Abstract
Suprasellar lesions are varied in pathology, but are challenging due to the proximity to the optic apparatus, pituitary gland, infundibulum, hypothalamus, and third ventricle. Surgical interventions to remove these lesions may result in visual field loss, endocrine dysfunction, and hydrocephalus. The endoscopic endonasal transplanum and transtuberculum approach is the defining endonasal endoscopic approach to the suprasellar lesions and is the most direct route to the region that avoids manipulation of the optic nerves and carotid artery that obviates the need for brain retraction. Meningiomas, craniopharyngiomas, and pituitary adenomas are common examples of lesions that can be resected using these approaches. These approaches differ from traditional microneurosurgical approaches with the instruments and endoscopic techniques that are utilized. Safety and success of these procedures require careful patient selection and expertise in the endonasal endoscopic method.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
5.1 Introduction
The suprasellar space is defined by the diaphragma sellae inferiorly and the floor of the third ventricle superiorly. A “craniectomy” achieved by removing the tuberculum sella, prechiasmatic sulcus, and posterior planum sphenoidale opens the suprasellar space. It can be divided into the infrachiasmatic, suprachiasmatic, and retrochiasmatic areas. The infrachiasmatic space is between the optic chiasm and the pituitary gland. The infundibulum is the key structure in this area and is covered by the suprasellar cistern arachnoid anteriorly and the membrane of Liliequist posteriorly. Tuberculum sellae meningiomas that extend into this area displace the infundibulum and superior hypophyseal arteries posteriorly. The suprachiasmatic space is above the optic chiasm as the name implies. The posterior olfactory tract, the A1 segments, the anterior communicating artery, and A2 segments of the anterior cerebral artery are the key structures in this area. Planum meningiomas arise in this space and generally displace the optic chiasm and anterior cerebral artery complexes as well as recurrent artery of Heubner and the fronto-orbital artery posteriorly and/or inferiorly. The retrochiasmatic space extends from the infundibulum to the posterior perforated substance, cerebral peduncles, and interpeduncular cistern posteriorly and to the third ventricle superiorly. Craniopharyngiomas and Rathke’s cleft cysts often extend into this space [1].
5.2 Rationale
Surgical lesions of the suprasellar region are varied in pathology (Table 5.1), but they commonly present a challenge to the neurosurgeon due to the proximity to the optic nerves and chiasm, pituitary gland, infundibulum, hypothalamus, and third ventricle. Lesions in this region are frequently benign, but pathologies and surgical interventions to remove these may result in visual field loss, endocrine dysfunction, and hydrocephalus. Surgical decision-making becomes a complex process of balancing aggressive resection strategies with the goal of minimizing cognitive, ophthalmologic, and endocrine morbidity [2].
Until recently, lesions of the suprasellar space were treated solely with open transcranial approaches from above. These approaches involve brain retraction; require work through small triangles defined by the cranial nerves, the internal carotid artery (ICA) , and its branches; and cause cosmetic compromise [3,4,5,6]. The last decade has been marked by the advancement and the popularization of the endonasal endoscopic approaches (EEA) that use minimal access strategies such as a natural orifice like the nostrils but also facilitate aggressive oncologic surgery. The endoscopic endonasal transplanum and transtuberculum approach is the defining EEA to the suprasellar cistern and is the most direct route to the region that avoids manipulation of the optic nerves and carotid artery [5]. It provides a direct route to suprasellar lesions that obviates the need for brain retraction . Also, unlike a transcranial approach, it does not place critical neurovascular structures such as the optic nerves and carotid arteries between the surgeon and the tumor. It facilitates complete, bilateral optic canal decompression without manipulation of a compressed optic nerve. Moreover, approaching these tumors from below enables the surgeon to remove the bone at the base of the tumor, which is a common site for meningioma recurrence, and to interrupt the dural vascular supply early in the operation, minimizing blood loss [7].
With joint effort from the disciplines of neurosurgery and otolaryngology, endoscopic endonasal procedures can now deliver a unique view above the sella into the suprasellar cistern, even to the roof of the third ventricle and the interpeduncular cistern [8]. The key to the success of this “minimal access” but maximally aggressive approach is in careful case selection. Due to its limitations and capabilities, EEA requires specific understanding of the pathology from an endoscopic perspective and the acquisition of the key methods that are required to endoscopically access and resect these lesions [5]. The case selection and the surgical decision-making for an endonasal endoscopic surgeon involve three questions that need to be answered [5]: A target (where?), the nature of the lesion (what?), and the approach (how?). For the purpose of this chapter, the target is the suprasellar cistern, and we will go over the approach required to get there and discuss the nuances for specific pathologies.
5.3 Patient Selection
Indications
Any lesion located or extended into the suprasellar space exerting mass effect, causing neurologic, endocrinologic, or ophthalmologic symptoms, or any lesion which requires a tissue diagnosis is an indication for a suprasellar approach to either resect or biopsy these lesions as necessary. Large tumors that cannot be completely resected using an endonasal approach are not always a contraindication. Depending on the age of the patient and the surgical goals, internal decompression or staged resection with an additional transcranial or cranioendoscopic approach may be appropriate [9].
Patients with any visual symptoms or compression of the optic apparatus on imaging should undergo a detailed neuro-ophthalmologic examination with visual field testing. Full endocrinologic workup is usually indicated to establish baseline hormone deficiencies. A comprehensive neuroradiological evaluation of the lesion is of paramount importance. MRI of the brain and specifically a pituitary protocol MRI with fine coronal cuts is required for tumors of the sella. The location of the bony septations within the sphenoid sinus and the location of carotid arteries should be determined by CT or CTA as needed [7].
The pneumatization level of the sphenoid sinus should be evaluated. A detailed plan for the extent of the craniectomy to adequately expose a surgical corridor should be determined. Septal perforations and spurs should be identified to establish whether a nasoseptal flap can be raised and from which sides of the septum or whether another type of flap will be required for closure.
Contraindications and Considerations
The endonasal endoscopic approach is often not suitable for malignant tumors that might require en bloc resection. However, there are no data showing that en bloc resection is any better with a piecemeal gross-total resection with negative margins, followed with fractionated radiation or radiosurgery [7, 10,11,12,13,14]. Pathology which extends laterally over the orbits or lateral to or behind the carotid arteries is difficult to remove using EEA. The width of the planum sphenoidale, between the laminae papyracea, has been measured in cadaver studies at 26 ± 4 mm, which narrows to 16 ± 3 mm at the posterior aspect of the tuberculum sellae [7, 15]. This width defines the preferred corridor by the EEA and optimally exposes the medial aspect of the optic canals [7]. Beyond these boundaries, even though visualization is achieved with the use of angled scopes, resection of a lesion around a corner may not be technically feasible [9]. Encasement of neurovascular structures is not a contraindication to this approach, but the surgeon will have to consider his or her ability to safely dissect a tumor off a vital structure and should keep in mind the possibility of radiosurgery and fractionated radiation to control the growth of residual unresectable tumor [9].
Although, cavernous sinus invasion is not an absolute contraindication, it requires the surgeon to be cognizant of surgical goals. The additional risks to the neurovascular structures should be considered [16]. Similarly, vascular encasement of the A2 branches of the anterior cerebral artery is not an absolute contraindication but deserves a similar consideration. Edema within the brain or floor of the third ventricle is not an absolute contraindication, but leaving the tumor invading into the hypothalamus, which commonly occurs in craniopharyngiomas , may be appropriate to preserve function. It is important to remember the differential diagnosis of large macroadenomas. These may include suprasellar lesions such as hypothalamic hamartomas, large intracranial aneurysms, and germ cell tumors, which may not be suitable for this approach. Appropriate preoperative imaging and screening should be undertaken to rule out such lesions preoperatively [16].
5.4 Surgical Technique
Instruments
EEA instruments and the standard transcranial microsurgical instruments are different in design. Long straight, rather than bayoneted, or pistol-grip instruments are better for endoscopic approaches. Monopolar cautery is favored during the approach for nasal and sphenoid mucosal bleeding, while bipolar coagulation is used on the dura and intracranial structures. A tissue shaver or micro-debrider is useful for resection of intranasal pathology, whereas intracranial pathology requires instruments of precision such as a NICO Myriad (Indianapolis, IN) or gentle bimanual suction. 18″ and 30″ endoscopes with 0°, 30°, and 45° lenses are required. A sheath around the scope can be used to irrigate and clean the lens during the operation for maximized efficiency. A scope holder helps maintain a fixed, steady field of view during the case, which is very valuable during fine dissection although having a second individual drive the scope also has its advantages. High-definition, large monitors enhance visibility and surgeon’s comfort [16].
The Approach
The operation is done under general anesthesia. We routinely use cefazolin or triple antibiotics (vancomycin, a second-generation cephalosporin and Flagyl) when the arachnoid is expected to be opened. A lumbar drain is placed, and 0.25 ml of 10% fluorescein (AK-Fluor®; Akorn, Buffalo Grove, IL, USA) is injected in 10 ml of CSF to help visualize CSF leaks [17, 18]. With the use of cottonoids soaked in 4 ml of 4% cocaine, the nasal mucosa is vasoconstricted early during the preoperative preparations. The patient’s head is pinned in a Mayfield skull clamp, slightly extended (15°) and turned toward the patient’s right (15°) to facilitate exposure of the subfrontal anterior cranial compartment. The head is elevated above the heart to enable better venous drainage. The abdomen and/or lateral thigh are prepped for autologous fat and fascia lata grafts. By using a 0°, 18-cm, 4-mm rigid endoscope (Karl Storz, Tuttlingen, Germany), we inject the mucosa adjacent to the sphenopalatine, anterior and posterior ethmoidal arteries, and the middle turbinates with a mixture of 1% lidocaine and epinephrine (1:100,000) [19]. A bilateral approach is generally preferred for resection of meningiomas to improve visualization and working space. Since the endoscope sits in the top of the left nostril, the superior turbinate is often sacrificed on this side to create room. For tumors in which large dural and skull base defects are anticipated, we favor harvesting single or bilateral nasal septal flaps before proceeding with the intranasal exposure (Fig. 5.1). This maximizes the size of these mucosal grafts and preserves the vascular pedicle(s) until rotation and placement at the end of the surgery. The flaps are stored in the oropharynx during the remainder of the procedure [19].
The ostium of the sphenoid sinus is located and then enlarged to expose the sphenoid sinus (Fig. 5.2). The posterior third of the nasal septum adjacent to the vomer and maxillary crest is resected with a tissue shaver. At this point, a panoramic view of the sphenoid sinus is achieved, and bimanual surgery with four separate instruments becomes possible. The sphenoid sinus rostrum is fully exposed, and the floor and lateral wall of the sphenoid sinus are drilled down to facilitate placement of the nasoseptal flap at the end of the operation on a flush surface. Removing the anterior wall of the sphenoid sinus is recommended to provide enough room for the endoscope and instruments to fit within the sphenoid sinus during the procedure. Fracturing the thin cribriform plate should be avoided; it is a common site of iatrogenic CSF leak. Sphenoid septa are removed, and the mucosa of the sphenoid sinus is completely removed to prevent mucocele formation under the nasoseptal flap. The keel or rostrum of the sphenoid is removed so the flap will lay smoothly on the sinus floor and not have to stretch to reach the defect.
Hemostasis is achieved with the use of warm saline irrigation and/or thrombin-soaked gelfoam with gentle pressure. At this point a 0°, 30-cm, 4-mm rigid endoscope is introduced through the nostril and stabilized with a scope holder. Anatomical landmarks like the carotid protuberance, optic protuberance, and medial and lateral opticocarotid recesses are identified (Fig. 5.3). With the use of neuronavigation, the anterior and lateral extent of the sphenoid opening is evaluated. The borders of the opening are the medial opticocarotid recesses laterally and the clival recess inferiorly. At this point onward, the use of a diamond drill and copious irrigation is recommended for an accurate, atraumatic bone removal. The upper third of the sella is opened by using a high-speed drill, curette, and Kerrison rongeur. The opening is extended anteriorly above the level of the diaphragm sellae, and the planum sphenoidale is removed, the anterior extent of which is determined by the pathology. Certain cases may require bilateral posterior ethmoidectomies to optimally visualize the anterior part of the planum sphenoidale. Injury to the posterior ethmoidal arteries should be avoided by identifying and coagulating them. The use of image guidance is recommended at this stage. If necessary for the exposure, depending on the pathology, the bone overlying the medial opticocarotid recess is then drilled thin in an eggshell manner, and curettes are used to unroof the optic canals. Kerrison rongeurs should be avoided in osseous decompression of the medial optic nerves as the instrument’s footplate when placed within the tight confines of the optic canal can injure the nerve and result in vision loss. It is recommended that the location of the carotid and ophthalmic arteries are verified with the use of a Doppler ultrasound probe [19, 20].
Intradural Surgery
Prechiasmal tumors , represented most commonly by meningiomas of the planum and tuberculum sella, can be visualized once the dura is opened. The micro-Doppler should be used to identify the location of the carotid artery prior to opening the dura. In the case of carotid injury at any point in the operation, hemostasis should be achieved either by coagulation or packing, and the patient should be taken for emergent endovascular assessment and treatment [16]. The dura above and below the superior intercavernous sinus is opened with a sickle knife horizontally, and the sinus is coagulated and cut just medial to the cavernous sinus bilaterally. It is a safe habit to use the sickle knife only along the midline and extend the dural opening by a blunt dissector to prevent accidental carotid injury. Dura can be cut and coagulated and can be removed with a Kerrison since it will not be used during the closure. Internal decompression is performed, depending on the consistency of the tumor using suction, a NICO Myriad® (Indianapolis, IN, USA), monopolar ring cautery (Elliquence, Baldwin, NY, USA), or microscissors. Tumor decompression with the use of a pituitary rongeur is also possible, although care must be taken to avoid placing excessive traction on the tumor with unnecessary tension on neurovascular structures. The blood supply is interrupted by the nature of the transtuberculum transplanum approach, and the tumor could be internally decompressed without having to operate around the optic nerves or carotid arteries. Once decompression is achieved, the tumor capsule could be mobilized easily; then the ACoA complex and perforating arteries can be dissected sharply off the tumor. The optic nerves and pituitary stalk can be clearly seen posterior and inferior to the tumor and can be dissected off the back of the tumor, respecting the arachnoidal plane. The remaining capsule should be removed completely if possible. The resection cavity and the course of the optic nerve into the optic canal can be examined for residual tumor using a 45°, 18-cm long, 4-mm diameter rigid endoscope. For tuberculum meningiomas, the diaphragm, which is often the site of origin of the tumor, is removed in total at the end of the operation to ensure a complete resection [20].
Postchiasmal tumors are generally represented by craniopharyngiomas or Rathke’s cleft cysts, which arise from the back of the pituitary stalk and extend into the third ventricle behind the optic chiasm. Because the lesions usually extend posteriorly into the third ventricle, removal of the entire planum is usually not necessary to access them. Although the 30° scope may be useful as needed, most of the dissection can often be performed with a 0°, 30-cm, 4-mm rigid endoscope. After the dura is opened above and below the intercavernous sinus as described above, the arachnoid of the suprasellar cistern is incised, and a corridor is opened between the pituitary gland below and the optic chiasm above. This chiasm-pituitary corridor (CPC) is the gateway to access these lesions, and the size of this corridor does not usually affect the ability to access and safely resect them. If the tumor is immediately apparent and is pushing up the chiasm, this may increase the CPC. If this is not the case, slight upward pressure on the chiasm and downward pressure on the pituitary gland can be tolerated.
The stalk can be encountered in the front, in the middle, or behind the tumor. The patient’s preoperative hypothalamic-pituitary function and operative goal dictates the strategy of dealing with the stalk. If the patient already has hypopituitarism with DI, the surgeon can sacrifice and resect the stalk. It is possible to mobilize the pituitary gland or work through a corridor below the pituitary gland via another small bony opening [6]. Internal decompression of the tumor, especially in large tumors, with drainage of the associated cysts may facilitate mobilization of the capsule and sharp dissection. The solid components are carefully dissected free from the optic chiasm and stalk. It is extremely important to visualize and preserve critical neurovascular structures such as the carotid arteries, the anterior communicating artery complex, and hypothalamic and chiasmal perforators. In the face of hypothalamic invasions, it is recommended to leave capsule/tumor behind for adjuvant radiotherapy rather than risk hypothalamic injury. The tumor bed including the third ventricle and interpeduncular cistern can be visualized with a 45°, 18-cm, 4-mm rigid endoscope, and residual tumor may be removed if found [20].
Closure
After resecting large tumors, the defect in the skull base may be quite large, and there may be excessive dead space under the brain. We do not recommend using fat to fill this space as it is unnecessary if a good closure is done and the postoperative imaging will be confusing. Intradural Duraform (DePuy Synthes, West Chester, PA, USA) can be used although this is not required. We recommend the use of the “gasket-seal closure” after EEA [21, 22]. A fascia lata graft that is close to double the size of the defect in the skull base is laid over the craniectomy site. A piece of Medpor® (Porex, Fairburn, GA, USA) that is cut to fit the defect is countersunk over the graft and wedged in place (Fig. 5.4). The nasoseptal flap, kept in the nasopharynx during the procedure, is placed on the defect making sure that it is placed on top and beyond the fascia lata touching skull base at the edges. Finally, the closure is covered with polymerized hydrogel (DuraSeal®; Confluent Surgical, MA, USA) on top of the nasoseptal flap to keep it in place. The sphenoid sinus, ethmoid sinuses, and roof of the nose are filled with thrombin-infused gelatin matrix (FloSeal; Baxter, IL, USA) to facilitate hemostasis [19, 20]. If a large sellar opening is performed as would be done to resect a giant macroadenoma, we do not use the gasket-seal technique since the curvature from the bottom of the sella to the front of the planum does not accommodate a rigid inlay. In this situation, we place fat in the sella, buttress the fat with Medpor, and cover it with a nasoseptal flap and DuraSeal [16].
5.5 Common Lesions
Pituitary Adenomas
Pituitary adenomas represent approximately 7–17% of all intracranial tumors. They arise from adenohypophyseal cells in the anterior pituitary, and despite their benign histologic nature, they may enlarge and invade surrounding structures [23, 24]. They are categorized as functional or nonfunctional depending on whether they are hormonally active or not. Prolactinomas, the most common functional adenoma, are treated with dopamine-agonist medical therapy , with surgical treatment reserved for patients who fail or do not tolerate the medical therapy. Transsphenoidal surgery remains the primary treatment for adenomas secreting adrenocorticotropic hormone (ACTH, Cushing’s disease) and growth hormone (acromegaly) with biochemical remission rates significantly correlated with tumor size and invasiveness [25]. Nonfunctioning microadenomas (<1 cm) are usually clinically silent, macroadenomas commonly present with mass effect causing visual and hormonal deficits, and cranial nerve malfunction caused by involvement of the cavernous sinus. Surgery is generally indicated for patients with visual compromise or tumor growth documented on serial imaging studies [25, 26].
With significant suprasellar extension, especially with tumors that extend above the planum sphenoidale, there is often benefit of removing the tuberculum sellae and a part of the planum sphenoidale. This allows an extracapsular dissection of the tumor to ensure a complete resection. Although some authors have recommended a combined transcranial-transsphenoidal approach to these tumors, the view is adequate with an endoscopic transtuberculum, transplanum approach to completely remove the tumor without a craniotomy [9]. EEA provides a view from the ventral midline corridor, and the pathology is encountered prior to critical nerves and vessels, minimizing the risk of damage to these structures during tumor resection. Likewise, removal of the tuberculum sella and part of the planum sphenoidale, as well as exposure of the ventral and medial cavernous sinus, allows the surgeon to reach around the capsule of the tumor and not just perform an internal decompression but a gross-total resection [27, 28].
EEA can be safe and effective for the resection of pituitary adenomas of any size or invasiveness without significant lateral extension beyond the carotid bifurcation. Endonasal approaches to these lesions have been shown to have a significantly higher rate of gross-total resection, better visual outcome, and less recurrences. CSF leak rates and meningitis were found to be lower for endoscopic approaches than for transcranial approaches [28]. The advantages of endonasal approaches are most profound in tumors with suprasellar extension and CS invasion [29].
Craniopharyngiomas
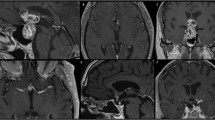
Craniopharyngiomas arise from the pituitary stalk and generally are located posterior to the chiasm extending into the third ventricle. They can cause hydrocephalus, visual loss, pituitary dysfunction, and diabetes insipidus (DI). The extended transplanum approach can provide an ideal corridor between the optic chiasm and the normal pituitary gland for their removal (Fig. 5.5). Although some authors have advocated subtotal resection followed by radiation due to high likelihood of causing deficits, gross-total resection offers a reasonably high likelihood of cure, particularly if performed transsphenoidally [20, 30, 31]. The transplanum, transtuberculum approach does place the stalk at high risk of injury due to the anatomical nature of the approach, with a potential of postoperative DI and hypopituitarism, but transcranial approaches equally place pituitary function at risk of injury, with rates of hypopituitarism reaching 70–80% [32, 33]. In addition, it is possible to minimize injury to the pituitary gland and stalk either by mobilizing or partially resecting the pituitary gland to enlarge the surgical corridor [9]. Another advantage of the endoscopic transplanum, transtuberculum approach is the unobstructed view of the entire third ventricle from below, which cannot be obtained with a transcranial/microscope-based approach, increasing the chances of gross-total resection with less morbidity with EEA [9] (Fig. 5.6). The risk of hyperphagia and hypothalamic injury with gross-total resection is largely dependent on the extent of tumor invasion, which is unchanged by the method of approach or visualization. Therefore, the risks of hyperphagia after gross-total resection are likely to be roughly equivalent after endoscopic transsphenoidal as after microscope-based transcranial approaches. If the goal of surgery is partial resection and cyst decompression, this can also be easily achieved with an endoscopic, transsphenoidal, transtuberculum approach [20].
A 45° endoscope provides a detailed view of the third ventricle below. Foramen of Monro (FM) visible bilaterally. Please note the ventriculostomy catheter visible in the lateral ventricle on the right through the FM, and it penetrates into the third ventricle close to midline. For patients with hydrocephalus, a ventriculostomy is preferred over lumbar drain
Meningiomas
Meningiomas of the planum sphenoidale and tuberculum sella and even some carefully selected small olfactory groove meningiomas are amenable to the endoscopic, endonasal transtuberculum, transplanum approach for resection. Tumors that extend lateral to the carotid may not be suitable to EES. Meningiomas of the planum sphenoidale and tuberculum sella are mostly prechiasmal, and the most common presentation is visual loss . Subfrontal and pterional transcranial approaches do not only require brain retraction but also place optic nerves and the carotid arteries between the tumor and the surgeon [34, 35]. On the contrary, the EEA permits the surgeon to be able to immediately internally debulk the tumor before encountering any of the critical neurovascular structures [9, 20]. Although gross-total resection is possible with this approach and is generally the goal, the transtuberculum, transplanum approach also makes possible a less morbid decompression of the optic apparatus in frail or elderly patients who are losing vision in preparation for post resection radiation or observation. Another advantage of approaching these tumors from below is the ability to interrupt the dural vascular supply to the tumor early in the operation. This option is particularly important if preoperative embolization is not possible. In addition, the transtuberculum , transplanum approach potentially offers a higher likelihood of curing these meningiomas. Not only the dura, but also the bone at the base of the tumor, is removed during the approach. These are precisely the areas that may be infiltrated by tumor that are most difficult to remove from a transcranial route. In addition, wide opening of the optic canals bilaterally can ensure removal of tumor remnants that lie below the optic nerve, which would be very difficult to remove with a transcranial approach [9] (Fig. 5.7).
Potential disadvantages of endonasal resection of meningiomas include a narrow working space and reduced degrees of freedom with the dissecting instruments. Additionally, the entire dural attachment and dural tail may not be completely exposed and removed. However, with increasing understanding of the adjacent anatomy from the endoscopic perspective and with angled instruments, appropriate access corridors can be established enabling bimanual, microscope-like dissection around the indwelling endoscope. Careful patient selection and knowledge of the limitations of the endonasal corridor can reduce the incidence of residual tumor. In addition, operating through the nose carries with it the theoretical risk of intracranial infection and CSF leak, given the challenge of reconstructing the dura and skull base from below. Somewhat surprisingly, however, the rate of postoperative infection with EEA is extremely low. Surgeon familiarity with endoscopic techniques greatly affects operative time, which can significantly impact patient outcomes [19, 36].
Rathke’s Cleft Cysts
Rathke’s cleft cysts (RCCs ) are benign congenital lesions believed to derive from remnants of Rathke’s pouch. Rathke’s cleft is the residual lumen between the anterior and intermediate lobe constitutes found after the formation of the pituitary gland. Further enlargement of Rathke’s cleft with proliferation of the cells lining it and accumulation of its secretions leads to RCCs [37].
These cysts can be encountered in 12–33% of normal pituitary glands in routine autopsies [38]. These cysts generally are sellar, although in one-third of cases, they can have a suprasellar component. Pure suprasellar lesions are rare at the time of diagnosis. They present with headaches, visual impairment, and endocrine dysfunction. On MRI, enhancement of the pituitary around the cyst wall may be observed leading to the classical aspect of “the egg in the cup” sign [39]. The treatment of Rathke’s cleft cysts mainly is surgical. A transsphenoidal approach, together with the drainage of the cyst accompanied by a biopsy of the cyst wall, usually is the preferred treatment to avoid any postoperative hypopituitarism or DI [38, 40].
Chordomas
Chordomas are rare (0.1% of skull base tumors) neoplasms originating from the notochord cells [37, 41]. Clinical presentation depends on the size and extension of the lesion, but the most common presenting symptoms are visual complaints, mainly diplopia. Intermittent or partial abducens nerve palsy is a common initial symptom of clival chordomas, related either to posterior cavernous sinus extension or invasion into Dorello’s canal. Chordomas tend to recur and metastasize, and their long-term prognosis is poor. Radical resection and aggressive adjuvant radiation therapy is the recommended treatment for these lesions [37, 41, 42]. EEA is becoming the gold standard to resect skull base chordomas [37, 42,43,44,45]. Isolated suprasellar chordomas are very rare; instead, they usually arise in the clivus and may have significant suprasellar extension which may require a transplanum approach to supplement the transclival approach to resect them [16].
5.6 Postoperative Care
Once the surgery is complete, extubation must be smooth to avoid dislodgment of the closure. During closure we routinely utilize CSF drainage to keep ICP low. CSF drainage via the lumbar drain is continued for 24 h for with a rate of 5 cc/hour. Patients are kept under surveillance for postoperative diabetes insipidus (DI). Patients may be administered a small dose of glucocorticoids postoperatively. If there is clearly damage to the pituitary-hypothalamic axis or known preoperative hypocortisolism, glucocorticoids are continued for the patient’s hospital stay and are tapered by the endocrinologist after discharge. Otherwise, a fasting morning cortisol level is obtained on the morning of the second postoperative day, and cortisol replacement is initiated only if the level is abnormally low. Infectious complications are rare, especially in the absence of a postoperative CSF leak. Antibiotics are delivered in the perioperative for 24–48 h. A postoperative MRI scan usually is obtained on the second postoperative day and then 3 months after surgery [9, 19].
5.7 Surgical Pearls
-
Early visual identification of the pituitary and stalk is important. Meticulous surgical dissection to preserve the pituitary stalk and supporting vasculature is important to prevent postoperative diabetes insipidus. Devascularization of the stalk can cause hypopituitarism and the superior hypophyseal arteries should be identified and preserved if possible. Branches to the chiasm should also be preserved if possible to avoid visual deterioration although collaterals from above exist.
-
For EEA, it is important not to make the bone opening too small. Once the surgeon is confident in their ability to close large skull base defects, larger bone openings are possible. Navigation is useful to determine the required size of the opening to expose the extent of the tumor. If the bone opening is too small, the surgeon is forced to pull the pathology into the field of view which risks injury to vessels attached to the back of the tumor.
-
For very large tumors and for extended approaches, the middle turbinate may be removed to provide additional visualization. Frequent internal decompression and extracapsular dissection permits the surgeon to avoid blindly pulling the tumor into the surgical field [16].
References
Patel CR, Fernandez-Miranda JC, Wang WH, Wang EW. Skull Base Anatomy. Otolaryngol Clin N Am. 2016;49(1):9–20.
McCrea HJ, George E, Settler A, Schwartz TH, Greenfield JP. Pediatric Suprasellar tumors. J Child Neurol. 2016 Oct;31(12):1367–76.
Patel SG, Singh B, Polluri A, Bridger PG, Cantu G, Cheesman AD, et al. Craniofacial surgery for malignant skull base tumors: report of an international collaborative study. Cancer. 2003;98(6):1179–87.
Origitano TC, Petruzzelli GJ, Leonetti JP, Vandevender D. Combined anterior and anterolateral approaches to the cranial base: complication analysis, avoidance, and management. Neurosurgery. 2006;58(4 Suppl 2):ONS-327–36; discussion ONS-36-7.
Schwartz TH, Fraser JF, Brown S, Tabaee A, Kacker A, Anand VK. Endoscopic cranial base surgery: classification of operative approaches. Neurosurgery. 2008;62(5):991–1002; discussion −5.
Silva D, Attia M, Kandasamy J, Alimi M, Anand VK, Schwartz TH. Endoscopic endonasal transsphenoidal “above and below” approach to the retroinfundibular area and interpeduncular cistern – cadaveric study and case illustrations. World Neurosurg. 2014;81(2):374–84.
Khan OH, Raithatha R, Anand VK, Schwartz TH. Endoscopic surgery of the Sella and Suprasellar region. In: Sataloff RT, editor. Sataloff’s comprehensive textbook of otolaryngology: head and neck surgery, vol. 2. New Delhi: Jaypee Brothers Medical Publishers; 2015. p. 805–21.
McCrea HJ, Yang T, Schwartz TH. Controversies: endoscopic resection. In: Evans JJ, Kenning TJ, editors. Craniopharyngiomas. Cambridge, MA: Academic Press; 2015.
Schwartz TH, Anand VK. The endoscopic endonasal transsphenoidal approach to the suprasellar cistern. Clin Neurosurg. 2007;54:226–35.
Harris AE, Lee JY, Omalu B, Flickinger JC, Kondziolka D, Lunsford LD. The effect of radiosurgery during management of aggressive meningiomas. Surg Neurol. 2003;60(4):298–305; discussion.
Kreil W, Luggin J, Fuchs I, Weigl V, Eustacchio S, Papaefthymiou G. Long term experience of gamma knife radiosurgery for benign skull base meningiomas. J Neurol Neurosurg Psychiatry. 2005;76(10):1425–30.
Paravati AJ, Heron DE, Gardner PA, Snyderman C, Ozhasoglu C, Quinn A, et al. Combined endoscopic endonasal surgery and fractionated stereotactic radiosurgery (fSRS) for complex cranial base tumors-early clinical outcomes. Technol Cancer Res Treat. 2010;9(5):489–98.
Pollock BE, Stafford SL, Utter A, Giannini C, Schreiner SA. Stereotactic radiosurgery provides equivalent tumor control to Simpson grade 1 resection for patients with small- to medium-size meningiomas. Int J Radiat Oncol Biol Phys. 2003;55(4):1000–5.
Milker-Zabel S, Zabel-du Bois A, Huber P, Schlegel W, Debus J. Fractionated stereotactic radiation therapy in the management of benign cavernous sinus meningiomas: long-term experience and review of the literature. Strahlenther Onkol. 2006;182(11):635–40.
Jho HD, Ha HG. Endoscopic endonasal skull base surgery: part 1 – the midline anterior fossa skull base. Minim Invasive Neurosurg. 2004;47(1):1–8.
Schwartz TH, Anand VJ. Endonasal transplanum approach to the anterior cranial fossa. In: Snyderman C, Gardner P, editors. Master techniques in otolaryngology-head and neck surgery. Philadelphia: Lippincott Williams & Wilkins; 2014.
Placantonakis DG, Tabaee A, Anand VK, Hiltzik D, Schwartz TH. Safety of low-dose intrathecal fluorescein in endoscopic cranial base surgery. Neurosurgery 2007;61(3 Suppl):161–5; discussion 5–6.
Banu MA, Kim JH, Shin BJ, Woodworth GF, Anand VK, Schwartz TH. Low-dose intrathecal fluorescein and etiology-based graft choice in endoscopic endonasal closure of CSF leaks. Clin Neurol Neurosurg. 2014;116:28–34.
Woodworth G, McCoul E, Anand V, Greenfiled J, Schwartz T. Endoscopic management of anterior cranial fossa meningiomas. Oper Tech Otolaryngol Head Neck Surg. 2011;22(4):Issue 4.
Laufer I, Anand VK, Schwartz TH. Endoscopic, endonasal extended transsphenoidal, transplanum transtuberculum approach for resection of suprasellar lesions. J Neurosurg. 2007;106(3):400–6.
Leng LZ, Brown S, Anand VK, Schwartz TH. “Gasket-seal” watertight closure in minimal-access endoscopic cranial base surgery. Neurosurgery. 2008;62(5 Suppl 2):ONSE342–3; discussion ONSE3.
Patel KS, Komotar RJ, Szentirmai O, Moussazadeh N, Raper DM, Starke RM, et al. Case-specific protocol to reduce cerebrospinal fluid leakage after endonasal endoscopic surgery. J Neurosurg. 2013;119(3):661–8.
Kovacs K, Horvath E. Pathology of pituitary tumors. Endocrinol Metab Clin N Am. 1987;16(3):529–51.
Hofstetter CP, Mannaa RH, Mubita L, Anand VK, Kennedy JW, Dehdashti AR, et al. Endoscopic endonasal transsphenoidal surgery for growth hormone-secreting pituitary adenomas. Neurosurg Focus. 2010;29(4):E6.
Messerer M, De Battista JC, Raverot G, Kassis S, Dubourg J, Lapras V, et al. Evidence of improved surgical outcome following endoscopy for nonfunctioning pituitary adenoma removal. Neurosurg Focus. 2011;30(4):E11.
Farrell CJ, Nyquist GG, Farag AA, Rosen MR, Evans JJ. Principles of pituitary surgery. Otolaryngol Clin N Am. 2016;49(1):95–106.
Kouri JG, Chen MY, Watson JC, Oldfield EH. Resection of suprasellar tumors by using a modified transsphenoidal approach. Report of four cases. J Neurosurg. 2000;92(6):1028–35.
Komotar RJ, Starke RM, Raper DM, Anand VK, Schwartz TH. Endoscopic endonasal compared with microscopic transsphenoidal and open transcranial resection of giant pituitary adenomas. Pituitary. 2012;15(2):150–9.
Hofstetter CP, Shin BJ, Mubita L, Huang C, Anand VK, Boockvar JA, et al. Endoscopic endonasal transsphenoidal surgery for functional pituitary adenomas. Neurosurg Focus. 2011;30(4):E10.
Fahlbusch R, Honegger J, Paulus W, Huk W, Buchfelder M. Surgical treatment of craniopharyngiomas: experience with 168 patients. J Neurosurg. 1999;90(2):237–50.
Yaşargil MG, Curcic M, Kis M, Siegenthaler G, Teddy PJ, Roth P. Total removal of craniopharyngiomas. Approaches and long-term results in 144 patients. J Neurosurg. 1990;73(1):3–11.
Honegger J, Buchfelder M, Fahlbusch R. Surgical treatment of craniopharyngiomas: endocrinological results. J Neurosurg. 1999;90(2):251–7.
Chakrabarti I, Amar AP, Couldwell W, Weiss MH. Long-term neurological, visual, and endocrine outcomes following transnasal resection of craniopharyngioma. J Neurosurg. 2005;102(4):650–7.
Benjamin V, Russell SM. The microsurgical nuances of resecting tuberculum sellae meningiomas. Neurosurgery. 2005;56(2 Suppl):411–7; discussion −7.
Buslei R, Nolde M, Hofmann B, Meissner S, Eyupoglu IY, Siebzehnrubl F, et al. Common mutations of beta-catenin in adamantinomatous craniopharyngiomas but not in other tumours originating from the sellar region. Acta Neuropathol. 2005;109(6):589–97.
Schaberg MR, Anand VK, Schwartz TH, Cobb W. Microscopic versus endoscopic transnasal pituitary surgery. Curr Opin Otolaryngol Head Neck Surg. 2010;18(1):8–14.
Bresson D, Herman P, Polivka M, Froelich S. Sellar lesions/pathology. Otolaryngol Clin N Am. 2016;49(1):63–93.
Frank G, Sciarretta V, Mazzatenta D, Farneti G, Modugno GC, Pasquini E. Transsphenoidal endoscopic approach in the treatment of Rathke’s cleft cyst. Neurosurgery. 2005;56(1):124–8; discussion 9.
Zada G, Lin N, Ojerholm E, Ramkissoon S, Laws ER. Craniopharyngioma and other cystic epithelial lesions of the sellar region: a review of clinical, imaging, and histopathological relationships. Neurosurg Focus. 2010;28(4):E4.
Aho CJ, Liu C, Zelman V, Couldwell WT, Weiss MH. Surgical outcomes in 118 patients with Rathke cleft cysts. J Neurosurg. 2005;102(2):189–93.
Tzortzidis F, Elahi F, Wright D, Natarajan SK, Sekhar LN. Patient outcome at long-term follow-up after aggressive microsurgical resection of cranial base chordomas. Neurosurgery. 2006;59(2):230–7; discussion −7.
Chibbaro S, Cornelius JF, Froelich S, Tigan L, Kehrli P, Debry C, et al. Endoscopic endonasal approach in the management of skull base chordomas – clinical experience on a large series, technique, outcome, and pitfalls. Neurosurg Rev. 2014;37(2):217–24; discussion 24–5.
Koutourousiou M, Gardner PA, Tormenti MJ, Henry SL, Stefko ST, Kassam AB, et al. Endoscopic endonasal approach for resection of cranial base chordomas: outcomes and learning curve. Neurosurgery. 2012;71(3):614–24; discussion 24–5.
DMS R, Komotar RJ, Starke RM, Anand VK, Schwartz TH. Endoscopic versus open approaches to the skull base: a comprehensive literature review. Oper Tech Otolaryngol Head Neck Surg. 2011;22(4):302–7.
Komotar RJ, Starke RM, Raper DM, Anand VK, Schwartz TH. The endoscope-assisted ventral approach compared with open microscope-assisted surgery for clival chordomas. World Neurosurg. 2011;76(3–4):318–27; discussion 259–62.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Omay, S.B., Anand, V.K., Schwartz, T.H. (2019). 5 Suprasellar Pathology. In: Evans, J., Kenning, T., Farrell, C., Kshettry, V. (eds) Endoscopic and Keyhole Cranial Base Surgery . Springer, Cham. https://doi.org/10.1007/978-3-319-64379-3_5
Download citation
DOI: https://doi.org/10.1007/978-3-319-64379-3_5
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-64378-6
Online ISBN: 978-3-319-64379-3
eBook Packages: MedicineMedicine (R0)