Abstract
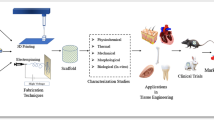
Polymeric, ceramic and hybrid material-based three-dimensional (3D) scaffold or matrix structures are important for successful tissue engineering. While the number of approaches utilizing the use of cell-based scaffold and matrix structures is constantly growing, it is essential to provide a framework of their typical preparation and evaluation for tissue engineering. This chapter describes the fabrication of 3D scaffolds using two-photon polymerization, decellularization and cell encapsulation methods and easy-to-use protocols allowing assessing the cell morphology, cytotoxicity and viability in these scaffolds.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
To date, the number of scaffold materials and fabrication methods proposed for tissue engineering has significantly increased [1,2,3,4,5,6,7,8,9,10,11,12,13,14,15]. To create an “ideal” scaffold, most scientists try to mimic the native extracellular matrix at the nanoscale level. Therefore, this scaffold should promote cell attachment, proliferation, and differentiation, deliver and retain cells and growth factors, ensure nutrient and oxygen delivery and optimum mechanical and biological environment for tissue regeneration [2, 3].
The most frequently used for tissue engineering are electrospinning, freeze drying, decellularization, and laser-based techniques (Table 5.1). However, this chapter mostly focuses on three methods of scaffold fabrication (two-photon polymerization, decellularization, and cell encapsulation) in order to show the main trends in this field and to present different approaches.
All these methods (two-photon polymerization, decellularization, and cell encapsulation) have their specific limitations. For instance, two-photon polymerization is relatively expensive and permits only the formation of microscale-sized scaffolds. Decellularized materials can cause serious infectious diseases, because the process of their production requires animal or human tissues and organs, which can be contaminated with prions, viruses, bacteria, or fungi. When the cells are encapsulated within a gel, it is hard to manipulate with gel structure and mechanical properties. Nevertheless, two-photon polymerization, decellularization, and cell encapsulation enable the fabrication of biocompatible and biodegradable structures, which can be used to achieve a particular goal in tissue engineering. Their role in modern tissue engineering cannot be overestimated.
This chapter aims to describe the 3D scaffold fabrication using three different methods and protocols of cell morphology and cytotoxicity assessment via SEM, Live/Dead staining, including confocal microscopy, and MTT-assay.
2 Materials
Prepare all solutions using deionized water and analytical grade reagents. Prepare and store all reagents at room temperature (unless indicated otherwise). Diligently follow all waste disposal regulations when disposing waste materials. We do not recommend adding sodium azide to the reagents. (see Note 1 ).
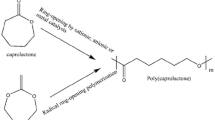
2.1 Reactive Photo-Curing System
Important: preparation and handling of photosensitive monomer composition as well as two-photon polymerized (2PP) scaffolds fabrication should be performed in a yellow light photochemical lab environment.
-
1.
Resolving tetrafunctional polylactides with terminal methacrylic groups (PLA): Add 1.2 mL of dichloromethane to 600 mg of PLA. Weight 6 mg of photoinitiator powder and mix on a magnetic stirrer until PLA and photoinitiator are completely dissolved. Store at 4–8 °C in brown glass bottles wrapped with Parafilm, no longer than one month.
-
2.
IRGACURE® 2959, IRGACURE® 369 (Ciba, Germany), Michler’s ketone (Sigma-Aldrich, St. Louis, MO, USA) (see Note 2 ).
-
3.
Glass coverslips.
2.2 Cell Cultures and Medium
All solutions, glassware, etc., should be sterile and all procedures should be carried out under aseptic conditions and in the sterile environment of a laminar flow cabinet.
-
1.
L929 mouse fibroblast cell line (see Note 3 ).
-
2.
Human adipose-derived stem cells (hASCs) (see Notes 3 , 4 ).
-
3.
Growth medium: DMEM/F12, 10% fetal bovine serum, 1% penicillin-streptomycin. Store at 4 °C for no longer than two weeks.
-
4.
TrypLE Express Enzyme (1X) (Gibco BRL, Bethesda, MD, USA) (see Note 5 ).
-
5.
Sterile phosphate buffered saline (PBS), without calcium and magnesium.
-
6.
Trypan Blue: 0.4% solution in water.
-
7.
75 cm2 cell culture flask.
-
8.
Petri dishes or 24, 48-well plates.
-
9.
Glass-bottom Petri dishes (see Note 6 ).
2.3 Fibrin Gel Components
All solutions and glassware, should be sterile and all procedures should be carried out under aseptic conditions and in the sterile environment of a laminar air flow HEPA-filter cabinet.
-
1.
Fibrinogen solution: gradually dissolve 1 g of fibrinogen in 40 mL sterile PBS at 37 °C (see Note 7 ) under aseptic conditions to achieve the concentration 25 mg/mL. Aliquot into Eppendorf microtubes (0.5 and/or 1.0 mL). Store at −20 °C in tubes wrapped with Parafilm.
-
2.
Thrombin stock solution: dissolve 1 KU thrombin in 10 mL sterile PBS under aseptic conditions to make stock concentration of 100 U/mL. Aliquot into Eppendorf tubes (300 μL or less). Store at −20 °C in tubes wrapped with Parafilm.
-
3.
Thrombin solution: add 50 μL thrombin stock solution to 950 μL sterile PBS and mix (see Note 8 ).
2.4 Material and Agents for Decellularization
-
1.
Bovine pericardium (see Note 9 ).
-
2.
Sodium dodecyl sulfate (SDS): 0.25% solution in hypotonic buffer (see Note 10 ). Store at 4 °C, no longer than 1 year.
-
3.
Distilled water.
-
4.
Hypotonic buffered solution: 10 mM Tris-HCl, pH 7.5. Store at 4 °C, no longer than one year.
-
5.
Phosphate buffered saline (PBS).
-
6.
Hypertonic buffered solution: mix 120 mL of 5 M NaCl, 4 mL of 1 M MgSO4, 2 mL of 0.5 M EDTA, 10 mL of 1 M HEPES, add distilled water to 900 mL. Adjust pH to 7.0 and add distilled water to 1000 mL. Store at 4 °C, no longer than one year (see Note 11 ).
2.5 MTT-Assay Components
-
1.
96-well plate.
-
2.
MTT solution: dissolve MTT (3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazoliumbromide) in MEM without supplements and without phenol red at a concentration of 1 mg/mL. Sterilize it using a syringe filter with 0.22 μm pore size (see Note 12 ).
-
3.
Eagle minimum essential medium (MEM), without phenol red, without glutamine and without NaHCO3.
-
4.
Isopropyl alcohol (analytical grade).
2.6 Live/Dead Staining Components
-
1.
Live/Dead Double Staining Kit (Sigma-Aldrich, St. Louis, MO, USA). Store at −20 °C protected from light and moisture.
-
2.
Assay solution: add 10 μL Calcein Green AM solution (Solution A) and 5 μL Propidium iodide solution (Solution B) to 5 mL PBS (see Notes 13 , 14 ).
-
3.
Phosphate buffered saline (PBS).
2.7 SEM Microscopy Components
3 Methods
Carry out all procedures at room temperature unless otherwise specified.
3.1 Fabrication via Two-Photon Polymerization
Preparation and handling of photosensitive monomer composition as well as 2PP scaffolds fabrication should be performed in a yellow light photochemical lab environment.
-
1.
Place the volume of photosensitive material composition on a glass coverslip to achieve required sizes and thickness of monomer sample and let it to dry out.
-
2.
Put the glass coverslip with material to the down side on the stage under the objective of the 2PP setup (Fig. 5.1).
-
3.
Fabricate the structure in the volume of monomer using custom 3D design and applying defined optimum structuring speed and laser intensity.
-
4.
Develop the produced structure in corresponding solvent until non-polymerized material is completely washed away. PLA structures should be developed in dichloromethane.
-
5.
Rinse the structure in ethanol for several minutes to remove rest material debris.
3.2 Tissue Decellularization
-
1.
Treat the bovine pericardium with hypotonic buffered solution for 14 h at 4 °C.
-
2.
Remove buffer and then wash the pericardium with hypotonic buffered solution with 0.25% SDS for 24 h at room temperature.
-
3.
Remove the previous buffer and wash with PBS for 30 min at 4 °C.
-
4.
Wash the tissues with distilled water for 12 h at 4 °C.
-
5.
Remove water and wash the pericardium with isotonic buffered solution (12 h at 4 °C).
-
6.
Treat the pericardium with hypertonic buffered solution for 6 h at 4 °C.
-
7.
Wash tissues with PBS for 3 h at 4 °C.
3.3 Scaffold Seeding
All solutions and glassware should be sterile and all procedures should be carried out under aseptic conditions and in the sterile environment of a laminar flow cabinet.
-
1.
Sterilize the scaffolds (see Note 17 ).
-
2.
Remove adipose-derived stem cells (ASC) from culture flasks by enzymatic digestion using TrypLE Express Enzyme and centrifuge them (200 g, 3 min).
-
3.
Resuspend cells in culture medium and adjust cell suspension at a density of 5 × 106 cells/mL (see Note 18 ).
-
4.
Put carefully one scaffold to each well in a 48-well plate.
-
5.
Add 20 μL of a cell suspension of 5 × 106 cells/mL (1 × 105 cells/scaffold).
-
6.
Incubate the scaffolds with cells for 15 min.
-
7.
Add 200 μL culture medium and incubate at 37 °C.
3.4 Cell Encapsulation in Fibrin Hydrogel
All solutions and glassware should be sterile and all procedures should be carried out under aseptic conditions and in the sterile environment of a laminar flow cabinet.
-
1.
Remove adipose-derived stem cells (ASCs) from culture flasks by enzymatic digestion using TrypLE Express Enzyme and collect them by centrifugation (200 g, 3 min).
-
2.
Resuspend cells in culture medium and adjust cell suspension at a density of 5 × 106 cells/mL.
-
3.
Add 100 μL of the fibrinogen solution to each well in a 24-well plate.
-
4.
Add 60 μL of a cell suspension of 5 × 106 cells/mL (=3 × 105 cells/well) and mix.
-
5.
Add 100 μL of the thrombin solution to the cell and fibrinogen mixture (see Note 19 ) to observe the stable hydrogel.
-
6.
Incubate at 37 °C for 3 min.
-
7.
Add 100–200 μL culture medium and incubate at 37 °C.
3.5 Extract Preparation for MTT-Assay
All solutions and glassware should be sterile and all procedures should be carried out under aseptic conditions and in the sterile environment of a laminar flow cabinet [16].
-
1.
Sterilize the samples (see Note 17 ).
-
2.
Put the scaffolds into a tube, add an appropriate MEM volume (Table 5.2), and tightly close the tube (see Note 20 ).
Table 5.2 Extraction ratios for test materials of various thicknesses [16] -
3.
Incubate these samples at 37 °C for 24 h.
-
4.
Take this medium (extract) and dilute it (see Note 21 ).
3.6 MTT-Assay
All solutions and glassware should be sterile and all procedures should be carried out under aseptic conditions and in the sterile environment of a laminar flow cabinet [17].
3.6.1 Day 1
-
1.
Remove L929 cells from culture flasks by enzymatic digestion using TrypLE Express Enzyme and collect them by centrifugation (200 g, 3 min).
-
2.
Resuspend cells in culture medium and adjust cell suspension at a density of 1 × 105 cells/mL (see Note 18 ).
-
3.
Using a multichannel pipette, dispense 100 μL culture medium only (blank) into the peripheral wells of a 96-well plate.
-
4.
In the remaining wells, dispense 100 μL of a cell suspension of 1 × 105 cells/mL (=1 × 104 cells/well).
-
5.
Incubate cells for 24 h (5% CO2, 37 °C, >90% humidity) so that cells form a half-confluent monolayer.
-
6.
Examine each plate under a phase contrast microscope to ensure that cells are evenly distributed across the wells of plate (see Note 22 ).
3.6.2 Day 2
-
1.
After 24 h incubation, aspirate culture medium from the cells.
-
2.
Per each well, add 100 μL of treatment medium containing either the appropriate concentration of sample extract, or the negative control, or the positive control, or nothing but blank (see Note 23 ).
-
3.
Incubate cells for 24 h (5% CO2, 37 °C, >90% humidity).
3.6.3 Day 3
-
1.
After 24 h treatment, examine each plate under a phase contrast microscope to identify systematic cell seeding errors and growth characteristics of control and treated cells. Record changes in the morphology of the cells due to cytotoxic effects of the test sample extract, but do not use these records for any quantitative measure of cytotoxicity (see Note 24 ).
-
2.
After the plate examination, carefully remove the culture medium (see Note 25 ).
-
3.
Add 50 μL of MTT solution to each test well.
-
4.
Incubate the plates for 2 h in the incubator at 37 °C.
-
5.
Remove the MTT solution and add 100 μL isopropyl alcohol in each well.
-
6.
Sway this plate and subsequently transfer it to a microplate reader equipped with a 570 nm filter to read the absorbance (reference wavelength 650 nm).
-
7.
Record and save data (see Note 26 ).
-
8.
Calculate the reduction of viability using the following equation (see Note 27 ) [17]:
Viab. % = 100 × OD570e/OD570b,where OD570e is the mean value of the measured optical density of the 100% test sample extracts or its dilutions; OD570b is the mean value of the measured optical density of the blanks.
3.7 Live/Dead staining
-
1.
Remove the growth medium and wash cells in scaffolds with PBS three times to remove residual esterase activity.
-
2.
Add 200 μL of assay solution per one scaffold with cells and incubate the mixture at 37 °C in CO2-incubator for 20 min.
-
3.
Measure fluorescence using a fluorescence microscope with 490 nm excitation for simultaneous monitoring of viable and dead cells. With 545 nm excitation, only dead cells can be observed.
3.8 Scanning Electron Microscopy (SEM)
-
1.
Remove the growth medium and wash cells/scaffold with PBS twice for 2 min.
-
2.
Rinse the samples with 2.5% glutaraldehyde for 15 min.
-
3.
Wash scaffold with PBS three times for 10 min.
-
4.
Fix the cell-seeded scaffolds with 4% osmium tetroxide for 30 min (see Note 16 ).
-
5.
Wash with deionized water three times for 5 min (see Note 28 ).
-
6.
Dehydrate the samples using ethanol (30%, 50%, 70%, 90%, 95%, 95%, 100%, 100%, 100% – 15 min for each solution) (see Note 28 ).
-
7.
Treat the scaffolds with ethanol-HDMS (1:1) solution for 1 h.
-
8.
Remove and add HDMS twice for 10 min.
-
9.
Store the samples in dry environment.
-
10.
Sputter 50-nm gold layer on the samples.
-
11.
Observe with a scanning electron microscope using customer adjustments (Fig. 5.2).
3.9 Confocal Microscopy
-
1.
Place a glass-bottom Petri dish with the stained cell-seeded scaffold on the object table in an inverted laser scanning confocal microscope. See the Table 5.3 for typical settings.
Table 5.3 Example of confocal microscope settings used for analysis of cells growing within scaffolds -
2.
On the central slice cell level, find the sample focal plane, which is characterized by maximum cell square with fluorescence signal.
-
3.
Vary the power of excitation beam and the detector digital gain to find the value where fluorescence signal is little less than the maximum value at the given image bit depth. In our case, the excitation beam power was set 10 μW for 405 nm laser and 6 μW for 488 nm laser (see Note 29 ).
4 Notes
-
1.
Before opening, bring all reagents, stored at 4 °C or below, to room temperature and incubate for at least 15 min. This prevents absorbing the excessive moisture from the air.
-
2.
Type of photoinitiator for the preparation of reactive photo-curing system is determined by the wavelength of laser irradiation used for 2PP structuring. For example, Irgacure 2959 ptotoinitiator has the peak absorption at appr. 260 nm and should be applied for 2PP structuring at 515 nm. Photoreactive curing mixture for near infrared laser system (780 nm) should be prepared with Irgacure 369 (absorption peak at approx. 325 nm) and Michler’ ketone (absorption peak at aprox. 390 nm) photoinitiators.
-
3.
All cell cultures should be free of mycoplasma contamination and routinely checked.
-
4.
hASCs were obtained from human adipose tissue collected from patients undergoing elective plastic surgery after obtaining informed consent. Isolation of the cells took place according to a protocol described elsewhere [18]. We used five to seven passages of hASCs.
-
5.
Instead of TrypLE Express Enzyme, 0.25% Trypsin/1 mM EDTA solution can be used. However, TrypLE Express Enzyme has some important advantages compared to some trypsin preparations: it is animal-origin free and is more specific than crude trypsin preparations thus reducing the cell damage during preparations. TrypLE Express is stable at room-temperature (up to 2 years) and provided as ready to use solution. TrypLE Express can be directly substituted for trypsin in existing protocols. Simple dilution inactivates it, avoiding the need for use of trypsin inhibitors.
-
6.
Glass-bottom Petri dishes are used for confocal microscopy and can be replaced by any other glass-bottom vessels or chambers, e.g. from Nunc, MatTek Corp. or Ibidi GmbH.
-
7.
Fibrinogen solution is easy to foam. Avoid bubbles; do not shake! Dissolve fibrinogen by small portions. This can last for more than 3 h.
-
8.
We find that it is best to prepare this fresh each time.
-
9.
Biomaterial should pass veterinary control and be free of any infectious agents.
-
10.
SDS precipitates at 4 °C. Therefore, it may need to be warmed prior to use.
-
11.
Any hypertonic buffered solution can be used. We prefer this recipe described in [19].
-
12.
MTT solution should be used the same day.
-
13.
Since the buffer solution of Calcein-AM is gradually hydrolyzed to generate fluorescent Calcein, the working solution cannot be stored for more than few hours. Close the bottle cap tightly after using a portion of Calcein AM solution to avoid moisture.
-
14.
Propidium iodide is suspected to be highly carcinogenic; careful handling is required.
-
15.
Glutaraldehyde is a toxic hazardous substance. Avoid contact with skin and eyes. Avoid inhalation of vapors or mist. Wash hands before and immediately after handling the product. Glutaraldehyde is corrosive to the respiratory tract, highly inflammable, toxic (if swallowed or inhaled, in contact with skin), harmful if swallowed or inhaled, fatal if inhaled and causes severe skin burns and eye damage, serious skin and eye irritation, an allergic skin reaction, allergy or asthma symptoms or breathing difficulties if inhaled, respiratory irritation, damage to organs. Moreover, it is very toxic to aquatic life with long lasting effects. Store in cool place. Keep container tightly closed in a dry and well-ventilated place. Containers, which are opened, must be carefully resealed and kept upright to prevent leakage. Recommended storage temperature is −20 °C. Store under inert gas. A licensed disposal company should dispose glutaraldehyde and contaminated items.
-
16.
Osmium tetroxide is a highly toxic hazardous substance. Avoid contact with skin, eyes, and clothing. Avoid inhalation of vapors or mist. Wash hands before and immediately after handling the product. Osmium tetroxide is extremely destructive to tissue of the mucous membranes and upper respiratory tract, eyes, and skin. It causes spasm, inflammation and edema of the larynx, spasm, inflammation and edema of the bronchi, pneumonitis, pulmonary edema, burning sensation, cough, wheezing, laryngitis, shortness of breath, headache. Store in cool place. Keep container tightly closed in a dry and well-ventilated place. Containers, which are opened, must be carefully resealed and kept upright to prevent leakage. Recommended storage temperature is 2–8 °C. A licensed disposal company should dispose osmium tetroxide and contaminated items.
-
17.
We sterilize scaffolds with 70% ethanol (two washes for 30 min) and then expose them to UV for 3 h [7]. Alternatively, gamma-irradiation and ethylene oxide sterilization can be used.
-
18.
The Neubauer hemocytometer (Sigma-Aldrich) or other cell counters can be used (e.g. from Bio-Rad, Beckman Coulter, or Roche). You need to stain cells with Trypan Blue (0.2% final conc.) to differ live and dead cells.
-
19.
Add thrombin carefully to cells and fibrinogen because the mixture can start to form a gel. While adding, continuously mix it for homogenous cell distribution.
-
20.
For most test materials, extractions are performed under static conditions. However, agitation may be deemed appropriate as an effort to more closely mimic an end use or to ensure that the extraction media come in contact with all relevant material surfaces. In any case, when agitation is considered appropriate, the method used should be marked.
-
21.
At least four different concentrations of the test sample extract or the positive control extract should be tested. The highest concentration used should be 100% extract and the other concentrations will be adequately spaced within a single logarithmic range. For the negative control, only the 100% extract should be tested. Culture medium should be used as blank.
-
22.
This incubation period ensures cell recovery, and adherence and progression to exponential growth phase. This check is performed to identify experimental errors.
-
23.
Positive and negative controls should be included in every cytotoxicity test. Positive control material is material which, when tested in accordance with ISO 10993-5, provides a reproducible cytotoxic response. The purpose of the positive control is to demonstrate an appropriate test system response. For example, an organotin-stabilized polyurethane has been used as positive control for solid materials and extracts. Dilutions of phenol, for example, have been used as a positive control for extracts. In addition to a material, pure chemicals (SDS or Triton X100) can also be used to demonstrate the performance of the test system. Negative control material is material which, when tested in accordance with ISO 10993-5, does not produce a cytotoxic response. The purpose of the negative control is to demonstrate background response of the cells. For example, high-density polyethylene for synthetic polymers, and aluminium oxide ceramic rods for dental material have been used as negative controls. ‘Blank’ is extraction vehicle not containing the test sample, retained in a vessel identical to that which holds the test sample and subjected to conditions identical to those to which the test sample is subjected during its extraction. The purpose of the blank is to evaluate the possible confounding effects due to the extraction vessel, vehicle and extraction process.
-
24.
Undesirable growth characteristics of control cells can indicate experimental error and can be cause for rejection of the assay.
-
25.
This is an important step, because reductive chemicals in the extract can also reduce MTT, causing false negative results.
-
26.
The data generated will be recorded in the raw data file. The results will be presented in tabular form, including experimental groups with the test item, negative, blank and positive controls. A decrease in number of living cells results in a decrease in the metabolic activity in the sample. This decrease directly correlates to the amount of blue-violet formazan formed, as monitored by the optical density at 570 nm.
-
27.
The lower the Viab.% value, the higher the cytotoxic potential of the test sample is. If viability is reduced to <70% of the blank, it has a cytotoxic potential. The 50% extract of the test sample should have at least the same or a higher viability than the 100% extract; otherwise, the test should be repeated.
-
28.
All wastes should be carefully collected, because they can contain osmium traces.
-
29.
For correct data processing, all images must be acquired under the same conditions. The parameters of excitation light (wavelengths, powers) and registration (diameter of confocal diaphragm, number of pixel, pixel dwell time, detection range, and detector digital gain) must remain the same between control and test groups.
References
Lu T, Li Y, Chen T (2013) Techniques for fabrication and construction of three-dimensional scaffolds for tissue engineering. Int J Nanomedicine 8:337–350
Loh QL, Choong C (2013) Three-dimensional scaffolds for tissue engineering applications: role of porosity and pore size. Tissue Eng Part B Rev 19(6):485–502
Skoog SA, Goering PL, Narayan RJ (2012) Stereolithography in tissue engineering. J Mater Sci 25(3):845–856. https://doi.org/10.1007/s10856-013-5107-y
Cheng CW, Solorio LD, Alsberg E (2014) Decellularized tissue and cell-derived extracellular matrices as scaffolds for orthopaedic. Tissue Eng Biotechnol Adv 32(2):462–484
O'Neill JD, Anfang R, Anandappa A, Costa J, Javidfar JJ, Wobma HM et al (2013) Decellularization of human and porcine lung tissues for pulmonary. Tissue Eng Ann Thorac Surg 96(3):1046–1056
Koroleva A, Gittard S, Schlie S et al (2012) Fabrication of fibrin scaffolds with controlled microscale architecture by a two-photon polymerization–micromolding technique. Biofabrication 4:015001
Timashev P, Kuznetsova D, Koroleva A et al (2016) Novel biodegradable star-shaped polylactide scaffolds for bone regeneration fabricated by two-photon polymerization. Nanomedicine 11(9):1041–1053. https://doi.org/10.2217/nnm-2015-0022
Timashev PS, Bardakova KN, Minaev NV et al (2016) Compatibility of cells of the nervous system with structured biodegradable chitosan-based hydrogel matrices. Appl Biochem Microbiol 52(5):508–514
Timashev PS, Vedunova MV, Guseva D et al (2016) 3D in vitro platform produced by two-photon polymerization for the analysis of neural network formation and function. Biomed Phys Eng Express 2(3):1–8
Williams JM, Adewunmi A, Schek RM, Flanagan CL, Krebsbach PH, Feinberg SE et al (2005) Bone tissue engineering using polycaprolactone scaffolds fabricated via selective laser sintering. Biomaterials 26(23):4817–4827
Inzana JA, Olvera D, Fuller SM, Kelly JP, Graeve OA, Schwarz EM et al (2014) 3D printing of composite calcium phosphate and collagen scaffolds for bone regeneration. Biomaterials 35(13):4026–4034
Yilgor P, Sousa RA, Reis RL, Hasirci N, Hasirci V (2008) 3D plotted PCL scaffolds for stem cell based bone tissue engineering. Macromol Symp 269:92–99
Yan L-P, Oliveira JM, Oliveira AL, Caridade SG, Mano JF, Reis RL (2011) Macro/microporous silk fibroin scaffolds with potential for articular cartilage and meniscus tissue engineering applications. Acta Biomater 8(1):289–301
Cheng T-Y, Chen M-H, Chang W-H, Huang M-Y, Wang T-W (2013) Neural stem cells encapsulated in a functionalized self-assembling peptide hydrogel for brain tissue engineering. Biomaterials 34(8):2005–2016
Tang M, Chen W, Weir MD, Thein-Han W, Xu HHK (2012) Human embryonic stem cell-encapsulation in alginate microbeads in macroporous calcium phosphate cement for bone tissue engineering. Acta Biomater 8(9):3436–3445
ISO 10993-12 (2012) Biological evaluation of medical devices—part 12: sample preparation and reference materials. 28 p
ISO 10993-5 (2009) Biological evaluation of medical devices—Part 5: tests for in vitro cytotoxicity. 42 p
Gruene M, Pflaum M, Deiwick A, Koch L, Schlie S, Unger C et al (2011) Adipogenic differentiation of laser-printed 3D tissue grafts consisting of human adipose-derived stem cells. Biofabrication 3:015005
Waterman-Storer CM (2001) Microtubule/organelle motility assays. Curr Protoc Cell Biol 00:13.1:13.1.1–13.1.21
Acknowledgments
This work was supported by the Russian Science Foundation, grant 15-15-00132.
Author information
Authors and Affiliations
Corresponding authors
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
Shpichka, A., Koroleva, A., Kuznetsova, D., Dmitriev, R.I., Timashev, P. (2017). Fabrication and Handling of 3D Scaffolds Based on Polymers and Decellularized Tissues. In: Dmitriev, R. (eds) Multi-Parametric Live Cell Microscopy of 3D Tissue Models. Advances in Experimental Medicine and Biology, vol 1035. Springer, Cham. https://doi.org/10.1007/978-3-319-67358-5_5
Download citation
DOI: https://doi.org/10.1007/978-3-319-67358-5_5
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-67357-8
Online ISBN: 978-3-319-67358-5
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)