Abstract
A comprehensive clinical assessment is the basis of safe and predictable treatment planning. A systematic approach further ensures that all relevant aspects and factors are included and considered. With the specific focus on the elderly patient, the clinical assessment commences with the first approach for an appointment and the patient’s ability and possible needs connected with attending the dental office. At the first visit, the clinical assessment is divided between obtaining a full patient history, performing a clinical examination and establishing the need for additional investigations. Specifically, for consideration of mandibular implant overdentures, investigations related to existing dentures and denture wearing history are important to establish clear indication for treatment. Similarly, a risk assessment in relation to implant therapy is recommended to ensure that the surgical aspect amongst other is appropriate and that no contraindications exist.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
1 Introduction
The aim of this chapter is to gather the clinical information that is required to safely and predictably plan and provide mandibular implant overdentures. Implant assistance for mandibular dentures is a therapy that is both scientifically and clinically validated, but it is not without risks [1]. Appropriate clinical assessment is therefore mentioned in recommendations for minimum standards of training for dentists who wish to undertake implant treatment (UK Training Standards in Implant Dentistry).
The focus on rehabilitation of the edentulous older patient adds a further important perspective to the clinical assessment. There is no age limit per se to provision of implant treatment [2], and the benefits of implant support for a mandibular denture are extensively documented [3,4,5]. Even so dental implants are still scarcely used in elderly patients and where indicated treatment should be encouraged, whilst patients are still in good health and able to live independently [6]. Barriers to implant treatment may be self-imposed by the patient. It could be through fear of the surgical aspect and it is important to discover this. The clinical assessment will also serve to determine if the implant therapy element is appropriate or whether there are risks and contraindications against doing so. As outlined already in the previous chapters, specific treatment considerations may exist and careful assessment is essential to identifying individual needs and challenges to provision of care.
This chapter sets out a systematic approach to clinical assessment to ensure that all relevant factors are considered. In turn this should assist the process of reaching the clinical diagnoses and indications that will guide the selection of the most appropriate treatment option.
1.1 Clinical Assessment
Clinical assessment includes a number of components. In a systematic approach, these are set out in a logical sequence as seen in Table 6.1. Assessment of the patient’s general status commences from the moment of first contact and continues throughout the assessment. This part will reveal physical and cognitive considerations. Next it is important to establish the patient’s reason for seeking treatment together with any other social, medical and dental information. This is followed by the actual clinical examination together with any additional investigations that may prove necessary or helpful to finally reaching diagnoses and summarising indications for treatment (the radiographic imaging under additional investigations has been covered as a separate topic by itself in the previous chapter). A risk assessment can also be undertaken, and an example of this is offered towards the end of the chapter. Through the chapter, factors that may impact on difficulty of treatment process and risk of complications are marked with  .
.
2 General Status of the Patient: Observations
As already mentioned, age is in itself not a barrier to implant therapy. Equally age is not a prognostic factor for the outcome of denture treatment [7]. However, advancing age and presence of medical conditions are likely to be reflected in both the patient’s physical and cognitive status [8]. In turn these may impact on the patient’s access to dental care and ability to cope with dental procedures in a dental chair. As such it is necessary to consider the needs of the individual throughout the whole treatment process. Useful information can be gained from the moment of first contact. This could be when the patient makes an appointment with the dental office or through a request for a dental visit to the patient’s abode.
2.1 Physical Status
The Seattle Care Pathway for securing oral health in older patients [9] is aimed at a structured, pragmatic and evidence-based approach to assessment, and it is designed to be globally applicable. It offers a helpful point of reference in this context through its Pathway categories which are based on level of dependency. The categories are ‘no dependency’, ‘pre-dependency’, ‘low dependency’, ‘medium dependency’ and ‘high dependency’. These categories are also closely linked with the Canadian Study of Health and Aging (CSHA) frailty scores [10].
The general status of the no dependency patient presents no immediate impediment to implant therapy although there may be other risk factors to be explored as detailed later in this chapter. The pre-dependency/less dependency patients will need more detailed evaluation of their medical status and its potential impact on oral health and implant treatment. The medium dependency patient will need careful investigation of the medical factors that are impacting on oral health before implant therapy can be considered. The health of the high dependency patient together with the difficulties of moving the patient may preclude consideration of implant therapy.
Signs of reduced mobility and frailty may be immediately obvious. The patient may be accompanied as a means of overcoming both of these, and it is sensible to enquire from the outset what measures might be needed to make the patient comfortable in the dental setting. Frailty could further hint at concern about nutritional status and give rise to more detailed history taking on this point.
There may also be clear signs of medical conditions. Examples are shortness of breath associated with chronic obstructive pulmonary disease (COPD), bruising of the skin linked to anticoagulation or changes to hands caused by arthritis. It could also be reduced sight and or hearing which can both impact on effective communication with the patient.
From an oral perspective, it may be immediately obvious that the patient is edentulous. The patient may present with no dentures or only one denture in situ or with dentures that are not restoring the patient’s physiognomy. The psychosocial impact of this is one concern, and the impact on nutritional status is very likely to be another [11].
Arthritic hands and details of the patient’s dress appearance with Velcro bands on shoes instead of shoelaces may hint at diminished dexterity. This is likely to be directly relevant to the patient’s ability to maintain oral hygiene around implants and associated prostheses. In turn, this has an important bearing on the complexity of the dental work that the patient will be able to manage.
The above are helpful in forming an initial if subjective impression of the patient. It should be backed up by more detailed assessment as outlined later in the chapter.
2.2 Personal Interest and Motivation
It is important to assess the patient’s personal interest and motivation for treatment. Even if the patient is unaccompanied, the driving force behind seeking a professional consultation may be a significant other person or event in the background. ‘My wife thinks I need new teeth’ or ‘my daughter is getting married’. The type and source of motivation is also likely to have a bearing on the expectations to outcome of the treatment.
The patient may also be attending at the behest of a relative or, as a decision of physician, care home or home carer. This may be a pointer to the cognitive status of the patient.
2.3 Signs of Anxiety
As for all dental patients, it is important to detect signs or suggestions of anxiety in the patient’s manner. For the older patient, the anxiety could be centred on being able to hear what the dentist is saying or being able to sit comfortably in the dental chair. It is always sensible to listen out for concerns that are expressed at the time of the initial arrangement of the appointment and to enquire from the outset what measures might be needed to make the patient comfortable in the dental setting.
Anxiety could also be linked to the prospect of implant therapy. Many older patients are known to refuse dental implants because of their fear of surgical complications, their feelings of frailty and distrust of the dental profession [12].
It is also important to consider that signs of anxiety could be due to reasons not related to the dental situation. If there is suggestion that this could be the case, the dental practitioner should consider and explore alternative explanations including the possibility of elder abuse.
2.4 Cognitive Status
It may be tempting to see an accompanying person as an immediate help to communication with or about the patient. However, unless there is clear information to the contrary, it is wise to explore and where possible first and foremost maintain direct communication with the patient.
Where the accompanying person has an official role as a guardian, they should be involved in any treatment planning decisions. A carer should also be party to the oral health education that is provided.
A specific reason for involving an accompanying person may be the presence of dementia. A patient with mild cognitive impairment (MCI) may also feel happier if a person of trust is present during the assessment. It will assist recollection and discussion after the consultation. Cognitive considerations have been covered in an earlier chapter, but as a quick reference here, MCI is defined as ‘cognitive decline greater than expected for an individual’s age and education level but not interfering notably with activities of daily life’ [13]. Epidemiological studies suggest a prevalence of 3–19% in adults older than 65 years. MCI can be stable or can even return to normal over time, but more than half progress to dementia within 5 years.
3 Reason for Attending
3.1 Patient’s Concerns
As in all treatment planning, it is very important to be clear on why the patient is seeking dental attention. This may be quite different from the professional findings arising from the ensuing clinical examination [14], and it must feature prominently in the overall treatment considerations and documentation.
The reason for attending is an entry point to gauging the nature and the magnitude of patient’s concerns. These may be specifically dental or more generally tied up with the physical impairment of tooth loss. The impact of tooth loss should not be underestimated [15].
The concerns may be linked to the patient’s daily life and activities such as eating, smiling and speaking [16, 17]. They could also present an impediment to participating in sport or sexual activity. They could even be forcing the patient into avoiding social events altogether—‘I don’t accept dinner invitations for fear of not being able to chew the food that is served’; ‘I don’t trust my denture not to move when I laugh’; and ‘the denture glue does not last long enough for me to go through an afternoon out with my friends’.
3.2 Expectations
The patient may have specific wishes that translate into expectations. Expectations to a new prosthesis can be very high. This has been shown in a study where patients were asked to indicate how satisfied they expected to be with their new prosthesis [18]. The patient may have specific hopes that implant therapy will resolve all of their concerns. This could to some extent be justified as there is evidence that implant-supported overdentures can have a positive impact on social and sexual activity by reducing the patient’s uneasiness [18]. However, expectations may exceed what is realistic. An example is a husband who requests the same implant treatment as his wife. She is very happy with her implant-supported maxillary and mandibular overdentures. Unfortunately, her successful outcome does not mean that implant therapy is indicated or even possible for him. It is therefore important to identify the patient’s expectations from the outset and address them individually to determine to which extent they are realistic and achievable.
Expectations can also be negative and based on apprehension about treatment. These could be due to past dental experiences or a result of fear of potential pain and complications associated with surgery [12]. For many the prospect of being without their denture(s) for even a short period is an immediate barrier to implant therapy. Older people may feel they are not strong enough to go through the surgical procedure. They are worried about infection, period of recovery and that their gum and jaw may be too thin and weak. As such they may feel the risks outweigh the potential benefits.
Studies show that only a limited number of elderly patients are as yet benefitting from the improvement that dental implants can offer for a mandibular denture. Time taken to present and discuss the advantages of implant therapy to older patients who are still in good health and able to live independently [6] is an important healthcare service both to the individual and for spreading the message to the age group in general. It is may also be essential to overcome a patient-imposed barrier to the most appropriate treatment.
4 Patient History
This part of the clinical assessment is intended to elicit any further information from the patient that may be relevant to the treatment planning. It can broadly be divided into three parts aimed at covering and exploring social, medical and dental information not already volunteered by the patient.
4.1 Social Factors
There may be a number of factors that could impact on a patient’s ability and willingness to accept a treatment plan. For older patient who still have work commitments these will need to be considered in the execution of the treatment plan. The patient may also have pre-existing booked events, e.g. holidays that need to be factored in. The importance of support from family and friends is well recognised [12] as is the absence of same. There can also be restrictions on the patient’s freedom if they are acting as a carer for a partner or significant other (Table 6.2).
4.2 Medical Factors
 The patient’s full medical history and current treatment need to be explored and discussed. Medical and pharmacological considerations have been covered in detail in a previous chapter. It should be noted that this point comes ahead of the clinical examination in the assessment sequence. This is to ensure that any medical impediment to the clinical or radiographic examination is picked up here.
The patient’s full medical history and current treatment need to be explored and discussed. Medical and pharmacological considerations have been covered in detail in a previous chapter. It should be noted that this point comes ahead of the clinical examination in the assessment sequence. This is to ensure that any medical impediment to the clinical or radiographic examination is picked up here.
The medical history should include details of current treatment, presence of systemic and local disease, list of prescription medicines and intake of any other over-the-counter or alternative therapy remedies. The medical history should also disclose any allergies and absolute or relative contraindications to dental treatment in general or implant therapy in particular as well as presence of known risk factors.
 Smoking is a proven risk factor for implant therapy [19]. The impact of alcohol consumption is less clear but could play a contributory role in terms of malnutrition, poor oral hygiene and compliance in terms of risk [20]. Smoking is classified as heavy when the patient smokes more than ten cigarettes per day. The guidelines for maximum units of alcohol per week vary between countries, but the general trend is in favour of a reduction.
Smoking is a proven risk factor for implant therapy [19]. The impact of alcohol consumption is less clear but could play a contributory role in terms of malnutrition, poor oral hygiene and compliance in terms of risk [20]. Smoking is classified as heavy when the patient smokes more than ten cigarettes per day. The guidelines for maximum units of alcohol per week vary between countries, but the general trend is in favour of a reduction.
Where malnutrition is suspected or it forms the basis of a medical referral for dental treatment, further information is needed. This is to ascertain the specific limitations imposed by the dental status on diet and nutrition as well as the impact on the patient’s health. Provision of an implant-supported mandibular overdenture does not in itself ensure a positive effect on nutrition compared to conventional complete dentures [21]. However, a customised diet advice may have a beneficial effect [22]. Through better chewing ability, the mandibular implant overdenture wearer is more likely to include fresh whole fruits and vegetables in their diet (Table 6.3).
4.3 Dental Factors
 The patient’s dental history is relevant to throwing light on potential dental risk factors. It should also include enquiry about previous denture wearing experience. The dental risk factors include reason for tooth loss, history or present evidence of parafunctional habits and previous implant history or experience.
The patient’s dental history is relevant to throwing light on potential dental risk factors. It should also include enquiry about previous denture wearing experience. The dental risk factors include reason for tooth loss, history or present evidence of parafunctional habits and previous implant history or experience.
Amongst the reasons for tooth loss, a history of  periodontal disease is particularly relevant. Patient susceptibility does not change simply because teeth have been removed [23]. A history of caries can also throw light on the patient’s understanding of dental disease, its prevention and past compliance.
periodontal disease is particularly relevant. Patient susceptibility does not change simply because teeth have been removed [23]. A history of caries can also throw light on the patient’s understanding of dental disease, its prevention and past compliance.
Bruxism is a documented risk factor for the durability of implant prostheses and components. It is also a factor to consider in choice of implant loading protocols. Confirmed presence would favour conventional loading and less ambitious surgical approaches.
 Details of previous implant therapy may disclose a history of complications or failure.
Details of previous implant therapy may disclose a history of complications or failure.
Current oral medicine concerns or treatment also comes under dental factors. These would include diseases of the oral mucosa such as denture stomatitis and  lichen planus.
lichen planus.
Based on current dental status, the consideration of denture wearing experience can be divided into two categories:
-
Partially edentulous looking at transition to edentulous
These patients may have no previous experience. The current trend is that the older population will keep teeth longer. The prosthodontically accepted recommendation to reduce the dental burden of maintenance through shortened dental arch solutions (SDA) [24, 25] may have obviated need for partial dentures. The age at which the transition to edentulous becomes necessary may therefore be advanced and linked to sudden changes in the patient’s circumstances. This could be due to changes in medical factors or in level of dependency that in turn leads to significant change in the patient’s own ability to maintain the residual dentition.
If the patient does have partial denture wearing experience, it is important to learn from both positive and negative comments. Positive comments could point to which implant configurations to explore in order to carry forward a hitherto successful partial denture design. From negative comments, there may be diagnostic measures to be considered under additional investigations to address any previously unsuccessful partial denture aspects.
-
Already edentulous
These patients can be divided into patients with short-term only experience versus long-term denture wearing. The short-term experience group may be patients who have recently made the transition to conventional complete dentures and are still struggling with coping with conventional dentures, in particular the mandibular denture. For the long-term group, the denture wearing experience as a whole may be favourable, but more recent changes due to advanced alveolar atrophy may have affected retention, stability or comfort of the denture(s) (Table 6.4).
5 Clinical Examination
The systematic approach to the assessment overall should also be developed and followed for the clinical examination. This ensures that a broader evaluation is undertaken even if the patient presents with a request for a specific focus for treatment. The aim is to record any and all clinical information that is relevant to reaching diagnosis and to detect any conditions outside of the normal range.
It is important to document what has been examined and what the findings are. A systematic clinical examination would include both an extraoral and an intraoral examination. In the context of mandibular overdentures, the examination would also include evaluation of the prosthodontic and surgical aspects. The categories to be considered are set out in Table 6.5.
5.1 Extraoral
5.1.1 Craniomandibular Examination
This involves the examination of the temporomandibular joints and muscles of mastication to detect any symptoms or signs of pain or dysfunction. If any are present, etiological factors should be evaluated together with their possible consequences for prosthodontic rehabilitation [26]. The range of opening of the mandible and range of lateral and protrusive movement should be checked together with deviations during the movements. Deviations and audible sounds such as click and crepitation suggest internal derangement in the joints. Limitations in the range of movement could be a sign of muscle tension, but it could also be a further sign of internal joint derangement.
 Limited opening, for example, can interfere with access for treatment and lead to strain and further discomfort to the patient. Internal derangement in the joints can put a question mark against the most suitable joint position to use for jaw registration. It should be noted that the prevalence of signs and symptoms of temporomandibular disorders amongst edentulous patients has been reported to be low [27]. This prevalence applies to both denture and non-denture wearers.
Limited opening, for example, can interfere with access for treatment and lead to strain and further discomfort to the patient. Internal derangement in the joints can put a question mark against the most suitable joint position to use for jaw registration. It should be noted that the prevalence of signs and symptoms of temporomandibular disorders amongst edentulous patients has been reported to be low [27]. This prevalence applies to both denture and non-denture wearers.
The extraoral examination should also include palpation of the regional lymph nodes.
This palpation may detect a localised infection. It could also detect more serious underlying conditions.
Movement disorders associated with, for example, Parkinson’s disease may also manifest themselves in the face and jaw. They could result in both an increase and a decrease of movement. This would be an important factor to take into consideration for the stability and retention of the prostheses.
5.1.2 Facial Examination
This involves the examination of facial proportions and symmetry, midline, lip support and vertical dimension. The lip support and vertical dimension of occlusion are particularly relevant to the partially and completely edentulous patient. Tooth loss and associated atrophy of the alveolar process will lead to a reduction in both. The assessment therefore centres on whether the existing prostheses are restoring both parameters correctly. Often the lip support and the vertical dimension are inadequate. This may be associated with the angular cheilitis or inflammation in the corners of the mouth caused by bacteria or fungal infections.
The lip support and vertical dimension may also be increased. To detect this error, patients with a removable dental prosthesis should be evaluated both with and without the existing prosthesis.
The facial examination should also note any other signs of pathology of the lips and face. This could be signs of paralysis, changes in colour or skin lesions that should be investigated further (Fig. 6.1).
5.1.3 Dentolabial Examination
This part centres on assessing facial proportions, upper and lower lip support, competency and lines at rest and in smile. It also includes assessment of position and relationship of upper and lower incisors. The position of the incisors is guided by aesthetics and functional requirements. It is helpful to observe the incisors during speech, and phonetics can provide a useful guide to incisal edge position. However, additional investigation via a diagnostic set-up may be needed to assess these parameters properly.
5.2 Intraoral Examination
5.2.1 Oral Cavity and Mucosa
Regardless of the patient’s primary reason for seeking dental attention, regular screening for oral pathology is recognised as an important factor in early detection and diagnosis of oral cancer; early intervention is likely to result in less extensive and more effective treatment. Oral cancer is the largest group of head and neck cancers. It is more common in men than in women, and the vast majority of cases are in people over the age of 50 [28, 29].
In a specific report on the geriatric population, the non-neoplastic lesions outnumbered the neoplastic [30]. The five most prevalent oral lesions in descending order of frequency were squamous cell carcinoma, focal fibrous hyperplasia (irritation fibroma), radicular cyst, osteomyelitis and epithelial dysplasia. The site of predilection was the labial/buccal mucosa, followed by the gingiva, mandibular bone, tongue and maxillary bone, respectively. Figure 6.2a shows a sessile lump that could be related to an underlying saliva gland. It could also interfere with the positioning of a post-dam compression area just anterior to the hard/soft palate vibration line.
Diseases of the oral mucosa may be relevant to both the denture aspect of treatment and to implant therapy. High success rates have been demonstrated for implants in patients affected by these diseases, but the severity of the diseases and medical complications should be evaluated [31]. The diseases may also compromise the patient’s ability to maintain adequate oral hygiene. Examples of diseases that affect the oral mucosa are lichen planus, epidermolysis bullosa and Sjögren’s syndrome.
The subjective sensation of dry mouth is referred to as xerostomia. This disorder is part of Sjögren’s syndrome, but it is also associated with medication, systemic diseases, other pathologies of the salivary glands and head and neck radiotherapy. Xerostomia is a side effect of a large number of drugs, and 70% of adults who take some kind of medication can suffer from it. Xerostomia has clear, negative effects on oral-dental tissue. Some of the best known side effects include demineralisation of tooth enamel, rampant caries, superinfections caused by fungal diseases (candidiasis), reactive gingival enlargement due to dehydration and loss of salivary antimicrobial properties. Xerostomia can also influence ingestion, swallowing and speech articulation, thus negatively affecting the quality of life of people suffering from it [32]. For documentation purposes, the extent of dry mouth should be described, for example, by referral to a dry mouth scale [33], and management should be considered as part of the subsequent treatment planning.
Mucosal findings may also be more specifically related to the existing dentures. The prevalence for at least one mucosal lesion has been reported as 54% [34]. The same study found the three most common lesions to be angular cheilitis (34%), traumatic ulcers (15%) and denture stomatitis (14%) amongst 84 elderly denture wearers recruited from geriatric residences and day care centres. In some cases of long-standing mucosal issues, the changes can be so marked as to be sinister in appearance (Fig. 6.2b). As a first measure, further questioning of the patient together with examination of the denture hygiene as well as the dentures(s) in situ may confirm a denture-induced diagnosis [35]. If concern remains, however, appropriate further investigation is required and by referral if necessary. The changes may also require some form of surgical correction, but often the situation will improve through appropriate adjustment of the denture.
A white crest line in the cheek referred to as linea alba and scalloping along the lateral border of the tongue may indicate tooth contact during  parafunction.
parafunction.
5.2.2 Residual Dentition
The presence of teeth can provide very useful information for the overall assessment and subsequent treatment planning. The patient’s level of  oral hygiene can be assessed together with evidence of
oral hygiene can be assessed together with evidence of  present and past dental disease. Findings include caries, endodontic issues, periodontal disease and tooth surface loss through mechanical attrition or chemical erosion. Evaluation of whether disease is active or controlled is important for the subsequent treatment planning. The presence of localised acute or chronic infection should be noted.
present and past dental disease. Findings include caries, endodontic issues, periodontal disease and tooth surface loss through mechanical attrition or chemical erosion. Evaluation of whether disease is active or controlled is important for the subsequent treatment planning. The presence of localised acute or chronic infection should be noted.
Even a reduced dentition may offer helpful prosthodontic information about the facial profile, incisor relationship, occlusal classification and vertical dimension of occlusion (Fig. 6.3). It is important to document this information in order that it can be used for reference after the teeth have been removed.
It could also be important to determine whether natural teeth could serve as the overdenture abutments, thereby avoiding the need for implant therapy. This could be very relevant in patients who are at risk of medication-related osteonecrosis of the jaw (MRONJ).  MRONJ in connection with implant placement is relatively rare, and the risk is considered similar to that of tooth extraction. However, in view of the potentially serious consequences of MRONJ, patients treated with antiresorptive drugs such as high-dose intravenous bisphosphonates are not candidates for implant therapy [36].
MRONJ in connection with implant placement is relatively rare, and the risk is considered similar to that of tooth extraction. However, in view of the potentially serious consequences of MRONJ, patients treated with antiresorptive drugs such as high-dose intravenous bisphosphonates are not candidates for implant therapy [36].
5.3 Prosthodontic Assessment
The anatomical situation of residual ridges has a bearing on the stability and retention than can be achieved particularly for the mandibular denture. Both the height and the shape of the residual ridge play a part, and continued loss of alveolar bone over time can cause previously stable dentures to become ill-fitting. It has been reported that more than 50% of those with mandibular complete dentures may have problems with stability and retention [4].
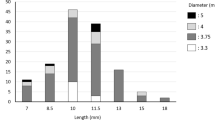
There are a number of descriptive classifications for the extent of atrophy of the alveolar ridges. One of these is the often cited Cawood and Howell classification [37] which describes five different stages of alveolar atrophy of the mandible classified as II to VI. A class II ridge is equivalent to the alveolar bone around a retained healthy root with a sound bone support. A mandibular class III retains a good, high and rounded ridge form, whereas class IV is the often seen knife-edge ridge shape. Class V is a flat ridge, and class VI is concave with atrophy extending beyond the original alveolar ridge into the basal bone of the mandible (Fig. 6.4).
In addition to the ridge classification, it is highly relevant to note encroachment by muscles and ligaments on the denture-supporting area. Equally, areas of flabby soft tissues with no underlying bony support will impact on both denture construction and performance and scope for implant placement (Fig. 6.5).
The mucosal status of denture-supporting areas changes in the older patient, and the tissues are likely to be thinner, less resilient and more friable.  Specifically for implant therapy, the evidence as to the true value of attached, keratinised mucosa in the formation of a stable peri-implant cuff is equivocal [38]. It is suggested, however, that the patient will find it easier to perform oral hygiene around the implant if it has a keratinised cuff. In turn, this may reduce susceptibility to inflammation, recession of the peri-implant mucosa and crestal bone loss.
Specifically for implant therapy, the evidence as to the true value of attached, keratinised mucosa in the formation of a stable peri-implant cuff is equivocal [38]. It is suggested, however, that the patient will find it easier to perform oral hygiene around the implant if it has a keratinised cuff. In turn, this may reduce susceptibility to inflammation, recession of the peri-implant mucosa and crestal bone loss.
5.3.1 Restorative Space
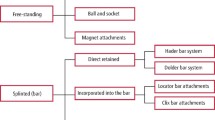
In a prosthodontically driven approach to implant therapy, the desired parameters of the definitive prostheses determine the appropriate implant configurations and individual implant positions. This ensures that the restorative dimensions are adequate to accommodate the spatial dimensions of both the implant and denture attachment components together with any internal denture reinforcement that may be required. Assessment and definition of the restorative space is therefore a very important consideration.
 The interarch distance has a direct bearing on the vertical dimension of the prostheses and hence the volume for attachment components within. In a Cawood and Howell class III situation, the benefits of a good high ridge may be countered by limited restorative space in which to accommodate denture teeth, body and attachments (Fig. 6.5).
The interarch distance has a direct bearing on the vertical dimension of the prostheses and hence the volume for attachment components within. In a Cawood and Howell class III situation, the benefits of a good high ridge may be countered by limited restorative space in which to accommodate denture teeth, body and attachments (Fig. 6.5).
Conversely a class V or class VI ridges are likely to have a correspondingly greater restorative space. Construction of a stable denture in these situations can be challenging. Irrespective of whether implant assistance is planned, the prosthesis stability, comfort and function should be maximised through physiologically optimal denture contours and physiologically appropriate denture tooth arrangement [39].
5.3.2 Existing Dentures
The aim of any new dentures is to restore the patient to optimal aesthetics, function and quality of life. As such the evaluation of the patient’s existing dentures, both previous and present, against established design principles can provide very helpful pointers to changes required or compromises to be accepted. For example, the patient may present with recent conventional complete dentures constructed in line with optimal design principles, but concerns persist regarding retention, stability and support of one or both dentures. At the other end of the spectrum, the dentures may be unsatisfactory from both a patient and professional point of view. It is also possible that the patient has previous dentures that used to be more successful than the present ones.
The denture evaluation can be divided into assessment of:
-
Fit and extension of base
-
Both have a direct bearing on denture support and retention. The examination should determine whether the base has a retentive seal and (Fig. 6.6) the extent to which the existing denture base is making use of the support that is available. Scope for improvement should also be assessed.
-
-
Facial support and position of incisors
-
Restoration of the patient’s physiognomy requires correct facial support. This is achieved through a combination of upper and lower lip support. The position of the incisors is guided by a combination of aesthetic and functional requirements (Fig. 6.7).
-
-
Jaw relationship
-
A comfortable three-dimensional relationship between the upper and lower jaws requires a correct lower face height and vertical dimension of occlusion as well as a comfortable jaw position.
-
-
 Denture occlusion
Denture occlusion-
This should be stabilising the position of the mandible against the maxilla. This is important during both static and dynamic occlusion. The posterior teeth should transfer the occlusal load as effectively as possible to the underlying ridges to aid stability of the dentures and thereby enhance chewing efficiency.
-
-
Features and contours of denture body
-
These should restore the missing tissue volume and assist the patient with muscular control of the denture. They should avoid contours and crevices that may encourage retention of food and buildup of extrinsic stains and complicate oral hygiene removal of bacterial biofilm (Fig. 6.8). Obvious signs of wear and damage should be noted.
-
The patient’s bite force should be assessed (Fig. 6.9). As a rule of thumb, the greater the bite force, the more implant support is indicated for the mandibular overdenture.
Patient satisfaction with a well-constructed maxillary denture can be equal to satisfaction after implant therapy [40]. Even so in an assessment for MI OVD, the potential impact on the performance and satisfaction, positive or negative, of the opposing conventional maxillary denture should be considered.
5.4 Surgical Assessment
Where the restorative assessment involves the entire prostheses, the surgical assessment for implant therapy is more site specific. The aim is to relate the prosthodontically preferred implant positions to the anatomical situation of soft and hard tissues at the prospective sites. In addition to the aforementioned presence or absence of keratinised mucosa, the  evaluation includes assessment of bone volume and proximity to vital structures such the mental foramen and mandibular canal. This assessment has already been covered in detail in the previous chapter in connection with additional investigations via radiographic imaging.
evaluation includes assessment of bone volume and proximity to vital structures such the mental foramen and mandibular canal. This assessment has already been covered in detail in the previous chapter in connection with additional investigations via radiographic imaging.
6 Radiographic Imaging (See Previous Chapter)
7 Additional Investigations
The need for and value of additional investigations have been mentioned throughout the chapter.
7.1 Diet-Related Investigations
-
Testing masticatory efficiency
-
Diet investigation and analyses [43]
-
Diminished masticatory efficiency may lead to a change in diet. Equally, the restoration of masticatory function via mandibular implant overdenture will not in itself necessarily lead to an improved diet. A diet analysis at the assessment stage can therefore disclose valuable information regarding the need for both functional denture improvement and professional diet advice [44].
-
7.2 Denture-Related Investigations
Diagnostic approach to new dentures:
Can be based on:
-
Testing possible changes for improvements by reversible measures
-
This could be by addition of wax to existing dentures to test scope for improvement of denture base extension, lip support and vertical dimension of occlusion (Fig. 6.10).
-
-
Use of photos from the patient’s dentate past
-
Useful information about the shape and size of the patient’s natural teeth, incisal relationship and facial contours can be gleaned from photos.
-
-
Dental information from dentate relatives
-
Guidance to tooth size, shape and arrangement can in some cases be gained from relatives.
-
Can lead to:
-
Trial/training bases
-
For patients who have a history of difficulty in accepting the presence of dentures, a gradual training process via training base can be very helpful.
-
-
Diagnostic set-up
-
This is essential in a prosthodontically driven approach to implant planning to ensure that the implant placement is determined by and compatible with the planned denture.

-
-
Radiographic/surgical templates
-
A diagnostic set-up or a successful existing denture can also be the basis for both radiographic and surgical templates to be used in implant planning and to guide placement.

-
8 Diagnoses and Specific Indications for Implant Therapy
Once the clinical assessment is completed, the information is synthesised into diagnoses. In addition to determining the need and scope for treatment, the diagnoses will also be the basis of defining indications for prosthodontic treatment and specific indications for implant therapy. With the potential risks of implant therapy in mind, it is a good idea at this point to consider some form of risk assessment.
9 Risk Assessment
It is important to remember that implant therapy is an elective treatment modality with the purpose of facilitating prosthodontic rehabilitation. By its nature, implant placement is also an invasive treatment. Whilst implant therapy is now considered routine, it is clear that implant therapy also presents with differing levels of difficulty and differing degrees of risk for prosthodontic and surgical complications. To ensure that the patient or a legal guardian is able to give full informed consent to treatment, it is important to document that both degree of treatment difficulty and potential risks have been assessed and discussed.
Amongst the information collected during the clinical assessment, there are findings that could influence/impact on treatment complexity and risk modifiers. These have been marked by the symbol  . These factors can be used to assess difficulty of the treatment process and risk of complication involved in prospective implant therapy.
. These factors can be used to assess difficulty of the treatment process and risk of complication involved in prospective implant therapy.
The International Team for Implantology (www.iti.org) offers a free online risk assessment tool (https://academy.iti.org) for this purpose. The tool is based on a book entitled The SAC Classification in Implant Dentistry [45], and it offers a systematic assessment to identify and document modifying factors and risks, thereby allowing contingency planning to be undertaken to minimise risks and undesirable outcomes (Fig. 6.11).
The tool poses a series of questions, and the user selects the most appropriate answer from a number of options. The patient factors highlighted by  through this clinical assessment chapter (summarised in Table 6.6) will provide the patient-specific information to guide which answer option to select. Depending on the selected answer, the underlying algorithm of the tool will pose further questions until a classification of the case as straightforward, advanced or complex can be offered. The tool also lists modifying factors that should be considered in the further treatment planning.
through this clinical assessment chapter (summarised in Table 6.6) will provide the patient-specific information to guide which answer option to select. Depending on the selected answer, the underlying algorithm of the tool will pose further questions until a classification of the case as straightforward, advanced or complex can be offered. The tool also lists modifying factors that should be considered in the further treatment planning.
Conclusion
The clinical assessment is a process of information gathering. It is a comprehensive undertaking, and a systematic approach is helpful to ensure that all relevant aspects have been included. With the particular focus on the older patient and the possibility of implant therapy, this includes consideration of specific factors as well as a risk assessment. A complete clinical assessment forms an important precursor to effective treatment planning and also to ensuring a safe and predictable outcome of the ensuing treatment.
References
Doundoulakis JH, Eckert SE, Lindquist CC, Jeffcoat MK. The implant-supported overdenture as an alternative to the complete mandibular denture. J Am Dent Assoc. 2003;134:1455–8.
Park JC, Baek WS, Choi SH, Cho KS, Jung UW. Long-term outcomes of dental implants placed in elderly patients: a retrospective clinical and radiographic analysis. Clin Oral Implants Res. 2017;28(2):186–91.
Feine JS, Carlsson GE, Awad MA, Chehade A, Duncan WJ, Gizani S, et al. The McGill Consensus Statement on Overdentures. Montreal, Quebec, Canada. May 24-25, 2002. Int J Prosthodont. 2002;15:413–4.
Thomason JM, Kelly SA, Bendkowski A, Ellis JS. Two implant retained overdentures—a review of the literature supporting the McGill and York consensus statements. J Dent. 2012;40:22–34.
British Society for the Study of Prosthetic Dentistry. The York consensus statement on implant-supported overdentures. Eur J Prosthodont Restor Dent. 2009;17:164–5.
Muller F, Salem K, Barbezat C, Herrmann FR, Schimmel M. Knowledge and attitude of elderly persons towards dental implants. Gerodontology. 2012;29:e914–23.
Critchlow SB, Ellis JS. Prognostic indicators for conventional complete denture therapy: a review of the literature. J Dent. 2010;38:2–9.
Katsoulis J, Schimmel M, Avrampou M, Stuck AE, Mericske-Stern R. Oral and general health status in patients treated in a dental consultation clinic of a geriatric ward in Bern, Switzerland. Gerodontology. 2012;29:e602–10.
Pretty IA, Ellwood RP, Lo EC, MacEntee MI, Muller F, Rooney E, et al. The Seattle Care Pathway for securing oral health in older patients. Gerodontology. 2014;31(Suppl 1):77–87.
Rockwood K, Song X, MacKnight C, Bergman H, Hogan DB, McDowell I, et al. A global clinical measure of fitness and frailty in elderly people. Can Med Assoc J. 2005;173:489–95.
Gil-Montoya JA, Ponce G, Sanchez Lara I, Barrios R, Llodra JC, Bravo M. Association of the oral health impact profile with malnutrition risk in Spanish elders. Arch Gerontol Geriatr. 2013;57(3):398–402.
Ellis JS, Levine A, Bedos C, Mojon P, Rosberger Z, Feine J, et al. Refusal of implant supported mandibular overdentures by elderly patients. Gerodontology. 2011;28:62–8.
Gauthier S, Reisberg B, Zaudig M, Petersen RC, Ritchie K, Broich K, et al. Mild cognitive impairment. Lancet. 2006;367:1262–70.
Awad MA, Feine JS. Measuring patient satisfaction with mandibular prostheses. Community Dent Oral Epidemiol. 1998;26:400–5.
Davis DM, Fiske J, Scott B, Radford DR. The emotional effects of tooth loss: a preliminary quantitative study. Br Dent J. 2000;188:503–6.
Hyland R, Ellis J, Thomason M, El-Feky A, Moynihan P. A qualitative study on patient perspectives of how conventional and implant-supported dentures affect eating. J Dent. 2009;37:718–23.
Trulsson U, Engstrand P, Berggren U, Nannmark U, Branemark PI. Edentulousness and oral rehabilitation: experiences from the patients’ perspective. Eur J Oral Sci. 2002;110:417–24.
Heydecke G, Thomason JM, Awad MA, Lund JP, Feine JS. Do mandibular implant overdentures and conventional complete dentures meet the expectations of edentulous patients? Quintessence Int. 2008;39:803–9.
Heitz-Mayfield LJ, Huynh-Ba G. History of treated periodontitis and smoking as risks for implant therapy. Int J Oral Maxillofac Implants. 2009;24(Suppl):39–68.
Ekfeldt A, Christiansson U, Eriksson T, Linden U, Lundqvist S, Rundcrantz T, et al. A retrospective analysis of factors associated with multiple implant failures in maxillae. Clin Oral Implants Res. 2001;12:462–7.
Awad MA, Morais JA, Wollin S, Khalil A, Gray-Donald K, Feine JS. Implant overdentures and nutrition: a randomized controlled trial. J Dent Res. 2012;91:39–46.
Ellis JS, Elfeky AF, Moynihan PJ, Seal C, Hyland RM, Thomason M. The impact of dietary advice on edentulous adults’ denture satisfaction and oral health-related quality of life 6 months after intervention. Clin Oral Implants Res. 2010;21:386–91.
Quirynen M, Van Assche N. Microbial changes after full-mouth tooth extraction, followed by 2-stage implant placement. J Clin Periodontol. 2011;38:581–9.
Kayser AF. Shortened dental arches and oral function. J Oral Rehabil. 1981;8:457–62.
Gerritsen AE, Witter DJ, Bronkhorst EM, Creugers NH. An observational cohort study on shortened dental arches—clinical course during a period of 27-35 years. Clin Oral Investig. 2013;17:859–66.
Chisnoiu AM, Picos AM, Popa S, Chisnoiu PD, Lascu L, Picos A, et al. Factors involved in the etiology of temporomandibular disorders—a literature review. Clujul Med. 2015;88:473–8.
Dervis E. Changes in temporomandibular disorders after treatment with new complete dentures. J Oral Rehabil. 2004;31:320–6.
Scully C, Kirby J. Statement on mouth cancer diagnosis and prevention. Br Dent J. 2014;216:37–8.
Petersen PE. Oral cancer prevention and control—the approach of the World Health Organization. Oral Oncol. 2009;45:454–60.
Dhanuthai K, Rojanawatsirivej S, Somkotra T, Shin HI, Hong SP, Darling M, et al. Geriatric oral lesions: a multicentric study. Geriatr Gerontol Int. 2016;16(2):237–43.
Candel-Marti ME, Ata-Ali J, Penarrocha-Oltra D, Penarrocha-Diago M, Bagan JV. Dental implants in patients with oral mucosal alterations: an update. Med Oral Patol Oral Cir Bucal. 2011;16:e787–93.
Miranda-Rius J, Brunet-Llobet L, Lahor-Soler E, Farre M. Salivary secretory disorders, inducing drugs, and clinical management. Int J Med Sci. 2015;12:811–24.
Challacombe SJ, Proctor GB. Clinical assessment. Br Dent J. 2014;217:486.
Martori E, Ayuso-Montero R, Martinez-Gomis J, Vinas M, Peraire M. Risk factors for denture-related oral mucosal lesions in a geriatric population. J Prosthet Dent. 2014;111:273–9.
Freitas JB, Gomez RS, De Abreu MH, Ferreira EFE. Relationship between the use of full dentures and mucosal alterations among elderly Brazilians. J Oral Rehabil. 2008;35:370–4.
Ruggiero SL, Dodson TB, Fantasia J, Goodday R, Aghaloo T, Mehrotra B, et al. American Association of Oral and Maxillofacial Surgeons position paper on medication-related osteonecrosis of the jaw—2014 update. J Oral Maxillofac Surg. 2014;72:1938–56.
Cawood JI, Howell RA. A classification of the edentulous jaws. Int J Oral Maxillofac Surg. 1988;17:232–6.
Wennstrom JL, Derks J. Is there a need for keratinized mucosa around implants to maintain health and tissue stability? Clin Oral Implants Res. 2012;23(Suppl 6):136–46.
Cagna DR, Massad JJ, Schiesser FJ. The neutral zone revisited: from historical concepts to modern application. J Prosthet Dent. 2009;101:405–12.
Thomason JM, Heydecke G, Feine JS, Ellis JS. How do patients perceive the benefit of reconstructive dentistry with regard to oral health-related quality of life and patient satisfaction? A systematic review. Clin Oral Implants Res. 2007;18:168–88.
Ribeiro JA, de Resende CM, Lopes AL, Mestriner W Jr, Roncalli AG, Farias-Neto A, et al. Evaluation of complete denture quality and masticatory efficiency in denture wearers. Int J Prosthodont. 2012;25:625–30.
Oliveira NM, Shaddox LM, Toda C, Paleari AG, Pero AC, Compagnoni MA. Methods for evaluation of masticatory efficiency in conventional complete denture wearers: a systematized review. Oral Health Dent Manag. 2014;13:757–62.
Moynihan PJ, Bradbury J, Müller F. Dietary consequences of oral health in frail elders. In: MI ME, Müller F, Wyatt C, editors. Oral healthcare and the frail elder: a clinical perspective. Ames: Wiley-Blackwell; 2011. p. 73–95.
Müller F, Nitschke I. Oral health, dental state and nutrition in older adults. Zeitschrift für Gerontologie und Geriatrie. 2005;38:334–41.
Dawson A, Chen S. The SAC Classification in implant dentistry. Berlin: Quintessence Publishing Co. Ltd. 2009.
Further Reading
The SAC Classification in Implant Dentistry jointly published by the ITI and the Quintessence Publishing Group (Dawson and Chen 2009)
Training standards in implant dentistry: Faculty of General Dental Practice, The Royal College of Surgeons of England. Available from: http://www.fgdp.org.uk/pdf/training_stds_imp_dent_guide_2008.pdf; 2008
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Stilwell, C. (2018). Clinical Assessment of Edentate Elders for Mandibular Implant Overdentures. In: Emami, E., Feine, J. (eds) Mandibular Implant Prostheses. Springer, Cham. https://doi.org/10.1007/978-3-319-71181-2_6
Download citation
DOI: https://doi.org/10.1007/978-3-319-71181-2_6
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-71179-9
Online ISBN: 978-3-319-71181-2
eBook Packages: MedicineMedicine (R0)








 Denture occlusion
Denture occlusion






