Abstract
Accurate identification of eloquent cortical areas is of paramount importance for safe surgical resection in cases of medically intractable epilepsy or in glioma cases. Despite all the recent advances in functional magnetic resonance imaging (fMRI) and diffusion tensor imaging (DTI) as well as in magnetic source imaging and high-density surface EEGs, direct electrical cortical stimulation remains the gold standard for accurately outlining cortical eloquent areas. Intraoperatively employed cortical stimulation and mapping through an awake craniotomy is not always feasible. Patients with anxiety or fear of undergoing an awake surgical procedure, those with conditions contraindicating an awake procedure, and pediatric patients may not be suitable for mapping through an awake craniotomy. In these cases, and also in cases of medically refractory epilepsy in which invasive EEG monitoring is required for localizing any epileptogenic focus/i, cortical mapping may safely be accomplished through an extraoperative stimulation via implanted subdural and/or depth electrodes. This chapter presents the surgical preparation, the preoperative planning, the surgical procedure, and the extraoperative stimulation and mapping processes and their nuances. The associated complications with the electrode implantation and the invasive EEG monitoring and stimulation are also presented. Moreover, the future perspectives of invasive EEG monitoring and extraoperative cortical stimulation and mapping are briefly presented.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Accurate identification of eloquent cortical areas is of paramount importance for safe surgical resection in cases of medically intractable epilepsy or in glioma cases. Despite all the recent advances in functional magnetic resonance imaging (fMRI) and diffusion tensor imaging (DTI) as well as in magnetic source imaging and high-density surface EEGs, direct electrical cortical stimulation remains the gold standard for accurately outlining cortical eloquent areas. Intraoperatively employed cortical stimulation and mapping through an awake craniotomy is not always feasible. Patients with anxiety or fear of undergoing an awake surgical procedure, those with conditions contraindicating an awake procedure, and pediatric patients may not be suitable for mapping through an awake craniotomy. In these cases, and also in cases of medically refractory epilepsy in which invasive EEG monitoring is required for localizing any epileptogenic focus/i, cortical mapping may safely be accomplished through an extraoperative stimulation via implanted subdural and/or depth electrodes. This chapter presents the surgical preparation, the preoperative planning, the surgical procedure, and the extraoperative stimulation and mapping processes and their nuances. The associated complications with the electrode implantation and the invasive EEG monitoring and stimulation are also presented. Moreover, the future perspectives of invasive EEG monitoring and extraoperative cortical stimulation and mapping are briefly presented.
11.1 Introduction
The great positive effect of maximal resection in the overall survival of patients with gliomas has been well documented [1,2,3,4,5]. Gross total resection and even supramarginal resection of low-grade gliomas (LGGs) have been demonstrated to significantly increase the five- and ten-year survival rates and to minimize or significantly decrease the frequency and the severity of any preoperative seizure activity [6,7,8]. Furthermore, such resection has been demonstrated to decrease the possibility of a tumor recurrence and of its advancement to a higher histologic grade [6,7,8]. Likewise, it has been shown that maximal tumor resection is associated with prolonged progression-free and overall survival as well as improved functional status in patients with high-grade gliomas (HGGs) [4, 5, 9,10,11]. However, maximal glioma resection may jeopardize any adjacent cortical areas, particularly in those cases in which gliomas are located in or near eloquent cortical areas.
The definition of eloquent cortical areas has evolved over time, especially during the last two decades with the great advances in the fields of neuroimaging and electrophysiology . Traditionally, the cortical areas associated with motor, sensory, and speech functions are considered eloquent. Anatomic models had outlined the precentral sulcus (Brodmann area 4), and the supplementary motor area (Brodmann area 6) as the main cortical areas associated with motor function, the postcentral sulcus (Brodmann areas 1, 2, and 3) as the main area associated with sensory function, and the Broca (Brodmann areas 44 and 45) and Wernicke areas (Brodmann areas 22, 39, and 40) as the main cortical areas associated with speech functions. However, the landmark study of Ojemann et al. [12] demonstrated that these anatomic models are highly inaccurate, and the functional cortical areas demonstrate significant variation in regard to their exact anatomic location. The wide clinical employment of direct electrical cortical stimulation during neurosurgical procedures practically redefined the boundaries of the eloquent cortical areas, especially those associated with speech, and it confirmed that every patient has his or her own unique cortical functional map.
Furthermore, the emergence of functional MRI methodologies (task-generated and resting-state fMRI and diffusion tensor imaging), the evolution of standard electrophysiologic studies (high-density surface EEGs), and the development of hybrid imaging modalities combing neurophysiologic and anatomic data (magnetic source imaging, superimposing magneto-encephalo-graphic data on high-resolution MRIs) significantly enhanced our knowledge regarding the cortical areas involved in the speech process and their complex connectivity. Numerous studies have provided insights into the involvement of several other cortical areas in addition to the Broca and Wernicke areas [13,14,15,16,17,18,19,20,21,22,23,24,25,26,27]. They have shown that there is involvement in the speech process of cortical areas located in the frontal, temporal, and insular lobes of the dominant hemisphere but also in the temporal lobe of the nondominant hemisphere. It has been proposed that these cortical areas could be the functional components of two interacting loops: a preparatory and an executive one. The key elements of the preparatory loop are the supplementary motor area, the insula, and the superior cerebellum, while the executive loop includes the primary motor cortex, the thalamus, and the inferior cerebellum (Fig. 11.1). It has also been recently demonstrated that these extensive and highly complex cortical networks are interconnected with numerous white matter bundles [13, 23, 28,29,30,31,32]. The arcuate, the uncinate, the inferior fronto-occipital, the superior longitudinal, the middle longitudinal, and the inferior longitudinal fasciculi interconnect these cortical areas and participate in the speech process [13, 23, 28,29,30,31,32]. Interestingly, several investigators have postulated that these complex and interconnecting cortical and subcortical networks may demonstrate plasticity over time and may be variable not only from patient to patient but even in the same patient [33,34,35].
Intraoperative direct electrical stimulation is considered the gold standard in identifying and outlining cortical and subcortical areas associated with speech [12, 36,37,38,39]. However, it requires the patient undergoing surgery to be awake, fully cooperative, and psychologically stable. These conditions may represent limiting factors for employing direct stimulation and cortical/subcortical mapping. In addition, the patient’s obesity, pre-existing respiratory difficulties, brain midline structure shift caused by mass effect and edema, stimulation-induced seizures, and occurrence of trigemino-cardiac reflex may be relative contraindications for an awake craniotomy (Table 11.1) [40,41,42,43]. It should also be pointed out that during an awake craniotomy only certain language tasks can be assessed, mainly because of time restrictions. The overall failure rate of awake procedures has been reported to range between 0.5% and 6.3% [40, 42, 43].
Extraoperative cortical stimulation and mapping represent a valid alternative option for those patients who cannot undergo an awake procedure. They may be suitable for pediatric patients, for patients who are afraid of undergoing an awake surgical procedure, or for cases in which an extensive stimulation and mapping process is required (multilingual patients, extensive mapping of complex neurocognitive functions). This methodology lends itself to the evaluation and the safe surgical planning of patients with medically refractory epilepsy, gliomas, or metastatic tumors of eloquent areas as well as vascular lesions arterio-venous malformations (AVMs) or cavernous malformations (CMs) of eloquent areas.
11.2 Preoperative Assessment
The whole process of the two separate surgical procedures and the extraoperative stimulation and mapping session or sessions are adequately explained to the patient and the patient’s family. A detailed written consent form is obtained. The patient is carefully evaluated by a neuropsychologist, while all the planned neuropsychological tests and their clinical significance are extensively discussed with the patient. The process of the extraoperative electrical stimulation and mapping is explained to the patient, and special emphasis is given to the fact that seizures may be induced by the electrical stimulation and can be safely managed.
The process of the implantation of the electrodes, the benefits, and the potential complications are also discussed with the patient. The importance of maintaining the implanted electrode tails in a secure position and clean is pointed out to the patient and the caregivers. Also, the fact that there will be a video-EEG recording (in epilepsy cases) is explained.
The patient’s conventional MRI , magnetic resonance venography (MRV) , or computer tomography venography (CTV) , fMRI, and EEG studies are carefully reviewed. In cases in which there are concerns regarding the white matter tracts, a DTI study is obtained. A standard preoperative work-up including a complete blood count, platelet count, prothrombin time (PT), partial thromboplastin time (PTT), bleeding time, and a basic blood biochemical profile are obtained. Especially for epilepsy patients, the chronic use of anticonvulsants may interfere with the patient’s clotting profile. The patient is routinely evaluated by a neuroanesthesiologist before surgery.
11.3 Surgical Planning
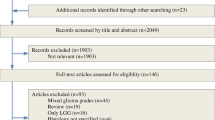
All the patient’s imaging studies (MRI, fMRI, DTI, MRV, or CTV) are uploaded in the navigation computer. In addition, the EEG data are taken into consideration for identifying any areas of epileptogenic activity. The areas of interest are identified, and their proximity to any potential eloquent cortical areas is examined. After confirming the areas that need to be covered by an electrode, the most efficient combination of subdural strip and grid and also depth (if necessary) electrodes is chosen (Fig. 11.2). It must be emphasized that a wide variation in shape and size of subdural electrodes is available for covering practically any cortical area. Furthermore, novel-shaped electrodes especially designed for certain anatomic areas (e.g., the insula) and hybrid electrodes with a combination of standard contacts and microwire arrays embedded in-between the contacts provide additional options for more accurate but also safer monitoring, stimulation, and mapping.
The potential entry point for depth electrodes as well as the surface cortical vein anatomy is carefully considered in order to minimize the risk of a venous injury during the insertion of the electrodes. The exit points of the tails of the subdural electrodes are carefully chosen in order to maximize sterility during the procedure and to minimize any mechanical friction, thereby avoiding any electrode migration during the monitoring period (Fig. 11.3). The most optimal surgical plan is finalized and saved for the day of the procedure, thus allowing the selection of the ideal position for the patient’s head and the three-point fixation device. Any particular concerns regarding the patient’s position during the procedure are discussed with the anesthesiology team.
Immediate postimplantation picture in a patient with left-sided temporal subdural electrode implantation for extraoperative EEG monitoring and cortical stimulation and mapping. The exiting electrode tails (arrow) are safely secured in the skin, while the exit points are in an adequate distance (at least 2.5 cm away) from the surgical wound skin incision. This will prevent any electrode misplacement and minimizes the risk of any postimplantation infections
11.4 Implantation of Electrodes
The day of the first procedure the patient takes all his or her medications early in the morning and is taken into the operating room. After a smooth general endotracheal anesthesia induction, the depth electrodes (if planned) are placed first in order to avoid any cerebrospinal fluid leak and thus minimize any inaccuracies. Subsequently, the planned craniotomy is performed. After the dural opening, the surface venous anatomy is confirmed. The subdural electrodes are carefully implanted, and their exiting tails are tunneled under the skin and exit at a distance of at least 2.5–3.0 cm from the surgical wound incision to minimize the risk of infection (Fig. 11.4). The importance of adequate exposure cannot be overemphasized so as to avoid any venous injuries and postoperative hematomas during the insertion of subdural grids and strips under the dura. The tails of the electrodes are safely anchored and secured at the skin. The bone edges at the exit points are drilled and smoothed in order to avoid any mechanical friction points and potential electrode breakage (Fig. 11.5). The surgical wound is thoroughly irrigated to remove any blood clots, which may interfere with the extraoperative monitoring and stimulation process.
A high-resolution photograph of the implanted electrodes is taken for the extraoperative stimulation process. The watertight closure of the dura is of paramount importance in order to avoid any postoperative cerebrospinal fluid leakages not only to mitigate any postoperative infections but also to avoid any electrode migration and displacement. The local application of collodion at the electrode exiting points serves exactly the same purpose.
A postoperative 1-mm slice thickness CT scan and an MRI are obtained in the immediate postoperative period for verifying the position of the implanted electrodes. The obtained images are fused, reconstructed in three-dimensional models, and used for electrode placement verification (Fig. 11.6).
11.5 Extraoperative Stimulation
The extraoperative stimulation in medically intractable epilepsy cases is performed after completing the monitoring period, which usually requires the recording of at least two to three episodes of the patient’s habitual seizures. In tumor cases, however, in which EEG monitoring is not necessary, the stimulation and mapping are usually performed 24 to 48 hours after the electrode implantation in order to minimize any implantation-associated artifacts.
The morning of the stimulation, the whole process is explained again to the patient. The patient’s comfort and the safe management of any stimulation-induced seizures are very important for the success of the stimulation and the detailed mapping. The whole process is video-recorded for future reference but also for research purposes.
The stimulation parameters may vary among different protocols. We routinely employ electric stimulation of 50 Hz frequency, alternating polarity of 0.2 ms, square-wave pulses, 3 s train, and current intensity of 2–6 mAmp. The initial stimulation may start at 2 mAmp, and then it may be progressively increased by 0.5 or 1 mAmp increments. Whenever there is a speech arrest, a phonemic error, or a paraphasia, a second round of stimulation is performed for confirming these findings after an adequate period of time. It should be pointed out that adequate time needs to be provided between stimuli in order to avoid any after-discharge electrical activity.
Numerous speech or other task tests may be employed during stimulation. We routinely perform at least a minimum menu of the following four speech tests: (i) Boston naming, (ii) listening comprehension of a text, (iii) reading of a text, and (iv) spontaneous speech. This core menu may be expanded to include other more complicated tests such as rehearsing, parroting, opposite/synonym word finding, noun production from a verb and vice versa, counting, and calculating, depending on the patient’s background and education level and skills. All these tests may be employed in more than one language for multilingual patients.
Furthermore, memory or other neuropsychological tests may be employed for evaluating certain skills and abilities, thus creating the respective cortical mappings. All other cognitive, psychological, or autonomic responses are recorded and are properly depicted on the generated cortical maps. In those cases in which a task-generated fMRI study has been previously performed, the employed paradigms may be tested for confirming the location of these functions but also for evaluating the accuracy of the fMRI results. The employment of extraoperative stimulation may provide significant clinical information as well as a large amount of electrophysiologic data for research purposes.
The stimulation and mapping can be performed in more than one session if the patient is not comfortable or if stimulation-induced seizures occur and interrupt one of the sessions. In addition, the patient’s relatives may be present during the whole process, which may be particularly helpful in cases of pediatric patients. The management of any stimulation-induced seizure activity can be safely done, but both the patient and the involved personnel need to be aware of this possibility. In our experience, including more than 150 tumor and epilepsy cases, the stimulation and mapping process could not be completed in only 3% of our patients. In approximately 15% of our cases this process required more than one session of stimulation and mapping.
11.6 Removal of Electrodes
All the collected data of the stimulation and the generated cortical maps are uploaded on to the navigation workstation and the surgical resection plan is created. The day of the second procedure, before prepping and draping of the surgical field, the electrode’s anchoring sutures are removed. After reopening the dural flap, the previously implanted electrodes are carefully removed and are sent for cultures. At the end of the procedure, the electrode exiting points are thoroughly irrigated with antibiotic solution and sutured.
11.7 Complications
The implantation of electrodes has been associated with various complications. In general, depth electrodes are considered safer than subdural electrodes [44,45,46]. Indeed, the occurrence of any depth electrode–associated complications has been reported to be 2.5% (overall morbidity), while the occurrence of hemorrhagic complications after depth electrode insertion was reported to be 0.2% [47,48,49,50].
Various complications have been reported in the pertinent literature in regard to the implantation of subdural strip and/or grid electrodes [44,45,46, 51,52,53,54]. Wellmer et al. [45] reported a cumulative complication rate of 23.1%, while in their recent series Yang et al. found that the subdural electrode–associated cumulative complication rate was 21.7% [54]. The subdural electrode associated mortality rate has been reported to be as high as 2.1% [52]. This is the result of increased intracranial pressure and cerebral edema development in the vast majority of these cases and is more common among children and in cases of interhemispheric, bulky, grid electrode implantation. The development of edema after subdural electrode implantation ranges in the literature between 0.5% and 14% [52]. In pediatric cases, when multiple subdural grid electrodes are planned to be implanted, it may be advantageous to insert an intracranial pressure monitor to properly manage the intracranial pressure.
The occurrence of an infection has been reported to vary from 1.1% to 17% [52]. In the vast majority of cases, the infection can be conservatively managed with systemic antibiotics, with no further consequences. The total number of the implanted electrodes and the duration of monitoring have been strongly associated with the development of postimplantation infection [45]. Likewise, the incidence of postimplantation cerebrospinal fluid leakage has been reported to range between 0% and 20% [52].
The development of postimplantation epidural hematoma has been reported to be 1.8%–2.5%, while that of a subdural hematoma has been 1.1%–14% (Fig. 11.7) [52]. Arya et al. [55], in their meta-analysis study including 21 previously published clinical series, found a 4% incidence of intracranial hemorrhage . They concluded, however, that only a small percentage (3.5%) of the complicated cases required a reoperation for managing their complication [55].
We have also previously reported the recording of nonhabitual seizures during the monitoring period in approximately 3% of our implant cases [44]. These findings may be the result of mechanical and/or chemical irritation of the underlying cortex caused by the implanted subdural grid [44]. This may be a confusing and misguiding finding in epilepsy cases, leading to erroneous conclusions regarding the localization of seizure focus/i.
11.8 Future Developments
The designing and the development of novel substrate materials for subdural strip and grid electrodes may further minimize the risk of any complications. Moreover, the wide clinical application of hybrid electrodes may well increase the accuracy of extraoperative stimulation and mapping. The designing and manufacturing of anatomically designated subdural electrodes for certain areas such as the insula and/or the mesial surface of the hemispheres will most probably increase the safety and the overall clinical utility of extraoperative monitoring, stimulation, and mapping strategies. However, thorough knowledge of the implantation surgical technique along with meticulous understanding of the potential complications remains of paramount importance.
References
Roelz R, Strohmaier D, Jabbarli R, Kraeutle R, Egger K, Coenen VA, et al. Residual tumor volume as best outcome predictor in low grade glioma - a nine-years near-randomized survey of surgery vs. biopsy. Sci Rep. 2016;6:32286.
Brown TJ, Brennan MC, Li M, Church EW, Brandmeir NJ, Rakszawski KL, et al. Association of the extent of resection with survival in glioblatoma: a systematic review and meta-analysis. JAMA Oncol. 2016;2:1460–9.
Suchorska B, Weller M, Tabatabai G, Senft C, Hau P, Sabel MC, et al. Complete resection of contrast-enhancing tumor volume is associated with improved survival in recurrent glioblastoma-results from the DIRECTOR trial. Neuro-Oncol. 2016;18:549–56.
Hervey-Jumper SL, Berger MS. Role of surgical resection in low- and high-grade gliomas. Curr Treat Options Neurol. 2014;16:284.
Sanai N, Berger MS. Glioma extent of resection and its impact on patient outcome. Neurosurgery. 2008;62:753–64. discussion, 264–6.
Lima GL, Zanello M, Mandonnet E, Taillandier L, Pallud J, Duffau H. Incidental diffuse low-grade gliomas: from early detection to preventive neuro-oncological surgery. Neurosurg Rev. 2016;39:377–84.
Duffau H, Taillandier L. New concepts in the management of diffuse low-grade glioma: Proposal of a multistage and individualized therapeutic approach. Neuro-Oncol. 2015;17:332–42.
Yordanova YN, Duffau H. Supratotal resection of diffuse gliomas: an overview of its multifaceted implications. Neurochirurgie. 2017:pii:S0028–3770(16)30133–3.
Lau D, Hervey-Jumper SL, Chang S, Molinaro AM, McDermott MW, Phillips JJ, et al. A prospective phase II clinical trial of 5-aminolevulinic acid to assess the correlation of intraoperative fluorescence intensity and degree of histologic cellularity during resection of high-grade gliomas. J Neurosurg. 2016;124:1300–9.
Rasul FT, Watts C. Novel surgical approaches to high-grade gliomas. Curr Treat Options Neurol. 2015;17:369.
Almenawer SA, Badhiwala JH, Alhazzani W, Greenspoon J, Farrokhyar F, Yarascavitch B, et al. Biopsy versus partial versus gross total resection in older patients with high-grade glioma: a systematic review and meta-analysis. Neuro-Oncol. 2015;17:868–81.
Ojemann G, Ojemann J, Lettich E, Berger M. Cortical language localization in left, dominant hemisphere. An electrical stimulation mapping investigation in 117 patients. J Neurosurg. 1989;71:316–26.
Duffau H. Mapping the connectome in awake surgery for gliomas: an update. J Neurosurg Sci. 2017; https://doi.org/10.23736/S0390-5616.17.04017-6. [Epub ahead of print.].
Tussis L, Sollmann N, Boeckh-Behrens T, Meyer B, Krieg SM. Identifying cortical first and second language sites via navigated transcranial magnetic stimulation of the left hemisphere in bilinguals. Brain Lang. 2017;168:106–16.
Maurer S, Giglhuber K, Sollmann N, Kelm A, Ille S, Hauck T, et al. Non-invasive mapping of face processing by navigated transcranial magnetic stimulation. Front Hum Neurosci. 2017;11:4.
Carota F, Kriegeskorte N, Nili H, Pulvermüller F. Representational similarity mapping of distributional semantics in left inferior frontal, middle temporal, and motor cortex. Cereb Cortex. 2017;1(27):294–309. https://doi.org/10.1093/cercor/bhw379.
Middlebrooks EH, Yagmurlu K, Szaflarski JP, Rahman M, Bozkurt B. A contemporary framework of language processing in the human brain in the context of preoperative and intraoperative language mapping. Neuroradiology. 2017;59:69–87.
Raffa G, Bährend I, Schneider H, Faust K, Germanò A, Vajkoczy P, Picht T. A novel technique for region and linguistic specific nTMS-based DTI fiber tracking of language pathways in brain tumor patients. Front Neurosci. 2016;10:552.
Branco P, Seixas D, Castro SL. Temporal reliability of ultra-high field resting-state MRI for single-subject sensorimotor and language mapping. Neuroimage. 2016:piiS1053–8119(16)30650–4.
Lyu B, Ge J, Niu Z, Tan LH, Gao JH. Predictive brain mechanisms in sound-to-meaning mapping during speech processing. J Neurosci. 2016;36:10813–22.
Sollmann N, Hauck T, Tussis L, Ille S, Maurer S, Boeckh-Behrens T, et al. Results on the spatial resolution of repetitive transcranial magnetic stimulation for cortical language mapping during object naming in healthy subjects. BMC Neurosci. 2016;17:67.
Makris N, Zhu A, Papadimitriou GM, Mouradian P, Ng I, Scaccianoce E, et al. Mapping temporo-parietal and temporo-occipital cortico-cortical connections of the human middle longitudinal fascicle in subject-specific, probabilistic, and stereotaxic Talairach spaces. Brain Imaging Behav. 2017;11(5):1258–77.
Negwer C, Ille S, Hauck T, Sollmann N, Maurer S, Kirschke JS, et al. Visualization of subcortical language pathways by diffusion tensor imaging fiber tracking based on rTMS language mapping. Brain Imaging Behav. 2016;20:1–6.
Sarubbo S, De Benedictis A, Merler S, Mandonnet E, Barbareschi M, Dallabona M, et al. Structural and functional integration between dorsal and ventral language streams as revealed by blunt dissection and direct electrical stimulation. Hum Brain Mapp. 2016;37:3858–72.
Cochereau J, Deverdun J, Herbet G, Charroud C, Boyer A, Moritz-Gasser S, et al. Comparison between resting state fMRI networks and responsive cortical stimulations in glioma patients. Hum Brain Mapp. 2016;37:3721–32.
Negwer C, Sollmann N, Ille S, Hauck T, Maurer S, Kirschke JS, et al. Language pathway tracking: comparing nTMS-based DTI fiber tracking with a cubic ROIs-based protocol. J Neurosurg. 2017;126:1006–14.
Huang H, Ding Z, Mao D, Yuan J, Zhu F, Chen S, et al. Presurgmapp: a matlab toolbox for presurgical mapping of eloquent functional areas based on task-related and resting-state functional MRI. Neuroinformatics. 2016;14:421–38.
D'Andrea G, Trillo’ G, Picotti V, Raco A. Functional magnetic resonance imaging (fMRI), pre-intraoperative tractography in neurosurgery: the experience of Sant' Andrea Rome university hospital. Acta Neurochir Suppl. 2017;124:241–50.
O'Donnell LJ, Suter Y, Rigolo L, Kahali P, Zhang F, Norton I, et al. Automated white matter fiber tract identification in patients with brain tumors. Neuroimage Clin. 2016;25:138–53.
Scaccianoce E, Laganà MM, Baglio F, Preti MG, Bergsland N, Cecconi P, et al. Combined DTI-fMRI analysis for a quantitative assessment of connections between WM bundles and their peripheral cortical fields in verbal fluency. Brain Topogr. 2016;29:814–23.
Ivanova MV, Isaev DY, Dragoy OV, Akinina YS, Petrushevskiy AG, Fedina ON, et al. Diffusion-tensor imaging of major white matter tracts and their role in language processing in aphasia. Cortex. 2016;85:165–81.
Wassermann D, Makris N, Rathi Y, Shenton M, Kikinis R, Kubicki M, et al. The white matter query language: a novel approach for describing human white matter anatomy. Brain Struct Funct. 2016;221:4705–21.
Hartwigsen G. Adaptive plasticity in the healthy language network: implications for language recovery after stroke. Neural Plast. 2016;2016:9674790.
Schlaffke L, Rüther NN, Heba S, Haag LM, Schultz T, Rosengarth K, et al. From perceptual to lexico-semantic analysis--cortical plasticity enabling new levels of processing. Hum Brain Mapp. 2015;36:4512–28.
Duffau H. The huge plastic potential of adult brain and the role of connectomics: new insights provided by serial mappings in glioma surgery. Cortex. 2014;58:325–37.
Austermuehle A, Cocjin J, Richard R, Agrawal S, Sepeta L, Gaillard WD, et al. Language fMRI and direct cortical stimulation in epilepsy preoperative planning. Ann Neurol. 2017;81:526–37.
Sollmann N, Ille S, Boeckh-Behrens T, Ringel F, Meyer B, Krieg SM. Mapping of cortical language function by functional magnetic resonance imaging and repetitive navigated transcranial magnetic stimulation in 40 healthy subjects. Acta Neurochir (Wien). 2016;58:1303–16.
Sollmann N, Kubitscheck A, Maurer S, Ille S, Hauck T, Kirschke JS, et al. Preoperative language mapping by repetitive navigated transcranial magnetic stimulation and diffusion tensor imaging fiber tracking and their comparison to intraoperative stimulation. Neuroradiology. 2016;58:807–18.
Brennan NP, Peck KK, Holodny A. Language mapping using fMRI and direct cortical stimulation for brain tumor surgery: the good, the bad, and the questionable. Top Magn Reson Imaging. 2016;25:1–10.
Hervey-Jumper SL, Li J, Lau D, Molinaro AM, Perry DW, Meng L, et al. Awake craniotomy to maximize glioma resection: methods and technical nuances over a 27-year period. J Neurosurg. 2015;123:325–39.
Ibrahim GM, Bernstein M. Awake craniotomy for supratentorial gliomas: why, when and how? CNS Oncol. 2012;1:71–83.
Nossek E, Matot I, Shahar T, Barzilai O, Rapoport Y, Gonen T, et al. Intraoperative seizures during awake craniotomy: incidence and consequences: analysis of 477 patients. Neurosurgery. 2013;73:135–40. discussion, 140.
Nossek E, Matot I, Shahar T, Barzilai O, Rapoport Y, Gonen T, et al. Failed awake craniotomy: a retrospective analysis in 424 patients undergoing craniotomy for brain tumor. J Neurosurg. 2013;118:243–9.
Fountas K, Smith J. Subdural electrode-associated complications: a 20-year experience. Stereotact Funct Neurosurg. 2007;85:264–72.
Wellmer J, van der Groeben F, Klarmann U, Weber C, Elger C, Urbach H, et al. Risks and benefits of invasive epilepsy surgery workup with implanted subdural and depth electrodes. Epilepsia. 2012;53:1322–32.
Hedegard E, Biellvi J, Edelvik A, Rydenhaq B, Flink R, Malmgren K. Complications to invasive epilepsy surgery workup with subdural and depth electrodes: a prospective population-based observational study. J Neurol Neurosurg Psychiatry. 2014;85:716–20.
Gonzalez-Martinez J, Bulacio J, Alexopoulos A, Jehi L, Bingaman W, Najm I. Stereoelectroencephalography in the “difficult to localize” refractory focal epilepsy: early experience from a North American epilepsy center. Epilepsia. 2013;54:323–30.
Gonzalez-Martinez J, Mullin J, Vadera S, Bulacio J, Hughes G, Jones S, et al. Stereotactic placement of depth electrodes in medically intractable epilepsy. J Neurosurg. 2014;120:639–44.
Bourdillon P, Ryvlin P, Isnard J, Montavont A, Catenoix A, Mauguiere F, et al. Stereotactic electroencephalography is a safe procedure, including for insular implantations. World Neurosurg. 2017;99:353–61.
Serletis D, Bulacio J, Bingaman W, Najm I, Gonzalez-Martinez J. The stereotactic approach for mapping epileptic networks: a prospective study of 200 patients. J Neurosurg. 2014;121:1239–46.
Hamer H, Morris H, Mascha E, Karafa M, Bingaman W, Bej M, et al. Complications of invasive video-EEG monitoring with subdural grid electrodes. Neurology. 2002;58:97–103.
Fountas K. Implanted subdural electrodes: safety issues and complication avoidance. Neurosurg Clin N Am. 2011;22:519–31. vii
Vale F, Pollock G, Dionisio J, Benbadis S, Tatum W. Outcome and complications of chronically implanted subdural electrodes for the treatment of medically resistant epilepsy. Clin Neurol Neurosurg. 2013;115:985–90.
Yang P, Zhang H, Pei J, Tian J, Lin Q, Mei Z, et al. Intracranial electroencephalography with subdural and/or depth electrodes in children with epilepsy: techniques, complications, and outcomes. Epilepsy Res. 2014;108:1662–70.
Arya R, Mangano F, Horn P, Holland K, Rose D, Glauser T. Adverse events related to extraoperative invasive EEG monitoring with subdural grid electrodes: a systematic review and meta-analysis. Epilepsia. 2013;54:828–39.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Fountas, K.N., Smith, J.R. (2019). Extraoperative Cortical Stimulation and Mapping. In: Fountas, K., Kapsalaki, E. (eds) Epilepsy Surgery and Intrinsic Brain Tumor Surgery. Springer, Cham. https://doi.org/10.1007/978-3-319-95918-4_11
Download citation
DOI: https://doi.org/10.1007/978-3-319-95918-4_11
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-95917-7
Online ISBN: 978-3-319-95918-4
eBook Packages: MedicineMedicine (R0)