Abstract
The surgical management of patients with primary hyperparathyroidism (PHPT) varies greatly among parathyroid surgeons, as well as across institutions. Four gland exploration, or bilateral neck exploration (BNE) has long been the “gold standard” operation for PHPT; it involves direct visualization of all parathyroid glands, with removal of enlarged parathyroid tissue, and has yielded excellent cure and complication rates, when performed by experienced surgeons. However, given that approximately 85% of patients with PHPT have single-gland disease, unilateral, minimally-invasive approaches have been advocated. The latter approaches require preoperative localization studies to identify the abnormal gland(s). While non-invasive imaging studies are routinely employed before index parathyroid surgery, negative, discordant or equivocal non-invasive localization studies are not uncommon, even in the unexplored patient. In this setting, an experienced parathyroid surgeon will still find and cure PHPT in the vast majority of patients. While bilateral neck exploration remains an excellent operation, controversy has developed in recent years, regarding the potential superiority of more focused, minimally invasive approaches. To address this issue, we evaluated the available literature for recommendations regarding the use of preoperative four-dimensional computed tomography (4DCT) versus direct, four gland exploration in patients with negative sestamibi and/or neck ultrasound studies. We summarize the available data and provide recommendations on how to surgically treat patients undergoing parathyroidectomy for PHPT.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Primary hyperparathyroidism
- Parathyroid adenoma
- 4D CT
- Four-gland exploration
- Bilateral neck exploration
- Sestamibi
- Neck ultrasound
- Non-invasive imaging
- Parathyroidectomy
- Minimally invasive parathyroidectomy
Introduction
Approximately 85% of patients with PHPT have single parathyroid gland enlargement, referred to as a parathyroid adenoma. A subset of patients with sporadic disease have multi-gland disease, in which all parathyroid glands are involved. Once the diagnosis of PHPT is made and patients meet surgical criteria, imaging studies are often undertaken to localize abnormal gland(s). Preoperative localization studies help identify patients who are candidates for minimally invasive approaches. While non-invasive imaging studies are routinely employed before index parathyroid surgery, negative, discordant or equivocal sestamibi and ultrasound studies are not uncommon, even in the unexplored patient. In recent years, four-dimensional computed tomography (4DCT) has been employed for parathyroid localization. The fourth dimension, time, accounts for differences in perfusion characteristics between the hyperfunctioning parathyroid gland and surrounding structures, such as the thyroid gland. Proponents of 4DCT hypothesize that routine institution of this preoperative localization study may lead to decreased operative time, shorter length of hospital stay, and improved cure rates. However, since BNE remains an excellent operation and avoids the increased radiation exposure associated with 4DCT, controversy has developed in recent years, regarding the optimal surgical approach for patients with PHPT. We evaluated the available literature for recommendations regarding the use of preoperative four-dimensional CT (4DCT) versus direct, four gland exploration in patients with negative sestamibi and/or neck ultrasound studies. To date, few large-scale studies have been performed to address this issue. Many of the recommendations in the literature have been based on the practices of single institutions. We summarize the available data and provide recommendations on how to surgically treat patients with non-localized PHPT (Table 16.1).
Search Strategy
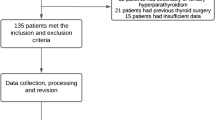
We conducted a focused review of the current guidelines related to preoperative localization studies for parathyroid adenomas/hyperplasia. We then performed a comprehensive review of the literature related to non-invasive imaging and parathyroid surgery. Literature searches were conducted in the PubMed database using the key words: primary hyperparathyroidism, parathyroid adenoma, 4D CT, four-gland exploration, bilateral neck exploration, sestamibi, non-invasive imaging, parathyroidectomy, and minimally invasive parathyroidectomy. Searches were limited to the English language, human subjects, and literature published in the last 15 years. Our search returned 618 articles; we critically reviewed 38 articles related to parathyroid surgery, as well as international guidelines from the Fourth International Workshop for the management of asymptomatic primary hyperparathyroidism. Emphasis was made on current national guidelines and recommendations.
Preoperative Localization of Abnormal Parathyroid Glands in Primary Hyperparathyroidism
The purpose of preoperative imaging in parathyroid surgery is to assist the surgeon in planning and performing an appropriate operation; such imaging should not be used for diagnosis, as PHPT is a biochemical diagnosis. Preoperative localization studies can help identify patients who may be candidates for a minimally invasive approach. An additional advantage is the potential for identification of concurrent thyroid disease, which may allow for a combined endocrine surgical procedure. A variety of non-invasive imaging options exist, including: neck ultrasound (U/S), sestamibi (SeS) ± single-photon emission computed tomography (SPECT), 4DCT, MRI, and positron emission tomography computed tomography (PET-CT).
The most commonly used non-invasive imaging for preoperative localization in PHPT are neck U/S, SeS ± SPECT, and 4DCT. Each imaging modality has its own advantages, as well as its own limitations. Parathyroid U/S has the best safety profile because it does not use ionizing radiation. Additionally, it is particularly sensitive in the detection of concurrent thyroid disease, and is relatively inexpensive. However, it requires a skilled technician to adequately demonstrate an abnormal parathyroid gland. It is also has very limited ability to identify ectopically-located parathyroid adenomas , such as in the retroesophageal or mediastinal location.
There exists a variety of nuclear scintigraphic agents and techniques. Currently, the most preferred non-invasive imaging study for parathyroid disease uses 99mTc-SeS with SPECT. This modality’s improved spatial resolution allows for detection of smaller parathyroid lesions than those found with sestamibi alone. However, similar to neck U/S, the sensitivity of SeS is greatly diminished by multiglandular parathyroid disease and concurrent thyroid pathology. More recently, 4DCT has been utilized for parathyroid localization; the fourth dimension (time) accounts for differences in perfusion characteristics between parathyroid adenomas/hyperplastic glands, and surrounding structures, such as the thyroid gland. Of note, because of the use of intravenous contrast, 4DCT should not be utilized in patients with known contrast allergy, renal insufficiency or known or suspected thyroid carcinoma.
In an effort to determine which non-invasive preoperative imaging modality is best for localizing abnormal parathyroid glands, several studies in the literature have been performed, most of which are retrospective analyses or case series (Table 16.2). Rodgers et al. [1] compared the results of preoperative imaging studies in 75 patients undergoing parathyroidectomy for PHPT. These investigators found that compared to neck U/S or SeS, 4DCT had significantly higher sensitivity and specificity for lateralization of the aberrant gland(s). Additionally, 4DCT localized the aberrant gland to the correct quadrant in 70% of cases, which was a significant improvement over neck U/S or SeS. Starker et al. [2] performed a retrospective analysis of a prospective database of patients undergoing parathyroidectomy for PHPT by a single experienced endocrine surgeon. Similar to the prior study, the researchers found 4DCT to be superior to neck U/S and SeS-SPECT, for both localization and lateralization of abnormal parathyroid tissue. A meta-analysis of 32 studies on preoperative localization techniques for patients with PHPT found that ultrasound and SeS were similar in their ability to preoperatively localize abnormal parathyroid glands, with pooled sensitivities of 76.1% and 78.9%, respectively [3]. Since an insufficient number of preoperative 4DCT studies were available for inclusion in this meta-analysis, the authors could not definitively demonstrate an advantage of 4DCT over U/S or SeS. However, results of those two studies suggested increased sensitivity of 4DCT. Recently, Suh et al. [4] carried out a prospective case series to compare 4DCT, U/S and SeS as methods of preoperative localization for patients undergoing parathyroidectomy. Thirty-eight patients underwent all three imaging modalities prior to surgery. All imaging studies were reviewed independently and in a blinded fashion. Once again, 4D CT proved superior in terms of sensitivity and specificity. In a most recent retrospective analysis, comparisons were made between the three aforementioned non-invasive imaging modalities for preoperative localization rate and accuracy in 200 patients who underwent parathyroidectomy for PHPT [5]. Results showed that in patients with single-gland disease, the sensitivity of 4DCT, SeS and U/S were 96%, 65.4% and 57.7%, respectively. Furthermore, these investigators used a modified 4DCT that decreased the effective radiation dose compared to standard 4DCT, noting an average radiation dose of 11–13 mSv, which is comparable to that of SeS. This was an important finding, as one criticism of the routine use of 4DCT has been the higher level of radiation dose given to patients, with its inherent increased risk of subsequent malignancy.
Recommendations
-
4DCT has higher sensitivity and specificity over U/S or SeS in the preoperative localization of abnormal parathyroid glands, and therefore may be considered as a first-line imaging choice for patients undergoing MIP, in centers/institutions where this modality is readily available.
-
4DCT should not be used in patients with suspected or definitive thyroid carcinoma, renal insufficiency, or in those allergic to intravenous contrast
-
The combination of U/S + SeS, when studies are concordant, serve as adequate localization prior to surgical intervention.
-
In cases of known multigland disease, or genetic causes of PHPT preoperative imaging for localization purposes are not necessary.
Because MIP requires preoperative imaging for localization of abnormal parathyroid glands, some surgeons question the cost-effectiveness of such a strategy, in comparison to the costs associated with BNE. In an effort to comprehensively evaluate the short-terms costs associated with various preoperative parathyroid localization strategies, cost-utility analysis models have been developed (Table 16.3). Wang et al. [6] described five different preoperative imaging algorithms to determine their incremental cost-utility ratio in patients with PHPT. They found that although U/S alone was the least expensive imaging modality ($6666), sestamibi-SPECT + U/S ± 4DCT was the most cost effective method. These savings are likely attributed to the decreased amount of BNE performed when this preoperative localization strategy is instituted. Lubitz et al. [7] developed a cost-analysis model to evaluate the short-term costs of preoperative localization strategies for patients with PHPT. In this model, U/S + 4DCT was the most cost effective strategy. However, both studies found that the most expensive strategy was direct BNE.
Recommendations
-
A combined imaging strategy of either U/S + sestamibi, U/S + 4DCT, or U/S + sestamibi ± 4DCT are the most cost effective strategies for preoperative localization in patients with PHPT.
-
Direct BNE is the most expensive approach , and should be limited to patients with known multigland disease, including those with genetic endocrine disorders (Table 16.3).
Unilateral Versus Bilateral Neck Exploration for Primary Hyperparathyroidism
Bilateral neck exploration (BNE) has long been the “gold standard” for the surgical management of primary hyperparathyroidism. However, in recent years, more focused, minimally invasive approaches have been promoted. This is largely due to the finding that a vast majority of patients with PHPT (85%) have single-gland disease. Therefore, a limited, unilateral approach could lead to curative rates comparable to BNE.
Data comparing BNE to minimally invasive parathyroidectomy (MIP) in patients with PHPT are limited. While several small to moderate-scale randomized clinical trials (RCTs) have been reported in the literature, the methods for BNE and MIP are extremely variable, making it somewhat challenging to compare across studies. The first RCT compared a video-assisted MIP approach to BNE in 38 patients undergoing surgery for PHPT [8]. While the authors found no difference in cure rate between the two groups, they reported shorter operative time, less pain and improved cosmesis in the MIP cohort. Several years later the same group of investigators compared a video-assisted MIP approach to an endoscopic BNE approach and found no differences in operative time, cure or complication rates between the two groups [9].
In 2002 Bergenfelz et al. [10] randomized 91 patients with PHPT to unilateral or bilateral neck exploration; preoperative scintigraphy and intraoperative parathyroid hormone (PTH) measurement guided the unilateral exploration. They found no differences in cost, transient recurrent laryngeal nerve (RLN) injury or short-term cure rates between the two groups. A five-year follow-up study confirmed comparable long-term cure rates between the two groups [11]. Another study by Bergenfelz et al. [12] looked specifically at the incidence of transient, post-operative hypocalcemia in 50 patients randomized to either MIP or BNE. The authors found a higher rate of transient hypocalcemia in the latter group. The remaining RCTs found no differences in cure or complication rates between MIP and BNE; variable differences in operative time and overall lower cost with BNE were reported [13,14,15,16].
In 2011, Udelsman et al. [17] compared the results of MIP with conventional BNE in a retrospective cohort of 1650 consecutive patients with PHPT. Interestingly, these authors found statistically significant higher curative rates, lower complication rates, as well as lower costs in the MIP group. To date, this study represents one of the largest series of patients who underwent parathyroidectomy for treatment of PHPT by a single, experienced endocrine surgeon.
Recommendations
A Surgical Taskforce, in connection with the Fourth International Workshop on the Management of Asymptomatic Primary Hyperparathyroidism developed evidence-based guidelines regarding surgery for PHPT [18]. They are as follows:
-
Both bilateral, or four-gland exploration, and minimally invasive parathyroidectomy yield excellent cure rates and minimal complication rates, when performed by an experienced surgeon.
-
Bilateral cervical exploration is the ideal operation for most patients with multigland disease, including those with genetic disease.
-
Minimally invasive parathyroidectomy procedures are not recommended in centers that do not have sophisticated imaging, intraoperative PTH assays, and experienced endocrine surgeons.
-
Intraoperative PTH assays are useful adjuncts during parathyroid surgery, and are essential, if focused approaches are employed.
-
Although minimally invasive techniques have become increasingly adopted, all parathyroid surgeons must be able to perform a standard bilateral cervical exploration, in the event that occult multigland disease is present (Table 16.4).
Four-Gland Exploration Versus 4D CT in Patients with Non-localized Primary Hyperparathyroidism
As mentioned earlier, four-gland exploration has long been the standard of care for the surgical treatment of PHPT. Recent data suggest that a more focused, or minimally invasive approach is fast becoming the “new standard”. Success of the latter approach requires adequate preoperative localization on radiologic evaluation, whereas the former approach does not require such imaging. While the choice between MIP and BNE remains a matter of debate, most parathyroid surgeons would likely proceed with MIP for patients with concordant positive imaging, while reserving BNE for cases with discordant imaging. However, there exists a subset of patients with discordant imaging (U/S and SeS)—to date, the management of such patients is not standardized.
Given that up to 70% of cases with discordant imaging still have single-gland disease [19], there is the possibility that a focused approach could be undertaken in many patients, pending some other means of preoperative localization (i.e. 4DCT). The other option would be to proceed straight to BNE to identify and remove the culprit gland. To date, there are no randomized trials comparing MIP to BNE in patients with PHPT and non-localized or discordant imaging. In an effort to assess the role of 4DCT in patients with negative or discordant preoperative U/S and SeS studies, Lubitz et al. [20] retrospectively reviewed 60 patients with PHPT and discordant preoperative U/S and SeS who underwent both localization with 4DCT and operative intervention by an experienced endocrine surgeon. These authors found that 4DCT correctly lateralized and localized the abnormal parathyroid gland(s) in 76 and 60% of cases, respectively. Although the majority of these patients underwent bilateral neck exploration (as per convention for non-localizing imaging), 4DCT imaging allowed for a focused approach in 34% of patients who would have otherwise undergone BNE. The authors concluded that 4DCT identifies patients amenable to focused intervention in more than half of the patients with negative (or discordant) U/S and SeS.
Summary of Recommendations
Preoperative Localization of Abnormal Parathyroid Glands in Primary Hyperparathyroidism
4DCT has higher sensitivity and specificity over U/S or SeS in the preoperative localization of abnormal parathyroid glands, and therefore may be considered as a first-line imaging choice for patients undergoing MIP, in centers/institutions where this modality is readily available (evidence quality strong; strong recommendation). The combination of U/S + SeS, when studies are concordant, serve as adequate localization prior to surgical intervention (evidence quality strong; strong recommendation). In cases of known multigland disease, or genetic causes of PHPT preoperative imaging for localization purposes are not necessary (evidence quality moderate; moderate recommendation) (Table 16.4).
Unilateral Versus Bilateral Neck Exploration for Primary Hyperparathyroidism
A combined imaging strategy of either U/S + sestamibi, U/S + 4DCT, or U/S + sestamibi ± 4DCT are the most cost effective strategies for preoperative localization in patients with PHPT (evidence quality moderate; moderate recommendation). Direct BNE is the most expensive approach, and should be limited to patients with known multigland disease, including those with genetic endocrine disorders (evidence quality moderate; moderate recommendation).
Four-Gland Exploration Versus 4D CT in Patients with Non-localized Primary Hyperparathyroidism
There are no randomized clinical trials comparing 4DCT as a third imaging study prior to parathyroidectomy, versus direct four-gland exploration without further imaging in patients with PHPT and negative or discordant preoperative U/S and SeS scanning. However 4DCT imaging may be beneficial in the subset of patients with PHPT and negative or discordant U/S and SeS. Future studies on the comparative effectiveness of these two surgical strategies are warranted.
Conclusion
We discuss the perioperative management of patients with PHPT and discordant preoperative imaging, specifically the use of preoperative four-dimensional computed tomography (4DCT) versus direct, four gland exploration in patients with negative sestamibi and/or neck ultrasound studies. While there are no prospective, randomized clinical trials comparing these two surgical strategies, a substantial amount of useful information can inferred from the current literature on this topic. The recommendations for preoperative localization strategies prior to focused parathyroidectomy are largely straightforward. Controversy remains regarding the best approach to operative management in patients with PHPT and discordant or negative U/S and SeS. Because this issue is of both clinical and economic significance, future randomized trials are necessary to determine how to best manage these patients.
A Personal View of the Data
We routinely use 4DCT as a preoperative imaging strategy for patients undergoing parathyroidectomy for PHPT. If referred patients have already undergone U/S and SeS, with positive concordant studies, then such patients proceed to MIP (in the absence of concomitant thyroid disease). However, if imaging is discordant, or if referral patients have only undergone one prior non-invasive imaging study (either U/S or SeS), then those patients undergo 4DCT prior to surgical intervention. Exceptions to this strategy include patients with either renal insufficiency, known or suspected well-differentiated thyroid cancer, or contrast allergy (in the latter case, pretreatment prior to 4DCT can allow for some studies to be carried out).
If 4DCT localized the abnormal parathyroid gland, then patients undergo a MIP; in cases of non-localization with 4DCT, or concern for multigland disease, patients either undergo a focused approach with the possibility to conversion to bilateral neck exploration, or proceed directly with BNE. The operative strategy for this subset of patients is made on a case-by-case basis, and involves several factors including (but not limited to) preoperative serum calcium and intact PTH (iPTH) levels, as well as a thorough review of all imaging studies undertaken. Additionally, we use intraoperative PTH monitoring as an adjunct to surgery for all cases, both MIP and four-gland exploratory procedures.
The major criticism of the routine use of 4DCT is its relatively high radiation dose and risk of subsequent cancer. However many authors have demonstrated radiation doses that are comparable to that obtained with SeS. Furthermore, reductions in radiation dose with modified 4DCT imaging may be attainable as more refined reconstruction techniques become available (Tables 16.5, 16.6, and 16.7).
References
Rodgers SE, Hunter GJ, Hamberg LM, Schellingerhout D, Doherty DB, Ayers GD, et al. Improved preoperative planning for directed parathyroidectomy with 4-dimensional computed tomography. Surgery. 2006;140(6):932–40. Discussion 40-1.
Starker LF, Mahajan A, Bjorklund P, Sze G, Udelsman R, Carling T. 4D parathyroid CT as the initial localization study for patients with de novo primary hyperparathyroidism. Ann Surg Oncol. 2011;18(6):1723–8.
Cheung K, Wang TS, Farrokhyar F, Roman SA, Sosa JA. A meta-analysis of preoperative localization techniques for patients with primary hyperparathyroidism. Ann Surg Oncol. 2012;19(2):577–83.
Suh YJ, Choi JY, Kim SJ, Chun IK, Yun TJ, Lee KE, et al. Comparison of 4D CT, ultrasonography, and 99mTc Sestamibi SPECT/CT in localizing single-gland primary hyperparathyroidism. Otolaryngol Head Neck Surg. 2014;18:1723–8.
Kukar M, Platz TA, Schaffner TJ, Elmarzouky R, Groman A, Kumar S, et al. The use of modified four-dimensional computed tomography in patients with primary hyperparathyroidism: an argument for the abandonment of routine sestamibi single-positron emission computed tomography (SPECT). Ann Surg Oncol. 2015;22(1):139–45.
Wang TS, Cheung K, Farrokhyar F, Roman SA, Sosa JA. Would scan, but which scan? A cost-utility analysis to optimize preoperative imaging for primary hyperparathyroidism. Surgery. 2011;150(6):1286–94.
Lubitz CC, Stephen AE, Hodin RA, Pandharipande P. Preoperative localization strategies for primary hyperparathyroidism: an economic analysis. Ann Surg Oncol. 2012;19(13):4202–9.
Miccoli P, Bendinelli C, Berti P, Vignali E, Pinchera A, Marcocci C. Video-assisted versus conventional parathyroidectomy in primary hyperparathyroidism: a prospective randomized study. Surgery. 1999;126(6):1117–21. Discussion 21-2.
Miccoli P, Berti P, Materazzi G, Ambrosini CE, Fregoli L, Donatini G. Endoscopic bilateral neck exploration versus quick intraoperative parathormone assay (qPTHa) during endoscopic parathyroidectomy: a prospective randomized trial. Surg Endosc. 2008;22(2):398–400.
Bergenfelz A, Lindblom P, Tibblin S, Westerdahl J. Unilateral versus bilateral neck exploration for primary hyperparathyroidism: a prospective randomized controlled trial. Ann Surg. 2002;236(5):543–51.
Westerdahl J, Bergenfelz A. Unilateral versus bilateral neck exploration for primary hyperparathyroidism: five-year follow-up of a randomized controlled trial. Ann Surg. 2007;246(6):976–80. Discussion 80-1.
Bergenfelz A, Kanngiesser V, Zielke A, Nies C, Rothmund M. Conventional bilateral cervical exploration versus open minimally invasive parathyroidectomy under local anaesthesia for primary hyperparathyroidism. Br J Surg. 2005;92(2):190–7.
Slepavicius A, Beisa V, Janusonis V, Strupas K. Focused versus conventional parathyroidectomy for primary hyperparathyroidism: a prospective, randomized, blinded trial. Langenbeck’s Arch Surg. 2008;393(5):659–66.
Aarum S, Nordenstrom J, Reihner E, Zedenius J, Jacobsson H, Danielsson R, et al. Operation for primary hyperparathyroidism: the new versus the old order. A randomised controlled trial of preoperative localisation. Scand J Surg. 2007;96(1):26–30.
Sozio A, Schietroma M, Franchi L, Mazzotta C, Cappelli S, Amicucci G. Parathyroidectomy: bilateral exploration of the neck vs minimally invasive radioguided treatment. Minerva Chir. 2005;60(2):83–9.
Russell CF, Dolan SJ, Laird JD. Randomized clinical trial comparing scan-directed unilateral versus bilateral cervical exploration for primary hyperparathyroidism due to solitary adenoma. Br J Surg. 2006;93(4):418–21.
Udelsman R, Lin Z, Donovan P. The superiority of minimally invasive parathyroidectomy based on 1650 consecutive patients with primary hyperparathyroidism. Ann Surg. 2011;253(3):585–91.
Udelsman R, Akerstrom G, Biagini C, Duh QY, Miccoli P, Niederle B, et al. The surgical management of asymptomatic primary hyperparathyroidism: proceedings of the fourth international workshop. J Clin Endocrinol Metab. 2014;99(10):3595–606.
Philippon M, Guerin C, Taieb D, Vaillant J, Morange I, Brue T, et al. Bilateral neck exploration in patients with primary hyperparathyroidism and discordant imaging results: a single-centre study. Eur J Endocrinol. 2014;170(5):719–25.
Lubitz CC, Hunter GJ, Hamberg LM, Parangi S, Ruan D, Gawande A, et al. Accuracy of 4-dimensional computed tomography in poorly localized patients with primary hyperparathyroidism. Surgery. 2010;148(6):1129–37. Discussion 37-8.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Quinn, C.E., Carling, T. (2018). Four-Gland Exploration Versus Four-Dimensional Computed Tomography in Patients with Nonlocalized Primary Hyperparathyroidism. In: Angelos, P., Grogan, R. (eds) Difficult Decisions in Endocrine Surgery. Difficult Decisions in Surgery: An Evidence-Based Approach. Springer, Cham. https://doi.org/10.1007/978-3-319-92860-9_16
Download citation
DOI: https://doi.org/10.1007/978-3-319-92860-9_16
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-92858-6
Online ISBN: 978-3-319-92860-9
eBook Packages: MedicineMedicine (R0)