Abstract
The certified geriatric pharmacist is a valuable resource to practitioners in the field. The pharmacist has a keen view of the patient as a whole (not just from the medication silo) and can be a vital partner in selection of medications, alternative therapies, and titration of doses in renal and hepatic impairment. This chapter will review the role of the consultant on the interdisciplinary team in geriatrics as well as changes with the aging process that affect medication use and lastly adverse effects, polypharmacy, and medication monitoring that the pharmacist can assist primary care physicians.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Consultant pharmacist
- Adverse effects
- Interdisciplinary team
- Medication monitoring
- Regulatory compliance
- Education
With the exponential growth expected over the next decade in the geriatric population, healthcare professionals will be challenged to match the demands to adequately treat this cohort [1,2,3]. Much of the care will default to primary care providers who will benefit from the resources of an interdisciplinary team to assist with assessments and treatment options [4]. The certified geriatric pharmacist is one such interdisciplinary team resource [5].
The certified geriatric pharmacist can help to manage many chronic disease states and assist with assessment and monitoring of the medication regimen in collaboration with the primary care provider [3, 5]. Trained geriatric pharmacists look at the patient as a “whole” and are not in a silo of one disease arena [6, 7]. Considering alternative therapy choices, titration of medications and adjustments of dose due to renal impairment are key roles the pharmacist can play [7, 8]. Drug information is another resource the certified geriatric pharmacist can provide with sufficient evidence-based medicine references that can assist in pharmacotherapy decision-making [9, 10].
A certified geriatric pharmacist has at least 2 years of practice with geriatric patients or a general pharmacy residency for 1 year and 1 year of practice [11]. In addition, the certified geriatric pharmacist has taken a written exam and passed [11]. The certification is good for 5 years and needs to be maintained with specific continuing education requirements set by the Commission for Certification in Geriatric Pharmacy (CCGP) [12]. Unlike other board certification programs, the CCGP is an internationally accepted certification [13]. Through the training process to become a certified geriatric pharmacist, the development in the expertise of the physiologic, pharmacokinetic, polypharmacy, and misuse, abuse, and compliance aberrations that occur with the aging process is achieved [14].
Many changes in the aging process can affect the use of medications [15]. For example, as people age the gastrointestinal tract, particularly the stomach, becomes more basic from the traditional acidic environment of a pH less than 5 [15, 16]. This change in acidity can affect how a tablet might be dissolved in the stomach or a drug is absorbed [16]. Another example is wrinkling of the skin [17]. With wrinkles the skin is less smooth, is less hydrated, and has decreased surface lipids [17]. The use of a transdermal patch may be affected by the impact wrinkles have on the absorption of the drug getting through the skin as well as the patch adherence to the skin [15, 18]. There is also an increased potential for skin tears and skin complications [15]. A transdermal patch may be valuable to decrease systemic adverse effects; however, they may have an increased cost and potential risks of their own [15, 18].
Socioeconomic value of medication therapy may also play a role in compliance with the medication regimen [19]. At times new medications or those medications that do not have generics available can have high costs associated with their use [20]. Financial burden can contribute to nonadherence if the geriatric patient cannot afford the medication [20]. This can also be affected by third-party payor’s refusal to share cost or when the shared cost is too much for the patient on a fixed monthly income [20]. On the other hand, some patients will struggle to pay the high costs and then take the medication every other day to make the medication last longer [19, 20]. Either scenario presents compliance issues [20]. The certified geriatric pharmacist can sometimes help the patient change to a different Medicare Part D plan (prescription coverage program) that better covers the costs of their individual medications or even look for pharmaceutical company financial assistance programs and lastly, the pharmacist can recommend an alternative medication that is covered by the insurance plan [21].
When a pharmacist reviews the medication regimen with the patient, there are situations where misuse and abuse can be detected [22]. Misuse may include, for example, overuse of an inhaler for chronic obstructive pulmonary disease or that the inhaler is not being orally inhaled but the patient is spraying on their chest or inhaling through their nose [23, 24]. This type of misuse can come from low health literacy or poor patient education [25]. Another area of misuse can be seen with pain medications, specifically opioids with abuse potential [26]. Even with elderly patients, abuse with the opioids is common [27]. The patient develops dependence on the opioid to get up every day [27]. This is a helpful “need” however, what can transpire is the transition to demands for pain medication and addiction from this dependent situation [27]. This can be followed by complications of the narcotic analgesic agents such as confusion, delirium, and the increased risk of fractures due to a mechanical fall [28].
There can be value in having collaborative agreements with certified geriatric pharmacists [29]. Pharmacists can assist with the assessment and monitoring of medication regimens, especially in regard to pain management, diabetes, and cardiovascular conditions [29]. The remainder of this chapter focuses on the services and value of having a consultant pharmacist embedded in your interdisciplinary team.
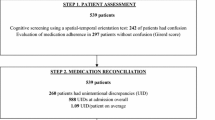
The consultant pharmacist can also be of great value with transitions of care and medication reconciliation [5, 30]. When a patient goes to the acute care hospital, the medication regimen will likely change [30]. As an example, consider an 87-year-old female having an aortic valve replacement who is sent home with at least five new medications. The discharge medication list may have some of the previous medications she was taking at home missing [30]. The pharmacist can review the home medications and the discharge medications and devise a medication regimen that covers all her medications [31]. Additionally the pharmacist can define a monitoring plan for the medication regimen including monitoring of the new warfarin added at the hospital [31]. With a specific protocol approved by the physician providers, the pharmacist can be delegated for the anticoagulation therapy lab monitoring and dose adjustments for the warfarin [32]. The need to review all medications, determine duplications, unnecessary agents on the return to home, and the need to simplify the medication regimen are all responsibilities that can be designated to the pharmacist for patients experiencing a transition of care [5, 30, 32].
As our 87-year-old patient transitions back to home and starts to make her follow-up visits to her many specialists such as the cardiologist, nephrologist, neurologist, and psychiatrist. there is a greater risk of polypharmacy as the number of specialists increases [33]. Continued visits with the geriatric pharmacist can benefit the patient. The pharmacist can communicate with the variety of specialists, simplify the medication regimen, as well as monitor for adverse effects of the medication regimen [31]. While medications may be started in the acute hospital, if the hospitalist started at a low dose, the medication may need to be titrated upward [30,31,32]. As a medication is titrated, always consider “start low, go slow, but go” to reach the individual therapeutic range [34].
The geriatric pharmacist is a vital resource in the therapeutic monitoring of medications [29]. The pharmacist can calculate the creatinine clearance (or GFR) and adjust the dose for renal impairment [29, 35, 36]. For example, our 87-year-old patient has been on memantine 10 mg twice daily for the past 6 months; however, during this last hospitalization, her kidneys take a turn for the worse. The pharmacist calculated her creatinine clearance to be 25 ml/min. The recommended dose for memantine when the renal function has declined to less than 30 ml/min is 5 mg twice a day [37]. This is a service the pharmacist can add to decrease accumulation of renally cleared medications and decrease the risk of adverse events [29, 35].
Psychoactive medications are another area that certified geriatric pharmacists can be delegated for monitoring [36]. For antipsychotic medications, the pharmacist can complete an Abnormal Involuntary Movement Scale (AIMS) and report the finding and recommendations for dose reductions [36, 38]. Additionally, the pharmacist can perform the Mini-Mental Status Exam or the Mini-Cog and the geriatric depression scale to assess cognition and depression [36, 38, 39]. The finding of these assessments can be reported to the provider with recommendations for changes in medication regimen as indicated [29]. Another service the pharmacist can provide is behavioral mapping [40, 41]. With a report form completed by the caregivers over 3 days, at 15-min intervals for the frequency of maladaptive behaviors, the pharmacist can plot the behaviors and assist the interdisciplinary team visualize at what times the behaviors are occurring and if the medication dosing is appropriate and if the behaviors are improving [40, 41]. This can identify that behaviors occur when the patient is hungry or having anxiety when a family member is scheduled to visit [40, 41]. When you can visually see the plot of the frequency of behaviors, it is much easier to consider non-pharmacologic interventions such as giving a snack if the patient is hungry or keeping the patient busy until the family member arrives [41]. Psychoactive medications can also contribute to countless therapy and disease state complications [42, 43]. Minimizing the use of psychoactive is fundamental to decreasing the risks and benefit ratio [44]. Especially in dementia, psychoactive medications can be useful and harmful at the same time [45]. We know that the antipsychotic agents are not FDA approved for use in dementia, yet they are used for hallucinations and psychosis that may cause a danger to the patient with self-injurious behaviors or a danger to others such as staff when working closely with the patient and they are kicking, hitting, and spitting [46]. While non-pharmacologic interventions are always first line and are preferred by all involved parties including the patient, there are times that the patient can benefit from the use of psychoactive medication in relation to improved quality of life, caregiver burden, and safety issues [45].
Another area where the geriatric pharmacist can be advantageous is in the development of an antibiotic stewardship program and the empiric selection, renal dose adjustment, and frequency and duration of therapy for antibiotics [47, 48]. With the antibiotic development pipeline declining, the need to reduce resistance to current available antibiotics is increasing [47, 48]. Geriatric patients living within a facility may harbor multidrug-resistant organisms that can be transmitted to other patients [47]. Consider that our 87-year-old was admitted to the hospital for a community-acquired Streptococcus pneumoniae but her nasal swab tested positive for Klebsiella pneumoniae ESBL. This changed the regimen in the hospital from simply a macrolide to ertapenem [49]. Whether living in a facility or in the community, our frail geriatric patients are at risk for multidrug-resistant organisms [50]. We need to save antibiotics for when there are sufficient signs and symptoms of an infection before starting an antibiotic [49, 50]. If an antibiotic is not started, the provider might consider having the patient return to the office in 24–72 hours to ensure no new signs of infection have developed [49, 50]. Empiric therapy is key to appropriate antibiotic use and should be based on the antibiogram for the cohort of patients seen in your practice [49, 51]. The laboratory can provide the antibiogram, and the pharmacist can help design a plan for your antibiotic stewardship program [51]. Pharmacists have ample knowledge to be helpful with selection of the appropriate spectrum and best antibiotic regimen to reduce the risk of resistance [51]. In the community setting, there is a great need to reduce unnecessary antibiotic use to diminish microorganism resistance, and the pharmacist can be a key to your practice [52].
Another area that the geriatric pharmacist can be of value is in looking for drug-drug interactions [29]. For example, our patient was taking sertraline 50 mg daily and was started on tramadol 50 mg every 6 h as needed for pain in the hospital. She was very anxious on return from the hospital, and the pharmacist noted the possibility of mild serotoninergic syndrome [53]. The pharmacist recommended changing the tramadol back to acetaminophen since the patient had not taken any tramadol since discharge from the hospital.
Adverse drug events can contribute to a geriatric patient being readmitted to the hospital [54]. The difference between an adverse drug event and a side effect is that a side effect is anticipated and mild in nature, such as diphenhydramine causing drowsiness [55]. An adverse drug event can be detrimental to the patient’s health [55], for example, blood in the urine with enoxaparin when bridging to warfarin. Our patient was also taking sertraline and the selective serotonin reuptake inhibitors (SSRI) as a class effect can decrease platelet aggregation and contribute to an increased risk of bleeding [56]. This can contribute to a longer hospital stay or a readmission. The pharmacist can play an important role in handling adverse events [57].
Adverse events can range from serotonin syndrome to QTc interval prolongation to medication-induced mechanical fall risk [57]. The certified geriatric pharmacist can remind the prescriber to consider an electrocardiogram to monitor for QTc interval prolongation to decrease the risk of a ventricular arrhythmia and a poor patient outcome [58].
In the setting of a mechanical fall, there are many factors that may contribute to the fall, and medications are one of them [59]. There are several medication fall risk predictors [59]. One of the easiest to use is the ASHP fall risk scoring system (Table 13.1). It looks at the classes of medication and quantifies the risk [60].
Another area that can be assessed by the pharmacist is anticholinergic burden, especially if signs and symptoms of anticholinergic adverse effects are noted such as dry mouth, dry eyes, urinary retention, constipation, or low blood pressure [61]. There are numerous medications such as furosemide and warfarin that have a low anticholinergic burden but when combined with multiple agents can contribute to adverse effects [62].
Dehydration and electrolyte imbalance are also common adverse events for the geriatric patient [63]. Many geriatric patients do not drink enough water [63]. Additionally, several medications can contribute to hyponatremia as an adverse effect, for example, the SSRIs, carbamazepine, and oxcarbazepine [63]. These adverse drug effects can be a factor in seizure risk and other negative patient outcomes [64]. Discussion of risk factors can help to avoid severe adverse events [63, 64].
Interdisciplinary team meetings can be a simple and effective use of time to get the more information about each patient [29]. The geriatric pharmacist can provide drug information and monitoring and suggest changes in the regimen with a verbal discussion of alternative therapy [29]. When the team members are present and interactive, the best pathway to positive outcomes for the patient can be devised [65]. Most interdisciplinary team meetings can take a few hours a week if done efficiently [66]. New patients can take more discussion to devise the care plan and should be dispersed over different meeting schedules to be efficient. Caregiver, patient, and family should be included when possible [67]. When a patient resides in a facility, the caregiver closest to the patient and the patient should at least attend virtually via teleconference or webinar [67].
While a patient is living within a facility, for example, an assisted living facility (ALF) compared to a skilled nursing facility (SNF) , a prescriber should keep in mind the federal and state regulations that apply to medication use within these types of facilities [68]. For example, our patient has been taking sertraline for years and was recently placed in a SNF for rehabilitation after a bout of pneumonia. The facility staff completed the assessment for depression, and currently this patient is not displaying any signs or symptoms of depression. The consultant pharmacist cites the federal regulations that suggest that as the prescriber you should reassess the need for the sertraline and consider a slow downward taper [68]. The prescriber knows that the patient has a long history of depression and decides to keep the dose at the current 50 mg daily regimen. The consultant pharmacist’s role in this scenario is to inform the prescriber of the guidelines and to obtain the documentation to support the fact that a dose reduction is clinically contraindicated [68].
Our patient is now being discharged home from the SNF, and the pharmacist is assessing her health literacy and understanding of her medication [29, 69]. Since she is now taking warfarin, the pharmacist asks if she can receive the medication education [69]. The pharmacist meets with the patient and reviews the diet, time to take the medication, and when to notify the prescriber if any symptoms of bruising or bleeding occur [69]. Pharmacists have value as medication education specialists and are often best suited to prepare and deliver this information [69]. Medical staff journal club organization or staff in-services about new uses of medications are additional valuable resources of the pharmacist [70].
References
Yax, Population Division Laura K. Sixty-five plus in the United States. Sixty Five Plus in the United States. 03 Feb. 2017.
Lee W-C, Sumaya CV. Geriatric workforce capacity: a pending crisis for nursing home residents. Front Public Health. 2013;1:24.
Gray SL, Elliott D, Semla T. Implications for pharmacy from the Institute of Medicine’s report on health care workforce and an aging America. Ann Pharmacother. 2009;43(6):1133–8.
Adams WL, Mcilvain HE, Lacy NL, Magsi H, Crabtree BF, Yenny SK, et al. Primary care for elderly people: why do doctors find it so hard? Gerontologist. 2002;42(6):835–42.
Keough ME, Field TS, Gurwitz JH. A model of community-based interdisciplinary team training in the care of the frail elderly. Acad Med. 2002;77(9):936.
Kasbekar R, Maples M, Bernacchi A, Duong L, Oramasionwu CU. The pharmacist’s role in preventing medication errors in older adults. Consult Pharm. 2014;29(12):838–42.
Johnson A, Guirguis E, Grace Y. Preventing medication errors in transitions of care: a patient case approach. J Am Pharm Assoc. 2017;55(2):e264–74.
Berthe A, Fronteau C, Le Fur E, Morin C, Huon JF. Medication reconciliation: a tool to prevent adverse drug events in geriatrics medicine. Geriatr Psychol Neuropsychiatr Vieil. 2017;15(1):19–24.
Burkiewicz JS, Zgarrick DP. Evidence-based practice by pharmacists: utilization and barriers. Ann Pharmacother. 2005;39(7–8):1214–9.
Knoer S, Eck AR, Lucas A. A review of American pharmacy: education, training, technology, and practice. J Pharm Health Care Sci. 2016;9(2)
About the Certified Geriatric Pharmacist Examination | CCGP. N.p., n.d. 03 Feb. 2017.
About the Certified Geriatric Pharmacist Examination | CCGP. N.p., n.d. 03 Feb. 2017.
What Is a Certified Group Psychotherapist (CGP)? CGP Certification. N.p., n.d. 03 Feb. 2017.
ASCP Updates Introductory Modules on Geriatric Pharmacy Review | CCGP. N.p., n.d. 03 Feb. 2017.
Nkansah N. Boot Camp Biology of Aging. Biology of Aging. San Francisco: UCSF, n.d.
Feldman M, Cryer B, Mcarthur KE, Huet BA, Lee E. Effects of aging and gastritis on gastric acid and pepsin secretion in humans: a prospective study. Gastroenterology. 1996;110(4):1043–52.
Why does skin wrinkle with age? What is the best way to slow or prevent this process? Scientific American. N.p., 23 Sept. 2005. 03 Feb. 2017.
Konda S, Meier-Davis S, Shudo B, Maibach J. Age-related percutaneous penetration part 2: effect of age on Dermatopharmacokinetics and overview of transdermal products. Skin Therapy Lett. 2012;17(6):5–7.
Alsabbagh MH, Wasem E, Lemstra M, Eurich D, Lix LM, Wilson TW, et al. Socioeconomic status and nonadherence to antihypertensive drugs: a systematic review and meta-analysis. Value Health. 2014;17(2):288–96.
Chan M. Reducing cost-related medication nonadherence in patients with diabetes. Physicians Practice. N.p., n.d. 03 Feb. 2017.
Bonner L. Annual medicare part D enrollment is here. American Pharmacists Association. N.p., 17 Oct. 2014. 03 Feb. 2017.
Silva C, Ramalho C, Luz I, Monteiro J, Fresco P. Drug-related problems in institutionalized, polymedicated elderly patients: opportunities for pharmacist intervention. Int J Clin Pharm. 2015;37(2):327–34.
Fan VS, Gylys-Colwell I, Locke E, Sumino K, Nguyen HQ, Thomas RM, et al. Overuse of short-acting beta-agonist bronchodilators in COPD during periods of clinical stability. Respir Med. 2016;116:100–6.
Takaku Y, Kurashima K, Ohta C, Ishiguro T, Kagiyama N, Yanagisawa T, et al. How many instructions are required to correct inhalation errors in patients with asthma and chronic obstructive pulmonary disease? Respir Med. 2017;123:110–5.
Rau JL. Practical problems with aerosol therapy in COPD. Respir Care. 2006;51(2):158–72.
Salinas GD, Susalka D, Burton S, Roepke N, Evanyo K, Biondi D, et al. Risk assessment and counseling behaviors of healthcare professionals managing patients with chronic pain: a National multifaceted assessment of physicians, pharmacists, and their patients. J Opioid Manag. 2012;8(5):273–84.
Chang Y-P, Compton P. Opioid misuse/abuse and quality persistent pain management in older adults. J Gerontol Nurs. 2016;42(12):21–30.
Krebs EE, Paudel M, Taylor BC, Bauer DC, Fink HA, Lane NE, et al. Association of opioids with falls, fractures, and physical performance among older men with persistent musculoskeletal pain. J Gen Intern Med. 2016;31(5):463–9.
Mcbane SE, Dopp AL, Abe A, Benavides S, Chester EA, Dixon DL, et al. Collaborative drug therapy management and comprehensive medication Management – 2015. Pharmacotherapy. 2015;35(4):e39–50.
Yvette C, Kripalani S. Medication use in the transition from hospital to home. Ann Acad Med Singap. 2008;37(2):136.
Carter MA, Amadio AL, Bruchet N. Should hospital pharmacists provide postdischarge follow-up care to high-risk patients? Can J Hosp Pharm. 2015;68(3):265–6.
Wilt V, Gums J, Ahmed O, Moore L. Outcome analysis of a pharmacist-managed anticoagulation service. Pharmacotherapy ACCP. 1995;15(6):732–9.
Veehof L, Schuling J. Polypharmacy in the elderly with chronic diseases: conflicting interests. Ned Tijdschr Geneeskd. 1997;141(4):177–9.
Pehlivan, Ozgur CoruhluSuleyman. “Worst Pills.” Worst Pills. N.p., n.d. 03 Feb. 2017.
Hanlon JT, Lindblad CI, Gray SL. Can clinical pharmacy services have a positive impact on drug-related problems and health outcomes in community-based older adults? Am J Geriatr Pharmacother. 2004;2(1):3–13.
Page AT, Potter K, Clifford R, Mclachlan AJ, Etherton-Beer C. Medication appropriateness tool for co-morbid health conditions in dementia: consensus recommendations from a multidisciplinary expert panel. Intern Med J. 2016;46(10):1189–97.
Pumerantz Library Proxy Login. N.p., n.d. 03 Feb. 2017.
Rubio-Valera M, Chen T, O’reilly C. New roles for pharmacists in community mental health care: a narrative review. Int J Environ Res Public Health. 2014;11(10):10967–90.
Reinhold J, Earl G. Clinical therapeutics primer: link to the evidence for the ambulatory care pharmacist, first edition. Burlington: Jones & Bartlett Learning; 2017.
Wolf-Klein GP, Levy AP, Silverstone FA, Smith H, Papain P, Foley CJ. Psychiatric profile of the noncompliant geriatric patient in the community. Int Psychogeriatr. 1989;1(2):177–84.
Borson S. Geriatric psychiatry, an issue of clinics in geriatric medicine – 9780323320122 | US Elsevier Health Bookshop. N.p., 25 July 2014. 03 Feb. 2017.
American Geriatrics Society 2015 Beers Criteria Update Expert Panel. American geriatrics society 2015 updated beers criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2015;63(11):2227–46.
Lin EH, Katon W, Von Korff M, Rutter C, Simon GE, Oliver M, et al. Relationship of depression and diabetes self-care, medication adherence, and preventive care. Diabetes Care. 2004;27(9):2154–60.
Gable R. 5.2 Altering consciousness with psychoactive drugs. Introduction to psychology. N.p.: Creative Commons, 2010. pp. 686–96.
Lindsey PL. Psychotropic medication use among older adults. J Gerontol Nurs. 2009;35(9):28–38.
Information for healthcare professionals: conventional antipsychotics. FDA information for healthcare professionals: conventional antipsychotics. N.p., n.d. 03 Feb. 2017.
Rhee SM, Stone ND. Antimicrobial stewardship in long-term care facilities. Infect Dis Clin N Am. 2014;28(2):237–46.
Dellit TH. Summary of the infectious diseases society of America and the society for healthcare epidemiology of America guidelines for developing an institutional program to enhance antimicrobial stewardship. Infect Dis Clin Pract. 2007;15(4):263–4.
IDSA Guidelines 2016: HAP, VAP & It’s the End of HCAP as We Know It (And I Feel Fine). PulmCCM. PulmCCM, 31 July 2016. 03 Feb. 2017.
Bonomo RA. Multiple antibiotic resistant bacteria in long term care facilities: an emerging problem in the practice of infectious diseases. Clin Infect Dis. 2000;31(6):1414–22.
Joshi S. Hospital antibiogram: a necessity. Indian J Med Microbiol. 2010;28(4):277–80.
Lee VC. The antibiotic resistance crisis part 1: causes and threats. Pharm Ther. 2015;40(4):277–83.
Mayo Clinic Staff Print. “Serotonin Syndrome.” Overview – Serotonin Syndrome – Mayo Clinic. N.p., 20 Jan. 2017. 03 Feb. 2017.
Dormann H, Neubert A, Criegee-Rieck M, Egger T, Radespiel-Troger M, Azaz-Livshits T, et al. Readmissions and adverse drug reactions in internal medicine: the economic impact. J Intern Med. 2004;255(6):653–63.
What is the difference between adverse drug reaction and side effect?? N.p., n.d. 03 Feb. 2017.
Mccloskey DJ, Postolache TT, Vittone BJ, Nghiem KL, Monsale JL, Wesley RA, et al. Selective serotonin reuptake inhibitors: measurement of effect on platelet function. Transl Res. 2008;151(3):168–72.
ASHP guidelines on adverse drug reaction monitoring and reporting. Medication Misadventures – Guidelines. N.p., n.d.
Mabasa VH, Yokoyama S, Man D, Martyn J. Analysis of orders for QTc-prolonging medication for intensive and cardiac care unit patients with pre-existing QTc prolongation (QTIPPP study). Can J Hosp Pharm. 2011;64(6):412–8.
Woolcott JC. Meta-analysis of the impact of 9 medication classes on falls in elderly persons. Arch Intern Med. 2009;169(21):1952.
Tool 3I: medication fall risk score and evaluation tools. Agency for Healthcare Research & Quality. U.S. HHS: Agency for Healthcare Research and Quality, 31 Jan. 2013. 03 Feb. 2017.
Hilmer SN. A drug burden index to define the functional burden of medications in older people. Arch Intern Med. 2007;167(8):781.
Drugs with possible anticholinergic effect. Anticholinergic cognitive burden scale drugs with possible anticholinergic effects (n.d.): http://www.agingbraincare.org/uploads/products/ACB_anticholingergic_possibles_Handout_040412.pdf.
Schlanger LE, Bailey JL, Sands JM. Electrolytes in the aging. Adv Chronic Kidney Dis. 2010;17(4):308–19.
Alomar MJ. Factors affecting the development of adverse drug reactions (review article). Saudi Pharm J. 2014;22(2):83–94.
Nancarrow SA, Booth A, Ariss S, Smith T, Enderby P, Roots A. Ten principles of good interdisciplinary team work. Hum Resour Health. 2013;11(1):19.
Kinship care wrap around services: eligibility and documentation requirements. PsycEXTRA Dataset (n.d.): n. pag. Center for Medicare and Medicaid Services.
Oliver Park D, Porock D, Demiris G, Courtney K. Patient and family involvement in hospice interdisciplinary teams. J Palliat Care. 2005;21(4):270–6.
CMS review of current standards of practice for long-term care pharmacy services long-term care pharmacy primer. Centers for Medicare and Medicaid Services (n.d.): n. pag.
Kaboli PJ, Hoth AB, Mcclimon BJ, Schnipper JL. Clinical pharmacists and inpatient medical care. Arch Intern Med. 2006;166(9):955.
Lamy PP, Westfall LK, Speedie SM. The effect of inservice education provided by consultant pharmacists on the behavior of nurses in long-term care facilities. Ann Pharmacother. 1981;15(10):777–81.
Acknowledgments
Elizabeth Akhparyan for her assistance with the references.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG
About this chapter
Cite this chapter
Hoffman, J. (2018). Collaboration with a Geriatric Pharmacist. In: Wasserman, M., Riopelle, J. (eds) Primary Care for Older Adults. Springer, Cham. https://doi.org/10.1007/978-3-319-61329-1_13
Download citation
DOI: https://doi.org/10.1007/978-3-319-61329-1_13
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-61327-7
Online ISBN: 978-3-319-61329-1
eBook Packages: MedicineMedicine (R0)