Abstract
Inappropriate use of diagnostic imaging in the emergency department setting is a growing concern. Multiple factors drive imaging utilization in the ED, and diagnostic imaging use has increased dramatically in the past two decades. Medical radiation now accounts for the largest percent of artificial exposure to ionizing radiation in the USA, and while a direct link between radiation exposure from imaging and cancer development has not been proven, there is increasing concern about the potential health effects of repeated exposure to medical radiation, especially in the pediatric population. Incidental findings are common and can be difficult to communicate and manage. Several methods have been proposed to reduce inappropriate imaging utilization, and clinical decision support integration with computerized order entry was recently mandated by the US Department of Health and Human Services. Further study into the impact of clinical decision support systems and radiologist-driven educational interventions is warranted, and development of guidelines for management of incidental findings is encouraged.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Imaging utilization
- Emergency imaging
- ACR appropriateness criteria
- Clinical decision support
- Incidental findings
- Radiation safety
- Evidence-based imaging
-
Utilization of medical imaging in the emergency department has increased in recent decades (moderate evidence).
-
Medical radiation accounts for the largest percentage of artificial exposure to ionizing radiation (moderate evidence).
-
A direct link between low-level radiation from diagnostic imaging and cancer development has not been proven. However, there is evidence suggesting increased risk of leukemia and brain cancer in children exposed to cumulative CT radiation doses of 50–60 mGy. Most estimates of long-term effects of low-level radiation exposure (100–150 mSv) come from the longitudinal survivor study of atomic bomb survivors (moderate evidence).
-
Incidental findings are common and their workup is expensive and may cause undue anxiety, excess radiation exposure, and risk of additional diagnostic procedures for mostly benign conditions (limited evidence).
-
Application of the clinical decision support such as the American College of Radiology (ACR) appropriateness criteria could decrease overutilization in the emergency department setting (limited evidence).
Definitions and Pathophysiology
Overutilization of imaging is defined as application of imaging when it is unlikely to improve outcomes [1]. Over the last two decades, utilization of medical imaging in the emergency department setting has dramatically increased. While imaging undoubtedly saves lives, potential overutilization is concerning for patients, health care providers, and health care payers. For patients, medical imaging is now the largest contributor of radiation exposure to individuals in the USA, the majority attributed to CT. For health care providers, imaging can rapidly aid in diagnosis and identification of life-threatening conditions, but incidental findings may add challenge in patient management. For health care payers, increased imaging utilization has been a major contributor to rising health care costs in the USA.
Epidemiology
According to the National Hospital Ambulatory Medical Care Survey, CT use during ED visits has increased 460% between 1995 and 2011, from 2.8% of encounters in 1995 to 15.8% in 2011 [2, 3]. In the same time, MRI utilization in the ED has increased 500% from 0.1% to 0.6%, and ultrasound has increased 210% from 1.2% to 3.8% of visits [2, 3]. Increased use of CT was seen in all 20 of the most common complaints presenting to the ED in this time period, with highest growth in abdominal pain, flank pain, chest pain, and shortness of breath [4]. In the pediatric population, CT use increased 23–435% depending on body part imaged between 2000 and 2006, far exceeding growth in patient volume and acuity and mimicking trends in the adult population [5]. In 2012, the last year for which complete data is available, 256.8 CT scans were performed per 1000 people, a rate 25% higher than for the next highest Organization for Economic Cooperation and Development (OECD) (developed) country. 104.8 MRIs were performed per 1000 people that same year, almost twice the average rate of OECD countries [6]. Several factors have likely contributed to the rise in imaging utilization in the USA, including advances in medical imaging, increased accessibility to imaging equipment, 24/7 interpretation by radiologists, fear of litigation, and shifting expectations of patients and emergency department clinicians [1, 7].
Overall Cost to Society
Inappropriate use of imaging in the emergency department results in excess radiation exposure, increased health care costs, and increased time of ED visits and imparts the additional anxiety, costs, and risks associated with incidental findings .
Goals of Imaging
The goal of imaging in the ED is to diagnose or exclude potentially life-threatening medical conditions in symptomatic patients. Screening of non-symptomatic patients is also performed in the ED in certain scenarios, for example, in protocol-driven imaging of trauma patients and in cases of suspected child abuse.
Methodology
Information from this chapter was obtained primarily through a MEDLINE search using PubMed (US National Library of Medicine, Bethesda, Maryland; http://www.ncbi.nlm.nih.gov/pubmed/) from 1980 to March 2015. Keywords were “emergency department radiology overutilization,” “emergency department radiology utilization,” “incidental finding radiology,” and the resultant related fields from this original database. The search was limited to English-language articles. The authors performed a critical review of the title and abstracts of indexed articles followed by the full text of articles that were relevant. Additional relevant articles were selected from the references of reviewed articles and published guidelines.
Discussion of Issues
Overutilization of Diagnostic Imaging in the ED Setting
There has been dramatic growth in imaging utilization in the past two decades. While imaging can provide a key diagnostic step in diagnosis and contribute to swift and appropriate patient care, it is unclear that improvements in outcomes have been commensurate with increases in imaging utilization . For example, between 2001 and 2010, there has been a 2.5-fold increase in CT utilization among adult fall patient ED visits, while the proportion of fall visits with life-threatening conditions has only increased by 2.5% [8]. In patients presenting to the ED with flank or kidney pain, prevalence of CT use increased from 4.0% to 42.5% from 1996 to 2007, while the number of patients ultimately diagnosed with urolithiasis or other significant diagnoses or admitted to the hospital did not substantially change [9]. In patients presenting to the ED with injury-related conditions, the prevalence of CT and MR use increased from 6% in 1998 to 15% in 2007 without corresponding change in prevalence of visits for which patients were either admitted to the hospital or to an intensive care unit [10]. Growth of imaging utilization has been so dramatic that multiple national campaigns have been established to evaluate and combat overutilization, including Image Gently, Image Wisely, and As Low as Reasonably Achievable (ALARA ), and initiatives by the National Council on Radiation Protection and Measurements, the Food and Drug Administration, and the American Board of Radiology Foundation [1, 11,12,13,14,15,16].
Studies have shown that ER physicians agree that overutilization of imaging is a problem, raising the question of why imaging is so frequently and at times inappropriately utilized. Fear of litigation has been cited as a factor driving imaging utilization in surveys of ED physicians, and imaging ordered for defensive purposes is thought to account for 5–25% of total imaging costs [1, 17, 18]. A survey of ED clinicians also found that concerns about patient satisfaction affect CT ordering decisions [18]. Lack of information about prior imaging studies may be a factor in overutilization, as studies have shown that ED physicians factor cumulative CT count into image ordering decisions only some of the time, but would take this information into account if information was more available [18]. Lack of education about risks of imaging is also a factor driving overutilization. A study of ED physicians found that the majority gave incorrect estimates of cancer risk from a 10 mSv exposure and incorrect estimates of effective radiation dose of a chest X-ray and CT abdomen-pelvis, two commonly ordered imaging exams [18]. Another study found that 75% of physicians underestimated cancer risk from CTs, and >90% of ED physicians and 50% of radiologists did not believe that CT scans increased cancer risk [19, 20]. Additionally, only 3% of surveyed patients believed that CTs increase lifetime cancer risk, and 7% of patients undergoing abdominal CT in the ED reported they had been told about the risks and benefits of their CT scan [20].
The current fee-for-service payment system for health services has been cited as a culprit for overutilization, though is probably less of an issue in the ED setting. Factors within the ED seem to affect utilization, as one study found that odds of low-cost imaging utilization are higher when the ED is slower and high-cost imaging higher when the ED is busier, possibly due to facilitated workup with increased cross-sectional imaging [21].
Risks of Radiation Exposure in Adults and Children
Radiation Terminology
Radiation is measured in standard international units (SI = Systeme Internationale). The intensity of X-ray radiation can be characterized by exposure in coulombs/kilogram or air kerma in Gray (Gy). The absorbed dose is the energy absorbed per unit of mass and is also measured in Gy. The equivalent dose describes the biologic impact to exposed tissue. The effective dose is the sum of products of dose equivalent multiplied by weighting factors depending on the radiosensitivity of exposed organs and is expressed in Sieverts (Sv). The effective dose is used to describe risks from medical imaging in which dose distribution is not homogenous and provides generic estimate of harm to the patient caused by radiation exposure. It should be noted that effective dose is only an estimate of true risk [22, 23]. CT accounts for a large proportion of diagnostic imaging-related radiation dose. CT dose index (CTDI ) in mGy and dose length product (DLP ), a measure that reflects the product of CTDI and the length of the scan in mGy-cm, describe radiation doses in CT. However, these reported doses represent dose to a phantom. Conversion factors for DLP into effective dose in the adult and pediatric patient have been published for a variety of examinations [24, 25].
Radiation Mechanisms of Effects
X-rays are a type of electromagnetic radiation that contains sufficient energy to overcome the binding energy of orbiting electrons, creating ions. Ionization, mostly in the form of hydroxyl radicals, can result in DNA strand breaks and base damage. Most DNA damage is repaired, but some double-stranded breaks are not repaired or misrepaired, which can lead to point mutations, chromosomal translocations, and gene fusion. The resulting cell damage may be teratogenic or result in long-term carcinogenesis.
Types of Biological Effects
Radiation effects fall into two categories: deterministic or stochastic. Deterministic effects are only seen above a certain threshold. These effects include cataracts, skin burns, and epilation (Table 4.1) [26,27,28]. Diagnostic imaging does not typically result in radiation doses high enough to meet the threshold for deterministic effects. Stochastic effects do not have a radiation dose threshold. The risk of a particular effect increases with increasing radiation dose; however, the severity of the effect is independent of dose. Radiation-induced genetic damage and carcinogenesis are stochastic phenomena.
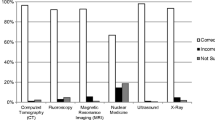
Radiation Exposure in Medical Imaging
Humans are exposed to background radiation from the ground (mostly from radon), building materials, cosmic rays, and food. Average annual background radiation is estimated at 2.4 mSv globally and 3.0 mSv in the USA, primarily due to higher naturally occuring radon levels in the USA [29,30,31]. An increasing proportion of total radiation exposure in the USA is due to radiation from medical imaging. The average annual dose due to medical radiation exposure is 0.2 mSv globally and 3.0 mSv in the USA.
Approximately 50% of US annual radiation exposure is due to medical radiation, while in 1980 it contributed less than a quarter of annual radiation dose [1, 32]. Medical radiation is used for both diagnosis and therapy. Diagnostic imaging tests including radiography, fluoroscopy, nuclear imaging, and CT utilize ionizing radiation. Diagnostic imaging uses low-level radiation, defined by effective dose <100–150 mSv. CT accounts for the largest proportion of radiation dose in diagnostic imaging, with effective dose for a whole-body CT scan of approximately 12 mSv. A risk projection model based on Japanese atomic bomb survivor data estimates that 1.5–2.0% of cancers in the USA may be attributable to CT scans [22, 33]. Additional approximate radiation doses for common exams in adults and children are described in Tables 4.2 and 4.3 [29, 34, 35].
There is debate regarding potential carcinogenesis from radiation doses below 100 mSv. The linear no-threshold model for radiation effects is the most widely accepted model for quantifying radiation exposure and is endorsed by the National Research Council in their BEIR VII report. In this model, approximately 1 in 1000 persons will develop cancer from an exposure to 10 mSv over a 70-year lifetime, compared to approximately 420 in 1000 persons who develop cancer unrelated to radiation exposures [29, 36]. There is increased risk for carcinogenesis with radiosensitive tissues that are included in the field (e.g., breast, lung, and thyroid).
Excess Radiation Due to Overutilization of Emergency Imaging
Concerns about radiation safety are particularly pertinent to imaging in the pediatric ED. Children are 2–5 times more sensitive to the effects of ionizing radiation than adults due to increased number of dividing cells and longer lead time to develop cancer [5, 22]. Although the exact effects of imaging-related radiation are not completely understood, studies have reported a positive association between CT radiation dose and subsequent development of leukemia and brain cancer in children and young adults. A recent retrospective study of patients in Great Britain estimated that cumulative CT doses of 50 mGy in patients less than 22 years of age nearly triples the risk of leukemia, and doses above 60 mGy may triple the risk of brain cancer [37]. A 2001 study estimated that with approximately 600,000 abdominal and head CTs performed per year in children <15 years old, 500 children will ultimately die from radiation-induced cancer [38]. Radiation sensitivity generally declines with age, reaching an adult plateau in the fourth decade of life and then slowly declining, with the exception of lung cancer (for which radiation-associated risk may increase into middle age) [38,39,40].
Many of the patients being imaged in the ED are men and women of childbearing age (or pregnant women). Studies which are occasionally repeated, such as CT for pulmonary embolism and renal stone CT, place radiosensitive breast tissue or gonads in the radiation field. A study estimated that a single CT for pulmonary embolism may incur a 1.011 relative risk of breast cancer for 25-year-old females and 1.022 relative risk of lung cancer [41]. Non-contrast CT for renal stone detection, which is often performed in young adults, imparts a mean effective dose of 8.5 mSv and dose to the uterus of 23 mGy using multidetector scanners [42, 43]. These exams are often repeated, with one study reporting 4% of patients undergoing CT evaluation for renal colic receiving three or more scans in a 6-year study period [42].
Monetary Costs Associated with Overutilization of Emergency Imaging
The cost of health care in the USA has increased at a rate greater than twice the general rate of inflation and accounted for 16.9% of the GDP in 2014 [44]. Comparatively, the USA has the highest proportion of health care cost for GDP among OECD countries, which average 9.3% of GDP expenditure on health care costs, while life expectancy in the USA is 1.5 years less than the OECD average [44]. Imaging contributes to the high cost of health care in the USA, with a 2005 study estimating inpatient imaging to account for approximately 10% of total hospital cost [45]. Advanced imaging drives the cost of medical imaging. Insurance reimbursements for CT range from $400 for a cervical spine CT to $1400 for an abdomen and pelvis CT, with expenditures on CTs equipment estimated at over $5 billion dollars between 2000 and 2005 [36]. Utilization of imaging in the ED accounts for a large part of imaging costs. For example, non-contrast head CTs in the ED in the USA cost an estimated $6.1 billion per year [46]. Head CTs and MRIs ordered for dizziness in USA EDs cost $470 million per year [47, 48]. Reduction in imaging overutilization will be necessary for any cost containment effort in US health care.
Does Imaging Increase Time in the ED?
Time Cost
The addition of medical imaging to diagnostic workup in the ED has been reported to increase patient visit time [49,50,51]. Imaging has been described as an independent variable in ED length of stay, with one study reporting increased length of stay of 1.0 h for X-ray, 4.7 h for ultrasound, and 0.7 h for CT [49]. Another study of ED visits for injury-related diagnoses found that visits during which CT or MRI was obtained lasted 126 min longer than those without CT or MRI [10]. Eliminating inappropriate imaging utilization may be a key step in reducing ED turnaround time and improving streamlined, effective patient care.
Impact of Incidental Findings in Emergency Imaging
Incidental findings, also known as incidentalomas, are findings identified on imaging that were not previously detected or clinically suspected. In the best scenario, these findings lead to expedited workup and treatment of previously unrecognized medical conditions that improves patient outcome. However, reporting of incidentalomas may also cause undue stress, radiation exposure, and potential morbidity of additional workup for mostly benign or indolent conditions. Additionally, a considerable amount of clinician time may be required to educate patients about implications of incidental findings and ensure appropriate follow-up. When coupled with the monetary cost of workup of incidental findings , this may challenge cost containment efforts for health care provision. Management of incidental findings is challenging due a paucity of data and clear guidelines on appropriate follow-up. Some incidental findings will almost certainly not yield a serious diagnosis and do not need further workup; however, the lack of definitive guidelines makes it difficult for many patients and physicians to accept any uncertainty in diagnosis and results in further testing that is most likely to reveal a benign diagnosis and could lead to morbidity [52, 53].
Incidental findings are common in ED imaging. Rates of incidental findings in ED patients vary from 34% to 43% in abdominal trauma patients and up to 45% in renal colic patients [54,55,56,57,58]. Rates of incidental findings in all-comers to the ED with CT have been reported at up to 56% for abdomen-pelvis CTs, 46% for chest CTs, and 20% for head CTs. The most common incidental findings include sinus disease, hepatic lesions, pulmonary nodules, adnexal enlargement, and osseous change [54]. For example, one study of ED chest CT Angiograms (CTAs) evaluating for pulmonary embolism (PE) reported 24% of patients to have had incidental findings that required diagnostic follow-up, including new pulmonary nodule in 13% of patients and new lymph node enlargement in 9% of patients [19].
One challenge of detection of incidental findings is effectively communicating findings to patients and documenting this communication. Overall rate of disclosure of incidental findings documented in discharge paperwork varies from 10 to 27% [54, 58, 59]. A recent study found that documented reporting of incidental findings in the ED ranged from 8 to 11% by body area imaged and 0–33% by incidental finding, with highest rates of reporting to patients including aortic dilatations, meningiomas, pulmonary nodules, bone lesions, and enlarged adnexa [54]. While it may be understandable that common and almost certainly benign incidental findings , such as simple renal cysts, are not disclosed or acted upon, follow-up of even moderate and severe findings in the ED patients may be challenging. A study of incidental CT findings in renal colic patients rated findings based on clinical severity and determined that only 18% of patients with “moderate” or “severe” incidental findings had follow-up within 2 years; however, none of these patients had a serious diagnosis on further workup [58].
One common incidental finding on CT is a thyroid nodule. Studies have reported incidental thyroid nodules (ITN) on cross-sectional imaging including the thyroid in up to 16% of patients [60, 61]. These pose a management dilemma, as their workup is expensive, often invasive, and often yields a benign diagnosis. ITNs are often followed with ultrasound and ultimately fine-needle aspiration (FNA) biopsy, an anxiety-provoking procedure costing up to $3000 [62]. Of patients undergoing FNA for an ITN, 25–41% proceed to surgery and 36–75% of these surgically excised ITNs prove to have benign pathology [63,64,65,66]. Overall malignancy rates of ITNs detected on CT and MRI have been reported at 0% to 11%. However, many of these cancers are small papillary carcinomas, which many experts believe to be subclinical disease.
Hepatic lesions are another common incidental finding, with one study reporting incidental hepatic lesions in 17% of outpatients undergoing CT of the abdomen and pelvis [67]. Workup for incidental hepatic lesions exposes patients to further radiation and at times percutaneous biopsy, a procedure that has morbidity of 2.0–4.8% and mortality of 0.05% [53, 68,69,70,71]. Autopsy reports have found as many as 52% of the general population has benign hepatic lesions [72]. It is thus critical to question whether an incidental hepatic lesion places the patient at risk for adverse outcome and to clearly describe scenarios in which imaging characteristics can satisfactorily differentiate benign from malignant lesions.
Universally accepted guidelines for management of most incidental findings in ED patients have not been established. Comparison with prior exams to determine stability of a lesion is critical to radiologists’ role in characterizing and managing incidentalomas. The American College of Radiology (ACR) has published a white paper outlining evidence-based recommendations for management of common incidentalomas detected on CT of the abdomen and pelvis based on size criteria, imaging characteristics, and patient comorbidities [53]. Adherence to these recommendations may reduce the variability, cost, and anxiety associated with workup of incidental findings . Further analysis is warranted to establish formal guidelines to establish the appropriate workup of common incidental findings .
Reducing Inappropriate Use of Imaging in the ED
Several methods have been proposed to reduce imaging overutilization in the emergency department. Radiologists may be tasked with an increased role in reviewing imaging orders for appropriateness before studies are performed. Educating clinicians about radiation dose, cost, and limitations of common imaging studies may substantially reduce overutilization [1]. This could be addressed in medical school and repeated throughout training and at meetings of referring physicians. Reducing duplicate imaging studies should be encouraged. Clinical decision support systems for clinicians requesting imaging is also being more widely implemented to reduce the inappropriate exam utilization.
Duplicate studies on ED patient transfer are common, with approximately 60% of patients transferred to a level 1 trauma center undergoing repeat CT exams, most of which do not alter outcomes [73,74,75]. Some institutions have adopted a standard CT protocol for all trauma patients transferred to the ED. A study at one such institution revealed that patients underwent an average of 4.5 additional CT exams due to fulfillment of the standard trauma imaging protocol. These studies demonstrated unexpected acute findings in 5.9% of transferred trauma patients; however, none of these findings changed clinical management [73]. Duplicate imaging can be reduced utilizing electronic image-sharing technology, which enables image sharing across institutions and should be encouraged to decrease the rate of unnecessary repeat scans. A study evaluating the impact of imaging CT import in ED transfer patients found a 17% reduction in mean rates of all subsequent diagnostic imaging and 29% reduction in post-transfer CT [76].
Clinical decision support is thought to be a key tool in reducing inappropriate radiologic exams. Clinical decision support (CDS) systems can be integrated into computerized order entry (CPOE), providing clinicians real-time evidence-based guidelines for consideration. CDS-CPOE integration has been mandated by the Department of Health and Human Services and outlined in its Health Information Technology for Economic and Clinical Health Act [77, 78]. CDS has been shown to decrease utilization and increase documented adherence to evidence-based guidelines without delayed reporting of significant findings [79,80,81]. The optimal CDS-CPOE system is one that would provide real-time feedback with clear, evidence-based guidelines to ordering clinicians [78]. After implementation of a CDS-CPOE system derived from the New Orleans Criteria, Canadian CT Head Rule, and CT in Head Injury Patients Prediction Rule, rates of non-contrast head CT for ED patients with mild traumatic brain injury decreased by 13% with no change in rate of delayed diagnosis of radiologically significant findings [80]. Similarly, implementation of an integrated CDS-CPOE system decreased rates of CT pulmonary angiography in the ED and increased yield of performed studies [79]. The ACR guidelines recommended application of National Emergency X-ray Utilization Study (NEXUS) criteria , which identify patients with low probability of cervical spine injury who do not need imaging, has been estimated to decrease the number of screening cervical spine CTs by 20% in a level 1 trauma center [82, 83]. The ACR has published appropriateness criteria for the most commonly encountered clinical scenarios including radiation risk of commonly ordered exams [84]. These criteria are readily available on the ACR website and may be used as a starting point for imaging-related clinical decision-making [84].
Future Research
Future research should provide:
-
Cost-effective analysis of imaging studies based on patient presentation
-
Comparative effectiveness research for the use of CT versus laboratory workup or non-ionizing imaging alternatives (US and MRI)
-
Formal guidelines for workup of incidental findings
-
Radiologist-driven educational interventions for medical students and ED clinicians and analysis of impact
-
Analysis of impact of CDS mandate on imaging utilization in the ED
Summary
-
There is growing concern that diagnostic imaging is overutilized in the ED setting.
-
Inappropriate utilization of imaging can result in excess radiation exposure.
-
Inappropriate medical imaging can increase ED turnaround time.
-
Incidental findings are common and may result in undue anxiety, cost, and risks associated with additional workup.
-
CDS is mandated by the Department of Health and Human Resources. Adherence to ACR appropriateness criteria may decrease overutilization of imaging in the ED setting.
References
Hendee WR, Becker GJ, Borgstede JP, et al. Radiology. 2010;257(1):240–5.
Stussman BJ. Adv Data. 1997;285:1–19.
Centers for Disease Control and Prevention. National Hospital Ambulatory Medical Care Survey: 2011 Emergency Department Summary Tables http://www.cdc.gov/nchs/ahcd/web_tables.htm
Kocher KE, Meurer WJ, Fazel R, et al. Ann Emerg Med. 2011;58:452–62.e3.
Broder J, Fordham LA, Warshauer DM. Emerg Radiol. 2007;14:227–32.
Organization for Economic Co-Operation and Development. StatExtracts: Health Status. OECD iLibrary. http://www.oecd-ilibrary.org/social-issues-migration-health/health-key-tables-from-oecd_20758480
Kirsch TD, Hsieh YH, Horana L, et al. J Emerg Med. 2011;41:302–9.
Brinjikji W, Kallmes DF, Cloft HJ. AJR Am J Roentgenol. 2015;204:558–62.
Westphalen AC, Hsia RY, Maselli JH, et al. Acad Emerg Med. 2011;18:699–707.
Korley FK, Pham JC, Kirsch TD. JAMA. 2010;304:1465–71.
Mills AM, Raja AS, Marin JR. Acad Emerg Med. 2015;22(5):625–31.
Goske MJ, Applegate KE, Boylan J, et al. Pediatr Radiol. 2008;38:265–9.
Slovis TL. Radiology. 2002;223:5–6.
Linton OW, Mettler FA Jr. AJR Am J Roentgenol. 2003;181:321–9.
Brink JA, Amis ES Jr. Radiology. 2010;257:601–2.
Food and Drug Administration. Pediatr Radiol. 2002;32(4):314–6.
Lee CI, Ponce NA, Ettner SL, et al. AJR Am J Roentgenol. 2012;199(5):1054–9.
Griffey RT, Jeffe DB, Bailey T. Acad Emerg Med. 2014;21:768–77.
Hall WB, Truitt SG, Scheunemann LP, et al. Arch Intern Med. 2009;169:1961–5.
Lee CI, Haims AH, Monico EP, et al. Radiology. 2004;231:393–8.
Wong HJ, Sistrom CL, Benzer TI, et al. Radiology. 2013;268:779–89.
Brenner DJ, Hall EJ. N Engl J Med. 2007;357(22):2277–84.
Loftus M, Sanelli P, Frush D, Applegate K. Radiation exposure from medical imaging. Evidence-based neuroimaging diagnosis and treatment. New York: Spring Science+Business; 2013. p. 63–77.
Thomas KE, Wang B. Pediatr Radiol. 2008;38:645–56.
Huda W, Vance A. AJR Am J Roentgenol. 2007;188:540–6.
International Committee on Radiation Protection (ICRP). Annals of the ICRP Publication 103. The 2007 Recommendations of the International Commission on Radiological Protection. http://www.icrp.org/docs/ICRP_Publication_103-Annals_of_the_ICRP_37(2-4)-Free_extract.pdf
International Committee on Radiation Protection (ICRP). Statement on Tissue Reactions. International Commission on Radiological Protection; 2011. http://www.icrp.org/docs/icrp%20statement%20on%20tissue%20reactions.pdf
UNSCEAR Report to the General Assembly Sources, Effects and Risks of Ionizing Radiation. New York; 2013. http://www.unscear.org/docs/reports/2013/13-85418_Report_2013_Annex_A.pdf
Health risks from exposure to low levels of ionizing radiation: BEIR VII – Phase 2. Washington, DC: National Research Council; 2006. The National Academies Press Washington, DC.
Sources and Effects of Ionizing Radiation, Volume 1. New York; 2008. http://www.unscear.org/docs/reports/2008/09-86753_Report_2008_Annex_B.pdf
Brenner DJ, Doll R, Goodhead DT, et al. Proc Natl Acad Sci USA. 2003;100(24):13761–6.
Schauer DA, Linton OW. Health Phys. 2009;97(1):1–5.
Berrington de Gonzalez A, Mahesh M, Kim KP, et al. Arch Intern Med. 2009;169:2071–7.
Mettler FA Jr, Huda W, Yoshizumi TT, et al. Radiology. 2008;248(1):254–63.
Brody AS, Frush DP, Huda W, et al. Pediatrics. 2007;120:677–82.
Broder J, Warshauer DM. Emerg Radiol. 2006;13:25–30.
Pearce MS, Salotti JA, Little MP, et al. Lancet. 2012;380(9840):499–505.
Brenner D, Elliston C, Hall E, et al. AJR Am J Roentgenol. 2001;176:289–96.
Preston DL, Cullings H, Suyama A, et al. J Natl Cancer Inst. 2008;100(6):428–36.
Hall EJ, Brenner DJ. Br J Radiol. 2012;85(1020):e1316–7.
Hurwitz LM, Reiman RE, Yoshizumi TT, et al. Radiology. 2007;245(3):742–50.
Katz SI, Saluja S, Brink JA, et al. AJR Am J Roentgenol. 2006;186(4):1120–4.
Spielmann AL, Heneghan JP, Lee LJ, et al. AJR Am J Roentgenol. 2002;178(5):1058–62.
Organization for Economic Co-Operation and Development. OECD Health Statistics 2014: How does the United States compare? http://www.oecd.org/unitedstates/Briefing-Note-UNITED-STATES02914.pdf.
Beinfeld MT, Gazelle GS. Diagnostic imaging costs: are they driving up the costs of hospital care? Radiology. 2005;235(3):934–9.
Wang X, You JJ. Radiology. 2013;266(3):783–90.
Saber Tehrani AS, Coughlan D, Hsieh YH, et al. Acad Emerg Med. 2013;20(7):689–96.
Bent C, Lee PS, Shen PY, et al. Emerg Radiol. 2015;22(5):511–6.
Yoon P, Steiner I, Reinhardt G. CJEM. 2003;5(3):155–61.
Pitts SR, Pines JM, Handrigan MT, et al. Ann Emerg Med. 2012;60(6):679–86.e3.
Kocher KE, Meurer WJ, Desmond JS, et al. Acad Emerg Med. 2012;19(5):525–34.
Casarella WJ. Radiology. 2002;224(3):927.
Berland LL, Silverman SG, Gore RM, et al. J Am Coll Radiol. 2010;7(10):754–73.
Thompson RJ, Wojcik SM, Grant WD, et al. Emerg Med Int. 2011;2011:624847.
Ekeh AP, Walusimbi M, Brigham E, et al. J Emerg Med. 2010;38(4):484–9.
Paluska TR, Sise MJ, Sack DI, et al. J Trauma. 2007;62(1):157–61.
Devine AS, Jackson CS, Lyons L, et al. West J Emerg Med. 2010;11(1):24–7.
Messersmith WA, Brown DF, Barry MJ. Am J Emerg Med. 2001;19(6):479–81.
Munk MD, Peitzman AB, Hostler DP, et al. J Emerg Med. 2010;38(3):346–50.
Yoon DY, Chang SK, Choi CS, et al. J Comput Assist Tomogr. 2008;32(5):810–5.
Youserm DM, Huang T, Loevner LA, et al. AJNR Am J Neuroradiol. 1997;18(8):1423–8.
Ahmed S, Horton KM, Jeffrey RB Jr, et al. AJR Am J Roentgenol. 2010;195(5):1066–71.
Hoang JK, Langer JE, Middleton WD, et al. J Am Coll Radiol. 2015;12(2):143–50.
Bahl M, Sosa JA, Nelson RC, et al. AJNR Am J Neuroradiol. 2014;35(11):2176–80.
Hobbs HA, Bahl M, Nelson RC, et al. AJR Am J Roentgenol. 2014;202(1):18–24.
Kroeker TR, le Nobel G, Merdad M, et al. Head Neck. 2014;36(1):126–9.
Jones EC, Chezmar JL, Nelson RC, et al. AJR Am J Roentgenol. 1992;158(3):535–9.
Padia SA, Baker ME, Schaeffer CJ, et al. J Clin Ultrasound. 2009;37(3):138–43.
Appelbaum L, Kane RA, Kruskal JB, et al. Radiology. 2009;250(2):453–8.
Whitmire LF, Galambos JT, Phillips VM, et al. J Clin Gastroenterol. 1985;7(6):511–5.
Piccinino F, Sagnelli E, Pasquale G, et al. J Hepatol. 1986;2(2):165–73.
Gore RM, Thakrar KH, Wenzke DR, et al. Cancer Imaging. 2012;12:373–84.
Heller MT, Kanal E, Almusa O, et al. et al. Emerg Radiol. 2014;21(4):341–7.
Emick DM, Carey TS, Charles AG, et al. J Trauma Acute Care Surg. 2012;72(5):1255–62.
Gupta R, Greer SE, Martin ED. J Trauma. 2010;69(2):253–5.
Sodickson A, Opraseuth J, Ledbetter S. Radiology. 2011;260(2):408–13.
Health Information Technology: Standards, Implementation Specifications, and Certification Criteria for Electronic Health Record Technology, 2014 Edition; Revisions to the Permanent Certification Program for Health Information Technology RIN 0991-AB822014. https://www.healthit.gov/policy-researchers-implementers/standards-and-certification-regulations
Khorasani R, Hentel K, Darer J, et al. AJR Am J Roentgenol. 2014;203(5):945–51.
Raja AS, Ip IK, Prevedello LM, et al. Rsna. 2011, 2012; 468–74.
Ip IK, Raja AS, Gupta A, et al. Am J Emerg Med. 2015;33(3):320–5.
Gupta A, Ip IK, Raja AS, et al. J Am Med Inform Assoc. 2014;21(e2):e347–51.
Griffith B, Bolton C, Goyal N, et al. AJR Am J Roentgenol. 2011;197(2):463–7.
Hoffman JR, Mower WR, Wolfson AB, et al. N Engl J Med. 2000;343(2):94–9.
ACR Appropriateness Criteria. American College of Radiology. http://www.acr.org/ac
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Weidman, E.K., Loftus, M.L. (2018). The Consequences of Inappropriate Use of Emergency Imaging. In: Kelly, A., Cronin, P., Puig, S., Applegate, K. (eds) Evidence-Based Emergency Imaging. Evidence-Based Imaging. Springer, Cham. https://doi.org/10.1007/978-3-319-67066-9_4
Download citation
DOI: https://doi.org/10.1007/978-3-319-67066-9_4
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-67064-5
Online ISBN: 978-3-319-67066-9
eBook Packages: MedicineMedicine (R0)