Abstract
This chapter reviews the evidence base of imaging in acute respiratory illnesses (ARI) in children and adults. Chest radiography is indicated in the very young and in patients older than 40 years with ARI suspected to have community-acquired pneumonia (CAR), especially in those who are ill enough to require hospitalization. In young children, the imaging findings of viral and bacterial lung infections frequently overlap, making their differentiation difficult. Improved communication of the radiographic findings and their limitations can decrease overprescription of antibiotics by referring physicians, when no bacterial cause can be proven. CT adds value to radiography only in pulmonary infections that are complicated, recurrent, or occur in patients with an impaired immune system. Ultrasound is favored over CT to determine the need and feasibility and need for percutaneous drainage of parapneumonic effusions and empyemas in children.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Pneumonia
- Radiography
- Computed tomography
- Ultrasound
- Evidence-based imaging
- Cost-effectiveness of diagnostics
- Emergency imaging
- Evidence-based imaging
-
Obtaining a CXR is appropriate in older patients (>40 y/o) with acute respiratory illness (ARI) (moderate evidence).
-
Obtaining a CXR is appropriate in patients with ARI and dementia (moderate evidence).
-
A CXR is not necessary for patients with ARI who are younger than 40 and have normal vital signs and a normal physical exam, provided they can follow-up, and that the risks of delayed diagnosis of pneumonia are minimal (moderate evidence).
-
A CXR is not necessary for patients with ARI, and a high pretest probability of community-acquired pneumonia (CAP) who will be treated for CAP regardless of CXR findings (moderate evidence).
-
CXRs are sufficiently sensitive and highly specific for the diagnosis of CAP in children (moderate evidence).
-
Imaging studies have a limited value with regard to differencing between bacterial and viral lower respiratory tract infection in children (moderate evidence).
-
Although CT is more sensitive than CXR for pneumonia, it is not indicated in immunocompetent adult or pediatric patients with suspected uncomplicated CAP (moderate evidence).
-
CT does provide more information than radiographs with regard to complicated pulmonary infections with bronchopleural fistula, empyema, or pleural effusion (moderate evidence).
-
In immunocompromised patients, CT is more sensitive and specific for pneumonia and should be performed in adult and pediatric cases where pneumonia is suspected, but the CXR is normal, equivocal, or nonspecific (strong evidence).
-
Ultrasound does have an advantage over CT in identifying and characterizing complicated effusions in children by being more cost-effective and not employing ionizing radiation (moderate evidence).
Definitions and Pathophysiology
Acute respiratory illness (ARI) is defined as one or more of the following: cough, sputum production, chest pain, or dyspnea (with or without fever) (Table 18.1). Most cases of ARI are caused by infection, and the most commonly encountered forms of acute infection in the chest are bronchitis and pneumonia. The distinction between acute bronchitis and pneumonia is an important one as ~90% of cases of acute bronchitis are viral in etiology and are self-limited. Pneumonia can be caused by bacterial, mycobacterial, viral, and fungal organisms and can be life-threatening; often requiring antimicrobial therapy [1]. As shown in Table 18.1, incidence of specific pathogens differs by age.
Acute bronchitis is inflammation of the airways. There are typically few if any findings on chest imaging. Pneumonia is inflammation of the pulmonary parenchyma primarily affecting the alveoli; the small sacs within the lung where gas exchange takes place, also called the “airspaces.” The primary imaging manifestations of pneumonia are those of “airspace/alveolar disease,” namely, partial alveolar filling (ground glass) and complete alveolar filling (consolidation) (Fig. 18.1a, b). “Tree-in-bud” is another common manifestation of infectious pneumonia and represents spread of infection through the terminal airways and into the central aspect of the airspaces (Fig. 18.1a, b) [2].
(a, b) Axial image from a non-contrast CT of a patient with community acquired pneumonia (CAP) (a) demonstrating airspace disease primarily manifesting as consolidation, aka complete alveolar filling. Note the air bronchogram and how the pulmonary vessels are not visible where they traverse the consolidation. CT image from a different patient with CMV pneumonia (b) demonstrates widespread ground glass, aka partial alveolar filling. Note how the pulmonary vessels are still visible as they traverse the ground-glass opacity. This patient also has some focal tree-in-bud nodularity in the dependent right lung representing endobronchial spread of infection. This pattern of mixed ground glass and nodules is common in CMV and can be very subtle on CXRs
Some of the major risk factors for pneumonia include recent viral respiratory tract infection, smoking, a variety of chronic lung diseases, young (<1 y/o) or old (>65 y/o) age, conditions that predispose to aspiration, and immunocompromised state [3].
Immunocompromised is defined as being in a state where the immune system is weakened or absent, some commonly encountered causes include acquired immunodeficiency syndrome (AIDS), chemotherapy, or other immunosuppressive drugs. Immunocompromised patients are susceptible to infection by “opportunistic” organisms. Also, they are more likely to develop widely disseminated infections. For example, in patients with AIDS, their CD4 count helps predict what types of pneumonias they are most at risk of developing (Table 18.2) [4].
Epidemiology
Pneumonia is a global health issue. Of the 156 million children estimated by the world health organization (WHO) to have pneumonia in 2008, 151 million cases occurred in developing nations, accounting for 1.6 million deaths that year, 28–34% of all deaths in those under 5 years of age [5, 6]. Pneumonia is the leading cause of death among children in low-income nations [5, 7]. The WHO estimates that one in three newborn infant deaths is due to pneumonia [8].
Pneumonia and influenza are the most common infectious causes of death in the US. In 2010, pneumonia and influenza combined was the ninth leading cause of death, accounting for approximately 50,000 deaths with an age-adjusted death rate of 15.1 per 100,000 people [9]. Pneumonia and influenza are more deadly among the elderly; death rates for those aged 65 and older in 2010 was 106.3 per 100,000 people [9]. Given the aging population, the burden of pneumonia is expected to increase, a common trend in most developed nations.
Overall Cost to Society
In 2005, the total cost to the US economy of influenza and pneumonia was estimated at $40.2 billion when including all direct and indirect costs [10]. Pneumonia was one of the top ten most expensive conditions seen during inpatient hospitalizations in the US in 2011, with an aggregate cost of nearly $10.6 billion for 1.1 million hospital stays [11]. CAP results in 10 million doctor visits and 64 million days of restricted activity annually [12]. Childhood pneumonias are a frequent cause of doctor visits, antibiotics prescriptions, loss of work days of parents, and reduction of quality of life [13].
Goals of Imaging
The main goal of imaging acute pulmonary infections in the emergency department is diagnosis. Early diagnosis will support adequate and early treatment; it could also prevent potential costs and complications. This is particularly important in patients with a weak immune system such as young children, the elderly, or the immunocompromised.
Methodology
A review of the current diagnostic imaging literature was performed utilizing PubMed, MEDLINE, and Google Scholar search databases covering January 1, 1980 through May 1, 2015. Searches were performed using various combinations of the following key terms:
-
Infection terms diagnosis, acute respiratory illness, acute bronchitis, lower respiratory tract infection, pneumonia, community-acquired pneumonia, opportunistic, HIV, AIDS, pleural effusion, parapneumonic effusion, empyema
-
Imaging terms imaging, radiology, radiography, chest, chest X-ray, chest radiography, computed tomography, CT, CAT scan, ultrasound
-
Population terms pediatric, child, children, adults, immunocompetent, immunocompromised
-
Other imaging terms cost, direct, indirect, epidemiology, impact, evidence based, appropriate, indication, indicated, guidelines
Searches were limited to English-language articles and human studies. Abstracts were reviewed and selected based on relevance, recentness, and methodology. Additional relevant articles were selected from the references of reviewed articles and from published guidelines. We excluded case reports, animal studies, and basic science articles.
Discussion of Issues
When Is a Chest Radiograph (CXR) Indicated for Workup of Suspected Chest Infection in Adults?
Summary of Evidence
-
Obtaining a CXR is appropriate in older patients (>40 years of age) with acute respiratory illness (ARI) (moderate evidence).
-
Obtaining a CXR is appropriate in patients with ARI and dementia (moderate evidence).
-
A CXR is not necessary for patients with ARI who are younger than 40 and have normal vital signs and a normal physical exam, provided they can follow-up, and that the risks of delayed diagnosis of pneumonia are minimal (moderate evidence).
-
A CXR is not necessary for patients with ARI and a high pretest probability of community-acquired pneumonia (CAP) who will be treated for CAP regardless of CXR findings (moderate evidence).
Supporting Evidence
Radiographs have been used in medical imaging for over 100 years, and the chest radiograph (CXR) is as relevant for diagnosis of cardiothoracic disease now as it was in the early days of radiography. The relatively low dose of ionizing radiation combined with excellent special resolution, low cost, and high availability make the CXR an excellent first step in the diagnostic work-up of patients with suspected chest infection. That being said, radiography, like any diagnostic tool, should be used judiciously.
Community-Acquired Pneumonia (CAP)
The major indication for obtaining a CXR in patients with ARI in the emergent setting is to confirm the diagnosis of community acquired pneumonia (CAP) when suspected based on history and physical exam. Airspace opacification , particularly consolidation (the classic finding of CAP), stands out against adjacent aerated lung and “silhouettes out” adjacent soft tissue structures resulting in a perceptible finding on CXR (Fig. 18.2a–d). Despite the fact that ARI is commonly encountered in the emergency setting, there is a paucity of large randomized controlled trials evaluating the utility of CXR in this setting. There are some data regarding when to utilize a CXR in suspected cases of CAP [14,15,16,17,18,19,20,21,22]. There are many societal guidelines concerning when to use a CXR in this setting. However, some of these guidelines are conflicting [23,24,25].
(a–d) Frontal (a) and lateral (b) CXRs from a patient with obvious CAP. Note the dense consolidation in the right upper lobe. On the lateral view the well-defined margin of the consolidation represents where it abuts the minor fissure. Frontal (c) and lateral (d) CXRs from a different patient demonstrate a slightly less obvious case of CAP in the right middle lobe. On the frontal view, there is indistinct increased density which hides the right heart border, a “silhouette sign.” On the lateral view, the consolidation is contained by the minor and major fissures resulting in well-defined margins
One of the larger prospective studies to address the use of radiography in the evaluation of ARI is Benacerraf et al. from 1981 [14]. One thousand one hundred two consecutive patients were evaluated with the goal of identifying selective indications for CXR based on age, symptoms, and physical exam findings. Put briefly, the study showed that for patients younger than 40 years with ARI symptoms but normal physical exam findings and absence of hemoptysis, the yield of CXR was exceedingly low. A study by Heckerling reviewing 464 patients confirmed that CXRs were nearly always negative in the absence of physical exam findings [15]. Patients with dementia were an exception and had a very high incidence of pneumonia on CXR (75.8%) whereas only two of the 106 patients presenting with acute asthma (1.9%) had pneumonia.
Several more recent studies have been published which evaluate when a CXR is appropriate in suspected CAP [16,17,18,19]. O’Brien et al. examined a series of 350 patients with ARI and a positive CXR with an equal number of age-matched patients with ARI and a negative CXR [16]. Their findings confirm earlier work, re-demonstrating the fact that CXRs are rarely positive in patients with ARI and a normal physical exam or normal vital signs. Only 5% of the cases of CAP occurred in this group of patients. Other studies, including a more recent Iranian study with a nearly identical design as O’Brien et al. had similar findings [18]. A random chart review by Nolt et al. identified vital sign abnormalities and age greater than 50 as independent predictors of CAP [19]. The data suggest that for most patients with ARI and an otherwise normal exam CXR is unnecessary. The authors did include exceptions for patients with unreliable follow-up or moderate to high likelihood of morbidity if CAP is not diagnosed promptly [16, 18].
A review of 2706 patients admitted to the hospital with a diagnosis of CAP by Basi et al. found that approximately one third of these patients had a negative initial CXR and only a small percentage developed radiographic evidence of pneumonia while in the hospital [20]. Other studies have shown similar findings [21, 22]. Studies such as these call into question the sensitivity of CXR for CAP in situations where there is a high pretest probability of pneumonia. In patients with a high probability of CAP based on symptoms, physical exam findings, and vital signs, the management plan is unlikely to change based on CXR findings making the exam unnecessary. Indeed, a study by Aagaard et al. showed that in clinical practice CXRs were only obtained in 61% of patients with a clinical diagnosis of pneumonia [21].
There are a variety of societal guidelines concerning the role of the CXR in the diagnostic work-up of CAP. Some of the most promulgated guidelines are those of the Infectious Diseases Society of America in conjunction with the American Thoracic Society (IDSA/ATS) [23], the American Association of Family Physicians (AAFP) [24], and the British Thoracic Society (BTS) [25]. According to the IDSA/ATS guidelines, chest radiography should be obtained whenever CAP is suspected in adults to establish the diagnosis and to aid in differentiating CAP from other common causes of ARI, such as acute bronchitis. The guidelines also state that CXRs are sometimes useful for suggesting the etiologic agent, prognosis, alternative diagnoses, and associated conditions. When the initial CXR is clear, but pneumonia is highly suspected, it may be reasonable to treat their condition presumptively with antibiotics and repeat the imaging in 24–48 h.
The AAFP also recommends CXR in the initial workup of suspected CAP to confirm the diagnosis, but gives more specific guidelines as to when a CXR in indicated for diagnosing CAP in the setting of ARI [26]:
CXR should be performed in:
-
Any patient with at least one of the following abnormal vital signs:
-
Temperature > 100° F (37.8° C)
-
Heart rate > 100 beats per minute
-
Respiratory rate > 20 breaths per minute
-
-
Any patient with at least two of the following clinical findings:
-
Decreased breath sounds
-
Crackles (rales)
-
Absence of asthma
-
The BTS guidelines are different from the American guidelines. They state that it is not necessary to perform a CXR in patients with suspected CAP unless:
-
The diagnosis is in doubt, and a chest radiograph will help in differential diagnosis and management of the acute illness.
-
Progress following treatment for suspected CAP is not satisfactory at review.
-
The patient is considered at risk of underlying lung pathology such as lung cancer.
This less aggressive approach toward CXR in the setting of suspected CAP could, at least in part, be related to the fact that medical imaging is a limited resource in the UK due to their nationalized healthcare system, the National Health Service (NHS) . These recommendations may also reflect an attempt at cost containment by the NHS. There is no strong data concerning the cost-effectiveness of obtaining a CXR in suspected CAP to either confirm or refute these guidelines.
When Is a CXR Indicated for Workup of Suspected Chest Infection in Children?
Summary of Evidence
Chest radiographs are sufficiently sensitive and highly specific for the diagnosis of CAP in children (moderate evidence).
-
Imaging studies have limited value in the differentiation between viral and bacterial lower respiratory tract infection in children (moderate evidence).
Supporting Evidence
Community-Acquired Pneumonia
Despite their limitations, there is moderate evidence to suggest that chest radiographs are sufficiently sensitive and highly specific for the diagnosis of community-acquired pneumonia (CAP) in children. Table 18.3 summarizes the test characteristics of the only three studies in which complete sensitivity and specificity data of chest radiography are available: reported sensitivities range between 71 and 87% and specificities from 90 to 98% [27,28,29]. In a few more limited studies, sensitivity and specificity values were not directly specified, but accuracy was reported to range between 58 and 77% [30, 31]. Of note, a large randomized clinical trial of children less than 5 years of age presenting in an ambulatory care setting with uncomplicated pneumonias failed to demonstrate any evidence that the routine performance of chest radiography improves clinical outcomes [32, 33].
When viral causes of ARI such as bronchiolitis are suspected, CXRs are not needed in uncomplicated cases. In a retrospective study of 298 patients in an urban children’s hospital at the University of Colorado by Roback et al., clinicians did not typically obtain CXRs in first-time wheezing episodes. The yield of radiography is greater when there is a high temperature, absence of a family history of asthma, and localized wheezing on physical exam [31]. Perlstein et al. developed a publication of a set of evidence-based guidelines as implemented at the Children’s Hospital of Cincinnati that demonstrated 20% decrease in number of CXRs ordered [34].
Therefore, recently published evidence-based practice recommendations by the Infectious Disease Society of America (IDSA) [35] and the British Thoracic Society (BTS) [36] recommend against the routine use of chest radiography in children with suspected community-acquired pneumonia who do not require hospitalization. Prior to the institution of these guidelines, CXRs were ordered in 83% of pediatric ambulatory emergency room visits, frequently inappropriately so [37]. Follow up CXRs after 4–6 weeks are only recommended for children with recurrent pneumonia involving the same lobe, to look for underlying anatomic causes [35].
In summary, accepted indications for chest radiography are severe disease necessitating hospitalization, confirmation of diagnosis when there is an atypical clinical presentation, initial assessment of complications, and exclusion of other thoracic causes of respiratory distress [33, 38].
Differentiation of Bacterial and Viral Pneumonia
In a study of 72 adult patients by Graffelman et al. in the primary care setting, limited value was found using chest radiography in predicting the etiology of viral versus bacterial lower respiratory infections. The positive predictive value and the negative predictive value for bacterial infection were 75% and 57%, respectively [39]. In young children, the classic segmental or lobar airspace consolidation as a radiographic hallmark of bacterial pneumonia is present in only a minority of cases, and this radiographic presentation is nearly absent in neonates. Bilateral interstitial opacities with peribronchial thickening and hyperinflation, thought to represent viral small airways disease (bronchiolitis, Fig. 18.3a, b), is in fact a nonspecific finding, that is indicative of a lower respiratory tract infection of any cause in young children [40]. The fixed hyperinflation, being the most important radiographic feature of pneumonia in infancy, is due to air trapping in the alveoli resulting from degrees of mucosal swelling in the relatively small-caliber terminal airways of infants that would not compromise air exchange in older individuals. In addition, the collateral pathways of ventilation via the channels of Kohn and Lambert are yet underdeveloped in small children, and finally there is more hypersecretion in the inflamed airways in children as compared to adults. This latter effect also contributes to mucous plugging of the airways, which frequently leads to (sub-) segmental atelectases, mimicking alveolar consolidations, which are frequently misinterpreted to represent bacterial pneumonia [40].
(a, b) An 18-month-old boy with respiratory syncytial virus pneumonia. (a) Frontal CXR shows perihilar streaky lung opacities and peribronchial thickening, typical of viral infections, with more focal opacity medially in the right lung base, from superimposed atelectasis. This was mistaken for alveolar consolidation indicative of bacterial pneumonia, and for this reason antibiotic treatment with Amoxicillin was given unnecessarily. (b) Lateral CXR better demonstrates air trapping in the right lung base, with flattening of the right hemidiaphragm (arrow)
A streptococcal pneumonia may initially have a strikingly round appearance in children younger than 8 years [40], thereby simulating an intrapulmonary mass or abscess, until it spreads further to reach a normal anatomic boundary such as a fissure (Fig. 18.4a, b). Staphylococcal pneumonias are frequently acquired after viral infections, such as influenza, and the virulence of this organism can cause complications such as lung necrosis (leading to post-infectious pseudocysts or pneumatoceles) or empyema. Mycoplasmal pneumonias seen predominantly in older children, although caused by a bacterium susceptible to specific antibiotics, have a radiographic appearance that frequently mimics that of a viral infection [40]. The contrary situation, a viral infection mimicking a bacterial infection, is much more common [40,41,42], and this is reflected in the low 30% positive predictive value of radiographic criteria to predict bacterial pneumonia [43]. Radiographic criteria alone overestimate the presence of bacterial pneumonia [40], potentially leading to overprescription of antibiotics. On the other hand, the main utility of CXRs in the ambulatory care setting may be that the high 92% negative predictive value of radiographic criteria for bacterial pneumonia [43] allows clinicians to withhold antibiotics in symptomatic children with a negative CXR [40].
(a, b) Frontal CXR (a) in a 37-year-old woman with HIV demonstrates round mass-like consolidation in the right lower lobe. The finding resolved several weeks later and after a course of antibiotics (b) consistent with round pneumonia. The non-segmental distribution of round pneumonia is thought to be related to exudative fluid tracking through interalveolar channels. Round pneumonia is more common in younger patients, is usually caused by Streptococcus pneumonia, and is often mistaken for a tumor or an atypical infection, such as a fungal infection
Viral and bacterial infections frequently coexist, and radiographic criteria alone do not reliably distinguish between them [35, 43, 44]. This is compounded by a reported high interobserver variability for interpretation of CXRs [45,46,47,48]. The overlap in clinical and radiographic manifestations of viral and bacterial infections of the lung in children frequently leads to communication problems between radiologists and referring physicians, due to use of inexact and poorly defined terminology in radiology reports [49]: the terms “peripheral airways disease,” “(focal) airspace consolidation,” or “(focal) infiltrate” are ambiguous, as they are interpreted in a nonuniform way by referring physicians. The only reliable finding was found to be the presence of an “alveolar infiltrate,” whereas the presence of an “interstitial infiltrate” was found to be unreliably diagnosed by pediatric radiologists [50]. As a result of this, referring physicians agree with radiologists’ interpretations in only 78% of cases, and antibiotics are frequently prescribed even when no bacterial agent can be proven [49, 51, 52]. It is, therefore, important not to overcall pediatric CXRs for the presence of a bacterial infection, which is the most common interpretation error made by radiologists unfamiliar with pediatric imaging [53, 54].
In What Situations Does Computed Tomography (CT) Add Value for Workup of Suspected Chest Infection?
Summary of Evidence
-
Although CT is more sensitive than CXR for pneumonia, it is not indicated in immunocompetent patients with suspected uncomplicated CAP (moderate evidence).
-
For complicated pulmonary infections with bronchopleural fistula, empyema, or pleural effusion, CT provides more information than plain radiographs (moderate evidence).
-
In the immunocompromised patient, CT is more sensitive and specific for pneumonia and should be performed in cases where pneumonia is suspected but the CXR is normal, equivocal, or nonspecific (strong evidence).
Supporting Evidence
Computed tomography is a 3D imaging technique with high contrast resolution. By its very nature, it will be more sensitive than CXR, which is 2D and has low contrast resolution. The increased sensitivity of CT comes with a cost. In addition to being much more expensive and less available, the dose of radiation from a chest CT is on the order of 100’s of times that of a CXR. As such, usage of CT is typically limited to situations where the examination has a high probability of changing patient management.
Community-Acquired Pneumonia
There have been a few studies evaluating the sensitivity of CT for CAP relative to CXR. Although no randomized controlled trials have been performed, there are a few retrospective reviews as well as one prospective study by Syrjala et al. which evaluated the use of CT for diagnosis of CAP by assessing 47 patients who had clinically suspected CAP and simultaneous CXR and CT [55]. CT identified all 18 cases diagnosed with CXR and an additional 8 cases which were radiographically occult. CXR “missed” 31% of the cases of pneumonia. One of the larger reviews by Hayden et al. identified 97 of 1057 ED patients with a diagnosis of pneumonia who had both CXR and CT [56]. Within this selected group, there were 26 patients (27%) who had pneumonia which was not visible on CXR. A recent observational cross-sectional study including 3423 patients by Self et al. examined CXR test characteristics for detection of pulmonary opacities relative to CT [57]. Chest radiographs showed poor sensitivity and positive predictive value (43.5% and 26.9%, respectively). A retrospective analysis of quality improvement data on adult ED patients admitted with pneumonia over 21 months in Rhode Island showed that 49/428 (11%) of the cases of pneumonia were diagnosed by CT in the setting of a negative CXR [58].
The available data clearly show that CT is more sensitive than CXR for the diagnosis of CAP. What is less clear is whether this increase in sensitivity justifies the added cost and risk of performing CT in what would prove to be a large number of patients with suspected CAP and a negative CXR. It is also not clear whether performing CT in this subset of patients would improve patient outcomes.
The IDSA/ATS consensus guidelines briefly address the use of CT in patients with suspected CAP and a negative CXR. They consider CT a reasonable alternative to empiric treatment with antibiotics and follow-up CXR when there is high clinical suspicion of CAP [23]. It would make sense to utilize CT in situations where it has the greatest change of adding value to the management of the patients. Intuitively, this would include critically ill patients in whom a timely diagnosis would reduce the morbidity and mortality associated with delayed diagnosis . The BTS guidelines state that CT scanning currently has no routine role in the investigation of CAP [25].
Complicated Pneumonia
A variety of complications, including parapneumonic effusions, empyema, cavitation, and bronchopleural fistula are possible with severe cases of pneumonia. Typically, these patients are ill and are often already hospitalized; however, complicated cases of pneumonia do occasionally present to the ED.
There have been a few studies examining the value CT adds to the workup of complicated pneumonia. Baber et al. demonstrate that CT adds value by detecting/characterizing complications in ill patients, helping to guide further management [59]. CT also helps to detect alternative diagnoses as demonstrated by Banker et al. [60]. This retrospective review sought to assess the impact of CT on clinical decision making in immunocompetent ED patients with CXR findings of pneumonia. The patients in the CT arm had more extensive clinical management, greater chance of having antibiotic regimen changed, longer hospital stay, and 16% of the CT patients had an alternative/additional diagnosis identified by CT (pulmonary embolism, lung cancer, hypersensitivity pneumonitis, multiple myeloma, renal cell carcinoma, small bowel obstruction, lung nodule, and endobronchial mass).
There are several studies in the pediatric literature which evaluate the role of CT in the management of complicated pneumonia. Donnelly et al. looked at 56 patients with complicated pneumonia who were not responding to treatment [61]. Chest CT was compared to a CXR performed earlier on the same day. All 56 CT scans demonstrated at least one finding (cavitary necrosis, abscess, bronchopleural fistula, cavitation, loculated pleural effusions, malpositioned chest tube, pericardial effusion, or bronchial obstruction) that were not seen on CXRs. A total of 110 findings were seen on CT and not on CXR, with an average of approximately of two findings per CT scan. In another retrospective analysis of 17 children who underwent both CT scanning and CXR, evidence of cavity necrosis is often seen on CT before or in the absence of findings on CXR [62].
In a case series of 42 immunocompetent children, CXR was suboptimal in detecting abscesses, bronchopleural fistulae, fluid loculations, and parenchymal involvement, when compared to CT [63]. Chest radiograph accuracy rates were reported as follows: fluid loculations (42%), abscess formation (40%), bronchopleural fistulae (33%), and parenchymal involvement (84%). A limitation of this study is the lack of reported sensitivity and specificity values. Despite these studies confirming the expected higher sensitivity of CT, it is unclear whether the value added by CT in these situations actually contributes to better patient outcomes.
Immunocompromised Patients with Acute Respiratory Illness (ARI) and a Negative Chest Radiograph
The number of immunocompromised patients is increasing driven primarily by increasing use of immunosuppressive drugs for organ transplantation, treating cancer, autoimmune conditions, and the continued presence of the human immunodeficiency virus (HIV) [64]. Pulmonary complications are common in immunocompromised patients, often initially manifesting with symptoms of ARI. Of all pulmonary complications, pulmonary infections comprise nearly 75%, many of which progress rapidly if left untreated [64, 65].
Immunocompromised patients with ARI warrant special consideration for a variety of reasons. First and foremost, the consequences of a delayed diagnosis of pneumonia are often dire. Second, immunocompromised patients are at risk for infection with a variety of opportunistic organisms which may require a unique treatment regimen. Identifying any findings which can help narrow the diagnosis to a specific organism is of great value. Also, some of these opportunistic infections can be quite subtle on CXR. This is exacerbated by the fact that these patients can have trouble mounting an effective inflammatory response to infection, necessitating a more sensitive imaging exam [66].
CT is more sensitive than CXR for pneumonia in immunocompetent patients [55,56,57,58]; studies show that this is true to an even greater extent for immunocompromised patients [64, 67,68,69]. Although CXR remains the initial imaging examination of choice due to its availability and low cost, when an immunocompromised patient with ARI and suspected pneumonia has a negative CXR, a CT scan should be performed. An observational study of immunosuppressed bone marrow transplant patients with suspected pneumonia showed sensitivities ranging between 39% and 59% using CT as the reference [64]. In a study of 49 patients with HIV and a diagnosis of CAP who received both CXR and CT at admission, CT identified all of the cases of CAP diagnosed on CXR, 9 cases. CT also identified lesions not visualized on CXR in the remaining 40 patients (82%). Some of these lesions included pleural effusions (n = 14), ground-glass opacification (n = 20), pericardial effusions (n = 8), cavitation (n = 4), cysts (n = 4), bullae (n = 4), abscess (n = 1), and pneumothorax (n = 1). In 20 of 23 cases, hilar lymphadenopathy identified on CT, was not recognized on CXR [67].
The pediatric literature also supports lowering the threshold for CT in immunocompromised patients [70,71,72,73] (Fig. 18.5a, b). In these high-risk groups, it is absolutely critical to have a high sensitivity, as failure to detect results in failure to treat and subsequent high mortality [72]. CT has been shown to have higher accuracy than plain radiography for early detection of pneumonia in immunocompromised and hospitalized patients [72, 74,75,76]. For example, in a series of 48 patients (median age of 11 years and range of 2–19 years), CXRs and CT were rated independently by three experienced radiologists and subsequently correlated with biopsy or bronchoscopic washing results [72]. CT was shown to identify more true-positive cases of bacterial and fungal pneumonia than radiography (91% versus 85%). Unfortunately, no detailed numbers of sensitivity and specificity were cited. In 87 adult patients with febrile neutropenia (median age 47, range 18–80 years), CT detected pneumonia 5 days on average earlier than chest radiographs and was more sensitive in the detection of poorly defined opacities, ill-defined nodules, consolidation, ground-glass opacities, pleural effusions, cavitations, and bullae [69].
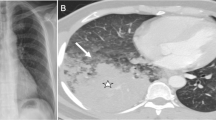
(a, b) Frontal CXR (a) from a patient with HIV, fever, and dyspnea. The patient was not on therapy for her HIV and had a CD4 count below 200. The study was read as normal, but due to the high index of suspicion for an opportunistic infection a follow-up CT was performed (b). Note the subtle patchy ground-glass opacity, a finding that is easily missed on CXR. The patient was presumptively diagnosed with Pneumocystis jiroveci pneumonia (PJP) which was confirmed with sputum testing. This case illustrates the importance of CT in the setting of an immunocompromised patient with a high index of suspicion for pneumonia and a negative CXR
Identifying Infectious Etiology in Immunocompromised Patients
In addition to increased sensitivity relative to CXR, CT also has increased specificity and is able to identify a variety of patterns of lung disease. Certain opportunistic infections have relatively characteristic patterns of pulmonary involvement which can be identified on CT with a higher degree of confidence relative to CXR [64]. Examples include Pneumocystis jiroveci pneumonia (PJP), invasive pulmonary aspergillosis, and cytomegalovirus (CMV) [77,78,79,80,81] (Fig. 18.6a–d). Recognizing these patterns and raising concerns for a particular organism based on imaging findings allows for early initiation of empiric therapy; microbiologic data may not be available for days or weeks in these cases [64, 82, 83].
(a–d) Cases showing the characteristic imaging patterns seen in PJP, angioinvasive aspergillosis, and CMV pneumonia. A frontal CXR (a) and CT (b) from a patient with HIV, low CD4 count , and PJP demonstrate the classic findings of ground-glass opacity with peripheral sparing. Also note the lack of lymph node enlargement and pleural effusions. A coronal reconstruction from a chest CT (c) from a patient with neutropenic fever demonstrates several nodular areas of consolidation with surrounding ground-glass halos representing hemorrhage. This is the classic imaging manifestation of angioinvasive aspergillus infection. Frontal CXR (d) and CT (e) images from a 41 y/o man with weakness, chills, and a CD4 count of 17 demonstrate the classic findings of CMV pneumonia. Note the widespread ground-glass opacity with superimposed areas of centrilobular nodularity. These cases illustrate the added specificity of CT over CXR. Although many infections have nonspecific findings on imaging, often there are findings which can help narrow the differential or even suggest a particular organism, as is the case with these examples. This allows for prompt empiric therapy and hopefully a better outcome for the patient
For the evaluation of children who are severely ill or immunocompromised, CT can add value in cases of fungal infection or PJP. Janzen et al., in a retrospective review of 45 children who underwent both CT and CXR, found that the first choice diagnosis was correct in 44% on chest CT and correct in 30% on CXR [70]. Equivocal or normal chest radiographs are common, reported in up to 39% of patients with PJP infection and in up to 10% of patients with other known pulmonary disease [84]. In adult AIDS patients, the high negative predictive value of high-resolution CT allows one to withhold empiric treatment for PJP pneumonia when the CT scan is negative [85].
CT can aid in the detection of fungal infections via identification of nodules, cavitation, ground-glass opacities, and halo effect [71, 72, 75]. CT can play an important role in evaluating pulmonary aspergillosis and candidal pneumonias [72]. In a study to evaluate if CT adds information to CXR, 33 cases were reviewed retrospectively [86]. It was found that in 16 cases CT added no additional useful information, but in 17 cases CT added confidence and changed management (biopsy, changing antibiotics, bronchoscopy).
In What Situations Does Ultrasound (US) Add Value for Workup of Suspected Chest Infection in Children?
Summary of Evidence
-
Ultrasound maintains an advantage over CT in identifying and characterizing complicated effusions, by its greater cost-effectiveness and because it does not employ ionizing radiation (moderate evidence).
Supporting Evidence
Complications of pneumonia in children are broadly due to accumulation of pleural fluid that may become infected and organize over time. Parapneumonic pleural effusions are almost exclusively seen in bacterial infections, and not in uncomplicated viral pneumonias [40]. However, fluid overload may also cause pleural effusions in hospitalized patients, making this distinction less clear in this group.
Ultrasound is the best test to further characterize these effusions and guide further treatment [87]. Based on appearance on imaging tests and response to treatment, pleural fluid collections may be classified as stage I (early exudative phase), stage II (intermediate fibrino-purulent phase), and stage III (late organizing phase). Reactive uncomplicated parapneumonic pleural effusions (stage I) are typically sonolucent and move with a change in patient position, whereas complicated (infected) pleural collections (stage II) exhibit an echo-complex pattern: echogenic debris, septations, and lack of movement with patient positioning [87, 88] (Fig. 18.7a–c). CT is poor in detecting these septations. CT can help to diagnose empyemas by virtue of demonstrating their mass effect on the underlying lung tissue, but published CT criteria to differentiate empyemas from uncomplicated reactive pleural effusion have been shown to be less reliable than sonographic evaluation [89].
(a–c) Empyema, role of ultrasound . Chest radiograph shows left-sided pleural collection. Ultrasound images demonstrate this collection to be complex (grade 2), with loculations, echogenic fluid, and fibrous adhesions. (Used with permission of Springer Science from Choy G, Yager PH, Noviski N, Westra SJ. Imaging of Chest Infections in Children. In Medina LS, et al., eds: Evidence-Based Imaging in Pediatrics: Improving the Quality of Imaging in Patient Care. New York: Springer Science; 2010.)
There are several studies evaluating the prognostic implications of the use of ultrasound versus CT and the implications for treatment decisions [87, 90,91,92]. Ultrasound can be helpful in both prognosis and treatment decisions. It is a low-cost test, widely available, portable, does not use ionizing radiation, and rarely requires sedation. This has to be contrasted to CT, which has a relatively high radiation dose, in the order of 100 times that of a CXR. Ultrasound is effective in demonstrating “high-grade” effusions containing septations, fronds, loculations, and debris. Ultrasound depiction of the thickness and number of these septations predict the success of chest tube drainage [87]. Kearney et al. demonstrated in a retrospective review of 50 patients who underwent both US and CT, that although both US and CT have effective roles, neither technique reliably identified the stage of pleural effusions or predicted whether patients would require surgical intervention [91]. The preponderance of evidence suggests that ultrasound is the most effective initial cross-sectional modality when pleural complications are suspected [87, 90, 92], whereas CT is the preferred modality to diagnose parenchymal complications [87, 89, 91, 93,94,95] (Fig. 18.7a–c).
Imaging Case Studies
Case 1
Figure 18.1a, b addresses a patient with community acquired pneumonia.
Case 2
Figure 18.2a–d addresses a patient with obvious CAP.
Case 3
In Fig. 18.3a, b, an 18-month-old boy with respiratory syncytial virus pneumonia is presented.
Case 4
Figure 18.4a, b presents a 37-year-old woman with HIV with round, mass-like consolidation in the right lower lobe.
Case 5
In Fig. 18.5a, b, a patient with HIV, fever, and dyspnea is presented.
Case 6
Figure 18.6a–d presents cases demonstrating characteristic imaging patterns seen in PJP, angioinvasive asperillosis, and CMV pneumonia .
Case 7
Figure 18.7a–c demonstrates the role of ultrasound in empyema.
Suggested Imaging Protocols
-
Radiography : Lateral and posterior-Anterior (PA) views are optimal. Anterior-Posterior (AP) views can be useful. Decubitus views can be helpful in distinguishing free-flowing pleural fluid versus loculated fluid collections when effusions are suspected. With extensive pulmonary parenchymal consolidation, however, the value of decubitus films for the identification of loculated versus free pleural fluid is known to be limited.
-
Chest CT: In chest infections , use of intravenous contrast is best tailored for the clinical question. Pulmonary parenchymal findings are usually easily characterized on non-contrast examinations, whereas mediastinal and pleural findings are often better characterized with contrast. Lower mA techniques (and kVp reduction in small children) can be used in the chest due to the high intrinsic contrast of air-filled lung parenchyma. Three-dimensional renditions (virtual bronchoscopy) and coronal reformats can be helpful tools to use before moving on to bronchoscopy or surgery.
-
Ultrasound : Screening includes the whole pleural space and not only the lung bases. For more overview through inter- and subcostal scanning, lower frequency (3.5–7 MHz) sector transducers are used at first; subsequently, higher frequency (10–12.5 MHz) linear transducers can be useful in uncovering more detail in the near field before marking for needle placement [96].
Future Research
Future research should focus on the following:
-
Cost-effectiveness research, for example: what is the cost-effectiveness of CXR and CT in suspected CAP?
-
How can non-ionizing imaging modalities such as ultrasound and magnetic resonance be utilized in the evaluation of pulmonary infection and its complications?
References
Gonzales R, Bartlett JG, Besser RE, et al. Ann Intern Med. 2001;134(6):521–9.
Hansell DM, Bankier AA, MacMahon H, et al. Radiology. 2008;246(3):697–722.
http://www.lung.org/lung-disease/pneumonia/understanding-pneumonia.html. Accessed 04/21/2015.
Allen CM, Al-Jahdali HH, Irion KL, et al. Ann Thorac Med. 2010;5(4):201–16.
Ruuskanen O, Lahti E, Jennings LC, et al. Lancet. 2011;377(9773):1264–75.
Singh V, Aneja S. Paediatr Respir Rev. 2011;12(1):52–9.
Kabra SK, Lodha R, Pandey RM. Cochrane Database Syst Rev. 2010;3(3):CD004874.
Rudan I, Boschi-Pinto C, Biloglav Z, et al. Bull World Health Organ. 2008;86(5):408–16.
Murphy SL, Xu J, Kochanek KD. Natl Vital Stat Rep. 2011;60(4):1–51.
Centers for Disease Control. MMWR Prevention and Control of Influenza: Recommendations of the Advisory Committee on Immunization Practices (ACIP). Vol. 56: June 2007.
Torio CM, Andrews RM. National Inpatient Hospital Costs: The Most Expensive Conditions by Payer, 2011. HCUP Statistical Brief #160. Agency for Healthcare Research and Quality, Rockville, MD, August 2013.
Current estimates from the National Health Interview Survey, 1994. US Department of Health and Human Services 1995; PHS 96-1521, Series 10:1528–935.
Shoham Y, Dagan R, Givon-Lavi N, et al. Pediatrics. 2005;115(5):1213–9.
Benacerraf BR, McLoud TC, Rhea JT, et al. Radiology. 1981;138(2):293–9.
Heckerling PS. Arch Intern Med. 1986;146(7):1321–4.
O’Brien WT Sr, Rohweder DA, Lattin GE Jr, et al. J Am Coll Radiol. 2006;3(9):703–6.
Okimoto N, Yamato K, Kurihara T, et al. Respirology. 2006;11(3):322–4.
Ebrahimzadeh A, Mohammadifard M, Naseh G, et al. Iran J Radiol. 2015;12(1):e13547.
Nolt BR, Gonzales R, Maselli J, et al. Am J Emerg Med. 2007;25(6):631–6.
Basi SK, Marrie TJ, Huang JQ, Majumdar SR. Am J Med. 2004;117(5):305–11.
Aagaard E, Maselli J, Gonzales R. Med Decis Mak. 2006;26(6):599–605.
Hagaman JT, Rouan GW, Shipley RT, et al. Am J Med Sci. 2009;337(4):236–40.
Mandell LA, Wunderink RG, Anzueto A, et al. Clin Infect Dis. 2007;44(Suppl 2):S27–72.
Watkins RR, Lemonovich TL. Am Fam Physician. 2011;83(11):1299–306.
Lim WS, Baudouin SV, George RC, et al. Thorax. 2009;64:iii1–iii55.
Adapted from Ebell MH. Am Fam Physician 2007;76(4):562.
Rigsby CK, Strife JL, Johnson ND, et al. Pediatr Radiol. 2004;34(5):379–83.
Lamme T, Nijhout M, Cadman D, et al. CMAJ. 1986;134(4):353–6.
Patenaude Y, Blais C, Leduc CP. Investig Radiol. 1995;30(1):44–8.
Graffelman AW, le Cessie S, Knuistingh Neven A, et al. J Fam Pract. 2007;56(6):465–70.
Roback MG, Dreitlein DA. Pediatr Emerg Care. 1998;14(3):181–4.
Swingler GH, Zwarenstein M. Cochrane Database Syst Rev (Online). 2005(3):CD001268.
Swingler GH, Hussey GD, Zwarenstein M. Lancet. 1998;351(9100):404–8.
Perlstein PH, Kotagal UR, Bolling C, et al. Pediatrics. 1999;104(6):1334–41.
Bradley JS, Byington CL, Shah SS, et al. Clin Infect Dis. 2011;53(7):617–30.
Harris M, Clark J, Coote N, et al. Thorax. 2011;66(Suppl 2):ii1–23.
Neuman MI, Shah SS, Shapiro DJ, et al. Acad Emerg Med Off J Soc Acad Emerg Med. 2013;20(3):240–6.
Alario AJ, McCarthy PL, Markowitz R, et al. J Pediatr. 1987;111(2):187–93.
Graffelman AW, Willemssen FE, Zonderland HM, et al. Br J Gen Pract. 2008;58(547):93–7.
Donnelly LF. J Thorac Imaging. 2001;16(4):238–50.
Osborne D. Am J Roentgenol. 1978;130(1):29–33.
Han BK, Son JA, Yoon HK, et al. Am J Roentgenol. 1998;170(4):1077–80.
Bettenay FA, de Campo JF, DB MC. Pediatr Radiol. 1988;18(6):453–4.
Miller WT Jr, Mickus TJ, Barbosa E, et al. Am J Roentgenol. 2011;197(5):1088–95.
Bloomfield FH, Teele RL, Voss M, et al. Pediatr Radiol. 1999;29(6):459–62.
Davies HD, Wang EE, Manson D, et al. Pediatr Infect Dis J. 1996;15(7):600–4.
Johnson J, Kline JA. Emerg Radiol. 2010;17(4):285–90.
Stickler GB, Hoffman AD, Taylor WF. Clin Pediatr (Phila). 1984;23(7):398–9.
Spottswood SE, Liaw K, Hernanz-Schulman M, et al. Pediatr Radiol. 2009;39(4):348–53.
Neuman MI, Lee EY, Bixby S, et al. J Hosp Med. 2012;7(4):294–8.
Grossman LK, Caplan SE. Ann Emerg Med. 1988;17(1):43–6.
Shiley KT, Lautenbach E, Lee I. Infect Control Hosp Epidemiol. 2010;31(11):1177–83.
Donnelly LF. In: Donnelly LF, editor. Diagnostic imaging: pediatrics. Amirsys; 2005. 900p.
Riggs W. Appl Radiol. 1996:38–9.
Syrjälä H, Broas M, Suramo I, et al. Clin Infect Dis. 1998;27(2):358.
Hayden GE, Wrenn KW. J Emerg Med. 2009;36(3):266–70.
Self WH, Courtney DM, McNaughton CD, et al. Am J Emerg Med. 2013;31(2):401–5.
Maughan BC, Asselin N, Carey JL, et al. RI Med J. 2014;97(8):20–3.
Baber CE, Hedlund LW, Oddson TA, et al. Radiology. 1980;135(3):755–8.
Banker PD, Jain VR, Haramati LB. Emerg Radiol. 2007;14(6):383–8.
Donnelly LF, Klosterman LA. Am J Roentgenol. 1998;170(6):1627–31.
Donnelly LF, Klosterman LA. Am J Roentgenol. 1998;171(1):253–6.
Tan Kendrick AP, Ling H, Subramaniam R, et al. Pediatr Radiol. 2002;32(1):16–21.
Cereser L, Zuiani C, Graziani G, et al. Radiol Med. 2010;115(2):205–14.
Safadi AR, Soubani AO. Eur J Intern Med. 2009;20(3):268–79.
ACR Appropriateness Criteria® acute respiratory illness in immunocompromised patients. Updated 2014.
Nyamande K, Lalloo UG, Vawda F, et al. Br J Radiol. 2007;80(953):302.
Schueller G, Matzek W, Kalhs P, et al. Eur J Radiol. 2005;53(3):489–94.
Heussel CP, Kauczor HU, Heussel G, et al. Am J Roentgenol. 1997;169(5):1347–53.
Janzen DL, Padley SP, Adler BD, et al. Clin Radiol. 1993;47(3):159–65.
Mori M, Galvin JR, Barloon TJ, et al. Radiology. 1991;178(3):721–6.
Winer-Muram HT, Arheart KL, Jennings SG, et al. Radiology. 1997;204(3):643–9.
Winer-Muram HT, Rubin SA, Fletcher BD, et al. Radiology. 1994;193(1):127–33.
Katz DS, Leung AN. Clin Chest Med. 1999;20(3):549–62.
Kuhlman JE, Fishman EK, Burch PA, et al. Chest. 1987;92(1):95–9.
Winer-Muram HT, Rubin SA, Kauffman WM, et al. Clin Radiol. 1995;50(12):842–7.
Hachem R, Sumoza D, Hanna H, et al. Cancer. 2006;106(7):1581–6.
Hardak E, Brook O, Yigla M. Lung. 2010;188(2):159–63.
Park YS, Seo JB, Lee YK, et al. Clin Radiol. 2008;63(6):673–80.
Vogel MN, Brodoefel H, Hierl T, et al. Br J Radiol. 2007;80(955):516–23.
Demirkazik FB, Akin A, Uzun O, et al. Diagn Interv Radiol. 2008;14(2):75–82.
Franquet T. Eur Radiol. 2006;16(3):707–18.
Ketai L, Jordan K, Marom EM. Clin Chest Med. 2008;29(1):77–105. vi
Franquet T. Eur Respir J. 2001;18(1):196–208.
Hidalgo A, Falco V, Mauleon S, et al. Eur Radiol. 2003;13(5):1179–84.
Barloon TJ, Galvin JR, Mori M, et al. Chest. 1991;99(4):928–33.
Ramnath RR, Heller RM, Ben-Ami T, et al. Pediatrics. 1998;101(1 Pt 1):68–71.
Mayo PH, Doelken P. Clin Chest Med. 2006;27(2):215–27.
Donnelly LF, Klosterman LA. Am J Roentgenol. 1997;169(1):179–82.
King S, Thomson A. Br Med Bull. 2002;61:203–14.
Kearney SE, Davies CW, Davies RJ, et al. Clin Radiol. 2000;55(7):542–7.
Kurian J, Levin TL, Han BK, et al. Am J Roentgenol. 2009;193(6):1648–54.
Tan Kendrick AP, Ling H, Subramaniam R, et al. Pediatr Radiol 2002, 9502;32(1):16–21.
Donnelly LF. Radiol Clin N Am. 2005;43(2):253–65.
Tu CY, Hsu WH, Hsia TC, et al. Chest. 2004;126(4):1274–80.
Coley BD. Radiol Clin N Am. 2005;43(2):405–18.
Acknowledgment
Dr. Westra would like to acknowledge the work of Drs. G. Choy, P. H. Yager, and N. Noviski, his coauthors in a previous chapter on Imaging of Chest Infections in Children in Medina LS, et al., eds: Evidence-Based Imaging in Pediatrics: Improving the Quality of Imaging in Patient Care, published by Springer Science. That chapter served as a starting point for the pediatric content in this chapter, which has been thoroughly updated and revised for the topic at hand.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Westra, S.J., Jokerst, C. (2018). Acute Chest Infections in Adults and Children: Evidence-Based Emergency Imaging. In: Kelly, A., Cronin, P., Puig, S., Applegate, K. (eds) Evidence-Based Emergency Imaging. Evidence-Based Imaging. Springer, Cham. https://doi.org/10.1007/978-3-319-67066-9_18
Download citation
DOI: https://doi.org/10.1007/978-3-319-67066-9_18
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-67064-5
Online ISBN: 978-3-319-67066-9
eBook Packages: MedicineMedicine (R0)