Abstract
Background
In recent years, four-dimensional computed tomography (4DCT) has emerged as a new localization study for primary hyperparathyroidism (pHPT).
Objective
We aimed to assess the added value of 4DCT in our institution in the first 4 years of use.
Methods
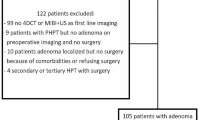
A retrospective cohort study was conducted from February 2004 to June 2015. Since 2011, patients over 50 years of age without concordant sestamibi-SPECT (SeS) and ultrasound (US) findings underwent 4DCT. Imaging results, surgical findings, histopathology, and postoperative biochemistry were collected.
Results
A total of 536 parathyroid operations in 510 patients were performed during the study period. The overall cure rate was 99.2% after reoperation in some patients, and the overall sensitivity for SeS was 76.0%, and 74.8% for US. Since 2011, 100 patients without concordant SeS/US findings have undergone 4DCT, with a sensitivity of 72.9%. This is in comparison to the sensitivities for SeS (48.3%) and US (52.3%). 4DCT was more sensitive in patients with persistent/recurrent disease (60.0% compared with SeS 43.8% and US 36.4%) and patients with multigland disease (67.4% compared with SeS 40.9% and US 42.1%). Comparison between outcomes in the pre- versus post-CT era demonstrated no difference in the initial cure rate (95.4 vs. 95.9%, p = 0.85) or the rate of minimally invasive parathyroidectomies (74.5 vs. 79.9%, p = 0.22).
Conclusion
Parathyroid 4DCT can aid surgical planning in cases without concordant SeS/US findings; however, the introduction of 4DCT as a second-line test did not change our overall cure rate or rate of minimally invasive parathyroidectomy. The role of 4DCT as the primary localization study for pHPT merits further investigation.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
In patients with primary hyperparathyroidism (pHPT), accurate preoperative localization of parathyroid adenomas (PTAs) is integral to operative planning.1 For patients with positive localization, minimally invasive parathyroidectomy (MIP) achieves comparable cure rates to traditional bilateral neck exploration (BNE), with lower complication rates and decreased postoperative pain.2,3 BNE is appropriate for pHPT patients with equivocal localization studies or multigland disease (MGD).
The primary preoperative imaging modalities in our institution are sestamibi-SPECT (SeS) and ultrasound (US). Concordant findings on SeS and US are associated with successful localization of PTAs and surgical cure in up to 98% of cases.1,4,5,6,7,8
In recent years, four-dimensional computed tomography (4DCT) has emerged as a new imaging modality for parathyroid localization. 4DCT provides anatomical localization by identifying PTAs based on their perfusion characteristics across multiple contrast phases. A meta-analysis looking into the three radiological modalities conducted by Cheung et al. reported improved sensitivity for 4DCT of 89.4% when compared with SeS (78.9%) and US (76.1%).5 With 4DCT providing more accurate localization of PTAs, Kukar et al. proposed the selection of 4DCT as the preoperative imaging modality of choice.9
With the introduction of 4DCT to our institution in 2011, we aimed to investigate the clinical value of 4DCT as a second-line test in localizing PTAs in patients with negative, equivocal, or discordant findings on SeS and US.
Methods
The Department of Research Governance and Ethics at Melbourne Health, Melbourne, VIC, Australia, approved the study. We retrospectively collected data of patients who underwent initial or reoperative parathyroidectomy for pHPT between February 2004 and June 2015. SeS and US were the initial imaging modalities in all patients. From 2011, all patients over 50 years of age with adequate renal function (defined as > 50 ml/min/1.73 m2) with negative, equivocal or discordant SeS and US findings also underwent 4DCT prior to surgery. Negative findings were defined when imaging failed to identify any PTA, while equivocal findings were defined when imaging reports suggested possible PTA localization with no definitive conclusion. Discordant findings were defined when SeS and US disagreed on the location of PTAs.
Patient age and sex, imaging findings, laboratory results, and pathology reports were collected from patients’ medical records. Cure was defined by histological findings confirming enlarged parathyroid gland(s), as well as normalizing of patient’s serum calcium and parathyroid hormone (PTH) 6 months after surgery. Correct localization was defined by an imaging modality’s ability to localize the PTA(s) to the correct side.
Sestamibi-SPECT Technique
A dual-phase protocol for SeS scans was used: 15 and 180 min after intravenous administration of approximately 800 MBq 99mTc-sestamibi. Planar images of the neck (level of the parotid gland) to the thorax (top of the heart) were performed, and a non-contrast CT coregistration scan was performed on a Siemens Somatom Emotion 16-slice CT scanner (Erlangen, Germany), from the top of the heart to the angle of the mandible. All studies were reported by one of three nuclear physicians.
Four-Dimensional Computed Tomography Technique
All 4DCT imaging was performed at a single institution using a Siemens Somatom Definition Flash 64-slice CT scanner (Erlangen, Germany). Three phases were performed: non-contrast, arterial, and venous phases. The scanning direction was caudo-cranial from the carina to the angle of the mandible. 100 mLs of iodinated contrast (Omnipaque 350) was injected at a rate of 4 mL/s. The descending aorta was monitored at the level of the carina and the scan triggered at a density of 150 Hounsfield units. The venous phase was acquired 30 s after the arterial phase. Images were reconstructed using a soft tissue kernel at 3 mm thickness in the axial and coronal planes, but the fine slice acquisition data were routinely reviewed in multiple planes. All studies were co-reported by two specialist radiologists with an interest in parathyroid imaging.
Statistical Analysis
Patient and clinical characteristics were reported as frequencies or relative frequencies for categorical data, and continuous data were reported as means and ranges. Statistics regarding the institution’s operative cases as well as cure rate were calculated, and the sensitivity and positive predictive value (PPV) of SeS and US were also calculated for the whole cohort.
Within the subgroup of patients with negative, equivocal, or discordant findings on SeS and US, and who subsequently underwent 4DCT imaging, the sensitivity and PPV for each of the three imaging modalities were calculated. Finally, surgical cure rates and proportion of cases being MIPs for both the pre- and post-CT era were calculated as relative frequencies, and comparisons were made using the Chi square test of independence.
Results
In the study period of February 2004 to June 2015, 536 consecutive parathyroidectomies were performed for pHPT on 510 patients. The average age of patients was 62 years (range 16–93) and 78.2% were female. The patient and clinical characteristics are summarized in Table 1.
The study comprised 384 MIPs, 107 BNEs, and an additional 45 reoperative cases (17 MIPs and 28 BNEs), 17 of whom had their initial surgery at an outside institution. The initial cure rate was 94.7%, while the overall cure rate was 99.2% after reoperation in some patients. The sensitivity and PPV were 76.0 and 93.1% for SeS, and 74.8 and 92.9% for US, respectively (Table 2).
Overall, 100 patients (104 operative cases) with negative, equivocal, or discordant findings on SeS and US underwent 4DCT. In this cohort, SeS had a sensitivity and PPV of 48.3 and 93.4%, respectively, US had a sensitivity of 52.3% and PPV of 88.9%, while 4DCT had a sensitivity of 72.9% and PPV of 86.9% (Table 3). In 31 patients, 4DCT identified a single PTA that was not appreciated on SeS and US, facilitating successful MIP. Conversely, of those who proceeded to 4DCT due to equivocal findings on SeS and US, three patients had a negative result on 4DCT, with the single PTA identified on either the SeS or US being correct.
In six cases, 4DCT identified ectopic PTAs not appreciated on SeS and US, including in the carotid sheath, and retroesophageal and mediastinal spaces (Fig. 1).
CT also significantly outperformed SeS and US in patients undergoing reoperative surgery, and patients who had MGD confirmed at surgery. As illustrated in Table 4, in the subset of patients with persistent or recurrent HPT, sensitivity of 4DCT was 60.0%, compared with 43.8% for SeS and 36.4% for US. In addition, 4DCT, with a sensitivity of 67.4%, was also better at identifying patients with MGD when compared with SeS (40.9%) and US (42.1%).
Among patients with MGD, six patients avoided further surgery because 4DCT detected bilateral disease that was not appreciated on SeS and US. Conversely, four patients had false positives, with 4DCT suggesting MGD when only a single PTA was present at surgery.
Comparison between our overall outcomes in the pre- vs. post-CT era demonstrated no difference in the initial cure rate (95.4 vs. 95.9%, respectively; p = 0.85) or the rate of MIPs (74.5 vs. 79.9%, respectively; p = 0.22).
Radiation Exposure
The median effective radiation dose for SeS was calculated to be 13.7 mSv, with a thyroid dose estimate of 41 mGy, while the median effective radiation dose for 4DCT was calculated to be approximately 9.3 mSv, with a thyroid dose estimate of 90 mGy.
Discussion
The conventional preoperative investigation for pHPT has been the combination of SeS scans and US, with concordant findings facilitating successful MIP. Correct preoperative identification of MGD, a problem encountered in 5.3% of our patients, could reduce the incidence of persistent disease, especially as intraoperative PTH measurements are not available at our institution. In our cohort, the sensitivity of SeS (76%) and US (74.8%) was comparable with the sensitivities of 78.9 and 76.1%, respectively, reported in the 2012 meta-analysis by Cheung et al.5
In our study, the overall sensitivity of the three imaging modalities are comparable (73–76%), despite 4DCT being performed preferentially in difficult-to-localize patients (where sensitivity of SeS and US were 48 and 52%, respectively), suggesting that 4DCT may be a superior initial imaging study, as reported by previous authors.7,9,10 This question is best addressed in an institution-specific manner, taking into account the respective accuracy of SeS and 4DCT, as well as issues such as local expertise and availability, patient preference (our patients prefer 4DCT as they are on site for considerably less time), and differences in radiation exposure, of particular concern in younger patients.
Considerations regarding radiation exposure have led to omitting the delayed venous phase in 4DCT, limiting the study to three phases as is done in our institution. This concept of removing phases from 4DCT has also been discussed in several previously published studies.1,11,12,13 At our institution, the total radiation dose was 47% higher with SeS compared with 4DCT, although exposure to the radiation-sensitive thyroid gland remains higher with 4DCT. Under these circumstances, the use of 4DCT as a first-line investigation merits further consideration.
The introduction of 4DCT did not translate into a significant improvement in our overall initial cure rate as this was already very high (95.4%) and our cohort size was small (n = 100). 4DCT did allow successful MIP in 31 of 100 patients who would have required BNE based on the SeS and US findings. Compared with the pre-CT era, the overall MIP rate improved, but not significantly. Several hypotheses can be offered for this result. SeS and US results in accurate localization of PTA(s) in most patients, rendering the contribution of 4DCT in the subset of patients without concordant data statistically insignificant (i.e. our cohort was too small). To detect a 5% difference in the rates of MIP between the pre- and post-CT era with 80% power at a significant level of 0.05 would require a sample size of 1787 participants in each group. In addition, despite SeS and US often failing to definitively localize a PTA, there is some hint on imaging that suggests where to begin the exploration. In effect, equivocal SeS would often be correct, and 4DCT merely served to increase the surgeon’s confidence in performing MIP. Furthermore, detection of MGD by 4DCT, while reducing the incidence of persistent disease, would have reduced the rate of MIP in the post-CT era. 4DCT also had a few false positive reports of MGD resulting in BNE, when MIP would have been curative. Finally, our study includes the period when 4DCT was first introduced, therefore the results may have been negatively impacted by the radiologists’ learning curve.
Limitations of this study include its retrospective nature and the relatively small subset of 104 operative cases who underwent 4DCT. Patients with concordant findings on SeS and US proceeded to operation without 4DCT. Therefore, the overall sensitivity and PPV of 4DCT in our entire cohort of patients with pHPT cannot be deduced. Lastly, interpretation of imaging was not blinded and physicians/radiologists had access to prior scans at the time of reporting SeS or 4DCT.
Conclusions
Parathyroid 4DCT can aid surgical planning in cases where SeS and US are inconclusive, and is more likely to identify patients with MGD. However, despite superior accuracy and facilitating successful MIP in 31 patients who otherwise would have had BNE, the introduction of 4DCT as a second-line test did not change our overall cure rate or rate of MIP. The role of 4DCT as the primary localization study for pHPT merits further investigation.
References
Brown SJ, et al., Four-dimensional computed tomography for parathyroid localization: a new imaging modality. ANZ J Surg. 2015;85(6): 483–87.
Goldstein RE, et al. Effect of minimally invasive radioguided parathyroidectomy on efficacy, length of stay, and costs in the management of primary hyperparathyroidism. Ann Surg. 2000;231(5):732–42.
Rodgers SE, et al. Improved preoperative planning for directed parathyroidectomy with 4-dimensional computed tomography. Surgery. 2006;140(6):932–40. discussion 940–41.
Chazen JL, et al. Diagnostic accuracy of 4D-CT for parathyroid adenomas and hyperplasia. AJNR Am J Neuroradiol. 2012;33(3):. 429–33.
Cheung K, et al. A meta-analysis of preoperative localization techniques for patients with primary hyperparathyroidism. Ann Surg Oncol. 2012;19(2):577–83.
Kutler DI, et al. Parathyroid localization with modified 4D-computed tomography and ultrasonography for patients with primary hyperparathyroidism. Laryngoscope. 2011; 121(6):1219–24.
Mortenson MM, et al. Parathyroid exploration in the reoperative neck: improved preoperative localization with 4D-computed tomography. J Am Coll Surg. 2008; 206(5):888-95. discussion 895–96.
Seeliger B, et al. Diagnostic value and clinical impact of complementary CT scan prior to surgery for non-localized primary hyperparathyroidism. Langenbecks Arch Surg. 2015;400(3):307–12.
Kukar M, et al. The use of modified four-dimensional computed tomography in patients with primary hyperparathyroidism: an argument for the abandonment of routine sestamibi single-positron emission computed tomography (SPECT). Ann Surg Oncol. 2015;22(1):139–45.
Starker LF, et al. 4D parathyroid CT as the initial localization study for patients with de novo primary hyperparathyroidism. Ann Surg Oncol. 2011;18(6):1723–28.
Campbell MJ, et al. Two-phase (low-dose) computed tomography is as effective as 4D-CT for identifying enlarged parathyroid glands. Int J Surg. 2015;14:80–84.
Kebebew E, et al. Predictors of single-gland vs multigland parathyroid disease in primary hyperparathyroidism: a simple and accurate scoring model. Arch Surg. 2006; 141(8):777–82. discussion 782.
Noureldine SI, et al. Multiphase computed tomography for localization of parathyroid disease in patients with primary hyperparathyroidism: how many phases do we really need? Surgery. 2014;156(6):1300–06. discussion 13006–07.
Disclosure
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tian, Y., Tanny, S.T., Einsiedel, P. et al. Four-Dimensional Computed Tomography: Clinical Impact for Patients with Primary Hyperparathyroidism. Ann Surg Oncol 25, 117–121 (2018). https://doi.org/10.1245/s10434-017-6115-9
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-017-6115-9