Abstract
Background
In our cost- and radiation-conscious environment, the feasibility of performing only a frontal radiograph for the diagnosis of pneumonia in children needs to be reassessed.
Objective
To determine the diagnostic efficacy of the frontal radiograph alone in comparison to the frontal and lateral combined radiographs for the radiographic diagnosis of pneumonia in children.
Materials and methods
Three radiologists retrospectively and independently reviewed the frontal radiographs alone and separately reviewed the frontal and lateral radiographs of 1,268 children referred from the emergency room for chest radiographs. A majority interpretation of at least two radiologists for the frontal views alone was compared with majority interpretation of the frontal and lateral combined views for the radiographic diagnosis of pneumonia. “Pneumonia” was defined as a focus of streaky or confluent lung opacity.
Results
For the radiographic diagnosis of pneumonia, the sensitivity and specificity of the frontal view alone were 85% and 98%, respectively. For the confluent lobar type of pneumonia, the sensitivity and specificity increased to 100%.
Conclusion
When the frontal view alone yields a diagnosis of confluent lobar pneumonia, this is highly reliable. However, nonlobar types of infiltrates will be underdiagnosed in 15% of patients using the frontal view alone. The clinical impact of these radiographically underdiagnosed pneumonias needs to be assessed prior to implementing the practice of using only frontal radiographs for diagnosing pneumonia.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Chest radiography is the most commonly performed pediatric imaging procedure. At our institution, 24,000 chest radiographs are performed per year, and approximately 30% of these are performed on patients referred from the emergency department for evaluation of possible pneumonia. The use of frontal and lateral views is standard practice in chest radiography [1, 2]. The evidence to support this standard practice based on a large group of children is lacking. The purpose of this study was to determine the diagnostic efficacy of the frontal radiograph alone in comparison to the frontal and lateral combined radiographs for the radiographic diagnosis of pneumonia in children referred from the emergency room.
Materials and methods
Population
This retrospective study was performed at a large metropolitan children’s hospital, which has primary, secondary, and tertiary care patients in its population base. Patients were selected for the study by searching the radiology billing database for emergency department patients who had chest radiographs performed between 1994 and 1995. Patients who had both frontal and lateral radiographs available for review were included in the study. Patients with only one-view chest radiographs were not included in the study.
Imaging
All patients identified had undergone standard chest radiography, including both frontal and lateral views. In general, frontal radiographs of children who were able to stand were performed in the erect position (anteroposterior in younger children and posteroanterior in older children). All other children were imaged supine (anteroposterior). DuPont-Sterling Cronex Ortho TL (Sterling Diagnostic Imaging, Wilmington, DE) film with a Kodak Lanex Regular screen (Eastman-Kodak, Rochester, NY) was used for all chest radiographs.
Image analysis
Groups of 50–100 radiographs were presented by a research assistant on a viewbox for review by three pediatric radiologists, two faculty members, and one fellow. All interpretations were performed independently. A consensus opinion was not generated for any patient [3]. For each patient, either the frontal radiograph alone was presented first, followed by the frontal and lateral radiographs during a different interpretation session, or the frontal and lateral radiographs were presented first, followed by the frontal radiograph alone during a different interpretation session. The interpretation sessions for the frontal view and frontal and lateral views of the same patient were separated in time by at least 2 weeks, and the order of presentation of the radiographs was changed to avoid recall of patient diagnosis. The official interpretation rendered at the time the radiographs were performed was not used in this study.
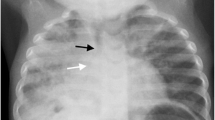
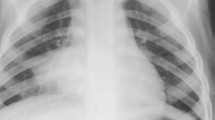
The images were reviewed for the presence or absence of pneumonia. Pneumonia as defined for the purposes of this study was any focus, either confluent or streaky, of increased lung opacity with or without associated air bronchograms and/or the presence of a silhouette sign. The images in Fig. 1 represent the radiographic range of what was defined as pneumonia in this study. A standardized data collection sheet was used by the research assistant to record the interpretation of each examination by each radiologist. Each study was given either interpreted as positive or negative for pneumonia. No indeterminate option was allowed. The presence or absence of peribronchial thickening, hyperinflation, cardiac abnormality, and bone abnormality was also recorded, but was not used for study analysis.
Statistical analysis
Using the pneumonia prevalence estimate from a published study, we estimated that a sample size of 1,218 patients would be necessary to detect a difference between the frontal and lateral combined views and frontal views alone using a positive rate of 20% for the frontal and lateral combined views and 15% for the frontal view alone for the presence of pneumonia (P=0.05; power 80%) [4].
Data were entered into a spreadsheet and analysis was performed using SAS (SAS Institute, Cary, NC). When the spreadsheet indicated an agreement of at least two of the three independent readers for the presence of pneumonia (majority interpretation), the study was considered positive for pneumonia. When the spreadsheet indicated an agreement of at least two of the three independent readers for the absence of pneumonia (majority interpretation), the study was considered negative for pneumonia. The data for the frontal and lateral combined views and the frontal views alone were evaluated separately.
The majority interpretation of each patient’s frontal view alone was then compared with the majority interpretation of the frontal and lateral views for each patient. From this comparison, the sensitivity, specificity, false-negative and false-positive rates, positive and negative predictive values, and accuracy of the frontal views alone for the diagnosis of pneumonia were calculated to determine the utility of the lateral view. Chi-squared analysis was used to determine if patient age had any effect on the usefulness of the lateral view.
For each individual reader’s interpretation of the frontal view alone and the frontal and lateral views combined, intrareader and interreader agreement rates and the generalized kappa statistic were calculated [5]. The kappa statistic was used as a statistical measure of the agreement in interpretation between the radiologists. Each individual reader’s interpretation of both the frontal views alone and the frontal and lateral combined views was compared with the majority interpretation of both the frontal views alone and frontal and lateral combined views, respectively, to evaluate the variance between individual readers.
Results
Majority data
A total of 1,268 patients ranging in age from newborn to 18 years (mean age 4 years) were included in the study. Forty-two percent were female and 58% were male. A total of 7,608 interpretations were performed. Using the majority interpretation of the frontal and lateral combined views, a radiological diagnosis of pneumonia was made in 240 of the 1,268 patients for a prevalence of disease in our population of 19%. Using the frontal view alone, a radiological diagnosis of pneumonia was made in 227 patients. Therefore, using the frontal view alone, pneumonia was underdiagnosed in 37 of 240 cases for a false-negative rate of 15%. Also, using the frontal view alone, a radiological diagnosis of no pneumonia was made in 1,041 patients versus 1,028 patients using the frontal and lateral combined views. Therefore, pneumonia was overdiagnosed in 24 of 1,028 of cases using the frontal view alone for a false-positive rate of 2.3% (Table 1). This yielded a sensitivity of 85%, specificity of 98%, positive predictive value of 89%, negative predictive value of 96%, and accuracy of 95% of the frontal view alone for the diagnosis of pneumonia. There were 165 cases for which the diagnosis of pneumonia was made by all three readers on the frontal and lateral combined views. All of these cases were also considered positive by all three readers on the frontal view alone. Upon review, in nearly all cases where all three readers read the radiographs as positive, the infiltrates present tended to be of the confluent-lobar type, as seen in Fig. 1. No cases of confluent lobar pneumonia were under- or overdiagnosed on the frontal views alone.
There was no statistically significant difference in the underdiagnosed cases of pneumonia on the frontal views alone compared to the frontal and lateral views combined for patient age using the Chi-squared method (P=0.5).
Individual reader variability
Interobserver agreement rates between the three readers for the frontal views alone and frontal and lateral combined views are listed in Tables 2 and 3, respectively. Intraobserver agreement rates for each reader for the frontal views alone and frontal and lateral combined views are listed in Table 4.
Discussion
The 19% prevalence of disease in our population underscores the difficulty of diagnosing pneumonia based on clinical signs and symptoms alone [6, 7, 8]. In our study, false-negative and positive rates of the frontal radiograph alone for the diagnosis of pneumonia are 15 and 2.3%, respectively. In a study of similar design, Kennedy et al. in a study of 414 children underdiagnosed pneumonia on the frontal view alone with a false-negative rate of 2.2% [9]. In another study of 357 children, the sensitivity and specificity for detection of pneumonia on the frontal view alone were 71 and 90%, respectively, for a false-negative rate of 29%. However, on a retrospective review, the authors considered only 6% of these false-negatives to be of significance [10]. The impact of these false-negative diagnoses on patient management and outcome was stated as low in both studies, but the relatively small sample sizes limit the statistical significance of these statements. Differences in age distribution of patients, emergency room referrals, sample sizes, and differences in population bases likely contribute to the differences in pneumonia detection rates between each of these studies and ours. In a retrospective study of 179 hospitalized children with suspected acute pulmonary illness, Lamme et al. found that the lateral view increased the sensitivity from 81 to 87% and the specificity from 94 to 96% when compared to the chart diagnosis. The impact of the radiographic diagnosis on the chart diagnosis in this study is not clear [4].
Our kappa values of 0.71 and 0.72 for interobserver agreement rates for the frontal and the frontal and lateral interpretations, respectively, indicate very good agreement between interpreters. In a prospective multicenter study performed in adults with suspected community-acquired pneumonia, an interobserver kappa value of 0.37 was reported for the presence or absence of an infiltrate, indicating a fair-to-good correlation [8]. That study was performed on an adult population, and copies of the initial radiographs were interpreted rather than original radiographs, both of which likely contribute to the lower kappa values relative to those found in our study. Melbye and Dale determined the kappa-agreement in readings of chest radiographs in 319 adults with suspected acute respiratory infections between three radiologists and a resident in radiology to be 0.50 and the kappa agreement between the same three radiologists and an consultant in chest medicine to be 0.72 [11]. These values more closely parallel those obtained in this study.
One major difficulty encountered in this study is the lack of availability of a true pathological gold standard for the diagnosis of pneumonia. Clinically, the diagnosis is also difficult because of the nonspecific nature of presenting symptoms and the difficulty in obtaining sputum cultures in children [6, 12]. We therefore chose to adopt predefined criteria for the radiographic diagnosis of pneumonia. The wide variability in what we considered pneumonia may have contributed to a decrease in our overall sensitivity for its diagnosis. Additionally, interstitial infiltrates, peribronchial thickening, and lung hyperinflation, which can be signs of bacterial or viral pneumonia, were not evaluated. In a prospective study of lower-respiratory infections in infants, the highest agreement rates for chest radiograph interpretation were in those positive for airspace disease with a kappa of 0.92. The agreement rate for a normal chest radiograph interpretation was 0.66 and for atelectasis 0.78 [13]. These results underscore the variability in interpretation of chest radiographs and also underscore the higher agreement rates for confluent lobar pneumonias. Our 100% specificity for diagnosing confluent lobar pneumonias parallels their results.
We did not assess the effect of the potential misdiagnosed cases of pneumonia using the frontal views alone on patient management, as the goal of this study was to determine the impact of the lateral radiograph on the radiological diagnosis of pneumonia. This study was designed to conform to level two of the six-tiered hierarchical model of efficacy of diagnostic imaging proposed by Fryback and Thornbury [14]. We do, however, recognize the importance of determining the impact of the radiographic diagnosis of pneumonia on the ultimate patient management and outcome. In a study of 155 emergency department children, Grossman et al. showed that the radiographic diagnosis of pneumonia alters treatment from a preradiography diagnosis in 22% of cases [6]. Since the radiological diagnosis has an impact on treatment, an accurate and consistent radiological diagnosis is necessary. Given the high sensitivity and specificity of the frontal radiograph alone for confluent lobar pneumonias, when the frontal view alone yields a diagnosis of confluent lobar pneumonia, this is highly reliable. In these cases, the lateral radiograph may be omitted without a penalty. With the slightly lower sensitivity of the frontal view alone for all types of infiltrates, pneumonia will be radiographically underdiagnosed in 15% of patients. Many of the nonconfluent streaky infiltrates may represent atelectasis and may not be treated clinically as pneumonia. The clinical effects of eliminating the lateral radiograph in these patients must be assessed prior to implementing the practice of performing frontal radiographs alone. In our cost- and radiation-conscious environment, omitting the frontal view without a significant clinical impact would be valuable.
References
Kirks DR (1991) Practical imaging: diagnostic radiology of infants and children, 2nd edn. Little, Brown, Boston, pp 516–519
Fraser RG, Paré JAP (1978) Diagnosis of diseases of the chest, 2nd edn. Saunders, Philadelphia, pp 185–186
Obuchowski NA, Zepp RC (1996) Simple steps for improving multiple-reader studies in radiology. AJR 166:517–521
Lamme T, Nijout M, Cadman D, et al (1986) Value of the lateral radiologic view of the chest in children with acute pulmonary illness. Can Med Assoc J 134:353–356
Bartko JJ, Carpenter WT (1976) On the methods and theory of reliability. J Nerv Ment Dis 163:307–313
Grossman LK, Caplan S (1988) Clinical, laboratory, and radiological information in the diagnosis of pneumonia in children. Ann Emerg Med 17:43–46
Kiekara O, Korppi M, Tanska S, et al (1996) Radiological diagnosis of pneumonia in children. Ann Med 28:69–72
Albaum MN, Hill LC, Miles M, et al (1996) Interobserver reliability of the chest radiograph in community-acquired pneumonia. Chest 110:343–350
Kennedy J, Dawson KP, Abbott GD (1986) Should a lateral chest radiograph be routine in suspected pneumonia? Aust Pediatr J 22:299–230
Patenaude Y, Blais C, Leduc CP (1995) Reliability of frontal chest X-ray in diagnosing pulmonary opacities in children. Invest Radiol 30:44–48
Melbye H, Dale K (1992) Interobserver variability in the radiographic diagnosis of adult outpatient pneumonia. Acta Radiol 33:79–81
Anonymous Editorial (1998) Pneumonia in childhood. The Lancet 1:741–743
Davies HD, Wang EEL, Manson D, et al (1996) Reliability of the chest radiograph in the diagnosis of lower respiratory infections in young children. Pediatr Infect Dis J 15:600–604
Thornbury JR (1994) Clinical efficacy of diagnostic imaging: love it or leave it. AJR 162:1–8
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rigsby, C.K., Strife, J.L., Johnson, N.D. et al. Is the frontal radiograph alone sufficient to evaluate for pneumonia in children?. Pediatr Radiol 34, 379–383 (2004). https://doi.org/10.1007/s00247-003-1128-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-003-1128-x