Abstract
This chapter reviews existing and ongoing research related to the use of transcranial direct current stimulation (tDCS) as a potential cognitive enhancement intervention in cognitively impaired individuals across a range of neurodegenerative diseases including Alzheimer’s type dementia (DAT), Parkinson’s disease dementia (PDD) or dementia with Lewy bodies (DLB), frontotemporal dementia – behavioral variant (bvFTD), and primary progressive aphasia (PPA). Methodological information, including treatment montage and session structure, efficacy/outcome, and other tDCS related details are provided for each study. While still relatively early in the clinical translation phase, tDCS appears to hold some promise in these clinical samples but considerably more work is needed to identify optimal treatment parameters as well as how these may be affected by disease severity.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Dementia , defined as subjective and objective cognitive and behavioral deficits that disrupt functioning (e.g., social, occupational) and represents a significant decline from previous level of functioning, constitutes a significant healthcare burden in middle and older aged adults. In a recent population-based sample of 856 American older adults drawn from the Health and Retirement Study, 13.9% of individuals over the age of 70 met criteria for dementia (Plassman et al. 2007). Global estimates of dementia range from 5% to 7% in most regions, with a significantly higher prevalence of 8.5% in Latin America and lower prevalence of 2–4% in sub-Saharan Africa (Prince et al. 2013). Rates of dementia diagnosis are also growing exponentially, with an estimated 115.4 million individuals worldwide expected to meet criteria by the year 2050 (Prince et al. 2013). The costs of dementia are notable; compared to individuals with heart disease, cancer, or other medical causes, individuals with dementia spend significantly more towards healthcare in their final 5 years of life, averaging $287,038 (Kelley et al. 2015). Among the neurodegenerative diseases, Alzheimer’s disease, Parkinson’s disease dementia, Lewy Body dementia, and frontotemporal dementia, make up the vast majority. Although grouped together under the general concept of dementia, there are important differences in the underlying etiologies that result in unique patterns of neuropsychological, behavioral/emotional, and functional disturbance. This chapter aims to provide a brief summary of each of the neurodegenerative dementias, accompanied by a review of the existing literature on the use of transcranial direct current stimulation (tDCS) as an intervention for the associated behavioral and cognitive sequelae.
Alzheimer’s Disease
Clinical Criteria
Among neurodegenerative dementias, dementia – Alzheimer’s type (DAT) or Alzheimer’s disease (AD) is the most common, occurring in 5.4 million Americans and one-in-nine U.S. adults aged 65 years or older (Alzheimer’s Association 2016). Alzheimer’s disease is characterized by a prominent memory impairment for recent information and events, most often experienced as forgetfulness in everyday life (Welsh-Bohmer and Warren 2006). Although histological confirmation is the gold standard for validating dementia subtype diagnosis, increased knowledge of AD-specific biomarkers (McKhann et al. 2011) and more robust measurement of cognitive impairment (Edmonds et al. 2015) have resulted in improved clinical criteria for diagnosing and staging AD (McKhann et al. 2011). A diagnosis of probable DAT requires evidence of an insidious onset, subjective decline, and a pattern of cognitive deficits not better accounted for by another dementia. While the “amnestic” (involving memory) subtype is most common, DAT can also manifest as primary dysfunction in the language, visuospatial, or executive domain (McKhann et al. 2011).
Neuropathology
The cardinal neuropathological characteristics of DAT include neurofibrillary tangles and senile beta-amyloid plaques that are ultimately accompanied by marked synaptic damage and neuronal loss. Neurofibrillary tangles (NFTs) are abnormal fibrous inclusions consisting primarily of hyper-phosphorylated tau protein, found within the perikaryal cytoplasm of pyramidal cells (Perl 2010; Serrano-Pozo et al. 2011). Although NFTs are present in other neuropathological processes (e.g., postencephalitic parkinsonism, cognitive impairment after brain injury, amyotrophic lateral sclerosis), DAT is marked by a characteristic distribution of NFTs that begins in the transentorhinal (perirhinal, entorhinal) cortex of the medial temporal lobes. NFT distribution generally then progresses into the CA1 and subicular subregions of the hippocampus, followed by the deep layers of the neocortex, and finally affect the primary motor and somatosensory cortices during the final disease stages (Perl 2010; Serrano-Pozo et al. 2011). The other characteristic pathology is dense-core beta amyloid plaques, which consist of extracellular deposits with a core of amyloid beta (Aβ) surrounded by dystrophic neuritis (Serrano-Pozo et al. 2011). In contrast to NFTs, Aβ plaques are initially distributed in the basal portions of the frontal, temporal, and parietal/occipital lobes (Stage A), then in all isocortical association areas with minimal deposition in the hippocampi and primary sensory, motor, and visual cortex (Stage B), and finally in all areas of the isocortex, as well as some subcortical regions (Stage C; Braak and Braak 1991). Amyloid angiopathy in the leptomeningeal arteries and small arteries and vessels of the posterior cortex is also evident in approximately 80% of adults with DAT. As may be expected by the distribution of the above pathologies, DAT is marked by synaptic loss in the limbic system, neocortex, and basal forebrain (Serrano-Pozo et al. 2011) through early damage to synapses and retrograde degeneration of the axons and dendritic trees.
Neuropsychological Profile
The precise pattern of neuropsychological deficit often depends on the time at which patients present for evaluation, with more advanced patients demonstrating greater and more pervasive cognitive deficits (see Welsh-Bohmer and Warren 2006). The general consensus is that decline in the ability to learn and remember new information (i.e. declarative or episodic memory) is an early characteristic feature of DAT. Deficient learning is often detectable via a relatively flat learning curve across multiple presentation trials. Recall of recently learned information (i.e., memory) is poor and generally unaided via enhanced structure or cueing on recognition measures. Semantic memory tends to be preserved in early stages of the disease, with gradual decline corresponding to disease progression. Although simple attention is preserved, working memory (i.e., the ability to mentally hold and manipulate information) is variably deficient. Patients with DAT also demonstrate deficits in executive functioning, specifically in problem solving, abstract reasoning, inhibition, and mental flexibility. Language deficits are also common; in particular, word-finding and confrontation naming difficulties, reduced fluency and difficulty comprehending complex information are experienced. With the exception of posterior onset variants of DAT, visuospatial abilities are preserved early in the disease course but gradually decline.
tDCS in DAT
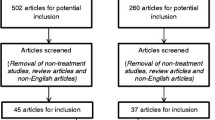
Given the pattern of deficits, a wide range of neocortical and cognitive targets could be considered when developing tDCS research. To date, we are not aware of any studies that have explicitly examined disease severity; rather, existing research has examined effects at the group level. A summary of published studies assessing effectiveness of tDCS for the treatment of cognitive impairments in DAT is provided in Table 16.1. As described below, tDCS has shown neuro-enhancing effects on multiple cognitive abilities on both short- and long-term bases, which are organized based on the targeted cognitive domain.
General Cognitive Functioning
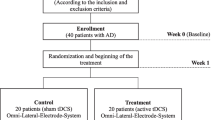
In one of the largest completed clinical trials of tDCS efficacy in DAT, Khedr and colleagues (2014) demonstrated the impact of tDCS on general cognitive and intellectual functioning in a sample of 34 patients. The study utilized 10 consecutive daily sessions of 25 min of 2 mA active (anode vs. cathode placed over target) or sham stimulation over the left dorsolateral prefrontal cortex (DLPFC; 6 cm anterior to M1) plus 2 months of maintenance on memantine. Outcomes on a range of cognitive tasks (MMSE and subtests of the Wechsler Adult Intelligence Scale – Third Edition (WAIS-III) as well as neurophysiological changes in EEG were evaluated directly after the last session and at one- and two-month follow-up. Results indicated that, relative to sham, active stimulation resulted in a gain of approximately two points immediately and an additional one point after one- and two-months on the MMSE. In contrast, only cathodal stimulation over this area augmented performance IQ scores on the WAIS-III (Khedr et al. 2014). The reasons for these changes are unclear, especially given the potential hyperpolarizing effect of stimulation under the cathode electrode on neural soma, but the authors posited that active stimulation of either polarity engaged remaining “cognitive reserve.” Prior findings of “excitatory” effects under the cathode at 2 mA have been reported in the motor cortex (Batsikadze et al. 2013; Wiethoff et al. 2014) and may support the authors’ posited explanation for their findings.
Other studies assessing global cognitive change have been less positive and reported no effect of tDCS over the left DLPFC (Suemoto et al. 2014) or left temporal lobe (Boggio et al. 2012). Suemoto and colleagues (2014) found no differences on the MMSE and the Alzheimer’s Disease Assessment Scale – Cognitive subscale (ADAS-Cog) in 40 AD patients who received six 20-min sessions of 2 mA sham or active (anode) tDCS over the left DLPFC. Boggio and colleagues (2012) utilized a double-blind crossover design in which 15 DAT patients received either repeated sham or active tDCS at 2 mA for 30 min per day, for five consecutive days. All participants completed both active and sham conditions, with several weeks in between each set of sessions. Dual anode electrodes were placed over the bilateral temporal lobes (T3 and T4) with the cathode placed noncephalically on the participants’ right arm. Participants demonstrated no change in global cognition, as measured by the MMSE and ADAS-Cog, after either set of sessions.
Overall then, there is little evidence that tDCS enhances global cognitive functioning, though several potential explanations exist for this finding. Critically, the stimulation montage should target the functional neuroanatomy of the targeted cognitive abilities. In this sense, global screening measures like the MMSE and ADAS-Cog may be too gross of tools to evaluate change in more selected brain regions/networks. As suggested below, there is some evidence that tDCS can enhance specific cognitive abilities as measured by more sensitive tasks. Additionally, the stimulation dose may have been insufficient to induce change at this global level. In this sense, the results of Khedr and colleagues (2014) are intriguing as they raise the possibility that tDCS may augment pharmacologic effects.
Memory
Several studies have demonstrated the beneficial effects of tDCS on memory using montages that targeted the frontal, parietal, and/or temporal lobes. Boggio and colleagues (2009) examined the memory performance of 10 DAT patients after a single 30-min session in which the anode was placed over either the left DLPFC (F3) or left temporal lobe (T3). Both locations resulted in improved visual recognition memory for animals, people, and objects when evaluated during stimulation (i.e., online task performance). Conversely, there was no effect on working memory (Digit Span subtest from the WAIS) or selective attention/inhibition (Stroop Color Word Test). The same group later reported enhanced visual recognition memory, which persisted at a 1 month follow-up after five consecutive daily 30-min sessions of 2 mA stimulation when the anode was placed over the bilateral temporal lobes (T3 & T4; cathode on right shoulder), relative to sham stimulation (Boggio et al. 2012).
Similar positive effects have been reported with verbal memory. In a double-blind randomized crossover design, Ferrucci et al. (2008) compared the effects of single 15-min sessions of anodal current, cathodal current, and sham stimulation on word recognition and visual attention in 10 DAT patients. This study used a bitemporal target location (P3-T5 and P6-T4) with non-cephalic placement of the other electrodes on the right shoulder, which was accomplished using dual tDCS units to each administer 1.5 mA. Placing the anodes over the target location significantly increased word recognition memory, whereas performance declined when cathodes were placed over the target location and remained stable following sham. These general results were recently replicated by Marceglia and colleagues (2016), who utilized the same study design and montage. In addition to demonstrating the enhancing effects of placing the anode, but not the cathode, over the targeted region on word recognition, the authors evaluated the neurophysiological effects of stimulation by electroencephalography (EEG). Patients with DAT generally demonstrate higher low-frequency theta oscillations in the temporoparietal cortex, a finding associated with poorer encoding in the hippocampal-cortical loops. Furthermore, DAT is associated with lower high-frequency alpha and beta oscillations in the frontal and temporoparietal cortex that underlies poorer search and retrieval of information. Marceglia and colleagues (2016) demonstrated that anodal tDCS specifically increased high-frequency alpha and beta oscillations in the temporoparietal area on EEG completed 30-min post-stimulation and posited that this effect drove the previously noted word recognition improvement (Marceglia et al. 2016).
tDCS may also have positive effects on verbal memory in early onset Alzheimer’s disease, a diagnosis given when the patient meets criteria for DAT before age 65, likely due to a genetic mutation. In a case study of early onset DAT, Bystad et al. (2016) administered 2.0 mA stimulation with the anode over the left temporal lobe (T3) for 12 (2 per day over 6 days), 30-min sessions. Primary outcomes included neuropsychological testing and EEG monitoring with data acquired at baseline, 2 days after the last stimulation session, and again at a two-month follow-up. The participant exhibited a statistically significant improvement in delayed verbal recall at both post-stimulation time points. EEG was re-evaluated only at 2 months but there were no significant changes relative to baseline. These findings highlight a potentially interesting dichotomy between the behaviors/cognitive functions of interest and the underlying neurophysiology but also suggest that such measures need to be consistently paired across evaluation time points.
Thus, placing the anode over the temporal lobe(s) appears to consistently enhance memory performance in patients with DAT with the effects of multiple daily sessions persist for a month or more. These findings highlight the importance of aligning the disease process (e.g., temporal lobes in DAT), cognitive abilities (e.g., memory), and stimulation montage (e.g., targeting the temporal cortex). However, considerably more work is needed to clarify dose-response relationships and the neurophysiological changes mediating the behavioral effects.
Attention
The previously described study by Ferrucci and colleagues (2008) also evaluated visual attention, given the vital contribution of the parietal lobes in this process. However, there were no effects of either tDCS polarity relative to sham. Ferrucci and colleagues attributed this lack of effect to two hypotheses: (a) that the visual attention system required for task performance is too complex to be affected by a single session of stimulation, and (b) that the particular montage utilized in the study failed to sufficiently stimulate posterior parietal regions implicated in visual attention. It is also reasonable to consider a lack of task sensitivity and inappropriate target location to these potential explanations. Thus, the attentional system is clearly an understudied target for tDCS in those with dementia.
Neuropsychiatric Symptoms
The cognitive sequelae of DAT are often accompanied by a constellation of neuropsychiatric symptoms that include mood disorders, apathy, social isolation, and “personality” changes associated with impulsivity or reduced inhibitory control. Currently, only one study has assessed the impact of tDCS on such symptoms. Suemoto and colleagues (2014) evaluated the effect of six sessions of sham or 1.5 mA stimulation where the anode was over the left DLPFC (10/20 location not listed) on apathy, depression, caregiver burden, and other neuropsychiatric symptoms in a sample of 40 moderate DAT patients. There was some general improvement in mood over the two-week period that was comparable in those receiving active and sham tDCS. Therefore, while tDCS has shown promise in treating symptoms of mood and anxiety disorders (Tortella et al. 2015), additional work is clearly needed to evaluate whether this promise extends to those with DAT (or other forms of dementia). As with all studies, the inclusion criteria for both patients and caregivers should be carefully evaluated to ensure sufficient symptoms.
Overall, tDCS shows promise for the treatment of the primary cognitive deficit in DAT patients: memory. In contrast, the few existing studies of tDCS targeting attention, working memory, and neuropsychiatric symptoms have found no significant effect. These conclusions should be viewed as preliminary given the relatively small number of studies in DAT in general. Additional targets, montages, and doses should be investigated in the future. Pharmacologic trials have recently begun investigating efficacy in earlier disease stages given the limited effects in more advanced DAT stages. Thus, it is also possible that tDCS would have optimal effects if implemented earlier in the disease course, such as during the clinical precursor stage of mild cognitive impairment (MCI).
Mild Cognitive Impairment
Clinical Criteria
The transitional phase of MCI offers an ideal point in which treatments that enhance or prolong cognitive functioning can be administered, though we have previously discussed several methodological challenges in this regard (Hampstead et al. 2014). For the purpose of this chapter, the term MCI will be used in reference to the clinical precursor phase of DAT. In 2011, a workgroup commissioned by the National Institute on Aging and Alzheimer’s Association published updated criteria defining MCI due to DAT (Albert et al. 2011) in order to facilitate the early identification of the conversion from cognitively asymptomatic to symptomatic. These revised criteria include (a) subjective report of cognitive decline via the patient, an informant, or skilled clinician, (b) objective evidence of impairment beyond expectations for the patient’s age and educational attainment in at least one cognitive domain and, (c) preserved functional independence (Albert et al. 2011). Recognizing that multiple medical conditions could result in the above cognitive phenotype, the criteria also specify that a diagnosis of MCI is inappropriate if symptoms arise from a different underlying pathophysiologic process (e.g., traumatic brain injury) or a different neurodegenerative dementia.
Neuropathology
The above noted clinical criteria were accompanied by a list of potential biomarkers that may inform etiology and prognosis of MCI due to DAT (Albert et al. 2011). These biomarkers closely mirror the known neuropathology in AD, including amyloid beta (Aβ) levels in the cerebrospinal fluid, positron emission tomography (PET) scanning with ligands to detect fibrillar Aβ, hippocampal volume loss, or glucose hypometabolism and hypoperfusion in the posterior temporal and parietal cortex via PET and single positron emission computerized tomography (SPECT) imaging. The presumed temporal order of DAT biomarker progression (i.e., Stage 1: cerebral amyloid accumulation; Stage 2: neurodegeneration; Stage 3 subtle cognitive decline Sperling et al. 2011) has recently been challenged (Edmonds et al. 2015) but may be a critical factor to consider as it relates to tDCS efficacy.
Neuropsychological Performance
As with DAT, the severity and extent of cognitive impairment varies as a function of when individuals present clinically. Impairments generally parallel those seen in DAT. Patients with MCI due to DAT most often demonstrate impairments in memory (i.e., amnestic MCI) but may also have difficulty with aspects of language or executive functioning. Patients may also demonstrate impairments across multiple domains, particularly as they are advancing towards a DAT diagnosis.
tDCS in MCI
To date, only one randomized controlled trial has been published using tDCS in patients with MCI due to DAT. Meinzer et al. (2015) utilized a randomized double-blind crossover design to evaluate the effects of a single 20-min session of 1 mA stimulation where the anode was placed over the left lateral PFC. During each session, participants performed a semantic word retrieval task during stimulation (or sham) while undergoing fMRI (note that resting state fMRI was also acquired; Meinzer et al. 2013). Active, but not sham, stimulation enhanced patient performance to levels comparable to those of healthy older adults who took part in an earlier study (Meinzer et al. 2013). These behavioral findings were reflected by the fMRI data where bilateral PFC hyperactivation during sham tDCS was significantly reduced after active tDCS to levels comparable to those of healthy older adults. These changes were not only evident in the PFC, but also the left basal ganglia and thalamus and right middle temporal gyrus. The authors interpreted these findings as evidence of increased neural efficiency and top-down control of task performance (Meinzer et al. 2015); a pattern that fits with a “restorative” model of tDCS effects.
Additional studies of the impact of tDCS on behavior and functional activity in MCI are ongoing. Cheng and colleagues (2015) have published the protocol for a randomized double-blind study that compares three intervention conditions: sham tDCS plus adaptive N-back cognitive training, active tDCS plus adaptive N-back training, and active tDCS plus general cognitive training. The proposed montage utilizes 35cm2 pad anode electrodes placed over the temporal lobes (T3 & T4), with a 35cm2 pad cathode placed on the right deltoid muscle. Each group will undergo 4 weeks of three training sessions per week, with primary outcome measures of working memory (Adaptive N-back task performance) and general cognitive functioning (Alzheimer’s Disease Assessment Scale – Cognitive subscale; ADAS-Cog) assessed at baseline and at 5 min post-stimulation during the fourth, eighth, and twelfth week sessions. Additional measures of language, memory, and neuropsychiatric symptoms will be assessed at baseline and after stimulation at week four, eight, and 12 to determine if tDCS and/or either cognitive training modality demonstrate far transfer effects.
We are currently performing a 2 (active vs. sham HD-tDCS) × 2 (mnemonic strategy training vs. autobiographical memory recall) double blind RCT in patients with MCI (NCT02155946). This trial builds on our earlier work that found mnemonic strategies not only enhanced long-term retention of learned information but were also accompanied by increased activation in the lateral PFC and other memory network regions in those with MCI (e.g., Hampstead et al. 2008, 2011, 2012a, b). However, two problems emerged in our earlier studies: (1) not all patients benefitted from mnemonic strategy training and (2) patients had difficulty transferring the skills to novel types of information. Thus, our ongoing study targets the lateral PFC using HD-tDCS (center anode at F5) in order to enhance the neuroplasticity of the network of interest and then capitalize on this process by pairing stimulation with mnemonic strategy training. Participants are randomized to active or sham HD-tDCS and to either mnemonic strategy training or the active control condition of autobiographical recall (analogous to reminiscence therapy). The four resulting groups are run in parallel. Participants complete baseline cognitive testing and fMRI during both task- and resting-state, followed by five consecutive daily training in which HD-tDCS (2 mA for 30 min) is performed concurrent with training. Cognitive and fMRI outcome measures are performed 3–4 days after the final stimulation session and again at 3-months. The primary outcome measures are ecologically relevant memory tasks (face-name and object-location associations) while secondary outcome measures include self-report of memory change (via the Multifactorial Memory Questionnaire) and objective evidence of near- and far-transfer (route memory and medical instructions from the Ecological Memory Simulations).
Parkinson’s Disease Dementia
Clinical Characteristics
Parkinson’s disease (PD) is the second most common neurodegenerative disease after DAT (de Lau and Breteler 2006). While diagnostic confirmation is performed post-mortem, probable PD requires the presence of two of the following symptoms: resting tremor, bradykinesia, rigidity or postural imbalance (Litvan et al. 2003). Symptoms typically have an asymmetric onset and are responsive to medications such as levodopa (Litvan et al. 2003). For cases in which cognitive impairments significantly interfere with instrumental activities of daily living (beyond the disturbance caused by motor symptoms), Parkinson’s disease dementia (PDD) is diagnosed. The prevalence of PDD varies; however, it is estimated that between 26% and 28% of newly diagnosed PD patients develop PDD in the three-to-five years after initial diagnosis (Reid et al. 1996).
Neuropathology
PD is characterized by degeneration of dopaminergic neurons in the substantia nigra (Lehéricy et al. 2012). PDD and dementia with Lewy Bodies (DLB) share the underlying neuropathology of accumulation of alpha-synuclein embedded in Lewy bodies (Yousuf and Daniyal 2012), but differ in the clinical presentation (i.e., DLB has onset of cognitive impairments before motor symptoms). There is associated atrophy of the cerebral grey matter in bilateral frontal and temporal lobes in patients with PDD but the medial temporal lobes are generally intact relative to DAT (Burton et al. 2004).
Neuropsychological Profile
Early cognitive changes in PD are associated with dysfunction in frontostriatal and dopaminergic systems (Kehagia et al. 2010) with cognitive impairment developing in 20% to 57% of patients in three-to-five years after diagnosis (Kehagia et al. 2010). The neuropsychological profile in PD includes executive dysfunction, as evidenced by impairments in executive abilities like working memory, cognitive flexibility, response inhibition and attention (Kehagia et al. 2010). These abilities are generally believed mediated by the dorsolateral prefrontal cortex (DLPFC) and associated subcortical circuits. As the disease progresses to non-dopaminergic neuronal systems, cognitive dysfunction may develop in visuospatial abilities, memory, and verbal fluency (Kehagia et al. 2010).
Medication management, such as dopaminergic agonists or levodopa, is the first line of treatment for PD symptoms given its ability to enhance dopamine availability. Such dopaminergic enhancement can improve executive functioning and is accompanied by increased bloodflow to the DLPFC (Cools et al. 2002). However, levodopa has a range of side effects (see Boravac 2016) and generally becomes less effective with disease progression (Advokat et al. 2014). Deep brain stimulation (DBS) has promising effects for treating PD motor symptoms as it provides direct electrical stimulation to the ventral intermediate nucleus, subthalamic nucleus, or the internal segment of the globus pallidus (Perlmutter and Mink 2006). Thus, there is precedent for the success of electrical stimulation in PD using invasive methods; a critical question is whether the weak electric currents associated with non-invasive in tDCS are sufficient to mitigate motor or cognitive impairment.
tDCS in Parkinson’s Disease
Improvements in motor symptoms have been found when the anode is placed over motor cortical regions (Benninger et al. 2015; Kaski et al. 2014) or the cerebellum (Ferrucci et al. 2015). However, this chapter focuses on cognitive changes associated with tDCS, a summary of which can be found in Table 16.2. Eleven studies have examined tDCS in PD, and only one study of other related Parkinsonism dementias (i.e., corticobasal syndrome). Of the 11 studies in PD, six have targeted cognition and five of these applied tDCS to the DLPFC as a method of enhancing executive functioning. These studies implemented slight variations in anode placement; three studies used F3 or F4, one study placed it halfway between F3/F4 and F7/F8, and one study did not specify the location. Regarding dose, current intensity at 1–2 mA, session duration was in the typical 20–25 min range for between one and 16 sessions. As with DAT, there is insufficient data to guide dose-response relationships. Only one of the studies measures outcomes online (Boggio et al. 2006) while the remainder tested participants offline and immediately following stimulation and up to a 16-week follow-up (Biundo et al. 2015). We discuss the efficacy of these studies below based on cognitive domain.
Executive Functioning
In one of the first tDCS studies in PD, Boggio and colleagues (2006) compared the effect of 1 mA, 2 mA, and sham stimulation with anode placement over the left DLPFC (F3) on n-back working memory task performance. Whereas no changes in 3-back performance were observed after sham or 1 mA of stimulation, 2 mA stimulation significantly increased accuracy. Critically, performance was unchanged when the anode was placed over M1. Together, these results highlight the importance of both stimulation location and electrical current intensity for tDCS efficacy in PD.
Pereira and colleagues (2013) used a randomized cross-over design with 2.0 mA stimulation where the anode was over the left DLPFC (F3) or left temporo-parietal cortex (P3-T5). Participants completed semantic and phonemic fluency tasks during fMRI immediately after stimulation. All participants completed both stimulation locations, which were counterbalanced and separated by a 2 h break. The results revealed significant improvements in phonemic fluency compared to baseline in both conditions. Functional neuroimaging during the tasks demonstrated increased connectivity in the frontal, parietal, and fusiform areas, which are associated with verbal fluency tasks in the DLPFC condition, but not the left temporo-parietal condition. The study completed both stimulations on the same day (2 h apart), which may have confounded the active tDCS results; however, the researchers questioned whether a single session of stimulation would have realistically have persisting effects over this time period.
Doruk and colleagues (2014) used a double-blind randomized procedure in which 18 PD patients received stimulation with either the anode over the left DLPFC (F3), the right DLPFC (F4), or sham. Each group completed ten 20-min sessions over two consecutive weeks (5 sessions per week). The participants completed a variety of executive functioning neuropsychological tasks before stimulation, post-stimulation, and at 1-month follow-up, including the Trail-Making Tests A & B (TMT), Wisconsin Card Sorting Task (WCST), Probabilistic Classification Learning (PCL), Working Memory (WM) Test, and the Stroop Color-Word Test. All groups demonstrated significant improvement on TMT-B immediately after the 10 sessions, which suggests general practice effects. However, these gains persisted at 1 month only in participants who received active stimulation over the DLPFC – regardless of hemisphere. There were no significant changes in any other cognitive measure. While these findings suggest some delayed benefits on select cognitive abilities, they may represent a spurious finding related to multiple comparisons and limited statistical power; therefore, replication is critical for validating these effects.
Manenti and colleagues (2016) examined the synergistic effects of physical therapy and tDCS in 20 patients with cognitive impairment associated with PD, examining both motor and cognitive outcomes. Since there is generally an asymmetric symptom presentation in PD, patients were randomized into active or sham groups using a covariate adaptive method based on age and side of motor symptoms. Specifically, the anode was placed over the DLPFC (8 cm frontally and 6 cm laterally from the scalp vertex) contralateral to the individual’s most affected limb. Each group completed ten 25-min sessions over 2 weeks (five consecutive days per week) while completing physical therapy exercises. Relative to sham, active stimulation resulted in significant post-treatment improvement on the Parkinson’s Disease Cognitive Rating Scale (PD-CRS), semantic fluency, and TMT-B tasks. Impressively, PD-CRS and semantic fluency gains persisted at a three-month follow-up.
Learning and Memory
A single study has evaluated the effects of tDCS on learning and memory in PD patients. Biundo and colleagues (2015) compared 4 weeks (16 total sessions) of concurrent computer-based cognitive training and active or sham tDCS with anode placement over the left DLPFC (F3) in 24 PD patients with memory deficits. Neuropsychological tests (e.g., Montreal Cognitive Assessment; Repeatable Battery for the Assessment of Neuropsychological Status [RBANS]) were administered at baseline, following the 4-week treatment, and at a 16-week follow-up. The active tDCS group showed significantly worse performance on a measure of psychomotor processing speed immediately post-training relative to sham but performances were comparable at 16 weeks. There were no statistically significant beneficial effects of active tDCS. However, there were encouraging trends at the follow-up wherein medium to large effect sizes suggested beneficial effects of active tDCS on the Story Learning subtest (p = 0.077; Cohen’s d = 0.9) and Immediate Memory Index (p = 0.075; Cohen’s d = 0.7) of the RBANS. Thus, additional work is clearly needed to determine whether these promising effect sizes represent actual improvement.
Corticobasal Syndrome
Corticobasal syndrome (CBS) is a neurodegenerative process characterized by insidious onset of stiffness, dystonia, and clumsiness resistant to levodopa treatment (Armstrong et al. 2013). Characteristic clinical presentation includes asymmetric onset of motor symptoms, “alien limb” syndrome, and apraxia (Boeve 2011). CBS is a collection of symptoms that are generally associated with corticobasal degeneration (CBD), a Parkinson’s plus syndrome; however, neuropathological studies have revealed that CBS is non-specific to CBD, but can be found in Alzheimer’s disease, progressive supranuclear palsy, and frontotemporal lobar degeneration (Lee et al. 2011). As levodopa is not efficacious in treating CBS, and genetic or neuropathological substrates for treatment have not been defined, tDCS may present an option for managing the symptoms of CBS.
tDCS in CBS
To date, only one study has examined tDCS as an intervention in CBS. Bianchi and colleagues (2015) used a double-blind randomized, sham-controlled crossover design with 14 individuals with bilateral or asymmetric limb apraxia and possible CBS. Seven min of 2.0 mA stimulation was administered with the anode over the right (about halfway between P4 and P8) or left parietal cortex (about halfway between P3 and P7) and the cathode on the contralateral deltoid muscle. Each participant completed the three conditions over 2 days (i.e., sham, then active condition on 1 day; active condition on another day). The results revealed a significant improvement in ideomotor praxis following stimulation over the left parietal cortex. No significant changes in praxis were found following sham stimulation or stimulation over the right parietal cortex. The findings provide interesting preliminary evidence that builds on decades of functional neuroanatomic work linking the left parietal cortex and ideomotor apraxia; however, larger and more homogenous samples are required to verify these findings and the clinical application of tDCS in this population.
Frontotemporal Dementia
Clinical Characteristics
Frontotemporal dementia (FTD) is a heterogeneous group of disorders characterized by progressive neurodegeneration of the frontal and temporal lobes (Bott et al. 2014). Age of onset is typically younger than other dementias with the average most commonly between 50 and 60 years old (Saykin and Rabin 2014). Approximately half of all FTD cases are behavioral variant (bvFTD), which is characterized by early changes in personality and impaired social functioning (Bott et al. 2014). In bvFTD there is focal atrophy bilaterally in the frontal lobes (Bott et al. 2014). The remaining half of FTD cases are classified as subtypes of primary progressive aphasia (PPA) and are characterized by focal language deficits (Bott et al. 2014). The semantic variant (svPPA) presents with loss of semantic knowledge and associated atrophy in the anterior temporal lobes bilaterally (Bott et al. 2014). The nonfluent variant/agrammatic (nfvPPA or avPPA) presents with motor-speech difficulties and agrammatism with associated atrophy in the left inferior frontal and insular regions (Bott et al. 2014). Logopenic variant (lvPPA) is characterized by slowed speech and frequent word-finding pauses and has cortical atrophy in the left temporoparietal junction area (Gorno-Tempini et al. 2011) (Table 16.3).
tDCS in FTD
Nine studies have examined tDCS effects in FTD, three of which have been case studies. Since there is great heterogeneity in clinical presentations of FTD and associated differential cortical atrophy, the majority of studies have focused on a specific FTD subtypes (i.e., one case study with behavioral variant, four studies with nonfluent PPA, and study study with semantic variant PPA). Three studies combined FTD subtypes; one combined behavioral variant (n = 9) and language variant (n = 1; Huey et al. 2007) and the others combined participants with nonfluent variant and logopenic variant PPA (Gervits et al. 2016; Tsapkini et al. 2014). Given this heterogeneity, tDCS studies have varied greatly in the montages focusing on the left DLPFC (Cotelli et al. 2014, 2016), language cortical areas (crosspoint between T3/P3 and C3/T5 or crosspoint between T3/Fz and F7/Cz; Wang et al. 2013), F7 and F3 (Huey et al. 2007), and on the temporal pole using MRI guidance. The stimulation intensities varied from 1 mA to 2 mA and sessions lasted for 20–25 min. The studies greatly varied in the duration of treatment ranging from single-session to 20 sessions over 4 weeks. With the exception of one study, all outcomes were measured offline and time points ranged from immediately following tDCS to 48 weeks after stimulation.
tDCS in Advanced FTD
Huey and colleagues (2007) used a double-blind sham-controlled design to examine the effects of anodal tDCS in advanced FTD. Ten participants that met criteria for FTD (nine with primarily behavioral symptoms and one with language symptoms) completed one 40-min session with 2 mA stimulation with the anode at F3. No significant differences were found between the active and sham conditions. The authors hypothesized that this lack of effect resulted from the current being impacted by increased CSF secondary to brain atrophy of the targeted region. While reasonable, the authors assumed atrophy to be present and did not confirm its presence using neuroimaging. Equally plausible explanations are the heterogeneity of the group, small sample size, and use of a single session design.
tDCS in bvFTD
A single case study has been performed with tDCS in bvFTD (Agarwal et al. 2016). A female 45-year-old patient diagnosed with probable bvFTD 4 months prior completed a total of ten, 20-min sessions that were administered twice per day (separated by 3 h) over five consecutive days. Stimulation was performed at 2 mA with the anode placed between F3 and FP1 and the cathode placed over the right supraorbital region. The patient demonstrated significant improvements in the FTD Rating Scale and in subjectively observed functional activities (i.e., speech output, cooking, washing clothes). Improvements persisted in follow-up appointments throughout the following 7 months (Agarwal et al. 2016).
tDCS in PPA
Gervits and colleagues (2016) studied the effects of tDCS with the anode placed over the left frontotemporal region (F7) in a case series of six un-blinded participants with PPA (two with nfvPPA, four with lvPPA). Participants received ten, 20-min stimulation sessions at 1.5 mA and were asked to narrate wordless picture books during stimulation. The participants completed a one-to-two hour linguistic assessment that measured a wide range of linguistic abilities that yielded four composite measures (Speech Production, Grammatical Comprehension, Repetition, and Semantic Processing) and one global composite score. Improvements were found in speech production and grammatical comprehension composite scores, and the effects persisted at 3 months; however, without sham control or comparison group, the role of expectation or placebo cannot be quantified.
Tsapkini and colleagues (2014) used a sham-controlled cross-over design with six patients with PPA (two nfvPPA; four lvPPA) to compare the effects of stimulation concurrent with spelling training. Here, the anode was placed over F7 since this area overlies the left inferior frontal gyrus, which is implicated in phoneme-to-grapheme translations. The participants completed 15 sessions (3–5 sessions per week) with a two-month washout period between conditions. The results revealed significant improvements in spelling ability for trained items in both sham and active tDCS; however, untrained item spelling improved only in the active tDCS condition and persisted at two-week and two-month follow-ups (Tsapkini et al. 2014).
A single case study has examined nfvPPA and demonstrated long-lasting language improvements. In a case study using a cross-over sham-controlled design, a 67-year-old nfvPPA patient completed two 20-min sessions of 1.2 mA stimulation where the anode was placed over “Wernicke’s area ” (crosspoint between T3-P3 and C3-T5) in the morning, and over “Broca’s area” (cross point between T3-Fz and F7-Cz) in the afternoon (Wang et al. 2013). The conditions were completed in the following order: Sham1, Active1, Sham2, Active2. The individual demonstrated improvements on the Psycholinguistic Assessment in Chinese Aphasia (PACA), with particular improvement in naming (2/30 items correct at baseline, 11/30 items correct post-stimulation) after the first active stimulation session only. No further gains were demonstrated after the second active condition.
Cotelli and colleagues (2014) used a randomized sham-controlled design to evaluate the effect of tDCS on naming in 16 patients with nfvPPA. Participants completed 10 (five session per week for 2 weeks) 25-min sessions of stimulation with the anode over the left DLPFC (8 cm frontally and 6 cm laterally from vertex) and cathode on the right shoulder. Stimulation was applied during anomia training. No control group was used; instead, pre-post analyses were completed, with naming performance measured at baseline, after the last stimulation session, and at three-month follow-up. Significant naming improvement was found post-intervention and persisted at the three-month follow-up. The authors also examined the impact of structural compromise on naming improvement and found that change in performance on trained object naming was positively correlated with baseline grey matter volume in the left fusiform, left middle temporal, and right inferior temporal gyri. Cotelli and colleagues (2016) later replicated the persistent effect of tDCS in 18 patients with nfvPPA who underwent the same montage, session schedule, and anomia training program. There were significant improvements in naming for both trained and untrained items that persisted at the three-month follow-up. Together, these results suggest that earlier intervention may promote greater benefit from tDCS and that tDCS may pair well with other behavioral interventions for the treatment of nfvPPA. Future studies must include control groups to determine (a) whether improvements can be can attributed to the intervention, as opposed to practice effects, and (b) whether tDCS specifically enhances the positive effects of behavioral interventions, such as anomia training.
Only one study has examined tDCS in svPPA . Teichmann and colleagues (2016) used a double-blind sham-controlled cross-over design to evaluate the effect of stimulation on semantic matching in 12 patients and 15 healthy controls. Participants completed one 20-min stimulation session for each of three montages (2 active; 1 sham). Electrode location was guided by baseline MRI scans that identified: 1) the left temporal pole, over which the anode was placed and stimulation applied in Condition 1, and 2) the right temporal pole, over which the cathode was placed and stimulation applied in Condition 2. Both stimulation conditions improved semantic matching relative to sham but only condition 2 (cathode over the right temporal pole) improved processing speed. While MRI guided electrode placement is atypical in tDCS, these findings provide interesting preliminary evidence that such methods also hold promise in this area of neuromodulation.
Conclusions and Future Directions
In summary, early trials of tDCS (both controlled and uncontrolled) as an intervention for neurodegenerative dementias demonstrate mixed but promising findings without the deleterious side effects of some pharmacological interventions. The efficacy of tDCS varies greatly across dementia subtype and cognitive domain, at least in part due to heterogeneity in study design. To date, no study has systematically varied important study design elements like comparison method (e.g. crossover vs. parallel groups), montage details (e.g., electrode size, placement), electrical current intensity, session schedule (e.g., number, duration, and spacing of sessions), or outcome measurement timing (e.g., online vs. offline measurement). Furthermore, outcome measures varied widely across studies and may not have always been optimally matched to montage or cognitive construct. The gross majority of studies also utilize traditional pad-based approaches to tDCS, with our ongoing RCT being the only study to our knowledge to use the more focal HD-tDCS approach. Such dose-response information is essential for better understanding tDCS effects.
A second potential explanation for the mixed findings relates to the inter-individual variability seen both within and across dementia subtypes. As noted above, neurodegeneration characterizes these conditions and may dramatically affect electrical current flow given evidence that inter-individual variability in skull and brain morphology impacts current density, flow, and localization in even healthy adults (Bikson et al. 2012; Datta et al. 2012). Thus, the traditional use of the 10/20 system may be insufficient even for tDCS targeting. Computational modeling and, possibly, MRI guided electrode placement may allow for more individualized montages that optimize results.
Finally, most published studies and clinical trials using tDCS for dementia have small and often heterogeneous samples comprised of patients with varying neuropathological burden and neuropsychological deficits. Larger trials are needed to elucidate whether a ‘critical period’ of maximal benefit from tDCS exists for healthy adults and those with cognitive impairment. Despite these limitations, tDCS offers a cost-effective, safe, and well-tolerated option that warrants further study.
References
Advokat, C. D., Comaty, J. E., & Julien, R. M. (2014). Julien’s primer of drug action. New York, NY: Worth Publishers.
Agarwal, S. M., Rajur, S., Bose, A., Shenoy, S., Miriyala, S., Shivakkumar, V., & Venkatasubramanian, G. (2016). Use of transcranial direct current stimulation (tDCS) in a woman with behavioral variant fronto-temporal dementia. Asian Journal of Psychiatry, 21, 31–32.
Albert, M. S., DeKosky, S. T., Dickson, D., Dubois, B., Feldman, H. H., Fox, B. C., … Phelps, C. H. (2011). The diagnosis of mild cognitive impairment due to Alzheimer’s disease: Recommendations for the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimer’s Dementia, 7(3), 270–279.
Alzheimer’s Association. (2016). 2016 Alzheimer’s disease facts and figures. Alzheimer’s & Dementia, 12(4), 1–84.
Armstrong, M. J., Litvan, I., Lang, A. E., Bak, T. H., Bhatia, K. P., Borroni, B., … Winer, W. J. (2013). Criteria for the diagnosis of corticobasal degeneration. Neurology, 80(5), 496–503.
Batsikadze, G., Moliadze, V., Paulus, W., Kuo, M. F., & Nitsche, M. A. (2013). Partially non-linear stimulation intensity-dependent effects of direct current stimulation on motor cortex excitability in humans. Journal of Physiology, 51(7), 1987–2000.
Benninger, D. H., Lomarev, M., Lopez, G., Wassermann, E. M., Li, X., Considine, E., & Hallett, M. (2015). Transcranial direct current stimulation for the treatment of Parkinson’s disease. J Neurol Neurosurg Psychiatry, 81, 1105–1111.
Bianchi, M., Cosseddu, M., Manenti, R., Brambilla, M., Rizzetti, C., Padovani, A., & Borroni, B. (2015). Left parietal cortex transcranial direct current stimulation enhances gesture processing in corticobasal syndrome. European Journal of Neurology, 22, 1317–1322.
Bikson, M., Rahman, A., Datta, A., Fregni, F., & Merabet, L. (2012). High-resolution modeling assisted design of customized and individualized transcranial direct current stimulation protocols. Neuromodulation, 15, 306–315.
Biundo, R., Fiorenzato, E., Gentile, G., Martinez-Martin, P., & Bisiacchi, P. (2015). Double-blind randomized trial of t-DCS versus sham in Parkinson patients with mild cognitive impairment receiving cognitive training. Brain Stimulation, 8, 1223–1240.
Boeve, B. F. (2011). The multiple phenotypes of corticobasal syndrome and corticobasal degeneration: Implications for further study. Journal of Molecular Neuroscience, 45, 350–353.
Boggio, P. S., Ferrucci, R., Mameli, F., Martins, D., Martins, O., Vergari, M., … Priori, A. (2012). Prolonged visual memory enhancement after direct current stimulation in Alzheimer’s disease. Brain Stimulation, 5, 223–230.
Boggio, P. S., Ferrucci, R., Rigonatti, S. P., Covre, P., Nitche, M., Pascual-Leone, A., & Fregni, F. (2006). Effects of transcranial direct current stimulation on working memory in patients with Parkinson's disease. Journal of Neurological Sciences, 249, 31–38.
Boggio, P. S., Khoury, L. P., Martins, D. C. S., Martins, O. E. M. S., Macedo, E. C., & Fregni, F. (2009). Temporal cortex direct current stimulation enhances performance on a visual recognition memory task in Alzheimer’s disease. Journal of Neurology, Neurosurgery, & Psychiatry, 80, 444–447.
Boravac, J. A. (2016). Side effects of a dopamine agonist therapy for Parkinson’s disease: A mini-review of clinical pharmacology. Yale Journal of Biology and Medicine, 89(1), 37–47.
Bott, N. T., Radke, A., Stephens, M. L., & Kramer, J. H. (2014). Frontotemporal dementia: diagnosis, deficits and management. Neurodegenerative disease management, 4(6), 439–454.
Braak, H., & Braak, E. (1991). Neuropathological stageing of Alzheimer-related changes. Acta Neuropathologica, 82(4), 239–259.
Burton, E. J., McKeith, I. G., Burn, D. J., Williams, D., & O’Brien, J. T. (2004). Cerebral atrophy in Parkinson’s disease with the without dementia: A comparison with Alzheimer’s disease, dementia with Lewy bodies and controls. Brain, 127, 791–800.
Bystad, M., Rasmussen, I. D., Abeler, K., & Aslaksen, P. M. (2016). Accelerated direct current stimulation in Alzheimer’s disease: A case study. Brain Stimulation, 9, 634–635.
Cheng, C. P. W., Chan, S. S. M., Mak, A. D. P., Chan, W. C., Cheng, S. T., Shi, L., … Lam, L. (2015). Would transcranial direct current stimulation (tDCS) enhance the effects of working memory training in older adults with mild neurocognitive disorder due ot Alzheimer’s disease: Study protocol for a randomized controlled trial. Trials, 16, 479–486.
Cools, R., Stefanova, E., Barker, R. A., Robbins, T. W., & Owen, A. M. (2002). Dopaminergic modulation of high-level cognition in Parkinson's disease: The role of the prefrontal cortex revealed by PET. Brain, 125, 584–594.
Cotelli, M., Manenti, R., Paternico, D., Cosseddu, M., Brambilla, M., Petesi, M., … Borroni, B. (2016). Grey matter density predicts the improvement of naming abilities after tDCS intervention in agrammatic variant of primary progressive aphasia. Brain Topography, 29, 738–751.
Cotelli, M., Manenti, R., Petesi, M., Brambilla, M., Cosseddu, M., Zanetti, O., … Borroni, B. (2014). Treatment of primary progressive aphasias by transcranial direct current stimulation combined with language training. Journal of Alzhemier's Disease, 39, 779–808.
Datta, A., Truong, D., Minhas, P., Parra, L. C., & Bikson, M. (2012). Inter-individual variation during transcranial direct current stimulation and normalization of dose using MRI-derived computational models. Frontiers in Psychiatry, 3(91), 1–8.
De Lau, L. M., & Breteler, M. M. (2006). Epidemiology of Parkinson's disease. Lancet Neurology, 5(6), 525–535.
Doruk, D., Gray, Z., Bravo, G. L., Pascual-Leone, A., & Fregni, F. (2014). Effects of tDCS on executive function in Parkinson's disease. Neuroscience Letters, 582, 27–31.
Edmonds, E. C., Delano-Wood, L., Galasko, D. R., Salmon, D. P., & Bondi, M. W. (2015). Subtle cognitive decline and biomarker staging in preclinical Alzheimer’s disease. Journal of Alzheimer’s Disease, 47, 231–242.
Ferrucci, R., Cortese, F., Bianchi, M., Pittera, D., Turrone, R., Bocci, T., … Priori, A. (2015). Cerebellar and motor cortical transcranial stimulation decrease Levodopa-induced dyskinesias in Parkinson’s disease. Cerebellum, 15(1), 43–47.
Ferrucci, R., Mameli, F., Guidi, I., Mrakic-Sposta, S., Vergari, M., Marceglia, S., … Priori, A. (2008). Transcranial direct current stimulation improves recognition memory in Alzheimer’s disease. Neurology, 71, 493–498.
Fregni, F., Boggio, P. S., Santos, M. C., Lima, M., Vieira, A. L., Rigonatti, S. P., … Pascual-Leone, A. (2006). Noninvasive cortical stimulation with transcranial direct current stimulation in Parkinson’s disease. Movement Disorders, 21(10), 1693–1702.
Gervits, F., Ash, S., Coslett, H. B., Rascovsky, K., & Grossman, M. (2016). Transcranial direct current stimulation for the treatment of primary progressive aphasia: An open-label pilot study. Brain & Language, 162, 35–41.
Gorno-Tempini, M. L., Hillis, A. E., Weintraub, S., Kertesz, A., Mendez, M., Cappa, S. F., … Grossman, M. (2011). Classification of primary progressive aphasia and its variants. Neurology, 76(11), 1006–1014.
Hampstead, B. M., Gillis, M. M., & Stringer, A. Y. (2014). Cognitive rehabilitation of memory for mild cognitive impairment: A methodological review and model for future research. Journal of the International Neuropsychological Society, 20(2), 135–151.
Hampstead, B. M., Sathian, K., Moore, A. B., Nalisnick, C., & Stringer, A. Y. (2008). Explicit memory training leads to improved memory for face-name pairs in patients with mild cognitive impairment: Results of a pilot investigation. Journal of the International Neuropsychological Society, 14(5), 883–889.
Hampstead, B. M., Sathian, K., Phillips, P. A., Amaraneni, A., Delaune, W. R., & Stringer, A. Y. (2012a). Mnemonic strategy training improves memory for object location associations in both healthy elderly and patients with amnestic mild cognitive impairment: A randomized, single-blind study. Neuropsychology, 26(3), 385–399.
Hampstead, B. M., Stringer, A. Y., Stilla, R. F., Deshpande, G., Hu, X., Moore, A. B., … Sathian, K. (2011). Activation and effective connectivity changes following explicit-memory training for face-name pairs in patients with mild cognitive impairment: A pilot study. Neurorehabilitation and Neural Repair, 25(3), 210–222.
Hampstead, B. M., Stringer, A. Y., Stilla, R. F., & Sathian, K. (2012b). Mnemonic strategy training partially restores hippocampal activity in patients with mild cognitive impairment. Hippocampus, 22(8), 1652–1658.
Huey, E. D., Probasco, J. C., Moll, J., Stocking, J., Ko, M.-H., Grafman, J., & Wassermann, E. M. (2007). No effect of DC brain polarization on verbal fluency in patients with advanced ftrontotemporal dementia. Clinical Neurophysiology, 118(6), 1417–1418.
Kaski, D., Allum, J. H., Bronstein, A. M., & Dominguez, R. O. (2014). Applying anodal tDCS during tango dancing in a patient with Parkinson’s disease. Neuroscience Letters, 568, 39–43.
Kehagia, A. A., Barker, R. A., & Robbins, T. W. (2010). Neuropsychological and clinical heterogeneity of cognitive impairment and dementia in patients with Parkinson's disease. Lancet Neurology, 9, 1200–1213.
Kelley, A. S., McGarry, K., Gorges, R., & Skinner, J. S. (2015). The burden of health care costs for patients with dementia in the last 5 years of life. Annals of Internal Medicine, 163(10), 729–736.
Khedr, E. M., El Gamel, N. F., El-Fetoh, N. A., Khalifa, H., Ahmed, E. M., Ali, A. M., … Karim, A. A. (2014). A double-blind randomized clinical trial on the efficacy of cortical direct current stimulation for the treatment of Alzheimer’s disease. Frontiers in Aging Neuroscience, 6(275), 1–12.
Lee, S. E., Rabinovici, G. D., Mayo, M. C., Wilson, S. M., Seeley, W. W., DeArmond, S. J., … Sidhu, M. (2011). Clinicopathological correlations in corticobasal degeneration. Annals of Neurology, 70, 327–340.
Lehéricy, S., Sharman, M. A., Longo Dos Santos, C., Paquin, R., & Gallea, C. (2012). Magnetic resonance imaging of the substantia nigra in Parkinson's disease. Movement Disorders, 27(7), 822–830.
Litvan, I., Bhatia, K. P., Burn, D. J., Goetz, C. G., Lang, A. E., McKeith, I., … Wenning, G. K. (2003). Movement Disorder Society Scientific Issues Committee report: SIC Task Force appraisal of clinical diagnostic criteria for Parkinsonian disorders. Movement Disorders, 18, 467–486.
Manenti, R., Brambilla, M., Benussi, A., Rosini, S., Cobelli, C., Ferrari, C., … Cotelli, M. (2016). Mild cognitive impairment in Parkinson's disease is improved by transcranial direct current stimulation combined with physical therapy. Movement Disorders, 31(5), 715–724.
Marceglia, S., Mrakic-Sposta, S., Rosa, M., Ferrucci, R., Mameli, F., Vergari, M., … Priori, A. (2016). Transcranial direct current stimulation modulates cortical neuronal activity in Alzheimer’s disease. Frontiers in Neuroscience, 10(134), 1–11.
McKhann, G. M., Knopman, D. S., Chertkow, H., Hyman, B. T., Jack, C. R., Kawas, C. H., … Phelps, C. H. (2011). The diagnosis of dementia due to Alzheimer’s disease: Recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimer’s Dementia, 7(3), 263–269.
Meinzer, M., Lindenberger, R., Antonenko, D., Flaisch, T., & Floel, A. (2013). Anodal transcranial direct current stimulation temporarily reverses age-associated cognitive decline and functional brain activity changes. Journal of Neuroscience, 33, 12470–12478.
Meinzer, M., Lindenberger, R., Phan, M. T., Ulm, L., Volk, C., & Floel, A. (2015). Transcranial direct current stimulation in mild cognitive impairment: Behavioral effects and neural mechanisms. Alzheimer’s and Dementia, 11, 1032–1040.
Pereira, J. B., Junque, C., Bartres-Faz, D., Marti, M., Sala-Llonch, R., Compta, Y., … Tolosa, E. (2013). Modulation of verbal fluency networks by transcranial direct current stimulation (tDCS) in Parkinson's disease. Brain Stimulation, 6, 16–24.
Perl, D. P. (2010). Neuropathology of Alzheimer’s disease. Mount Sinai Journal of Medicine, 77(1), 32–42.
Perlmutter, J. S., & Mink, J. W. (2006). Deep brain stimulation. Annual Review of Neuroscience, 29, 229–257.
Plassman, B. L., Langa, K. M., Fisher, G. G., Heeringa, S. G., Weir, D. R., Ofstedal, M. B., … Wallace, R. B. (2007). Prevalence of dementia in the United States: The aging, demographics, and memory study. Neuroepidemiology, 29, 125–132.
Prince, M., Bryce, R., Albanese, E., Wimo, A., Ribeiro, W., & Ferri, C. P. (2013). The global prevalence of dementia: A systematic review and metaanalysis. Alzheimer’s and Dementia, 9, 63–75.
Reid, W. G. J., Hely, M. A., Morris, J. G. L., Broe, G. A., Adena, M., Sullivan, D. J. O., & Williamson, P. M. (1996). A longitudinal study of Parkinson’s disease: Clinical and neuropsychological correlates of dementia. Journal of Clinical Neuroscience, 3, 327–333.
Saykin, A. J., & Rabin, L. A. (2014). Dementias and neurodegenerative diseases. In M. W. Parsons & T. A. Hammeke (Eds.), Clinical neuropsychology: A pocket handbook for assessment Washington, DC, US: American Psychological Association. (pp. 266–286). http://dx.doi.org/10.1037/14339-012
Serrano-Pozo, A., Frosch, M. P., Masliah, E., & Hyman, B. T. (2011). Neuropathological alterations in Alzheimer’s disease. Cold Spring Harbor Perspectives in Medicine, 1(1), 1–23.
Sperling, R. A., Aisen, P. S., Beckett, D. A., Craft, S., Fagan, A. M., Iwatsubo, T., … Phelps, C. H. (2011). Toward defining the preclinical stages of Alzheimer’s disease: Recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimer’s Dementia, 7(3), 280–292.
Suemoto, C. K., Apolinario, D., Nakamura-Palacios, E. M., Lopes, L., Paraizo Leite, R. E., Castro Sales, M., … Fregni, F. (2014). Effects of a non-focal plasticity protocol on apathy in moderate Alzheimer’s disease: A randomized, double-blind, sham-controlled trial. Brain Stimulation, 7, 308–313.
Teichmann, M., Lesoil, C., Godard, J., Vernet, M., Bertrand, A., Levy, R., … Kas, A. (2016). Direct current stimulation over the anterior temporal areas boosts semantic processing in primary progressive aphasia. Annals of Neurology.
Tortella, G., Casati, R., Aparicio, L. V. M., Mantovani, A., Senco, N., D’Urso, G., … Brunoni, A. R. (2015). Transcranial direct current stimulation in psychiatric disorders. World Journal of Psychiatry, 5(1), 88–102.
Tsapkini, K., Frangakis, C., Gomez, Y., Davis, C., & Hillis, A. E. (2014). Augmentation of spelling therapy with transcranial direct current stimulation in primary progressive aphasia: Preliminary results and challenges. Aphasiology, 28(8–9), 1112–1130.
Valentino, F., Cosentino, G., Brighina, F., Pozzi, N. G., Sandrini, G., Fierro, B., … Pacchetti, C. (2014). Transcranial direct current stimulation for treatment of freezing of gait: a cross-over study. Movement Disorders, 29(8), 1064–1069.
Verheyden, G., Purdey, J., Burnett, M., Cole, J., & Ashburn, A. (2013). Immediate effect of transcranial direct current stimulation on postural stability and functional mobility in Parkinson’s disease. Movement Disorders, 28(14), 2040–2041.
Wang, J., Wu, D., Chen, Y., Yuan, Y., & Zhang, M. (2013). Effects of transcranial direct current stimulation on language improvement and cortical activation in nonfluent variant primary progressive aphasia. Neuroscience Letters, 549, 29–33.
Welsh-Bohmer, K. A., & Warren, L. H. (2006). Neurodegenerative dementias. In D. K. Attix & K. A. Welsh-Bohmer (Eds.), Geriatric neuropsychology: Assessment and intervention (pp. 56–88). New York, NY: The Guilford Press.
Wiethoff, S., Hamada, M., & Rothwell, J. C. (2014). Variability in response to transcranial direct current stimulation of the motor cortex. Brain Stimulation, 7, 468–475.
Yousuf, M. S., & Daniyal, U. (2012). Dementia in Parkinson's disease – A comprehensive review. Journal of Parkinsonism & Restless Legs Syndrome, 21(1), 6–10.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Rahman-Filipiak, A., Reckow, J.M., Woods, A.J., Nitsche, M.A., Hampstead, B.M. (2019). The Use and Efficacy of Transcranial Direct Current Stimulation in Individuals with Neurodegenerative Dementias. In: Knotkova, H., Nitsche, M., Bikson, M., Woods, A. (eds) Practical Guide to Transcranial Direct Current Stimulation. Springer, Cham. https://doi.org/10.1007/978-3-319-95948-1_16
Download citation
DOI: https://doi.org/10.1007/978-3-319-95948-1_16
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-95947-4
Online ISBN: 978-3-319-95948-1
eBook Packages: MedicineMedicine (R0)