Abstract
P-wave correct interpretation may be of main importance. Its morphology and duration may help to increase the ECG sensitivity to diagnose a left ventricular hypertrophy or a diastolic dysfunction. A wide spectrum of cardiovascular and systemic disorders may involve the atria; more recently, the old atrial cardiomyopathy concept has been resumed. An atrial cardiomyopathy may lead to ugly complications such as atrial fibrillation and stroke. Recent clinical data in patients with an implanted cardiac device did show a lack of time correlation between atrial fibrillation and stroke. Thus, atrial fibrillation could be just an epiphenomenon related to abnormal atrial substrate (atrial cardiomyopathy). A recently published meta-analysis (He et al., Stroke 48:2066–72, 2017) has confirmed the association of three left atrial abnormalities easily assessable by means of a surface ECG, namely, increased P-terminal force in the precordial lead V1 (PTFV1) >40 ms mm, prolonged P-wave duration (PWD) >120 ms reflecting interatrial block and greater maximum P-wave area (PWA). Those parameters were associated not only with an increased risk of atrial fibrillation and other supraventricular arrhythmias but also of stroke. Furthermore, in patients with QRS and even repolarization abnormalities, a normal P-wave may be a good sign in favour of pseudo-abnormalities.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Atrial Cardiomyopathy
- Abnormal Atrial Substrate
- Interatrial Block
- Atrial Fibrillation
- Supraventricular Arrhythmias
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1.1 Case 1
A 63-year-old male with history of hypertension was admitted to the ER with aphasia and hemiparesis. Blood pressure was 140/85 mmHg. There were no clear heart murmurs or signs of heart failure. CT angiography showed left fronto-insulo-temporal hypodense area related to an acute ischemic lesion. Carotid arteries were normal at echocolordoppler.
The following was his standard 12-lead ECG (Fig. 1.1).
1.1.1 ECG Analysis
Sinus rhytm, heart rate 71 bpm, regular RR intervals.
There is a positive P-wave in leads I, II, III and VF, isoelectric in VL and negative in VR. P axis is +60; PR interval is 180 ms.
P-wave terminal force in lead V1 (PTFV1, the product of the depth of the terminal portion of P-wave in V1 multiplied by its duration) is 50 ms mm (Fig. 1.2).
P-wave duration (PWD) in lead II is 100 ms (Fig. 1.3).
P-wave area (PWA, the product of the duration and amplitude of the P-wave) is also higher than normal.
The QRS is 80 ms, with normal morphology and axis of +15°. Ventricular repolarization is normal with a QT interval of 380 ms and QTc (Bazett’s formula) of 413 ms.
Final ECG diagnosis: regular sinus rhythm and bi-atrial enlargement.
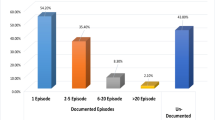
A 2D echocardiography and a 7-day-long ECG-Holter monitoring were recorded in order to check for paroxysmal AF episodes:
-
At echocardiography: mild dilatation of left and right atria, grade I diastolic dysfunction and moderate mitral regurgitation.
-
ECG monitoring did not document any episode of atrial fibrillation, atrial flutter or even atrial tachycardia.
Therefore, in this case the single 12-lead ECG could suggest an atrial pathology, probably due to end-diastole pressure overload, a likely consequence of undertreated arterial hypertension (Fig. 1.4).
1.1.2 From ECG to Pathology
There are many data in literature underlying how, in some patient that may have even QRS and repolarization abnormalities, a normal P-wave may be a quite specific index pointing to the absence of any cardiac dysfunction. On the other end, a P-wave abnormality may unmask a left ventricular hypertrophy [1, 2] or a diastolic dysfunction.
Over the past years, there has been a surge of interest towards a condition called “atrial cardiomyopathy”. For the first time, this term was used in a paper dating back in 1972 [3] describing a family whose members developed supraventricular arrhythmias, atrioventricular block and atrial standstill; the authors reported at autopsy how “the right atrium showed diffuse interstitial fibrosis with areas of subtotal muscle loss. There was extensive interstitial fibrosis throughout the wall”, thus identifying fibrosis as a key element underlying atrial pathologies. Other experiences were published later [4].
It was only in 1997, however, that the term atrial cardiomyopathy was adopted referring to patients affected by atrial fibrillation. In an editorial Douglas Zipes [5] commented on one of the first studies regarding pulmonary vein isolation as a treatment of atrial fibrillation. More recently, in 2016 [6], the European Heart Rhythm Association (EHRA), Heart Rhythm Society (HRS), Asia Pacific Heart Rhythm Society (APHRS) and Sociedad Latinoamericana de Estimulacion Cardiaca y Electrofisiología (SOLAECE), in cooperation with the American College of Cardiology and the American Heart Association, developed a consensus document on atrial cardiomyopathy, which is now defined as:
any complex of structural, architectural, contractile or electrophysiological changes affecting the atria with the potential to produce clinically relevant manifestations.
It is well recognized that the atria’s fundamental functions are not only to fill the ventricles but also to generate properly the cardiac rhythm and to secrete hormones such as the natriuretic peptides. Therefore, the atria may be involved in a wide spectrum of cardiovascular and systemic disorders, which are classified in a pathological-clinical way in that consensus document, according to whether the cardiomyocyte is mostly involved (Class I, such as in lone atrial fibrillation, diabetes mellitus or genetic cases), the fibroblast is mostly involved (Class II, such as in ageing or cigarette smoking), both cell types are involved (Class III, such as in valvular heart disease or congestive heart failure) or there are non-collagen deposits (Class IV, such as in isolated atrial amyloidosis, granulomatosis, inflammatory infiltrates or glycosphingolipids).
What is most interesting for the clinician is that this atrial cardiomyopathy can be involved in the development of complications, such as atrial fibrillation and stroke. It is well known that the risk of stroke and the consequent need to prescribe an anticoagulant in patients with atrial fibrillation do not depend on the duration or frequency of the arrhythmia but rather on the presence of clinical risk factors involved in the pathogenesis associated with the atrial cardiomyopathy, such as hypertension, heart failure, diabetes mellitus, a prior stroke or embolic event, age and evidence of atherosclerotic vascular disease, factors that grouped together are the bases of the CHA2DS2-VASc score [7].
One hypothesis is that most cases of cardioembolic stroke could not be a consequence of the blood stasis in the atrial appendages with clot formation, but rather stroke may be explained by the presence of the atrial cardiomyopathy independently of atrial fibrillation. Some clinical data in patients with an implanted cardiac device and thus a continuous rhythm monitoring have shown that there is not a strong time correlation between atrial fibrillation and stroke. In the ASSERT (Asymptomatic Atrial Fibrillation and Stroke Evaluation in Pacemaker Patients and the Atrial Fibrillation Reduction Atrial Pacing Trial) study, only 8% of the 51 patients who developed a stroke had an atrial fibrillation episode in 30 days preceding the cerebrovascular accident [8].
Thus, at present there is a belief considering that atrial fibrillation is not a direct cause of stroke but rather an epiphenomenon related to an abnormal atrial substrate (atrial cardiomyopathy) [9]. The atrial fibrosis (an element already recognized in the first paper of 1972), the inflammation state and the endothelial dysfunction may create a pro-thrombotic milieu.
Atrial fibrillation may be considered as one of the clinically relevant markers of an increased stroke risk, and, perhaps more importantly, the clinician should start as soon as possible to look more carefully for other markers that can increase the risk.
The ECG therefore is a fundamental and meaningful tool in this context. Starting in 1954 with the publication of a paper by Puech [10], it was recognized that an interatrial block of conduction is characterized by a wide P-wave in DII. It was early recognized that interatrial block is frequently associated with other conduction disturbances, such as sinus node dysfunction and atrioventricular conduction problems, and also with structural abnormalities of the left atrium, mainly enlargement, which, however, is not always present [11].
Bayés de Luna [12] described the association of interatrial block (defined as a P-wave duration of 120 ms or more with a biphasic morphology in DII, aVF or DII) [13] and supraventricular arrhythmias. The ECG findings could be explained by the sequential cranio-caudal activation of the right atrium followed by the retrograde activation of the left atrium.
More recently, it has been suggested that the Bayés syndrome, as it is now called, is associated with an increased risk of stroke [14, 15].
A recently published meta-analysis [16] has confirmed the association of three left atrial abnormalities easily assessable by means of a surface ECG, namely, increased P-terminal force in the precordial lead V1 (PTFV1) >40 ms mm, prolonged P-wave duration (PWD) >120 ms reflecting interatrial block or greater maximum P-wave area (PWA) not only with an increased risk of atrial fibrillation and other supraventricular arrhythmias but also with an increased risk of stroke.
A careful ECG P-wave analysis may be considered as useful instrument which, together with a clinical evaluation, echocardiogram, biomarkers and cardio-MRI, might help us find those patients who, independently of a known atrial fibrillation, are at risk of developing a cardioembolic stroke with consequent possible benefit coming from an anticoagulant therapy.
P-wave duration analysis can also be more accurate by evaluating the signal-averaged ECG (SAECG). SAECG is a simple noninvasive method, using cardiac electric signals from many surface electrodes, which has been used for years, initially to evaluate ventricular late potentials, and which has been extended to the P-wave to provide a more accurate evaluation of atrial conduction [17].
The values measured with all the leads are averaged to minimize interference and to see even the smallest alterations. A prolonged signal-averaged P-wave duration compared to the standard 12-lead ECG was found to be a more precise marker for the development of atrial fibrillation [18].
Other important findings detectable using SAECG are atrial late potentials. Late potentials are very-low-amplitude electric signals not visible with the standard 12-lead ECG. The QRS late potentials originally were studied to estimate the ventricular arrhythmia risk. Similarly, the P-wave (or atrial) late potential can be useful to stratify the risk for paroxysmal atrial fibrillation. Budeus et al. hypothesized that atrial late potentials found on P-wave SAECG could have a role in the development of paroxysmal atrial fibrillation [19, 20]. However, the predictive value of atrial late potentials has not yet been demonstrated.
In summary, atrial cardiomyopathy is a clinically meaningful concept that after many years of negligence is now under the light again, and its diagnostic correct evaluation could be of practical consequences. The ECG is therefore a simple and yet pivotal instrument that must not be forgotten in an era in which the diagnostic armamentarium is continuously enlarging but with also economic limitations.
1.2 Case 2
This ECG of an asymptomatic and obese (BMI 32) 65-year-old man was recorded on a preoperative visit for an elective noncardiac surgery. The past medical history is unremarkable except for hypertension and dyslipidemia both well managed with medications (Fig. 1.5).
1.2.1 ECG Analysis
Calibration: 0.5 cm/mV.
Speed: 25 mm/s.
RR interval: regular.
HR: 55 bpm.
P-wave duration: 80 ms.
P-wave morphology and amplitude: normal.
P-wave axis: P-wave is positive in leads I, II, VF and VL, isoelectric in lead III and negative in VR lead. Axis is +30°.
PR interval: 200 ms.
QRS duration: 80 ms.
QRS morphology and amplitude: at first sight we could say that QRS voltages are small; however, this ECG was recorded with 0.5 cm/mV gain, so actually the maximum amplitude in V6 is 1.5 mV, and in the peripheral lead, the criteria for low voltages are not satisfied. QRS amplitude is thus within normal limits.
In the QRS there is a minor right bundle conduction delay and absent R-wave progression in the precordial leads from V2 to V6. That pattern may be consistent with a possible previous silent myocardial infarction.
QRS axis: isoelectric in VF, positive in VR and almost negative in I and II leads. Thus, QRS axis is right deviated with a value of +120°.
ST segments and T waves were normal without any clear sign of acute myocardial ischemia.
QT interval: 440 ms with a QTc of 421 ms (Bazett).
Among the possible differential diagnosis, mostly related to the right axis deviation and the absence of R-wave progression, we should mention:
-
Previous silent anterior myocardial infarction
-
COPD
-
Congenital unknown cardiac abnormalities
In order to exclude major comorbidities, the patient was admitted to the cardiology department for further evaluation.
At echocardiography even with contrast, not any significant abnormalities were noticed. The overall ejection fraction was normal together with the regional wall motion. Thus, the ischemic aetiology was unlikely.
Because of the poor acoustic window, a cardiac MRI scan was afforded to exclude any congenital abnormalities that could have been missed at the transthoracic echocardiography.
The cardiac MRI surprisingly revealed the absence of the pericardium and of the pericardial fat.
Going back to ECG, we can notice that the morphology, the axis and the voltages of the P-waves are completely normal. This should have helped us to exclude any major cardiac congenital abnormalities. In fact, those should have led to atrial overload.
The complete congenital absence of the pericardium is a very uncommon finding. Subjects are often asymptomatic, but the first clinical presentation could be a non-exertional chest pain [21, 22]. Describing in detail this condition is not the purpose of this chapter and textbook, though we will focus on the ECG tracing associated to this rare malformation.
The ECG abnormalities consistent with congenital absence of pericardium described in literature are quite unspecific. They include sinus bradycardia, complete or incomplete bundle branch block, poor R-wave progression in the precordial leads secondary to a left displacement of the QRS transitional zone and prominent P-waves in case of a presence of a right atrial overload [21,22,23,24,25,26,27,28].
The ECG we report has two of these features (incomplete RBBB and poor R-wave progression), while P-waves are normal.
P-wave focusing may therefore help not only in the right ECG interpretation but mainly in the correct clinical evaluation.
References
Obbiassi M, Secchi MB, Mariotti G, et al. P wave analysis for the electrocardiographic diagnosis of left ventricular hypertrophy. A study of a population with arterial hypertension. G Ital Cardiol. 1979;9(10):1118–25.
Okin PM, Gerdts E, Wachtell K, et al. Relationship of left atrial enlargement to persistence or development of ECG left ventricular hypertrophy in hypertensive patients: implications for the development of new atrial fibrillation. J Hypertens. 2010;28(7):1534–40.
Nagle RE, Smith B, Williams DO. Familial atrial cardiomyopathy with heart block. Br Heart J. 1972;34:205.
Capucci A, Bracchetti D, Magnani B. Permanent atrial paralysis: clinical and instrumental study of a case. Boll Soc Ital Cardiol. 1977;22(1):45–9.
Zipes DP. Atrial fibrillation. A tachycardia induced atrial cardiomyopathy. Circulation. 1997;95:562–4.
Goette A, Kalman JM, Aguinaga L, et al. EHRA/HRS/APHRS/SOLAECE expert consensus on atrial cardiomyopathies: definition, characterisation, and clinical implication. J Arrhythm. 2016;32(4):247–78.
Lip GYH, Halperin J. Improving stroke risk stratification in atrial fibrillation. Am J Med. 2010;123:484–8.
Brambatti M, Connolly SJ, Gold MR, ASSERT Investigators, et al. Temporal relationship between subclinical atrial fibrillation and embolic events. Circulation. 2014;129:2094–9.
Kamel H, Okin PM, Elkind MS, et al. Atrial fibrillation and mechanisms of stroke: time for a new model. Stroke. 2016;47(3):895–900.
Puech P. L’activite´ electrique auriculaire normale et pathologuique. Paris: Masson; 1956. p. 206.
Chhabra L, Devadoss R, Chaubey VK, et al. Interatrial block in the modern era. Curr Cardiol Rev. 2014;10:181–9.
Baye’s de Luna A, Cladellas M, Oter R, et al. Interatrial conduction block and retrograde activation of the left atrium and paroxysmal supraventricular tachyarrhythmia. Eur Heart J. 1988;9:1112–8.
Castillo P, Vernant P. Troubles de la conduction interauriculaire par bloc du faisceau de Bachmann. Arch Mal Coeur. 1971;64:1490.
Bacharova L, Wagner GS. The time for naming the interatrial block syndrome: Bayes syndrome. J Electrocardiol. 2015;48:133–4.
Ariyarajah V, Puri P, Apiyasawat S, et al. Interatrial block: a novel risk factor for embolic stroke? Ann Noninvasive Electrocardiol. 2007;12:15–20.
He J, Tse G, Korantzopoulos P, et al. P-wave indices and risk of ischemic stroke a systematic review and meta-analysis. Stroke. 2017;48:2066–72.
Guichard JB, Nattel S. Atrial cardiomyopathy: a useful notion in cardiac disease management or a passing fad? J Am Coll Cardiol. 2017;70(6):756–65.
Blanche C, et al. Value of P-wave signal averaging to predict atrial fibrillation recurrences after pulmonary vein isolation. Europace. 2013;15(2):198–204.
Steinberg SA, Guidera JS. The signal-averaged P wave duration: a rapid and noninvasive marker of risk of atrial fibrillation. J Am Coll Cardiol. 1993;21:1645–51.
Budeus M, et al. Detection of atrial late potentials with P wave signal-averaged electrocardiogram among patients with paroxysmal atrial fibrillation. Z Kardiol. 2003;92(5):362–9.
Maolo A, Contadini D. Difficult interpretation of ECG: small clues may make the difference. The role of the P-wave. In: Capucci A, editor. Clinical cases in cardiology. Cham: Springer; 2015.
Gatzoulis MA, Munk MD, Merchant N, et al. Isolated congenital absence of the pericardium: clinical presentation, diagnosis, and management. Ann Thorac Surg. 2000;69:1209–15.
Abbas AE, Appleton CP, Liu PT, et al. Congenital absence of the pericardium: case presentation and review of literature. Int J Cardiol. 2005;98(1):21–5.
Connolly HM, Click RL, Schattenberg TT, et al. Congenital absence of the pericardium: echocardiography as a diagnostic tool. J Am Soc Echocardiogr. 1995;8:87–92.
Salem DN, Hymanson AS, Isner JM, et al. Congenital pericardial defect diagnosed by computed tomography. Catheter Cardiovasc Diagn. 1985;11:75–9.
Shiavone W. Congenital absence of the left position of parietal pericardium demonstrated by nuclear magnetic resonance imaging. Am J Cardiol. 1985;55:1439.
Rais-Bahrami K, Granholm T, Short BL, et al. Absence of pericardium in an infant with congenital diaphragmatic hernia. Am J Perinatol. 1995;12:172–3.
Spodik D. Congenital abnormalities of the pericardium. The pericardium: a comprehensive review. 1st ed. New York: Marcel Dekker; 1997. p. 65–75.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Beltrame, M., Compagnucci, P., Maolo, A. (2019). P-Waves Are the Main Clues for Correct ECG Interpretation. In: Capucci, A. (eds) New Concepts in ECG Interpretation. Springer, Cham. https://doi.org/10.1007/978-3-319-91677-4_1
Download citation
DOI: https://doi.org/10.1007/978-3-319-91677-4_1
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-91676-7
Online ISBN: 978-3-319-91677-4
eBook Packages: MedicineMedicine (R0)