Abstract
The use of stem cells in promoting healing in the human body is an exciting and developing field. Steps to apply these cells to improve cartilage repair began with benchtop research four decades ago and have taken strides in the last decade through clinical trials. This chapter provides an overview of the development of these treatments and insight into the future of stem cell therapy in cartilage repair. With an improved understanding of the historical studies leading up to our current state, we will be better prepared to move forward with research and development and to better the treatment of our patients with cartilage injuries.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
The developing human body is created, or rather replicated and differentiated, from a single cell. Initially this single cell is comprised of two haploids (half-cells) that unite to create one single cell or “embryo.” Development of the human body from this single, immature, pluripotent cell, or stem cell, involves a sophisticated process of cell division, cell differentiation, and inter-cell signaling. This stem cell progresses into a multi-organ body comprised of many tissue types and cell lines. Some cells in our body maintain some abilities of these immature cells and are also referred to as stem cells.
Currently, there are three general domains of stem cells: embryonic stem cells (ESCs), induced pluripotent stem cells (iPSCs), and adult stem cells. It is generally considered that most adult stem cells are multipotent, i.e., they can differentiate only toward end-stage cell lines of the germ layer from which they derived. One exception is the mobilized peripheral blood stem cell which has been found to be pluripotent in animal study [1, 2]. ESCs and iPSCs are considered pluripotent, i.e., they can differentiate to end-stage lines of all three germ layers. ESCs are derived from embryonal tissue, have ethical concerns, and have fallen onto the back burner of stem cell research. Induced pluripotent stem cells are derived through the genetic manipulation of somatic cells, have safety concerns, and are under further benchtop development. Adult stem cells can be harvested from multiple human tissues, have been fully developed on the benchtop but require clinical translation with efficacy studies, and have therefore become the current major focus of research clinicians. Since the majority of regenerative cartilage research and development has focused on adult stem cells, it will be the focus of this chapter.
There are four stem capabilities which differentiate these cells from other cells in our body: the ability to self-renew, the ability to differentiate into distinctive end-stage cell types, the ability to monitor and respond to environmental change, and the ability to release a number of molecules to affect their environment [3]. There are cells with stem capability in many tissues including adipose tissue, the synovium of joints, the superficial and deep layers of cartilage, the blood, tendon tissue, and muscle tissue. While initial in vitro study of these cells focused on their ability to divide and differentiate, recent animal and human studies have investigated the natural function of these cells in vivo. It is now clear that some adult stem cells have the ability to monitor their local and the systemic environment for stimuli, mobilize locally and/or systemically in settings of environmental insult, interact with their surrounding environment through paracrine effects, and differentiate to an end-stage cell if necessary [1, 2, 4,5,6,7,8,9] (Fig. 13.1). Stem cells can release a broad spectrum of macromolecules through secretory vessels, sometimes called exosomes or secretomes , which may contain proteins, chemokines, cytokines, and messenger RNA with trophic, chemotactic, and immunomodulatory potential depending upon the environmental stimuli [11]. Through these secretomes, which have paracrine cellular effects, or through differentiation, they participate in injury response, tissue healing, and tissue regeneration [9]. Considering these properties, it is clear that these cells are innate to the body’s maintenance, repair, and stress response systems.
The four capabilities attributed to stem cells : replicate, differentiate, monitor/mobilize, and exert paracrine effects. (Reprinted from Anz [10]. With permission from Springer Verlag)
Cell Sources and Processing Considerations
In an attempt to harvest the properties of stem cells, researchers and clinicians have studied tissues from different sources and preparation processes. It is important to delineate concentrated and/or simple processed tissues from culture-expanded tissues, as these methods produce different cell numbers. For example, adult bone marrow contains plasma, red blood cells, platelets, red blood cell/platelet precursors, and other nucleated cells. Through centrifugation and selective harvest, one can obtain a fraction of bone marrow which has nucleated cells with stem capabilities, with quantitative studies suggesting 30–317,400 cells/mL of bone marrow are available [12]. Additionally, upon culture of a fraction of bone marrow, selection of the plastic-adherent cells after culture, and further culture of these adherent cells, one can obtain an even greater number of stem cells. The cells obtained from the culture process from bone marrow have been termed “bone marrow-derived mesenchymal stem cells” (BM MSCs ). Similarly, adipose tissue can be harvested, processed through enzymatic or mechanical methods, centrifuged, and either applied with or without culture expansion. The non-cultured product is often referred to as stromal vascular fraction (SVF ), with yields ranging from 4737 cells/mL of adipose tissue to 1,550,000 cells/mL of tissue [12]. SVF can also be cultured to increase stem cell yield, and the product is called adipose-derived stem cells (ADSCs ). One must consider all steps involved in a product’s preparation in order to evaluate its potential value. Developmental hurdles of culture expansion include risks involving bacterial contamination and cellular transformation. Within the United States, the FDA has ruled that they consider cultured cells as drugs which require pre-market development and approval [13].
Preclinical In Vitro Development
Alexander Maximow is a Russian-born scientist who is credited with the earliest discoveries involving stem cells. His work at the University of Chicago in the 1920s included “morphology of the mesenchymal reactions” and the development of cells into fibroblasts in vitro [14, 15]. Further work on cells from bone marrow progressed in the 1960s [16], but the foundational work applying stem cells to cartilage repair started in the lab of Arnold Caplan in the late 1970s [17, 18]. Caplan and his colleagues were the first to differentiate cultured cells from bone marrow aspirate into multiple tissues including chondrocytes, adipocytes, and osteocytes. Initially, studies began with inducing embryonic chick limb mesenchymal cells to differentiate into cartilage cells. Since the end-stage cells arose from mesoderm, the term mesenchymal stem cell (MSC) was coined [19]. Caplan’s work progressed and tracked to orthopedic applications leading to the release of his monograph entitled “Mesenchymal Stem Cells” in the Journal of Orthopedic Research in 1991. In this paper, he proposed that 1 day MSCs could be isolated from autologous tissue, culture expanded ex vivo, and reimplanted for differentiation into repair tissue, such as cartilage or bone [7].
Scientists all over the world have continued to study stem cells from diverse sources uncovering mechanisms of cell differentiation and cell signaling. To review all in vitro studies is beyond the scope of this article; important lessons in the process will be highlighted. It has become clear that stem cells can be induced into cartilage cells, with work starting with bone marrow-derived cultured cells [20]. Additionally, cells from other tissue sources have shown potential to differentiate to cartilage including cells derived from fat, periosteum, synovium, and muscle [20,21,22,23,24]. Initial comparative studies proved that bone marrow-derived cells have more chondrogenic potential than adipose-derived cells [25, 26]. Further differentiation studies compared cells derived from bone marrow, synovium, periosteum, fat, and muscle with superior cartilage growth from cells derived from bone marrow and synovium [23] (Fig. 13.2). Later direct comparison of synovium to bone marrow determined that synovial-derived cells have the greatest chondrogenic potential [23, 27]. Recent studies have identified stem cells in different layers of cartilage with emerging mechanisms in cartilage maintenance and repair response [28,29,30,31,32]. Early in vitro and in vivo studies are investigating the potential of these stem cells compared to other mesenchymal sources [24, 33]. Considering multiple cell sources have proven productive in benchtop study, the logistics around processing and application in light of regulatory/developmental requirements will likely guide clinical applications.
Chondrogenic potential of 5 human tissue sources after 3 culture passages followed by pelleting the cells and incubating for 21 days. Panel (a) represents the gross appearance next to a 1-mm scaled ruler. Panel (b) represents the histologic appearance with toluidine blue staining. Panel (c) compares the wet weight of the pellets from 6 individual donors. Values are the mean and SD of 3 samples from each source in each donor. (Reprinted from Sakaguchi et al. [23]. With permission from John Wiley & Sons)
Preclinical Animal Development
Similar to benchtop review, the entirety of animal study is beyond the scope of this article, and highlights will be made. Benchtop work was first translated to animal experiments in the early 1990s. Building upon Caplan’s work and with his collaboration, Wakitani et al. [34] implanted bone marrow-cultured MSCs on a collagen gel into a cartilage defect in rabbit model. The MSCs differentiated into chondrocytes by the 2nd week after implantation, and by the 24th week, tissue had organized into cartilage tissue and a subchondral bone plate redeveloped (Fig. 13.3). This study provided proof of Caplan’s concept that cells could be harvested, cultured ex vivo, and reimplanted for tissue repair. Similar studies have been performed with adipose tissue [35, 36], synovium [37, 38], and periosteum [39]. In a comparative study, bone marrow-derived stem cells were found to have superior cartilage formation ability than those cells derived from adipose cells in a canine model [40].
In a rabbit model BM MSC implanted into a cartilage defect in a collagen gel differentiated into chondrocytes by the second week after implantation (a) and by the 24th week tissue had organized into cartilage tissue and a subchondral bone plate redeveloped (b). (Reprinted from Wakitani et al. [34]. With permission from Wolters Kluwer Health Inc.)
In addition to implantation of cells within a scaffold, another tested concept is that stem cells injected into a local environment, i.e., a joint, have the potential to home (or localize) to an area of injury and participate in cartilage healing. Lee et al. investigated this concept in a mini-pig [41]. After the creation of a cartilage defect, one group received an intra-articular injection of BM MSC (average seven million cells) suspended in hyaluronic acid (HA) followed by two additional weekly HA injections, another group received three weekly HA injections, and a third group received three weekly saline injections. While both the HA and MSC groups were superior to saline, the MSC group showed improved histologic and morphologic evaluation. The BM MSC were labeled with carboxyfluorescein, and upon histologic examination, the labeled cells were homed to and integrated into the repair tissue (Fig. 13.4). A similar study of an injection of stem cells instead of direct implantation has been performed with the same conclusions drawn in a meniscus injury model [42], cultured synovial-derived stem cells (SDSC ), and a large-animal model and BM MSC [43].
Carboxyfluorescein-labeled BM MSC administered by intra-articular injection after the creation of a cartilage defect in a mini-pig model homed to and integrated into repair tissue. (Reprinted from Lee et al. [41]. With permission from John Wiley & Sons)
A concept without conclusion is whether immature stem cells or stem cells differentiated toward the chondrocyte lineage perform best in cartilage repair models. In a porcine model, cultured BM MSC embedded in a collagen scaffold were compared to cultured BM MSC pretreated with transforming growth factor β to differentiate the cells toward a chondrocyte line. The repair tissue in the undifferentiated group illustrated superior histologic and morphologic repair tissue. In contrast, in an ovine model, researchers determined the optimal predifferentiation period of MSC with chondrogenic medium in vitro. The predifferentiated cells were then implanted in a hydrogel and compared to undifferentiated MSC in a hydrogel. The predifferentiated cells showed better histologic scores with morphologic and immunohistochemical properties of hyaline cartilage [44].
With consideration of developmental and regulatory hurdles, researchers have also studied bone marrow aspirate concentrate as an adjunct to cartilage repair procedures. The use of bone marrow aspirate concentrate implanted at the time of a marrow stimulation procedure and as a single or series of injections after a marrow stimulation procedure has been shown to improve cartilage repair in an equine and caprine model [45, 46].
Clinical Development Overview
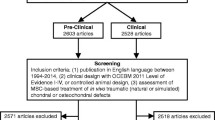
The application of stem cells in human studies has emerged and continues to emerge in three phases: case report/series design, comparative treatment study, and randomized controlled study. A recent systematic review in 2016 found 60 clinical studies including 9 case reports, 31 case series, 13 comparative trials, and 7 randomized controlled studies. On review, 20 of the studies investigated BM MSC , 16 investigated SVF , 16 investigated BMC, 5 studies investigated peripheral blood stem cells (PBSC ), 1 study investigated ADSC, 1 study investigated SDSC , and 1 study compared BMC to PBSC . Twenty-six of the sixty studies involved injection of cells intra-articularly for administration, and 33 investigated surgical implantation either in an open or arthroscopic fashion [47]. Generally speaking, stem cell treatments for cartilage repair have been safe and effective yet require further well-designed comparative study. Progress for each cell source will be summarized and landmark studies discussed in depth.
Clinical Development of BM MSC
BM MSC have the longest track record with initial work arising out of Japan. In 2002, Wakitani published a comparative study involving 12 patients undergoing HTO with BM MSC surgically implanted with a scaffold compared to 12 patients who underwent HTO alone [48]. At 16 months, clinical outcomes between the two groups were similar, while histologic and arthroscopic examination revealed better tissue in the MSC group. Subsequent case reports and case series of open surgical implantations with varying surgical methods followed with encouraging histologic and clinical outcome scores [49,50,51,52,53,54,55]. Additionally, case series have followed, investigating the injection of BM MSC for the symptomatic treatment of osteoarthritis with encouraging early results [56,57,58,59,60,61].
Comparative work of note has emerged from a group of research clinicians in Singapore since 2010 [62, 63]. Building on the mini-pig work described in the preclinical animal section, the group reported a comparative study of BM MSC implanted under a periosteal patch versus cultured chondrocytes under a periosteal patch, i.e., autologous chondrocyte implantation (ACI ) [62]. In a matched population, there was no difference in clinical outcomes between the groups at 24 months. Intra-cohort analysis revealed that older patients with ACI did not perform as well as younger patients with ACI, while older patients with the BM MSC performed as well as younger patients with BM MSC . Authors concluded that the stem cell method was the less aggressive, less expensive, and less morbid of the two procedures. The initial comparative study was followed by a second comparative study evaluating open periosteal implantation with intra-articular injection of BM MSC s after arthroscopic marrow stimulation [63]. At 24 months there was similar improvement in both groups leading the authors to suggest that the injection method was superior due to less morbidity. In 2013, the group reported on the results of a randomized controlled trial evaluating patients with unicompartmental OA and varus malalignment. Half of the patients were randomized to high tibial osteotomy (HTO) , arthroscopic microfracture , and one postoperative injection of HA. The other half of the patients were randomized to HTO, arthroscopic microfracture, and one postoperative injection of BM MSC suspended in HA. At 2-year follow-up, both groups illustrated improved yet similar outcome scores, while the BM MSC group produced better MRI scores [64].
Clinical Development of SVF and ADSC
To date developmental studies of adipose-derived tissue have involved SVF with the exception of one study involving ADSC. The majority of the work has emerged from a group out of South Korea investigating the use of SVF to augment arthroscopic procedures and osteotomy as well as investigating its role for osteoarthritis. Studies started with harvesting adipose tissue from the infrapatellar fat pad and progressed to liposuction harvest from the buttock region. The methodology for the group involves processing the tissue with centrifugation and collagenase and reliably produces four million ADSC s from 120 mL of lipoaspirate. The group has investigated one administration time point via intra-articular injection, arthroscopic implantation without a scaffold with PRP, and arthroscopic implantation with a fibrin scaffold. They conclude that arthroscopic implantation with a fibrin scaffold is safe and the most effective method for SVF administration. They have shown that it can improve the clinical results of simple arthroscopic debridement, marrow stimulation, and osteotomy. Comparison of this technique to other cartilage repair procedures is lacking at this time. This group has reported significant clinical and morphologic improvement when evaluated with MRI, yet histologic results have shown room for further development. These authors have determined that older age, higher BMI, and a larger defect size were negative predictors in all studies [65,66,67,68,69,70,71,72,73,74].
One study has investigated the dose-response relationship of ADSC to treat degenerative cartilage lesions with injection. The first phase of the study compared a 10 million cell injection, a 50 million cell injection, and a 100 million cell injection, with the best results reported in the 100 million injection group. The second phase followed nine patients receiving a single 100 million cell injection. No treatment-related adverse events were reported. WOMAC scores remained improved at 6 months after injection in the high-dose group. Second-look arthroscopy and histology suggest the regeneration of cartilage in the high-dose group [75].
Clinical Development of PBSC
Clinical results have also been emerging with PBSC . This concept follows the footsteps of the hematology oncology profession with development of the harvest of stem cells for bone marrow transplant. While originally bone marrow transplant involved bone marrow aspiration harvest, the profession developed harvest via pharmaceutical mobilization and venous harvest with apheresis. Pharmaceutical mobilization stimulates an upregulation of production of stem cells in the bone marrow and release of these cells to the peripheral circulation. Apheresis harvest involves a machine which uses centrifugation, optics, and continuous venous access for a period of 1–4 h to collect PBSC . For example, with orthopedic indications in mind, a 140-mL harvest contains on average 140 million PBSC, and the harvest can be aliquoted and stored for serial/multiple injections [76] (Fig. 13.5). This cell source has established safety data involving large registries and characterization of the cells, suggesting that they are more immature than BM MSC and have functional properties similar to ESC [1, 77]. One striking advantage of this cell source is the ability to harvest at one time point millions of cells which can be aliquoted and stored for serial injections throughout the maturation phase of the cartilage healing. This method leverages the body’s potential to create stem cells and does not require cell culture to produce hundreds of millions of cells.
Pharmaceutical mobilization of peripheral blood stem cells to the blood and closed-loop apheresis harvest (a) over 1–4 h allow for the harvest of millions of stem cells which can be aliquoted and stored (b) for serial injections. (Reprinted from Anz [10]. With permission from Springer Verlag)
The majority of developmental work applying PBSC to cartilage repair has emerged from a group in Malaysia. Saw et al. first reported a case series involving arthroscopic marrow stimulation followed by multiple postoperative intra-articular injections in five patients, with safety data and histology suggesting good cartilage repair tissue [76]. The case series was followed by a RCT comparing arthroscopic marrow stimulation followed by 8 postoperative PBSC intra-articular injections over the course of 6 months compared to arthroscopic marrow stimulation followed by 8 postoperative HA intra-articular injections. At 2 years, histology and MRI results favored the treatment group, but the clinical outcomes scores did not reveal superiority. On average, each stem cell injection in the intervention group contained eight million stem cells [78]. This group recently published a case series combining the cartilage procedure with HTO. Repair cartilage in this combination procedure when graded with ICRS scoring system approached 95% of that of normal articular cartilage. Similar encouraging results were seen in two additional case series involving PBSC and one comparative study of open implantation of PBSC to BMC [79,80,81].
Clinical Development of SDSC
Research involving the use of synovial-derived cultured cells has been arising from Japan. In one study, synovial-derived cultured cells have performed well at 3 years in a case series of 10 patients with single cartilage defects with a median size of 2 cm2, illustrating improvement in a MRI score, qualitative histology, and outcome scores. Administration involved culture expansion for 14 days, followed by arthroscopic application, allowing the suspension to rest in the horizontally placed defect for 10 min to allow adherence of the cells [82] (Fig. 13.6). Alternative work has developed a scaffold-free tissue-engineered construct from SDSC . A safety trial involving 10 patients was completed in 2015 with encouraging 1-year results [83].
Synovial-derived cultured cells have performed well at 3 years in a case series. Methods involved arthroscopic harvest culture expansion for 14 days in a clean room and an arthroscopic administration which involved holding the defect upward and allowing the suspension to sit for 10 min to allow adherence of the cells. (Reprinted from Sekiya et al. [82]. With permission from Creative Commons Attribution 4.0 International License: http://creativecommons.org/licenses/by/4.0/)
Clinical Development of BMC
With regulatory hurdles to the clinical implementation of cultured cells in all modern countries, clinical researchers in Italy have pioneered the direct surgical implantation of bone marrow concentrate involving a hyaluronic acid matrix. In 2009, a prospective clinical study reported on the repair of talar osteochondral lesions in 48 patients. With a minimum follow-up of 24 months, clinical results improved. Histology results illustrated variable tissue quality, with none being entirely hyaline cartilage [84]. Work continued with multiple case series involving the knee and ankle and culminated with a randomized controlled trial in the ankle and a prospective comparative study in the knee [85,86,87,88,89,90,91,92,93,94,95,96,97]. Of these, a prospective knee study evaluated 37 patients with large patellofemoral chondral defects and compared BMC under a HA scaffold method to matrix-induced autologous chondrocyte implantation (MACI ). Both groups showed significant improvement in clinical scores, and there was no significant difference in improvement between the two groups, except for the IKDC subjective score, which favored the BMAC group [97]. Subtle superiority was observed in the BMC group including deterioration in MACI from 2-year to final follow-up and anatomic defect location proving a hurdle for the MACI group. Upon MRI review, complete filing was observed in 76% of patients in MACI and 81% of patients in BMAC. Biopsies were obtained in four patients in each group with analysis revealing hyaline-like features (Fig. 13.7). A similar comparative study was performed in 80 patients with osteochondral lesions of the talus. Clinical results were similar in both groups at 48 months, with subtle superiority of the BMC group in return to sport and MRI evaluation [94].
Histologic comparison of matrix-assisted chondrocyte implantation to bone marrow aspirate concentrate implanted in a HA scaffold showed hyaline-like features in 75% of the specimens in both groups. (Reprinted from Gobbi et al. [97]. With permission from SAGE Publications Inc.)
Conclusion
The application of stem cells to cartilage injury has come a long way. The translation from bench to bedside has taken 40 years, but clinical success has been documented in several trials. Varying approaches are being developed around the world owing to different and evolving regulatory requirements. It appears that with high cell numbers and repeated administration, intra-articular injection is viable, while one-step surgical implantation is preferred for low cell number and single-point administration technologies, i.e., cell concentrate technologies. We look forward to the coming decade of clinical development and postulate that within that decade we will see multiple technologies available for patient care.
References
Cesselli D, Beltrami AP, Rigo S, et al. Multipotent progenitor cells are present in human peripheral blood. Circ Res. 2009;104(10):1225–34.
Ogawa M, LaRue AC, Mehrotra M. Hematopoietic stem cells are pluripotent and not just “hematopoietic”. Blood Cell Mol Dis. 2013;51:3–8.
Caplan AI. New era of cell-based orthopedic therapies. Tissue Eng Part B Rev. 2009;15:195–200.
Spencer NG, Caplan AI. Mesenchymal stem cells: mechanisms of inflammation. Annu Rev Pathol. 2011;6:457–78.
Rochefort GY, Delorme B, Lopez A, Herault O, Bonnet P, Charbord P, Eder V, Domenech J. Multipotential mesenchymal stem cells are mobilized into peripheral blood by hypoxia. Stem Cells. 2006;24(10):2202–8.
Marycz K, Mierzejewska K, Smieszek A, Suszynska E, Malicka I, Kucia M, Ratajczak MZ. Endurance exercise mobilizes developmentally early stem cells into peripheral blood and increases their number in bone marrow: implications for tissue regeneration. Stem Cells Int. 2016. Available at https://www.hindawi.com/journals/sci/2016/5756901/. Accessed 13 Aug 2017.
Caplan AI. Mesenchymal stem cells. J Orthop Res. 1991;9:641–50.
Wright DE, Wagers AJ, Gulati AP, Johnson FL, Weissman IL. Physiological migration of hematopoietic stem and progenitor cells. Science. 2001;294:1933–6.
Caplan AI. Adult mesenchymal stem cells for tissue engineering versus regenerative medicine. J Cell Physiol. 2007;213:341–7.
Anz AW. Biological augmentation of meniscal repairs. In: LaPrade R, Arendt E, Getgood A, Faucett S, editors. The menisci. Heidelberg: Springer; 2017. p. 137–46.
Caplan AI. Mesenchymal stem cells: time to change the name! Stem Cells Transl Med. 2017;6(6):1445–51.
Vangsness CT Jr, Sternberg H, Harris L. Umbilical cord tissue offers the greatest number of harvestable mesenchymal stem cells for research and clinical application: a literature review of different harvest sites. Arthroscopy. 2015;31(9):1836–43.
Anz AW. Current and future stem cell regulation: a call to action. Am J Orthop. 2016;45(5):274–318.
Maximow AA. Morphology of the mesenchymal reactions. Arch Pathol. 1927;4:557–606.
Maximow AA. Development of non-granular leucocytes (lymphocytes and monocytes) into polyblasts (macrophages) and fibroblasts in vitro. Proc Soc Exp Biol Med. 1927;24:570–2.
Friedenstein AJ, Piatetzky-Shapiro II, Petrakova KV. Osteogenesis in transplants of bone marrow cells. J Embryol Exp Morphol. 1966;6(3):381–90.
Caplan AI. Muscle, cartilage and bone development and differentiation from chick limb mesenchymal cells. In: Ede DA, Hinchliffe JR, Balls M, editors. Vertebrate limb and somite morphogenesis. Cambridge: Cambridge University Press; 1977. p. 199–213.
DeLuca S, Heinegard D, Hascall VC, Kimura JH, Caplan AI. Chemical and physical changes in proteoglycans during development of chick limb bud chondrocytes grown in vitro. J Biol Chem. 1977;252:6600–8.
Murphy MB, Moncivais K, Caplan AI. Mesenchymal stem cells: environmentally responsive therapeutics for regenerative medicine. Exp Mol Med. 2013;45:e54.
Johnstone B, Hering TM, Caplan AI, Goldberg VM, Yoo JU. In vitro chondrogenesis of bone marrow-derived mesenchymal progenitor cells. Exp Cell Res. 1998;238(1):265–72.
Dragoo JL, Samimi B, Zhu M, Hame SL, Thomas BJ, Lieberman JR, Hedrick MH, Benhaim P. Tissue-engineered cartilage and bone using stem cells from human infrapatellar fat pads. J Bone Joint Surg (Br). 2003;85-B:740–7.
De Bari C, Dell’Accio F, Tylzanowski P, Luyten FP. Multipotent mesenchymal stem cells from adult human synovial membrane. Arthritis Rheum. 2001;44(8):1928–42.
Sakaguchi Y, Sekiya I, Yagishita K, Muneta T. Comparison of human stem cells derived from various mesenchymal tissues: superiority of synovium as a cell source. Arthritis Rheum. 2005;52(8):2521–9.
Jiang Y, Cai Y, Zhang W, Yin Z, Hu C, Tong T, Lu P, Zhang S, Neculai D, Tuan RS, Ouyang HW. Human cartilage-derived progenitor cells from committed chondrocytes for efficient cartilage repair and regeneration. Stem Cells Transl Med. 2016;5(6):733–44.
Jakobsen RB, Shahdadfar A, Reinholt FP, Brinchmann JE. Chondrogenesis in a hyaluronic acid scaffold: comparison between chondrocytes and MSC from bone marrow and adipose tissue. Knee Surg Sports Traumatol Arthrosc. 2010;18(10):1407–16.
Danisovic L, Varga I, Polák S, Ulicná M, Hlavacková L, Böhmer D, Vojtassák J. Comparison of in vitro chondrogenic potential of human mesenchymal stem cells derived from bone marrow and adipose tissue. Gen Physiol Biophys. 2009;28(1):56–62.
Shirasawa S, Sekiya I, Sakaguchi Y, Yagishita K, Ichinose S, Muneta T. In vitro chondrogenesis of human synovium-derived mesenchymal stem cells: optimal condition and comparison with bone marrow-derived cells. J Cell Biochem. 2006;97(1):84–97.
Dowthwaite GP, Bishop JC, Redman SN, et al. The surface of articular cartilage contains a progenitor cell populations. J Cell Sci. 2004;117(6):889–97.
Williams R, Khan IM, Richardson K, et al. Identification and clonal characterisation of a progenitor cell sub-population in normal human articular cartilage. PLoS One. 2010;5(10):e13246.
Yu Y, Zheng H, Buckwalter JA, Martin JA. Single cell sorting identifies progenitor cell population from full thickness bovine articular cartilage. Osteoarthr Cartil. 2014;22(9):1318–26.
Chen S, Lee BH, Bae Y. Notch signaling in skeletal stem cells. Calcif Tissue Int. 2014;94(1):68–77.
Koelling S, Kruegel J, Irmer M, et al. Migratory chondrogenic progenitor cells from repair tissue during the later stages of human osteoarthritis. Cell Stem Cell. 2009;4(4):324–35.
Zhou C, Zheng H, Seol D, Yu Y, Martin JA. Gene expression profiles reveal that chondrogenic progenitor cells and synovial cells are closely related. J Orthop Res. 2014;32(8):981–8.
Wakitani S, Goto T, Pineda SJ, Young RG, Mansour JM, Caplan AI, Goldberg VM. Mesenchymal cell-based repair of large, full-thickness defects of articular cartilage. J Bone Joint Surg Am. 1994;76(4):579–92.
Dragoo JL, Carlson G, McCormick F, Khan-Farooqi H, Zhu M, Zuk PA, Benhaim P. Healing full-thickness cartilage defects using adipose-derived stem cells. Tissue Eng. 2007;13(7):1615–21.
Masuoka K, Asazuma T, Hattori H, Yoshihara Y, Sato M, Matsumura K, Matsui T, Takase B, Nemoto K, Ishihara M. Tissue engineering of articular cartilage with autologous cultured adipose tissue-derived stromal cells using atelocollagen honeycomb-shaped scaffold with a membrane sealing in rabbits. J Biomed Mater Res B Appl Biomater. 2006;79(1):25–34.
Nakamura T, Sekiya I, Muneta T, Hatsushika D, Horie M, Tsuji K, Kawarasaki T, Watanabe A, Hishikawa S, Fujimoto Y, Tanaka H, Kobayashi E. Arthroscopic, histological and MRI analyses of cartilage repair after a minimally invasive method of transplantation of allogeneic synovial mesenchymal stromal cells into cartilage defects in pigs. Cytotherapy. 2012;14(3):327–38.
Koga H, Muneta T, Ju YJ, Nagase T, Nimura A, Mochizuki T, Ichinose S, von der Mark K, Sekiya I. Synovial stem cells are regionally specified according to local microenvironments after implantation for cartilage regeneration. Stem Cells. 2007;25(3):689–96.
Martin-Hernandez C, Cebamanos-Celma J, Molina-Ros A, Ballester-Jimenez JJ, Ballester-Soleda J. Regenerated cartilage produced by autogenous periosteal grafts: a histologic and mechanical study in rabbits under the influence of continuous passive motion. Arthroscopy. 2010;26(1):76–83.
Reich CM, Raabe O, Wenisch S, Bridger PS, Kramer M, Arnhold S. Isolation, culture and chondrogenic differentiation of canine adipose tissue- and bone marrow-derived mesenchymal stem cells: a comparative study. Vet Res Commun. 2012;36(2):139–48.
Lee KB, Hui JH, Song IC, Ardany L, Lee EH. Injectable mesenchymal stem cell therapy for large cartilage defects--a porcine model. Stem Cells. 2007;25(11):2964–71.
Horie M, Sekiya I, Muneta T, Ichinose S, Matsumoto K, Saito H, Murakami T, Kobayashi E. Intra-articular injected synovial stem cells differentiate into meniscal cells directly and promote meniscal regeneration without mobilization to distant organs in rat massive meniscal defect. Stem Cells. 2009;27(4):878–87.
McIlwraith CW, Frisbie DD, Rodkey WG, Kisiday JD, Werpy NM, Kawcak CE, Steadman JR. Evaluation of intra-articular mesenchymal stem cells to augment healing of microfractured chondral defects. Arthroscopy. 2011;27(11):1552–61.
Zscharnack M, Help P, Richter R, Signer T, Schulz R, Sommerson J, Josten C, Bader A, Marquis B. Repair of chronic osteochondral defects using pre differentiated mesenchymal stem cells in an ovine model. Am J Sports Med. 2010;38(9):1857–69.
Fortier LA, Potter HG, Rickey EJ, Schnabel LV, Foo LF, Chong LR, Stokol T, Cheetham J, Nixon AJ. Concentrated bone marrow aspirate improves full-thickness cartilage repair compared with microfracture in the equine model. J Bone Joint Surg Am. 2010;92(10):1927–37.
Saw KY, Hussin P, Loke SC, Azam M, Chen HC, Tay YG, Low S, Wallin KL, Ragavanaidu K. Articular cartilage regeneration with autologous marrow aspirate and hyaluronic acid: an experimental study in a goat model. Arthroscopy. 2009;25(12):1391–400.
Filardo G, Perdisa F, Roffi A, Marcacci M, Kon E. Stem cells in articular cartilage regeneration. J Orthop Surg Res. 2016;11:42.
Wakitani S, Imoto K, Yamamoto T, Saito M, Murata N, Yoneda M. Human autologous culture expanded bone marrow mesenchymal cell transplantation for repair of cartilage defects in osteoarthritic knees. Osteoarthr Cartil. 2002;10:199–206.
Wakitani S, Mitsuoka T, Nakamura N, Toritsuka Y, Nakamura Y, Horibe S. Autologous bone marrow stromal cell transplantation for repair of full-thickness articular cartilage defects in human patellae: two case reports. Cell Transplant. 2004;13:595–600.
Adachi N, Ochi M, Deie M, Ito Y. Transplant of mesenchymal stem cells and hydroxyapatite ceramics to treat severe osteochondral damage after septic arthritis of the knee. J Rheumatol. 2005;32:1615–8.
Wakitani S, Nawata M, Tensho K, Okabe T, Machida H, Ohgushi H. Repair of articular cartilage defects in the patello-femoral joint with autologous bone marrow mesenchymal cell transplantation: three case reports involving nine defects in five knees. J Tissue Eng Regen Med. 2007;1(1):74–9.
Kuroda R, Ishida K, Matsumoto T, Akisue T, Fujioka H, Mizuno K, Ohgushi H, Wakitani S, Kurosaka M. Treatment of a full-thickness articular cartilage defect in the femoral condyle of an athlete with autologous bone-marrow stromal cells. Osteoarthr Cartil. 2007;15:226–31.
Haleem AM, Singergy AA, Sabry D, Atta HM, Rashed LA, Chu CR, El Shewy MT, Azzam A, Abdel Aziz MT. The clinical use of human culture-expanded autologous bone marrow mesenchymal stem cells transplanted on platelet-rich fibrin glue in the treatment of articular cartilage defects: a pilot study and preliminary results. Cartilage. 2010;1:253–61.
Kasemkijwattana C, Hongeng S, Kesprayura S, Rungsinaporn V, Chaipinyo K, Chansiri K. Autologous bone marrow mesenchymal stem cells implantation for cartilage defects: two cases report. J Med Assoc Thail. 2011;94(3):395–400.
Richter M, Zech S. Matrix-associated stem cell transplantation (MAST) in chondral defects of foot and ankle is effective. Foot Ankle Surg. 2013;19(2):84–90.
Centeno CJ, Busse D, Kisiday J, Keohan C, Freeman M, Karli D. Increased knee cartilage volume in degenerative joint disease using percutaneously implanted, autologous mesenchymal stem cells. Pain Physician. 2008;11(3):343–53.
Davatchi F, Abdollahi BS, Mohyeddin M, Shahram F, Nikbin B. Mesenchymal stem cell therapy for knee osteoarthritis. Preliminary report of four patients. Int J Rheum Dis. 2011;14(2):211–5.
Soler RR, Munar A, Soler RF, Peirau X, Huguet M, Alberca M, Sánchez A, García Sancho J, Orozco L. Treatment of knee osteoarthritis with autologous expanded bone marrow mesenchymal stem cells: 50 cases clinical and MRI results at one year follow-up. J Stem Cell Res Ther. 2015;5(6):285–91.
Davatchi F, Sadeghi Abdollahi B, Mohyeddin M, Nikbin B. Mesenchymal stem cell therapy for knee osteoarthritis: 5 years follow-up of three patients. Int J Rheum Dis. 2015;19(3):219–25.
Orozco L, Munar A, Soler R, Alberca M, Soler F, Huguet M, Sentis J, Sanchez A, Garcia-Sancho J. Treatment of knee osteoarthritis with autologous mesenchymal stem cells: two-year follow-up results. Transplantation. 2014;97(11):e66–8.
Emadedin M, Aghdami N, Taghiyar L, Fazeli R, Moghadasali R, Jahangir S, Farjad R, Baghaban Eslaminejad M. Intra-articular injection of autologous mesenchymal stem cells in six patients with knee osteoarthritis. Arch Iran Med. 2012;15(7):422–8.
Nejadnik H, Hui JH, Feng Choong EP, Tai BC, Lee EH. Autologous bone marrow-derived mesenchymal stem cells versus autologous chondrocyte implantation: an observational cohort study. Am J Sports Med. 2010;38:1110–6.
Lee KB, Wang VT, Chan YH, Hui JH. A novel, minimally-invasive technique of cartilage repair in the human knee using arthroscopic microfracture and injections of mesenchymal stem cells and hyaluronic acid—a prospective comparative study on safety and short-term efficacy. Ann Acad Med Singap. 2012;41:511–7.
Wong KL, Lee KB, Tai BC, Law P, Lee EH, Hui JH. Injectable cultured bone marrow-derived mesenchymal stem cells in varus knees with cartilage defects undergoing high tibial osteotomy: a prospective, randomized controlled clinical trial with 2 years’ follow-up. Arthroscopy. 2013;29(12):2020–8.
Koh YG, Choi YJ. Infrapatellar fat pad-derived mesenchymal stem cell therapy for knee osteoarthritis. Knee. 2012;19:902–7.
Koh YG, Jo SB, Kwon OR, Suh DS, Lee SW, Park SH, Choi YJ. Mesenchymal stem cell injections improve symptoms of knee osteoarthritis. Arthroscopy. 2013;29:748–55.
Koh YG, Choi YJ, Kwon SK, Kim YS, Yeo JE. Clinical results and second-look arthroscopic findings after treatment with adipose-derived stem cells for knee osteoarthritis. Knee Surg Sports Traumatol Arthrosc. 2015;23:1308–16.
Kim YS, Park EH, Kim YC, Koh YG. Clinical outcomes of mesenchymal stem cell injection with arthroscopic treatment in older patients with osteochondral lesions of the talus. Am J Sports Med. 2013;41:1090–9.
Koh YG, Kwon OR, Kim YS, Choi YJ, Tak DH. Adipose-derived mesenchymal stem cells with microfracture versus microfracture alone: 2-year follow-up of a prospective randomized trial. Arthroscopy. 2016;32:97–109.
Koh YG, Choi YJ, Kwon OR, Kim YS. Second-look arthroscopic evaluation of cartilage lesions after mesenchymal stem cell implantation in osteoarthritic knees. Am J Sports Med. 2014;42:1628–37.
Kim YS, Choi YJ, Suh DS, Heo DB, Kim YI, Ryu JS, Koh YG. Mesenchymal stem cell implantation in osteoarthritic knees: is fibrin glue effective as a scaffold? Am J Sports Med. 2015;43:176–85.
Kim YS, Lee HJ, Choi YJ, Kim YI, Koh YG. Does an injection of a stromal vascular fraction containing adipose-derived mesenchymal stem cells influence the outcomes of marrow stimulation in osteochondral lesions of the talus? A clinical and magnetic resonance imaging study. Am J Sports Med. 2014;42:2424–34.
Kim YS, Choi YJ, Koh YG. Mesenchymal stem cell implantation in knee osteoarthritis: an assessment of the factors influencing clinical outcomes. Am J Sports Med. 2015;43:2293–301.
Kim YS, Choi YJ, Lee SW, Kwon OR, Suh DS, Heo DB, Koh YG. Assessment of clinical and MRI outcomes after mesenchymal stem cell implantation in patients with knee osteoarthritis: a prospective study. Osteoarthr Cartil. 2016;24:237–45.
Jo CH, Lee YG, Shin WH, Kim H, Chai JW, Jeong EC, Kim JE, Shim H, Shin JS, Shin IS, et al. Intra-articular injection of mesenchymal stem cells for the treatment of osteoarthritis of the knee: a proof-of-concept clinical trial. Stem Cells. 2014;32:1254–66.
Saw KY, Anz A, Merican S, Tay YG, Ragavanaidu K, Jee CS, McGuire DA. Articular cartilage regeneration with autologous peripheral blood progenitor cells and hyaluronic acid after arthroscopic subchondral drilling: a report of 5 cases with histology. Arthroscopy. 2011;27:493–506.
Hölig K, Kramer M, Kroschinsky F, Bornhäuser M, Mengling T, Schmidt AH, Rutt C, Ehninger G. Safety and efficacy of hematopoietic stem cell collection from mobilized peripheral blood in unrelated volunteers: 12 years of single-center experience in 3928 donors. Blood. 2009;114(18):3757–63.
Saw KY, Anz A, Siew-Yoke Jee C, Merican S, Ching-Soong Ng R, Roohi SA, Ragavanaidu K. Articular cartilage regeneration with autologous peripheral blood stem cells versus hyaluronic acid: a randomized controlled trial. Arthroscopy. 2013;29:684–94.
Turajane T, Chaweewannakorn U, Larbpaiboonpong V, Aojanepong J, Thitiset T, Honsawek S, Fongsarun J, Papadopoulos KI. Combination of intra-articular autologous activated peripheral blood stem cells with growth factor addition/ preservation and hyaluronic acid in conjunction with arthroscopic microdrilling mesenchymal cell stimulation improves quality of life and regenerates articular cartilage in early osteoarthritic knee disease. J Med Assoc Thail. 2013;96:580–8.
Fu WL, Ao YF, Ke XY, Zheng ZZ, Gong X, Jiang D, Yu JK. Repair of large full-thickness cartilage defect by activating endogenous peripheral blood stem cells and autologous periosteum flap transplantation combined with patellofemoral realignment. Knee. 2014;21:609–12.
Skowronski J, Skowronski R, Rutka M. Cartilage lesions of the knee treated with blood mesenchymal stem cells – results. Ortop Traumatol Rehabil. 2012;14:569–77.
Sekiya I, Muneta T, Horie M, Koga H. Arthroscopic transplantation of synovial stem cells improves clinical outcomes in knees with cartilage defects. Clin Orthop Relat Res. 2015;473(7):2316–26.
Shimomura K, Ando W, Moriguchi Y, Sugita N, Yasui Y, Koizumi K, Fujie H, Hart DA, Yoshikawa H, Nakamuracorresponding N. Next generation mesenchymal stem cell (MSC)–based cartilage repair using scaffold-free tissue engineered constructs generated with synovial mesenchymal stem cells. Cartilage. 2015;6(2 Suppl):13S–29S.
Giannini S, Buda R, Vannini F, Cavallo M, Grigolo B. One-step bone marrow-derived cell transplantation in talar osteochondral lesions. Clin Orthop Relat Res. 2009;467:3307–20.
Buda R, Vannini F, Cavallo M, Grigolo B, Cenacchi A, Giannini S. Osteochondral lesions of the knee: a new one-step repair technique with bone-marrow-derived cells. J Bone Joint Surg Am. 2010;92(Suppl 2):2–11.
Giannini S, Buda R, Cavallo M, Ruffilli A, Cenacchi A, Cavallo C, Vannini F. Cartilage repair evolution in post-traumatic osteochondral lesions of the talus: from open field autologous chondrocyte to bone-marrow-derived cells transplantation. Injury. 2010;41:1196–203.
Gigante A, Calcagno S, Cecconi S, Ramazzotti D, Manzotti S, Enea D. Use of collagen scaffold and autologous bone marrow concentrate as a one-step cartilage repair in the knee: histological results of second-look biopsies at 1 year follow-up. Int J Immunopathol Pharmacol. 2011;24:69–72.
Gigante A, Cecconi S, Calcagno S, Busilacchi A, Enea D. Arthroscopic knee cartilage repair with covered microfracture and bone marrow concentrate. Arthrosc Tech. 2012;1:e175–80.
Buda R, Vannini F, Cavallo M, Baldassarri M, Luciani D, Mazzotti A, Pungetti C, Olivieri A, Giannini S. One-step arthroscopic technique for the treatment of osteochondral lesions of the knee with bone-marrow-derived cells: three years results. Musculoskelet Surg. 2013;97:145–51.
Giannini S, Buda R, Battaglia M, Cavallo M, Ruffilli A, Ramponi L, Pagliazzi G, Vannini F. One-step repair in talar osteochondral lesions: 4-year clinical results and t2-mapping capability in outcome prediction. Am J Sports Med. 2013;41:511–8.
Buda R, Vannini F, Cavallo M, Baldassarri M, Natali S, Castagnini F, Giannini S. One-step bone marrow-derived cell transplantation in talarosteochondral lesions: mid-term results. Joints. 2013;1:102–7.
Cadossi M, Buda RE, Ramponi L, Sambri A, Natali S, Giannini S. Bone marrow-derived cells and biophysical stimulation for talar osteochondral lesions: a randomized controlled study. Foot Ankle Int. 2014;35:981–7.
Gobbi A, Karnatzikos G, Sankineani SR. One-step surgery with multipotent stem cells for the treatment of large full-thickness chondral defects of the knee. Am J Sports Med. 2014;42:648–57.
Buda R, Vannini F, Castagnini F, Cavallo M, Ruffilli A, Ramponi L, Pagliazzi G, Giannini S. Regenerative treatment in osteochondral lesions of the talus: autologous chondrocyte implantation versus one-step bone marrow derived cells transplantation. Int Orthop. 2015;39:893–900.
Buda R, Cavallo M, Castagnini F, Cenacchi A, Natali S, Vannini F, Giannini S. Treatment of hemophilic ankle arthropathy with one-step arthroscopic bone marrow-derived cells transplantation. Cartilage. 2015;6:150–5.
Buda R, Castagnini F, Cavallo M, Ramponi L, Vannini F, Giannini S. “One-step” bone marrow-derived cells transplantation and joint debridement for osteochondral lesions of the talus in ankle osteoarthritis: clinical and radiological outcomes at 36 months. Arch Orthop Trauma Surg. 2016;136(1):107–16.
Gobbi A, Chaurasia S, Karnatzikos G, Nakamura N. Matrix-induced autologous chondrocyte implantation versus multipotent stem cells for the treatment of large patellofemoral chondral lesions: a nonrandomized prospective trial. Cartilage. 2015;6:82–97.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Anz, A.W., Pinegar, C.O. (2018). The Role of Stem Cells in Surgical Repair. In: Farr, J., Gomoll, A. (eds) Cartilage Restoration. Springer, Cham. https://doi.org/10.1007/978-3-319-77152-6_13
Download citation
DOI: https://doi.org/10.1007/978-3-319-77152-6_13
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-77151-9
Online ISBN: 978-3-319-77152-6
eBook Packages: MedicineMedicine (R0)