants. All statistical analyses were conducted with SPSS (version 12.0). Values are presented as M±SD with significance set at P<.05.
Daily non-school physical activity reported in the CAAL was calculated by summing the minutes of all the activities performed in one day, adding these totals for 5 weekdays or 2 weekends, and dividing number of days accordingly. The duration of the activity was defined as the midpoint of the time interval: 5.5 min for 1–10, 15.5 min for 11–20, and so forth (Garcia et al., 1997). The five most frequently cited activities according to school level were also determined.
Results
Intraclass correlation coefficients demonstrated strong relationships between measured days: weekends R=.83, CI .63–.92 and weekdays R=.93, CI .87–.92. There were no differences between days, so the 2 weekends and 5 weekdays were combined for further analysis.
Weekly Physical Activity
Complete data sets were available for 203 monitored days. Twenty-four participants wore the accelerometer for the full 7 days. Seven monitored days (3 weekends and 4 weekdays) were lost from 6 participants due to incomplete monitoring data (<8 h per day). For the total group, 47% of youth (n=14) accumulated at least 60 min of daily MVPA. There were no differences in overall physical activity or MVPA between weekdays and weekends, but participants acquired more bouts of 5- and 10-min continuous MVPA on weekends compared to weekdays (+1.4 and +.9 times/day, respectively) (Table 2).
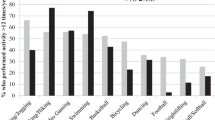
When analyzed according to school level, 78% of ES (n=7) and 67% of MS (n=6) youth accumulated recommended MVPA, while only .08% of HS youth (n=1) met this guideline. No group met the recommendation of engaging in bouts of 20-min, continuous MVPA at least three times a week (Table 3). There were significant differences between the three school levels for all physical activity variables. Youth in ES were more active overall than those in HS (+309.3) and spent more time in MVPA compared to MS (+57.4) and HS (+92.9) groups. However, there were no differences in overall physical activity or MVPA between MS and HS groups. Youth in ES also acquired more bouts of continuous MVPA throughout the week compared to MS (+7.4, +3.9, +.9 times/day for 5-, 10-, and 20-min continuous MVPA, respectively) and HS (+8.6, +4.1, +.9 times/day for 5-, 10-, and 20-min continuous MVPA, respectively) groups. Further analysis according to school level and day of week revealed that ES youth spent more time in 10-min continuous MVPA on both weekdays and weekends than MS (+2.8 and +4.9) and HS (+3.1 and +5.0) groups (Table 3, Fig. 1).
School Day Time Period
Significant differences in physical activity were demonstrated between groups on all physical activity variables during different periods of the school day (Table 4). Youth in ES were more active overall than those in HS (+331.7) and spent more time in MVPA compared to both MS (+17.3) and HS (+24.8) groups. Youth in ES were also more continuously active at all levels (5-, 10-, and 20-minute bouts) than MS (+2.0, +1.0, and +.3 times/day, respectively) and HS (+2.1, +1.0, and +.3 times/day, respectively) groups. All participants were more active after school (+98.9), but engaged in more MVPA during school (+5.8).
A significant interaction effect was observed for all continuous MVPA time periods. Youth in ES spent more time in continuous MVPA during school than MS (+2.7, +1.4, +.5 for 5-, 10- and 20-min continuous MVPA, respectively) and HS groups (+2.8, +1.3, +.5 for 5-, 10- and 20-min continuous MVPA, respectively). After school, youth in ES spent more time in 5-min continuous MVPA than the HS group (+1.5), and engaged in more 10-min continuous MVPA than both MS (+.6) and HS (+.7) youth (Figs. 2 & 3). No significant group differences existed in 20-min continuous MVPA after school.
Questionnaire
About 80% of youth were able to complete the questionnaire on their own and 20% needed parent assistance. Complete data sets were available for 148 weekdays, with 2 days lost because participants forgot to fill out the log. Participant compliance with completing the CAAL for weekends varied greatly. Even though instructions were provided verbally and in written form, many participants either failed or partially completed the weekend entries. As a result, these data were not included in the analysis. Daily average time spent in non-school physical activity during weekdays was 30, 43 and 17 min in ES, MS, and HS youth, respectively. Walking was the most frequently reported form of physical activity (7.93 min/day). Other popular activities included tae kwon do/karate/martial arts (3.09 min/day), weightlifting (2.68 min/day), swimming (1.24 min/day), ice/roller skating (1.21 min/day), and jogging/running (.81 min/day).
Discussion
To date, this is one of the few attempts to examine physical activity levels and patterns in youth with ASD. The results indicate that youth with ASD are less active than previous reports on peers without disabilities (Trost et al., 2002). However, other aspects of physical activity behavior are similar to those observed in youth without disabilities: (a) physical activity declines with school level in this group (USDHHS, 2000; 2002); (b) some youth with ASD accumulate recommended amounts of MVPA, but this varies according to school level (USDHHS, 2000); (c) there are no clear patterns in overall PA or MVPA according to type of day or school day time period (Trost et al., 2000); and (d) this population does not regularly engage in continuous MVPA (Trost et al., 2002). Unfortunately, it appears that youth with ASD are at similar risk for health problems associated with inactivity as those without disabilities.
It is recommended that youth accumulate 60 min or more of MVPA each day, but most do not meet this standard (USDHHS, 2000, 2002). Less than half of the participants in this study were moderately active on a regular basis and the HS group was particularly inactive which coincides with related research on youth without disabilities (Allison & Adlaf, 1997). While it was expected that youth with ASD would exhibit lower physical activity levels than peers without disabilities, the lack of apparent differences in activity patterns between groups was surprising, although the data on this topic are equivocal. In the current study, day of week had no impact on physical activity variables, except participants engaged in more bouts of 10-min continuous MVPA on weekends, and this primarily occurred in the ES group. Some studies have found no differences in overall physical activity of children between weekdays and weekends (Gilbey & Gilbey, 1995; Sallo & Silla, 1997), while others have observed that adolescents were more active during either weekdays (Trost et al., 2000) or weekends (Huang & Malina, 1996).
In contrast to day of week, there was a tendency for physical activity patterns to vary during time periods within school days. Youth in ES spent more time in MVPA during school than those in MS and HS, but this pattern was not replicated after school. Rosser and Frey (2005) conducted the only other study that examined time periods in children with ASD and also found that more time is spent in MVPA during school compared to after school. Similar research on youth without disabilities has not provided a consensus regarding youth activity patterns during time periods (Mota et al., 2003; Trost et al., 2000).
Despite the lack of agreement regarding activity patterns, research is very consistent that youth typically do not engage in long bouts of continuous activity (Trost et al., 2002; USDHHS, 2000), which was also evident in the current study. Physical activity guidelines suggest that youth should engage in some level of continuous MVPA every day or each week (USDHHS, 2002). Participants with ASD engaged in very few sustained bouts of MVPA, with ES youth acquiring more bouts of continuous activity than the other groups, and all participants were more continuously active on weekends. The average number of weekly, 20-min, continuous MVPA bouts approached zero for all groups, but there was a clear trend for greater participation in shorter bouts of continuous MVPA (e.g., 5- and 10-min). Since both youth with and without ASD are unlikely to engage in long bouts of continuous MVPA, and there is no established relationship between continuous physical activity and health benefits in this population, recommendations should be reconsidered.
The observed physical activity behaviors of youth with ASD in this study can be partially described by the social model of disability. According to this model, it can be argued that low levels of physical activity in this population are due to “society’s failure to provide appropriate services and adequately ensure [that] the needs of disabled people are fully taken into account in its social organization” (Oliver, 1996, p. 32). That is, youth with ASD are disadvantaged because of societal treatment, rather than characteristics of the actual impairment, and lack of societal acceptance and support might limit access to community and education physical activity opportunities (Llewellyn & Hogan, 2000).
This was illustrated by the limited quality and quantity of activity options for participants, regardless of the day or time period. Youth with ASD were essentially afforded the same physical activity opportunities as peers during the school day, but were not regularly active during these times. For example, ES youth attended physical education 2–3 times per week for 30–45 min per session and 52% of MS and HS youth were enrolled in physical education, whereas almost 44% of secondary level youth without disabilities are not enrolled in physical education (USDHHS, 2000). Regardless of physical education attendance rates, most participants reported limited activity during this time. Rosser and Frey (2005) also observed low levels of MVPA during physical education in children with ASD, but this was not different from peers without disabilities. In addition, many children with ASD received physical education from special education teachers or classroom aides, neither of which was qualified to provide appropriate instruction in this area. Previous research has shown that physical education does not promote enough MVPA because there is excessive sitting or standing in line before engaging in activities (McKenzie, Marshall, Sallis, & Conway, 2000). Physical education presents an important opportunity to engage in physical activity, and more emphasis should be placed on delivery of quality instruction by teachers with proper certification and experience working with youth with ASD.
Recess was an activity option not available to all participants and likely accounted from some of the observed differences between groups. Youth in ES attended recess every day and youth in MS and HS had no recess time. Recess time was not specifically examined in this study, but evidence suggests that all young children are more likely to be active during unstructured play environments (Pate, Baranowski, Dowda, & Trost, 1996). Rosser and Frey (2005) observed that children with ASD had high physical activity levels in recess because they often engaged in play with playground equipment and activities that were unstructured or required little, if any, social interaction. However, this time period was limited with an average recess time of 15 min, and most children were removed from recess early by teachers to ease transitions between classes or start assignments early in subsequent classes. Maximal participation in MVPA during recess should be promoted for youth with ASD in ES, and since changes in school time structure with age are not typically modifiable, other physical activity options for older youth must be scheduled into the day to compensate for a lack of recess.
Access to extracurricular activities is where large disparities in activity options between youth with and without disabilities appear to occur. Approximately 40% of participants were enrolled in extracurricular physical activity programs, but only 10% of these were HS students, and time spent in those activities was minimal (e.g., approximately 30 min per week). The majority of programs identified were segregated and offered within one community. Those who resided outside this community were either not aware of or did not have access to specialized physical activity programs. In contrast, a majority of ES youth without disabilities (84%) participate in at least one community-based physical activity and approximately 37% of HS youth without disabilities participate in community-based sport teams (Kann, Warren, & Harris, 1999). Youth with ASD, particularly those of HS age, do not exhibit the same physical activity participation rates as peers without disabilities, which appears to have a negative impact on physical activity levels in this group. Rosser (2004) also found that both integrated and segregated extracurricular physical activity programs for youth with ASD were lacking, according to parent and teacher reports. It appears that unavailability of physical activity programs is a significant factor in the physical activity behavior of youth with ASD.
The influence of participant’s residence on access to physical activity programs further supports the social model of disability as a partial explanation of the current findings. As previously mentioned, most extracurricular physical activity occurred in one community. This particular community offered a variety of services that promoted physical activity for youth with ASD, including adapted swimming and martial arts through the local YMCA, therapeutic horseback riding, Challenger baseball, and a university adapted physical education program. The YMCA and local parks and recreation organization also employed an inclusion specialist that designed individualized programs so consumers could participate in either integrated or segregated activities. In general, this community provided services and supports so that youth with ASD could successfully participate in physical activity (Llewellyn & Hogan, 2000). Unfortunately, other participants resided in communities that did not offer these supports; even though physical activity resources were available (e.g., youth sports programs, health club facilities, etc.). This suggests that availability of resources is not enough, and creating access to resources through appropriate programming, staff training, and activity modification is imperative for youth with ASD to successfully engage in physical activity. For this to occur, society must provide the necessary supports.
While the social model of disability has provided a reasonable framework for partially describing physical activity patterns in this group, no model can explicitly explain all aspects of behavior (Llewellyn & Hogan, 2000). Individual personality traits must also be considered when examining physical activity behavior and it is important to understand that autistic traits are part of the individual. For example, several youth with ASD reported a lack of enjoyment for anything physical and did not like “feeling of sweaty”. These individuals chose to be inactive, coinciding with the majority of society which also chooses to be inactive (USDHHS, 2002). Most participants indicated a lack of enjoyment for team sports and preferred individual activities such as martial arts and swimming. These activities typically occurred within a group context, but there were no performance expectations that could influence group outcomes and this made those experiences less stressful. Walking was the most frequently reported non-school activity, and it was the only activity in which almost all youth consistently participated. Orsmond, Krauss, and Seltzer (2004) also found that adolescents and adults with ASD preferred recreational activities that did not present extensive social demands (e.g., walking). This is different from research examining common activities in 6th–8th graders without disabilities, where male adolescents predominantly engaged in team-oriented sports (Harrell et al., 2003). These findings suggest that youth with ASD might develop a greater predilection for physical activity if allowed to choose activities based on preference, rather than socialization opportunities.
Institutional change is difficult and long-term; therefore, physical activity interventions for this group should focus on promoting individual or dual activities that often require fewer societal supports. Team sports demand an ability to quickly understand, process, and respond to social cues under the pressure of competition, and expecting an individual with ASD to function or be accepted by peers in this setting is unrealistic. Individual or dual activities (e.g., running, swimming, tennis) present several advantages compared to traditional team sports (e.g., basketball, baseball), particularly for youth with ASD, because: (a) fewer social demands exist; (b) fewer people are needed to participate, which is more practical in terms of time and effort; (c) these activities are more easily continued into adulthood, again because there is less reliance on others; (d) the rhythmic nature of many individual activities are conducive to repetitive traits often associated with ASD; and (e) these activities can be performed using family resources, without reliance on external supports. There exist several excellent references to assist professionals, practitioners, and parents with developing and implementing appropriate physical activity or recreation programs for youth with ASD (Hawkins, 1991; Houston-Wilson & Lieberman, 2003; Reid & O’Connor, 2003).
The cross-sectional design of this study limits generalization. Physical activity may have been underestimated because accelerometers are less accurate when assessing non-weight bearing activities (e.g., swimming and bicycling), but few participants reported significant amounts of these activities. These devices are still one of the most commonly used, noninvasive, objective indicators of physical activity in field settings (Dale et al., 2002). Assessing the influence of stereotypic behavior on physical activity was beyond the confines of this research design. Although most participants reportedly engaged in some form of stereotypy, typically pacing or rocking, these actions were not considered severe enough to warrant intervention, and obtaining accurate information on these movements could not be obtained without direct observation. Similar behaviors in those without disabilities (e.g., fidgeting) are usually incorporated as part of overall activity; however, since stereotypic behaviors are more prevalent in youth with ASD, future research should assess the relative contribution of these movements to physical activity in this group. Even though all attempts were made to obtain a homogenous sample of youth that were high-functioning on the autism spectrum, differences in social skills, behaviors, cognitive abilities, and medications were also not evaluated and might have influenced findings. Further research is needed to understand the impact of these variables on physical activity behavior in this population.
Design limitations notwithstanding, these results provide meaningful, novel information regarding physical activity patterns of youth with ASD. Similar to youth without disabilities, this population is at risk for health problems associated with inactivity. Efforts should focus on identifying appropriate in-school and leisure-time physical activity options that encourage MVPA and meet the unique needs of youth with ASD. Additional inquiry is needed to (a) investigate gender differences, specific diagnostic categories, or evaluate physical activity based on some type of social skills inventory, and (b) identify the relative contribution of various physical activity determinants in this population. It is important that health issues in people with ASD are examined beyond the symptoms of the condition so that healthy lifestyles, including physical activity participation, can be promoted.
References
Allison, K. R., & Adlaf, E. M. (1997). Age and sex differences in physical inactivity among Ontario teenagers. Canadian Journal of Public Health, 88(3), 177–180.
Autism Society of America. (2002). Retrieved November 5:2002, http://www.autism-society.org/.
Berenson, G. S., & Srnivasan, S. R. (2005). Cardiovascular risk factors in youth with implications for aging: The Bogalusa heart study. Neurobiology of Aging, 26, 303–307.
Biddle, S. J. H., Sallis, J. F., & Cavill, N. (1998). Young and active? Young people and health-enhancing physical activity: Evidence and implications. London: Health Education Authority.
Celiberti, D. A., Bobo, H. E., Kelly, K. S., Harris, S. L., & Handleman, J. S. (1997). The differential and temporal effects of antecedent exercise on the self-stimulatory behavior of a child with autism. Research in Developmental Disabilities, 18(2), 139–150.
Dale, D., Welk, G. J., & Matthews, C. E. (2002). Methods for assessing physical activity and challenges for research. In G. J. Welk (Ed.), Physical activity assessments for health-related research (pp. 19–34). Champaign, IL: Human Kinetics.
Elliott, R. O. J., Dobbin, A. R., Rose, G. D., & Soper, H. V. (1994). Vigorous, aerobic exercise versus general motor training activities: Effects on maladaptive and stereotypic behaviors of adults with both autism and mental retardation. Journal of Autism and Developmental Disorders, 24(5), 565–576.
Freedson, P. S., Melanson, E., & Sirard, J. (1997). Calibration of the computer science and applications, Inc. accelerometer. Medicine and Science in Sports and Exercise, 30(5), 934–940.
Garcia, A. W., George, T. R., Coviak, C., Antonakos, C., & Pender, N. J. (1997). Development of the child/adolescent activity log: A comprehensive and feasible measure of leisure-time physical activity. International Journal of Behavioral Medicine, 4(4), 323–338.
Gavarry, O., Giacomoni, M., Bernard, T., Seymat, M., & Falgairette, G. (2003). Habitual physical activity in children and adolescents during school and free days. Medicine and Science in Sports and Exercise, 35(3), 525–531.
Gilbey, H., & Gilbey, M. (1995). The physical activity of Singapore primary children as estimated by heart rate monitoring. Pediatric Exercise Science, 7, 26–35.
Harrell, J. S., Pearce, P. F., Markland, E. T., Wilson, K., Bradley, C. B., & McMurray, R. G. (2003). Assessing physical activity in adolescents: Common activities of children in 6th–8th grades. Journal of The American Academy of Nurse Practitioners, 15(4), 170–178.
Hawkins, B. A. (1991). Autism. In D. R. Austin, & M .E. Crawford (Eds.), Therapeutic recreation: An introduction (pp. 138–162). Upper Saddle River, NJ: Prentice-Hall, Inc.
Houston-Wilson, C., & Lieberman, L. J. (2003). Strategies for teaching students with autism in physical education. The Journal of Physical Education, Recreation, & Dance, 74(6), 40–44.
Huang, Y. C., & Malina, R. M. (1996). Physical activity and correlates of estimated energy expenditure in Taiwanese adolescents 12–14 years of age. American Journal of Human Biology, 8, 225–236.
Kann, L., Warren, W., & Harris, W. A. (1999). Youth risk behavior surveillance–United States, 1995. Journal of School Health, 66, 365–377.
Kohl, H. W., Fulton, J. E., & Caspersen, C. J. (2000). Assessment of physical activity among children and adolescents: A review and synthesis. Preventive Medicine, 31, S54–S76.
Levinson, L., & Reid, G. (1991). Patterns of physical activity among youngsters with developmental disabilities. Canadian Association for Health, Physical Education, and Recreation, 56, 24–28.
Llewellyn, A., & Hogan, K. (2000). The use and abuse of models of disability. Disability & Society, 15(1), 157–165.
Longmuir, P. E., & Bar-Or, O. (2000). Factors influencing the physical activity levels of youths with physical and sensory disabilities. Adapted Physical Activity Quarterly, 17, 40–53.
McKenzie, T. L., Marshall, S. J., Sallis, J. F., & Conway, T. L. (2000). Student activity levels, lesson context, and teacher behavior during middle school physical education. Research Quarterly for Exercise and Sport, 71, 249–259.
Mota, J., Santos, P., Guerra, S., Ribeiro, J. C., & Duarte, J. A. (2003). Patterns of daily physical activity during school days in children and adolescents. American Journal of Human Biology, 15, 547–553.
Oliver, M. (1996). Understanding disability: From theory to practice. New York: St.Martin’s Press
Orsmond, G. I., Krauss, M. W., & Seltzer, M. M. (2004). Peer relationships and social and recreational activities among adolescents and adults with autism. Journal of Autism and Developmental Disorders, 34(3), 245–256.
Pate, R. R., Baranowski, T., Dowda, M., & Trost, S. G. (1996). Tracking of physical activity in young children. Medicine and Science in Sports and Exercise, 28(1), 92–96.
Reid, G., & O’Connor, J. (2003). The autism spectrum disorders: activity selection, assessment, and program organization: Part II. Palaestra, 19(1), 20–27.
Rosser D. D. (2004). Physical activity patterns of children with autistic spectrum disorders. Unpublished doctoral dissertation, Texas A&M University, College Station.
Rosser, D. D., & Frey, G. C. (2005). Comparisons of physical activity levels between children with and without autistic spectruam disorders. Adapted Physical Activity Quarterly, 22, 146–159.
Sallo, M., & Silla, R. (1997). Physical activity with moderate to vigorous intensity in preschool and first-grade schoolchildren. Pediatric Exercise Science, 9, 44–54.
Scahill, L., & Koenig, K. (1999). Pharmacotherapy in children and adolescents with pervasive developmental disorders. Journal of Child & Adolescent Psychiatric Nursing, 12(1), 41–43.
Strauss, R. S., Rodzilsky, D., Burack, G., & Colin, M. (2001). Psychosocial correlates of physical activity in healthy children. Archives of Pediatrics & Adolescent Medicine, 155(8), 897–902.
Suzuki, M., Saitch, S., Tasaki, Y., Shimomura, Y., Makishima, R., & Hosoy, N. (1991). Nutritional status and daily physical activity of handicapped students in Tokyo metropolitan schools for deaf, blind, mentally retarded and physically handicapped individuals. American Journal of Clinical Nutrition, 54, 1101–1111.
Taylor, W. C., Baranowski, T., & Sallis, J. F. (1994). Family determinants of childhood physical activity: A social-cognitive model. In R. K. Dishman (Ed.), Advances in exercise adherence (pp. 319–342). Champaign, IL: Human Kinetics.
Trost, S. G., Pate, R. R., Freedson, P. S., Sallis, J. F., & Taylor, W. C. (2000). Using objective physical activity measures with youth: How many days of monitoring are needed? Medicine and Science in Sports and Exercise, 32(2), 426–431.
Trost, S. G., Pate, R. R., Sallis, J. F., Freedson, P. S., Taylor, W. C., Dowda, M., et al. (2002). Age and gender differences in objectively measured physical activity in youth. Medicine and Science in Sports and Exercise, 34(2), 350–355.
Trost S. G., Ward D. S., Moorehead S. M., Watson P. D., Riner W., & Burke, J. R. (1998). Validity of the computer science and applications (CSA) activity monitor in children. Medicine & Science in Sports & Exercise, 30, 629–633.
U.S. Department of Health, Human Services. (2000). Healthy people 2010: Understanding and improving health. (2nd ed.). Washington, DC: U.S. Government Printing Office.
U.S. Department of Health and Human Services. (2002). Healthy people 2010: Physical activity and fitness. Retrieved March 29, 2002, from http://www.health.gov/healthypeople/Document/HTML/Volume2/22Physical.htm.
Acknowledgments
This research received support from the Indiana University Graduate School Research Grant program, School of Health, Physical Education, Recreation, and Dance Research Grant-In-Aid, and The AAU/Bell-Updyke-Willett Kinesiology Research Fund. We would like to express our gratitude to all participants for their support in this study. Additional gratitude is extended to Mr. Hongwei Guan and Dr. Hal Morris (deceased) for their valuable technical assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pan, CY., Frey, G.C. Physical Activity Patterns in Youth with Autism Spectrum Disorders. J Autism Dev Disord 36, 597–606 (2006). https://doi.org/10.1007/s10803-006-0101-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10803-006-0101-6