Abstract
The development of novel and consistent biologic surrogates for drug discovery, toxicology, and cancer research is presently intense and involves a growing number of research groups and institutions around the world. The Twilight of the days of immortalized cell lines as the workhorse of most of our drug development and cancer research efforts seem now to be heading to their end with the introduction of body-on-a-chip platforms, bioengineered tissues and stem cell organoids. In this chapter, we describe the fundamental work and the different strategies that lead to some of the breakthroughs in the generation of hepatic tissue ex vivo. Lastly, we define its increasing use and applications by pharmaceutical industry and research laboratories.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
The necessity of reliable biologic surrogates for drug discovery, toxicology, including more basic biology disciplines – like cell biology, biochemistry, cancer, etc. – has been a constant source of research and concern [1]. From the early days of the first immortalized cell culture lines (including the world famous HeLa cells [2]) to body-on-a-chip platforms there are roughly 60 years of intense research and development (R&D) work.
In the particular case of the liver, it is one of the most important organs in metabolism and homeostasis, since it plays a critical role in these physiologic functions. It is responsible for the production of many proteins, vitamins, lipids, carbohydrates, carries on the detoxification of several metabolites and synthesizes substances necessary for homeostasis and digestion. Hence, since early on, the culture of primary hepatocytes became a priority, to capture liver’s vital role in xenobiotic metabolism and human physiology in a petri dish. In this line of work, hepatocyte isolation started in the mid-1960s, when Howard et al. isolated rat hepatocytes developing a combined mechanical/enzymatic digestion technique, later improved by Berry and Friend [3, 4]. This method was additionally enhanced by Seglen to become the two-step collagenase perfusion technique, still widely used in today’s laboratories [5].
Despite these advances in isolation and cell culture, culturing primary hepatocytes was never a trivial and easy task. In 2D cultures, they showed a natural propensity to suffer de-differentiation into fibroblastic-like cells and lose their liver-specific functions, since these types of cultures did not reproduce their physiologic niche.
It was not until 1989, that Dunn JC et al. finally published a reliable and secure method to extend their in vitro viability and function by culturing them in a collagen I gel sandwich, becoming the gold standard culture method still in use today [6]. Although, even by extending their viability in vitro, function decays rapidly with time, limiting their use in drug metabolism and toxicology to the initial days of the culture. These prompted researchers in the field to look into other culture configurations that could maintain function and viability at higher levels for a longer time.
2 Strategies for the Generation of Hepatic Tissue
2.1 Hepatocyte Aggregates and Spheroids
Spheroids are spontaneous non-adherent aggregations of cells that form a 3D tissue construct. Primary hepatocytes are capable of creating these structures called hepatospheres, where the majority of attachments among cells and extracellular matrix are preserved, being this essential to maintain both hepatic differentiation and functionality [1]. Studies in primary rat hepatocyte spheroids have demonstrated that they can recreate the liver’s microanatomy [7].
However, size is an important aspect in the formation of spheroids that needs to be always kept in mind size [8]. Glickis et al. found that cell viability decline with increasing spheroid size. They created a mathematical model based on his group’s observations that hepatocyte spheroids larger than 100 μm might block the diffusion of oxygen causing necrotic areas in their core [9].
In a first step, the spheroids originate small cell aggregates stimulated by integrin-ECM binding. These multiple multicellular aggregates give rise to a spheroid via cadherin-cadherin interactions. Hence, spheroid assembly represents the most energy efficient structure by minimizing their surface.
In 1961, Moscona et al. described how from individual embryonic cells it is possible to generate in vitro tissue-like constructions under standard controlled conditions [10]. The term aggregation pattern began being used to describe the capacity of different cell types in certain conditions to give rise to aggregates within 24 h. However, it was not until the 1980s when Landry et al. started to use the word spheroids to describe 3D cellular aggregates [11]. In this work, isolated rat liver cells re-aggregate and form structures very similar to those that we can find in vivo when prevented from attaching to a solid surface. This way, the cells produced their own ECM and hepatocytes can preserve their metabolic functions [11].
The key in the spheroids formation is to discover a reproducible protocol capable of rebuilding, in the case of the liver, the hepatic tissue. Presently, there are several techniques to achieve this, such as (1) non-adherent dishes under static conditions, (2) agitation cultures or (3) hanging drops.
The simplest way is to seed the hepatocytes in a low adherent well. After an initial attachment to the surface, the hepatocytes give rise to a monolayer that little by little separates from the dish forming spheroids. Also, different conditions like uncoated plates with a positive surface charge, coated dishes with albumin, or the single elimination of serum factors have been demonstrated to be useful in spheroid formation [12]. By contrast, coatings with collagens, fibronectin or laminin inhibit spheroid formation since they support hepatocyte adhesion.
Besides static conditions, agitation cultures such as rocked and rotary cultures in Petri dishes or bioreactors have been developed to improve spheroid formation. One example of this was the development of an innovative bioreactor in 2005 that rapidly gives rise to spheroids when loaded with porcine hepatocytes [12]. Compared with monolayer cultures, hepatocyte spheroids from this bioreactor showed less cell death and increased metabolic functions [12].
Though, recently it has been demonstrated that rocked cultures increase the spheroids formation due to an increment of the number of times hepatocytes clash compared with rotary cultures [13].
However, all techniques described above have several drawbacks, among them, we can distinguish the necessity of manually achieving a homogeneous population of aggregates since irregular geometry is typical. Kelm et al. described a universal method to form hanging drops applicable to a lot of cell lines [14]. This culture method consists of a few cells in suspension seeded upside down in the lid of a culture dish. The hepatospheres formed have high size reproducibility with less than 10% of variations.
A big challenge in tissue engineering is vascularization; therefore it is critical to constructing a functional vascular network. For this reason, the introduction of endothelial cells in the hepatocyte spheroids production has emerged as a possible solution [15]. Not only due to the intended need of angiogenesis but also to increase cell functionality by adding a non-parenchymal cell population.
Stellate cells also have an important role in revascularization after liver injury as they secrete laminin between hepatocytes, which will lay down a pathway that will give rise to the hepatic sinusoids. Hence, spheroids formed by hepatocytes and stellate cells are also an attractive in vitro system that has today great potential in drug discovery and many other applications [16]. The search for more biologically relevant systems is making scientists more aware of the importance of the hepatic non-parenchymal cell populations when assembling these cellular structures.
2.2 Liver Tissue Engineering
Up to date, only liver transplantation provides treatment for a huge variety of end-stage liver diseases. Due to the shortage of liver donors, hepatic tissue engineering has become a promising strategy for the treatment of different liver diseases. In this quest, a large effort has been dedicated to the development of suitable supporting biomaterials that mimic the liver extracellular matrix (ECM) and that allow steady cell growth, the maintenance of their differentiation and metabolic functions, and hepatic tissue organization with the mechanical and biological properties observed in vivo. As mentioned above, it is also fundamental to identify the most appropriate cells, to recapitulate in vitro the natural liver microarchitecture, comprised of multiple cell types. Under specific stimuli, these cells should interact with neighboring cells and the ECM and form liver parenchymal tissue, which could then be transplanted into patients to repair damaged tissue and increase liver function. From this point of view, this tissue engineered liver constructs are also excellent biological surrogates for the most multiple biomedical and pharmaceutical applications. Hence, we will provide a short review of some of the efforts in this area.
Briefly, different types of biomaterials have been used to date, and alginate scaffolds constitute one of the most widely used in tissue engineering due to its hydrophilic properties, porosity, weak adhesive properties and excellent tissue compatibility. Some studies suggest that alginate scaffolds loaded with hepatocytes or mesenchymal stem cells (MSC) increase the survival of animal models with 70–80% partial hepatectomy [17, 18]. Alginate scaffolds can also be used not for direct implantation, but for encapsulation of hepatocytes differentiated from bone marrow–derived MSC (BM-MSCs) [19]. This represents a new source of hepatic cells required for liver tissue engineering, as well as human embryonic (hES) or induced pluripotent stem cells (hiPS). These scaffolds are also used to induce hepatocyte differentiation in vitro [20]. Chitosan is another biomaterial used as a scaffold. It consists of linear amino heteropolysaccharide derived from chitin with unusual characteristics like low cytotoxicity, high biocompatibility, and high biodegradability. Its structure is very similar to the glycosaminoglycans (GAGs) present in the liver ECM. In this study [21], Shang et al. built a hybrid sponge made of galactosylated chitosan and hyaluronic acid to mimic the liver microenvironment and seeded hepatocytes and endothelial cells.
As mentioned above, type I collagen has also been used extensively for hepatocyte in vitro models. Because these cells lose their differentiated functions in 2D cultures, collagen sandwich consists of a matrix for cell attachment, allowing hepatic polarity and maintenance of their differentiated functions [22]. This is due to the capacity of sandwiches to mimic liver microenvironment, promoting cell-cell and cell-ECM interactions [23]. In other studies [24], like Melgar-Lesmes et al., people have used collagen constructs to seed endothelial cells. These matrices were then transplanted into living animals, showing liver damage reparation, suggesting that endothelial cells play a critical role in hepatic repair. Ranucci et al. bet on the utilization of void size collagen foams to induce rat hepatocyte differentiation, suggesting that pore sizes of the substrate (collagen I in this case) are quite relevant for particular cell morphogenesis [25]. Hyaluronic acid is another example. It consists of one of the main components of the ECM and plays a significant role in cell proliferation and migration. It is also commonly used for liver tissue engineering as a scaffold for cell growth [26, 27].
Not only naturally-derived materials have been used in liver tissue engineering efforts. Due to historical reasons, polyglycolic acid (PGA) scaffolds have been extensively used at the beginning of this field of science to generate hepatic tissue when seeded with primary hepatocytes, showing some albumin and urea secretion capability [28, 29].
More complex composite biomaterials have also been designed. The use of some of the compounds described above (chitosan, gelatin, type I collagen and hyaluronic acid) plus a conducting polymer: 3,4-ethylenedioxythiophene (PEDOT) [30]. The reason for the use of this polymer is to conduct charges to make local electrical fields inside of the scaffold, which would improve cell attachment, proliferation and protein expression of the seeded cells.
Recently, another innovative technique is to use acellular matrix derived from cells in culture. Kanninen et al. [31] demonstrated that after seeding hiPS in a HepaRG-derived acellular matrix, this matrix induced hepatic commitment of the hiPS, suggesting the importance of HepaRG acellular matrix in hepatic differentiation and maturation. Tiwari et at. also used these type of acellular scaffold, in this case, to seed hematopoietic stem/progenitor cells for its expansion [32].
Hence, despite the different strategies chosen by the multiple authors described above, most of the generated hepatic tissues reported have shown some degree of functionality, either in transplantation or in vitro assays. However, the end goal of producing bona fide hepatic tissue in vitro with the complexity observed in vivo is still distant in most of the presented cases.
2.3 Liver Bioengineering and Liver Organoids
In the past years, organ bioengineering has flourished, and several techniques have proved to be suitable candidates for the job at hand. Most strategies have relied on scaffolds with increasing complexity to replicate the liver microarchitecture and niche better, but there is also some work done in scaffold-free organogenesis focused approaches.
Recently, there has been an alternative to the approaches mentioned above, in which instead of trying to produce liver tissue or hepatic niche cell cultures and co-cultures, researchers have been thinking of the more sophisticated alternative of whole bioengineering liver or physiologically relevant liver structures like liver lobes, liver buds, liver vasculature and ducts.
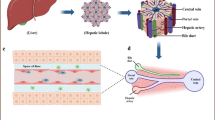
So far, the most widely described technique for liver bioengineering is the use of decellularized liver scaffolds for liver regeneration. In this technique, the rationale is that if the ECM remains in good condition after decellularization, then the different components of the ECM will serve as a guide for the cells and will aid not only in the attachment but also in the formation of the various structures that characterize hepatic tissue. This kind of approach is based on a two-step process, the decellularization step and the recellularization step.
For decellularization, since the objective is to remove all cells and cellular material, protocols are based on the combination of various cell-damaging factors such as freezing/thawing cycles, hypotonic stress, enzymes, shear stress and lipid surfactant action. The chemical action of detergent solutions is the most widely described method for dense non-hollow organs such as the liver. These solutions are perfused throughout the vasculature to detach the cellular material from the ECM so that only the structured ECM remains. As far as these solutions go, there is a tendency for the use of detergents such as Triton X-100 and SDS [33,34,35,36,37], but there have also been various other papers using solutions ranging from enzymes such as trypsin to chelating agents such as EDTA or EGTA [38, 39]. Additionally, there have been successful attempts while using as an inlet the vena cava, the portal vein, and the hepatic artery, as well as using fixed flow [35], fixed pressure [36] or even oscillating conditions [37].
After this step, again through perfusion, hepatocytes, stellate cells, endothelial cells and various other cell types can be used to repopulate the obtained scaffold. Some examples include the repopulation with mesenchymal and endothelial cell lines for vascular regeneration [40] or the repopulation with hepatic cell lines for metabolic, viability or functional assessments [34, 41].
A very similar approach to the one mentioned before relies on the substitution of the decellularized liver scaffold with an artificial biomimetic scaffold. By using an artificial scaffold, some issues pertaining the utilization of an animal-derived scaffold would be eliminated such as the possibility of transmission of zoonotic diseases and the vast ethical constraints associated with products of animal origin. As the objective is to create a structured microenvironment that resembles the natural liver ECM in which the cells can generate functional, structured and vascularized liver tissue, the artificial scaffold has to provide both support and a plethora of different cues to direct the cells towards the desired goal, liver organogenesis. So, to do just that, a biomimicry approach reliant on biofabrication techniques such as 3D printing, can be used. Either to generate an artificial scaffold, which can then be seeded with the desired cell types or to produce an already seeded scaffold/tissue if the cells are present in the printing solution (bioprinting) [42,43,44,45,46].
A different tactic, when compared to the previous ones, is to rely on the multipotency of progenitor cells and their ability of self-organizing into complex structures. In this way, through the study of developmental biology, protocols could be designed to mimic the natural conditions that lead to liver organogenesis. So far, the most relevant example is the liver bud experiment [47, 48], in which by controlling the set of conditions to which a 2D co-culture of iPS-derived hepatocytes, MSCs and hUVECs is exposed to, this culture contracts into a 3D budding structure reminiscent of a liver. It is worth mentioning that in this trial, the liver bud was able to form a non-functioning vascular network and rapidly emulated an adult liver when connected to a working vasculature (when transplanted). Additionally, it has been shown to be functional as it helped rescue drug-induced lethal liver failure models.
Other experiments related, pertain to the creation of hepatic/liver organoids from hepatic cell lines that even without having all of the defined organ structure, still show function and regenerative capabilities, such as the ability to generate new bile ducts or the actual organoid development from a single cell [49]. Liver organoids have also been obtained by using hydrogels in microfluidic settings [50], and similar results like the development of bile duct have also been achieved through encapsulation in alginate [51].
2.4 Future Perspectives
Regarding applications of liver bioengineering strategies, the most prominent (and most distant) one is transplantation. When considering this target, one must consider all of the safety concerns common for all medical applications and for that each different technique shows its strengths. When thinking of an off-the-shelf product for transplantation, the fastest option would be to have already a full liver ready for transplant, which is incompatible with an autologous and theoretically safer transplant. This fact leads to two routes, one being the production of sterile scaffolds ready to be seeded with the patient’s cells to generate a functional, transplantable liver or the production of allogenic bioengineered livers. Regarding Immunogenicity, the primary concern is the cells since natural scaffolds do not seem to trigger an intense immune response and in the long term are completely substituted by the patient’s own ECM (scaffolds are bioabsorbed completely in 90 days [52]). Artificial scaffolds meant for this aim will have to be designed and prepared so that they pass all quality controls for medical use.
Other more easily achieved, and just as critical applications, include disease modeling, and drug testing. For these requests, the liver buds appear to be excellent candidates as if the study is a disease that causes liver malformation. In these cases, development of the liver bud can be easily followed. Other diseases can also be observed and studied over time with this strategy. Drugs can also be tested in this system to study not only normal parameters such as efficacy/toxicity and drug metabolism but also the effect of drugs in liver organogenesis. Other liver bioengineering strategies like biofabrication [42, 53] and liver organoids [50] can also be used for this kind of applications.
3 Drug Development and Toxicology
3.1 Need of Engineered Liver Tissues for Drug Development
To launch a single drug into the market is a very hard (12–15 years) and costly ($3 – $5 billion) process [54]. After an initial screening, lead candidate compounds are characterized in vitro and in vivo for their ADME-Tox (absorption, distribution, metabolism, excretion and toxicity) properties before proceeding with clinical trials. However, most of the compounds (>90%) fail during these final stages. 43% of these failures occur due to a lack of efficacy and 33% due to the appearance of adverse effects [55], particularly in the liver, a phenomenon known as DILI (drug-induced liver injury) [56]. Taking into account that the liver is the organ where most drugs are metabolized and transformed to metabolites/active compounds, some of these substances by-products may result toxic to the own liver and the rest of the body. Hence, drug withdrawals at clinical stages in humans are mainly due to the use of inappropriate/inaccurate in vitro and in vivo liver models in the course of drug studies.
On the other hand, the liver is the target organ of some very common current diseases, such as infectious HBV, HCV [57], malaria [58], overnutrition-induced (type 2 diabetes, NAFLD, fibrosis, cirrhosis) [59,60,61] or tumoral diseases (hepatocellular carcinoma represents the 6th most common cancer worldwide) [62].
Considering all the above, liver models result necessarily for the development of novel drugs, not only for the study of xenobiotics metabolism and toxicity but also for the development of specific drugs for liver diseases. Hence, more realistic in vitro human liver models that resemble as closely as possible in vivo liver structure, physiology and pharmacological response are needed.
3.2 Limitations of Current In Vitro Liver Models to Test Drugs
As mentioned above, maintaining liver parenchymal function ex vivo results essential to generate stable systems for efficacy and toxicology drug studies, so fully functional hepatocytes are needed. For that, the 3D relationship of cells within the differential microenvironments of the liver (e.g. periportal versus pericentral), the regional hemodynamic flow patterns, and other physiological factors, such as oxygen tension and cytokine profiles have to be simulated in vitro. However, current cell-based models that are routinely used in drug testing are simple monoculture systems (typically standard microtiter plate formats) employed under static, non-physiologic conditions, that makes them suboptimal models for drug efficacy and safety testing, unable to mimic or predict more complex mechanisms of action [63].
Hepatocyte viability in suspension decreases significantly after 4 h [4]. Because of that, for years cryopreserved human hepatocytes in monolayer cultures have been the gold standard to test drug metabolism and toxicity [64]. However, cryopreservation also reduced hepatocyte viability, and function [65] and their culture in monolayer downregulate cell receptors involved in cell-cell and cell-extracellular matrix interactions, reducing drastically cell functionality over time [64]. The development of 2D cultures models, such as sandwich culture, allowed for increasing basal and induced drug-metabolizing enzyme activities and simulating in vivo biliary excretion rates [64, 66]. However, dedifferentiation of hepatocytes in long-term cultures and the lack of non-parenchymal cells that interact with hepatocytes continued being inherent disadvantages of these models [67]. The co-culture of hepatocytes with other liver cells, such as stellate cells, Kupffer cells, liver sinusoidal endothelial cells or liver epithelial cells diminishes to some extent these limitations, improving longevity/functionality of cells and producing higher expression of CYP and Phase II isoforms than in monotypic culture [68,69,70,71]. Nevertheless, co-cultures are usually based on the random mixing of different cell types and, thus, do not account for their particular anatomical relationship. More recently, looking for more relevant models, to emulate three-dimensional organization and morphology of hepatocytes within the liver, 3D cultures have been developed. 3D cultures range in complexity from monotypic or heterotypic spheroids [72, 73] to 3D scaffold systems [1] or more advanced models using microfluidic in vitro systems [1, 74]. Multiple commercial 3D co-culture platforms have been developed for drug screening and drug studies, such as the “Hepatopac” platform [75]; the 3D InSight™ Human Liver Microtissues of Insphero, the HepaChip® in vitro microfluidic system [76] or the Hμrel® microliver platforms [77].
Today, despite the fact that some issues have been addressed for certain applications with the models mentioned above, others continue to be biologically and technically challenging [66, 78].
3.3 Organoids in Drug Development
Organoids represent more complex models that try to simulate three-dimensional cell-cell and cell-ECM relationships in more relevant physiological conditions which mimic liver microenvironments arrangement and result amenable to high-throughput screening of compounds and feasible enough to guarantee long-term studies.
The optimal liver role is not only dependent on the coordinated function of the parenchymal and non-parenchymal cells within the hepatic acinus but also dependent on hepatic blood microcirculation. Aspects of the microcirculation can be simulated in vitro, via perfusion models, to create a dynamic in vivo like environment. In the last years, different macroscopic perfused in vitro liver systems, initially developed as bioartificial liver devices, have been created [74], providing evidence that perfusion can improve longevity and function in sophisticated hepatic systems, and thus show a better in vivo mimicry. Although these models represent the most physiologically practical systems, their size makes them unfeasible to be used in drug testing studies, as they lack the throughput and analytical flexibility for drug screening. The use of these organoids in drug development involves their miniaturization to a microscopic level. This new class of in vitro tools, often called “on-a-chip” tissue models, can mimic the architecture of small tissue sections and individual characteristics of the dynamic in vivo flow environment, while also offering more precise spatial and temporal control of soluble factors. These models, apart from resulting amendable to high throughput screening approaches, can be engineered for a real-time monitoring of the state of cells and their extracellular environment, which is crucial for determining cellular mechanisms of action in drugs [74].
Several organoid systems have been developed for drug screening and testing. One of the best examples of these organoids rests on microfluidic systems. Already in 2006, Kane et al. developed a microfluidic co-culture system of hepatocytes and T3-J2 fibroblasts in an 8 × 8 well array, demonstrating stable albumin and urea excretion for 32 days. Some years later, Hμrel Corporation developed a similar microfluidic in vitro liver platform for drug screening with commercial purposes (Hμrelflow TM) [77]. This platform, formed by multiple fluidically interconnected microscale cell culture compartments, enables simulation of the interaction of test substrates with two or more organs which provide an enhanced prediction of human response. In fact, in vivo-like absorption, distribution, metabolism, bioaccumulation, and toxicity of naphthalene were demonstrated when lung, adipose, and liver cells were fluidically connected [77]. Furthermore, the size of the system enabled microscopic imaging, oxygen sensing, physiologically appropriate ratios of chamber sizes, hydrodynamic shear stress and less consumption of media and cells. Even so, some issues, such as sample removal, complexity to maintain recirculation, cell monolayers on chips and not physiological tissue constructs limit the model significantly. Some years later, Au et al. developed another microfluidic model, a microfluidic organoid for drug screening (MODS) platform [79]. The novelty of this system comparing with previously developed MODS, was the ability to evaluate different conditions simultaneously and the automation of time-consuming processes such as the generation of mixtures and the formation of serial dilution series, which can result in more efficient screening of lead drug candidates. Recently, Vernetti et al. have developed and characterized a sophisticated system for investigating drug safety and efficacy in liver models of disease. This system includes a human 3D microfluidic four-cell sequentially layered, self-assembly liver model (SQL-SAL), and furthermore, fluorescent protein biosensors for mechanistic readouts and a microphysiology system database (MPS-Db) to manage, analyze, and model data [80].
Hollow fiber reactors have also been adapted to drug testing. In 2010, Schelzer et al. developed a microscale prototype of a hollow-fiber reactor. In this model, the bioreactor consisted of four cell chambers each of which included four compartments, (one for cells, two for culture medium, and the last one for oxygen supply) connected to provide the cells with a physiologically-based environment [81]. The prototype allowed for small numbers of cells and limited reagent use, microscopic evaluation of the cells and monitoring of oxygen concentrations. Later, a similar system with co-culture of parenchymal and non-parenchymal liver cells was also developed for studies of pharmacokinetics and drug toxicity, showing maintained albumin synthesis and CYP activity for 2–3 weeks [82]. Nevertheless, some limitations also arise in this kind of systems, such as the lack of physiologic gradients typically seen in liver tissue, the complexity of many tubing lines or the limited throughput since only a few different conditions can be assessed simultaneously.
As also mentioned above, decellularization constitutes a novel approach in liver models [33, 83]. This macroscopic model that can be used to investigate the liver development and regeneration can also be miniaturized for high-throughput drug studies.
Apart from physiological models, in the last years, organotypic models of liver diseases are also being developed for drug testing. Drug metabolism, toxicity, and efficacy in diseased livers differ substantially comparing with healthy conditions, so accurate models of disease are required. In this sense, Skardal et al. developed liver-based cell organoids in a rotating wall vessel bioreactor that inoculated with colon carcinoma cells to generate liver-tumor organoids for in vitro modeling of liver metastasis [84]. Recently, Leite et al. have developed hepatic organoids with fibrotic features, such as hepatic stellate cell activation and collagen secretion and deposition, for the study of drug-induced liver fibrosis [85]. Similarly, Lee et al. have generated a reversible- and irreversible-injured alcoholic liver disease model in spheroid-based microfluidic chips where rat primary hepatocytes and hepatic stellate cells (HSCs) are co-cultured [86].
Although enormous advances have been made in the last years to developed more realistic and predictive in vitro liver models for drug testing, the field is still dawning. There are critical issues that should be solved for the field to move forward. Standardizing model/platform characterization for drug-based studies (viability, secretory capacity, enzymatic and toxicology activities and drug transporter activity should be established for each model). Building specificity and sensitivity of the systems, recreating more accurately parenchyma zonation, developing better detection systems and better materials [74], or finding new unlimited fully functional cell sources [87] are some of the challenges to face today in the development of in vitro liver models for drug studies.
3.4 Cancer Research
Liver cancer leads to a considerable number of cancer-related deaths worldwide. Primary liver cancer, hepatocellular carcinoma (HCC), is the 5th most frequent cancer and the 3rd leading cause of cancer death. Approximately 700,000 people die because HCC every year [88]. Moreover, metastasis to the liver is a common occurrence in patients with cancer affecting other organs, usually by hematologic dissemination. The presence of liver metastasis changes dramatically patient’s survival, leading to the 2nd highest number of cancer-related deaths in the U.S [89].
In the majority of in vitro models of carcinogenesis tumor growth and metastasis are not optimal. The 2D models cannot represent the complexity of in vivo cancer architecture and the interactions between the healthy tissue and cancer cells. Liver organoids, as described above, are 3D in vitro cultures that can replicate much better the microenvironment of in vivo tissue. For this reason, organoids can be useful to evaluate better the cellular changes that lead to tumorigenesis and cancer progression [90, 91]. Further, organoids 3D culture could serve as a model to test cancer response to a drug. Drug diffusion kinetics and metabolism change dramatically in 3D culture. Probably because in this context it is also possible to reproduce the interactions between cells and matrix, that are not well recreated in 2D models. This hypothesis could explain why drugs that are effective in 2D models are often ineffective when tested in patient [90, 91].
Primary organoid culture including epithelial and mesenchymal cells has been successfully used in pancreatic, gastric and colorectal cancers [90, 91]. Nowadays, unlike other cancers, there is a lack of evidence and data published about utilization of liver organoids in primary liver cancer research, such as HCC and intrahepatic cholangiocarcinoma. Only one study released by Kosaka et al. has evaluated the application for cytotoxicity assay of alcohols of spheroid cultures of human hepatoblastoma cells (HuH-6 line) [92].
Recently liver organoids have been used for in vitro modeling of liver metastasis of colorectal adenocarcinoma [84]. Skardal et al. have evaluated the role of liver tumor organoids for modeling tumor growth and drug response in vitro. In this work, the authors created a liver-based cell organoid in a rotating wall vessel bioreactor that then was inoculated with colon carcinoma cells (CCC). The authors observed that there was a clear phenotypic difference between CCC cultivated in 2D and those inoculated in the liver organoids. In particular, inoculated CCC present a transition from an epithelial to a mesenchymal phenotype showing weak expression of ZO-1, E-cadherin, and vinculin, cytoplasmic expression of beta-catenin and expression of N-cadherin and MMP-9. All these changes suggest a switch to a mesenchymal, mobile and metastatic phenotype, similar to those of the metastatic CCC in vivo. CCC cells in the 2D culture did not present these changes and showed an epithelial phenotype. Another aim of the study was to evaluate the potential role of organoids as a model for drug screening studies. The authors were able to demonstrate that modification of WNT signal pathway through its activation or inhibition could modify the response to 5-fluorouracil [84].
The results of this study are an example of the potential of liver organoids in cancer research. 3D culture models offer a more accurate environment for the study of tumorigenesis and progression. The greater advantage versus 2D models is that organoids seem to be a more precise model of the architecture of the tissue in vivo. Recently, the introduction of novel biomaterials and biofabrication techniques also allowed for a more accurately evaluation of the interaction between cells and ECM.
Finally, the field which liver cell-based organoids seem to have more application is the advanced personalized medicine. Liver malignancies affect a considerable number of patients and are a leading cause of cancer-related death worldwide. In patients with primary liver cancer or liver metastasis future studies may use host-tissue based organoids to screen pharmacologic agents for activity against tumors and toxicity in the normal tissues.
4 Conclusions
Liver tissue engineering and bioengineering of whole livers are shaping the present and potentially the future of regenerative medicine. Nevertheless, the use of these lab created hepatic tissues is exploding in multiple biomedical and pharmaceutical applications. Most of the organoids, tissues and whole organs described above might not be ready for prime time at the bedside, but they already represent very accurate liver models to spur a new age of drug testing and discovery. When compared to the classic 2D models, their higher metabolic function and bona fide physiology are an assurance that we might have finally the tools to change the decades’ old models of 2D hepatocyte culture. To the field of toxicological and pharmaceutical research, maybe the time to modify the model used in the past two decades as come, hopefully changing with it the trend of drug development attrition rates.
References
Godoy P et al (2013) Recent advances in 2D and 3D in vitro systems using primary hepatocytes, alternative hepatocyte sources and non-parenchymal liver cells and their use in investigating mechanisms of hepatotoxicity, cell signaling and ADME. Arch Toxicol 87:1315–1530
Scherer WF, Syverton JT, Gey GO (1953) Studies on the propagation in vitro of poliomyelitis viruses. IV. Viral multiplication in a stable strain of human malignant epithelial cells (strain HeLa) derived from an epidermoid carcinoma of the cervix. J Exp Med 97:695–710
Howard RB, Christensen AK, Gibbs FA, Pesch LA (1967) The enzymatic preparation of isolated intact parenchymal cells from rat liver. J Cell Biol 35:675–684
Berry MN, Friend DS (1969) High-yield preparation of isolated rat liver parenchymal cells: a biochemical and fine structural study. J Cell Biol 43:506–520
Seglen PO (1976) Preparation of isolated rat liver cells. Methods Cell Biol 13:29–83
Dunn JC, Yarmush ML, Koebe HG, Tompkins RG (1989) Hepatocyte function and extracellular matrix geometry: long-term culture in a sandwich configuration. FASEB J: official publication of the Federation of American Societies for Experimental Biology 3:174–177
Abu-Absi SF, Friend JR, Hansen LK, Hu WS (2002) Structural polarity and functional bile canaliculi in rat hepatocyte spheroids. Exp Cell Res 274:56–67
Lin RZ, Chang HY (2008) Recent advances in three-dimensional multicellular spheroid culture for biomedical research. Biotechnol J 3:1172–1184
Glicklis R, Merchuk JC, Cohen S (2004) Modeling mass transfer in hepatocyte spheroids via cell viability, spheroid size, and hepatocellular functions. Biotechnol Bioeng 86:672–680
Moscona A (1961) Rotation-mediated histogenetic aggregation of dissociated cells A quantifiable approach to cell interactions in vitro. Exp Cell Res 22:455–475
Landry J, Bernier D, Ouellet C, Goyette R, Marceau N (1985) Spheroidal aggregate culture of rat liver cells: histotypic reorganization, biomatrix deposition, and maintenance of functional activities. J Cell Biol 101:914–923
Koide N et al (1990) Formation of multicellular spheroids composed of adult rat hepatocytes in dishes with positively charged surfaces and under other nonadherent environments. Exp Cell Res 186:227–235
Brophy CM et al (2009) Rat hepatocyte spheroids formed by rocked technique maintain differentiated hepatocyte gene expression and function. Hepatology 49:578–586
Kelm JM, Timmins NE, Brown CJ, Fussenegger M, Nielsen LK (2003) Method for generation of homogeneous multicellular tumor spheroids applicable to a wide variety of cell types. Biotechnol Bioeng 83:173–180
Inamori M, Mizumoto H, Kajiwara T (2009) An approach for formation of vascularized liver tissue by endothelial cell-covered hepatocyte spheroid integration. Tissue Eng Part A 15:2029–2037
Abu-Absi SF, Hansen LK, Hu WS (2004) Three-dimensional co-culture of hepatocytes and stellate cells. Cytotechnology 45:125–140
Shteyer E et al (2014) Reduced liver cell death using an alginate scaffold bandage: a novel approach for liver reconstruction after extended partial hepatectomy. Acta Biomater 10:3209–3216
Lin J et al (2015) Use an alginate scaffold-bone marrow stromal cell (BMSC) complex for the treatment of acute liver failure in rats. Int J Clin Exp Med 8:12593–12600
Lin N et al (2010) Differentiation of bone marrow-derived mesenchymal stem cells into hepatocyte-like cells in an alginate scaffold. Cell Prolif 43:427–434
Dvir-Ginzberg M, Elkayam T, Cohen S (2008) Induced differentiation and maturation of newborn liver cells into functional hepatic tissue in macroporous alginate scaffolds. FASEB J: official publication of the Federation of American Societies for Experimental Biology 22:1440–1449
Shang Y et al (2014) Hybrid sponge comprised of galactosylated chitosan and hyaluronic acid mediates the co-culture of hepatocytes and endothelial cells. J Biosci Bioeng 117:99–106
Chien HW, Lai JY, Tsai WB (2014) Galactosylated electrospun membranes for hepatocyte sandwich culture. Colloids Surf B Biointerfaces 116:576–581
Berthiaume F, Moghe PV, Toner M, Yarmush ML (1996) Effect of extracellular matrix topology on cell structure, function, and physiological responsiveness: hepatocytes cultured in a sandwich configuration. FASEB J: official publication of the Federation of American Societies for Experimental Biology 10:1471–1484
Melgar-Lesmes P, Balcells M, Edelman ER (2017) Implantation of healthy matrix-embedded endothelial cells rescues dysfunctional endothelium and ischaemic tissue in liver engraftment. Gut 66:1297–1305
Ranucci CS, Kumar A, Batra SP, Moghe PV (2000) Control of hepatocyte function on collagen foams: sizing matrix pores toward selective induction of 2-D and 3-D cellular morphogenesis. Biomaterials 21:783–793
Turner WS et al (2007) Human hepatoblast phenotype maintained by hyaluronan hydrogels. J Biom Mat Res Part B Appl Biom 82:156–168
Katsuda T, Teratani T, Ochiya T, Sakai Y (2010) Transplantation of a fetal liver cell-loaded hyaluronic acid sponge onto the mesentery recovers a Wilson’s disease model rat. J Biochem 148:281–288
Kaihara S et al (2000) Survival and function of rat hepatocytes cocultured with nonparenchymal cells or sinusoidal endothelial cells on biodegradable polymers under flow conditions. J Pediatr Surg 35:1287–1290
Kim SS et al (2000) Dynamic seeding and in vitro culture of hepatocytes in a flow perfusion system. Tissue Eng 6:39–44
Rad AT et al (2014) Conducting scaffolds for liver tissue engineering. J Biomed Mater Res A 102:4169–4181
Kanninen LK et al (2016) Hepatic differentiation of human pluripotent stem cells on human liver progenitor HepaRG-derived acellular matrix. Exp Cell Res 341:207–217
Tiwari A et al (2016) Expansion of human hematopoietic stem/progenitor cells on decellularized matrix scaffolds. Curr Protoc Stem Cell Biol 36:1C 15 11–11C 15 16
Baptista PM et al (2011) The use of whole organ decellularization for the generation of a vascularized liver organoid. Hepatology 53:604–617
Sabetkish S et al (2015) Whole-organ tissue engineering: decellularization and recellularization of three-dimensional matrix liver scaffolds. J Biomed Mater Res A 103:1498–1508
Wang Y et al (2015) Method for perfusion decellularization of porcine whole liver and kidney for use as a scaffold for clinical-scale bioengineering engrafts. Xenotransplantation 22:48–61
Buhler NE, Schulze-Osthoff K, Konigsrainer A, Schenk M (2015) Controlled processing of a full-sized porcine liver to a decellularized matrix in 24 h. J Biosci Bioeng 119:609–613
Struecker B et al (2015) Porcine liver decellularization under oscillating pressure conditions: a technical refinement to improve the homogeneity of the decellularization process. Tissue Eng Part C Methods 21:303–313
Soto-Gutierrez A et al (2011) A whole-organ regenerative medicine approach for liver replacement. Tissue Eng Part C Methods 17:677–686
Nari GA et al (2013) Preparation of a three-dimensional extracellular matrix by decellularization of rabbit livers. Revista espanola de enfermedades digestivas : organo oficial de la Sociedad Espanola de Patologia Digestiva 105:138–143
Baptista PM et al (2016) Fluid flow regulation of revascularization and cellular organization in a bioengineered liver platform. Tissue Eng Part C Methods 22:199–207
Mazza G et al (2015) Decellularized human liver as a natural 3D-scaffold for liver bioengineering and transplantation. Sci Rep 5:13079
Chang R, Emami K, Wu H, Sun W (2010) Biofabrication of a three-dimensional liver micro-organ as an in vitro drug metabolism model. Biofabrication 2:045004
Faulkner-Jones A et al (2015) Bioprinting of human pluripotent stem cells and their directed differentiation into hepatocyte-like cells for the generation of mini-livers in 3D. Biofabrication 7:044102
Gong H, Agustin J, Wootton D, Zhou JG (2014) Biomimetic design and fabrication of porous chitosan-gelatin liver scaffolds with hierarchical channel network. J Mater Sci Mater Med 25:113–120
Dickson I (2016) Liver: bioprinted liver lobules. Nat Rev Gastroenterol Hepatol 13:190
Skardal A et al (2015) A hydrogel bioink toolkit for mimicking native tissue biochemical and mechanical properties in bioprinted tissue constructs. Acta Biomater 25:24–34
Takebe T et al (2013) Vascularized and functional human liver from an iPSC-derived organ bud transplant. Nature 499:481–484
Takebe T et al (2014) Generation of a vascularized and functional human liver from an iPSC-derived organ bud transplant. Nat Protoc 9:396–409
Huch M et al (2013) In vitro expansion of single Lgr5+ liver stem cells induced by Wnt-driven regeneration. Nature 494:247–250
Nantasanti S et al (2015) Disease modeling and gene therapy of copper storage disease in canine hepatic organoids. Stem Cell Rep 5:895–907
Cheng N, Wauthier E, Reid LM (2008) Mature human hepatocytes from ex vivo differentiation of alginate-encapsulated hepatoblasts. Tissue Eng Part A 14:1–7
Faulk DM, Wildemann JD, Badylak SF (2015) Decellularization and cell seeding of whole liver biologic scaffolds composed of extracellular matrix. J Clin Exp Hepatol 5:69–80
Skardal A, Devarasetty M, Soker S, Hall AR (2015) In situ patterned micro 3D liver constructs for parallel toxicology testing in a fluidic device. Biofabrication 7:031001
Rawlins MD (2004) Cutting the cost of drug development? Nat Rev Drug Discov 3:360–364
Kola I, Landis J (2004) Can the pharmaceutical industry reduce attrition rates? Nat Rev Drug Discov 3:711–715
Kaplowitz N (2005) Idiosyncratic drug hepatotoxicity. Nat Rev Drug Discov 4:489–499
Rizzetto M, Ciancio A (2012) Epidemiology of hepatitis D. Semin Liver Dis 32:211–219
WHO (2016) World Malaria Report 2015. WHO
Smith BW, Adams LA (2011) Nonalcoholic fatty liver disease and diabetes mellitus: pathogenesis and treatment. Nat Rev Endocrinol 7:456–465
Cusi K (2009) Nonalcoholic fatty liver disease in type 2 diabetes mellitus. Curr Opin Endocrinol Diabetes Obes 16:141–149
Koppe SWP (2014) Obesity and the liver: nonalcoholic fatty liver disease. Transl Res: the journal of laboratory and clinical medicine 164:312–322
McGuire S (2016) World cancer report 2014. Geneva, Switzerland: World Health Organization, International Agency for Research on Cancer, WHO Press, 2015. Adv Nutr (Bethesda, MD) 7:418–419
LeCluyse EL, Witek RP, Andersen ME, Powers MJ (2012) Organotypic liver culture models: meeting current challenges in toxicity testing. Crit Rev Toxicol 42:501–548
Hewitt NJ et al (2007) Primary hepatocytes: current understanding of the regulation of metabolic enzymes and transporter proteins, and pharmaceutical practice for the use of hepatocytes in metabolism, enzyme induction, transporter, clearance, and hepatotoxicity studies. Drug Metab Rev 39:159–234
Terry C, Hughes RD, Mitry RR, Lehec SC, Dhawan A (2007) Cryopreservation-induced nonattachment of human hepatocytes: role of adhesion molecules. Cell Transplant 16:639–647
Gómez-Lechón MJ, Tolosa L, Conde I, Donato MT (2014) Competency of different cell models to predict human hepatotoxic drugs. Expert Opin Drug Metab Toxicol 10:1553–1568
Rowe C et al (2010) Network analysis of primary hepatocyte dedifferentiation using a shotgun proteomics approach. J Proteome Res 9:2658–2668
Bale SS et al (2015) Long-term coculture strategies for primary hepatocytes and liver sinusoidal endothelial cells. Tissue Eng Part C Methods 21:413–422
Krause P, Saghatolislam F, Koenig S, Unthan-Fechner K, Probst I (2009) Maintaining hepatocyte differentiation in vitro through co-culture with hepatic stellate cells. In Vitro Cell Dev Biol Anim 45:205–212
Ohno M, Motojima K, Okano T, Taniguchi A (2008) Up-regulation of drug-metabolizing enzyme genes in layered co-culture of a human liver cell line and endothelial cells. Tissue Eng Part A 14:1861–1869
Tukov FF et al (2006) Modeling inflammation-drug interactions in vitro: a rat Kupffer cell-hepatocyte coculture system. ToxicolIn Vitro : an international journal published in association with BIBRA 20:1488–1499
Luebke-Wheeler JL, Nedredal G, Yee L, Amiot BP, Nyberg SL (2009) E-cadherin protects primary hepatocyte spheroids from cell death by a caspase-independent mechanism. Cell Transplant 18:1281–1287
Sakai Y, Yamagami S, Nakazawa K (2010) Comparative analysis of gene expression in rat liver tissue and monolayer- and spheroid-cultured hepatocytes. Cells Tissues Organs 191:281–288
Usta OB et al (2015) Microengineered cell and tissue systems for drug screening and toxicology applications: evolution of in-vitro liver technologies. Technology 3:1–26
Chan TS et al (2013) Meeting the challenge of predicting hepatic clearance of compounds slowly metabolized by cytochrome P450 using a novel hepatocyte model. Hepato Pac Drug Metab Dispos: the biological fate of chemicals 41:2024–2032
Schütte J et al (2010) A method for patterned in situ biofunctionalization in injection-molded microfluidic devices. Lab Chip 10:2551–2558
Baxter GT (2009) Hurel – an in vivo-surrogate assay platform for cell-based studies. Altern Lab Anim: ATLA 37(Suppl 1):11–18
Guillouzo A, Guguen-Guillouzo C (2008) Evolving concepts in liver tissue modeling and implications for in vitro toxicology. Expert Opin Drug Metab Toxicol 4:1279–1294
Au SH, Chamberlain MD, Mahesh S, Sefton MV, Wheeler AR (2014) Hepatic organoids for microfluidic drug screening. Lab Chip 14:3290–3299
Vernetti LA et al (2016) A human liver microphysiology platform for investigating physiology, drug safety, and disease models. Exp Biol Med (Maywood) 241:101–114
Schmelzer E et al (2010) Three-dimensional perfusion bioreactor culture supports differentiation of human fetal liver cells. Tissue Eng Part A 16:2007–2016
Zeilinger K et al (2011) Scaling down of a clinical three-dimensional perfusion multicompartment hollow fiber liver bioreactor developed for extracorporeal liver support to an analytical scale device useful for hepatic pharmacological in vitro studies. Tissue Eng Part C Methods 17:549–556
Uygun BE et al (2010) Organ reengineering through development of a transplantable recellularized liver graft using decellularized liver matrix. Nat Med 16:814–820
Skardal A, Devarasetty M, Rodman C, Atala A, Soker S (2015) Liver-tumor hybrid organoids for modeling tumor growth and drug response in vitro. Ann Biomed Eng 43:2361–2373
Leite SB et al (2016) Novel human hepatic organoid model enables testing of drug-induced liver fibrosis in vitro. Biomaterials 78:1–10
Lee J et al (2016) A 3D alcoholic liver disease model on a chip. Integr Biol: quantitative biosciences from nano to macro 8:302–308
Huch M et al (2015) Long-term culture of genome-stable bipotent stem cells from adult human liver. Cell 160:299–312
Bruix J, Reig M, Sherman M (2016) Evidence-based diagnosis, staging, and treatment of patients with hepatocellular carcinoma. Gastroenterology 150:835–853
Young M, Ordonez L, Clarke AR (2013) What are the best routes to effectively model human colorectal cancer? Mol Oncol 7:178–189
Saito M et al (2006) Reconstruction of liver organoid using a bioreactor. World J Gastroenterol 12:1881–1888
Dedhia PH, Bertaux-Skeirik N, Zavros Y, Spence JR (2016) Organoid models of human gastrointestinal development and disease. Gastroenterology 150:1098–1112
Kosaka T et al (1996) Spheroid cultures of human hepatoblastoma cells (HuH-6 line) and their application for cytotoxicity assay of alcohols. Acta Med Okayama 50:61–66
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG
About this chapter
Cite this chapter
Solanas, E. et al. (2018). Tissue Organoids: Liver. In: Soker, S., Skardal, A. (eds) Tumor Organoids. Cancer Drug Discovery and Development. Humana Press, Cham. https://doi.org/10.1007/978-3-319-60511-1_2
Download citation
DOI: https://doi.org/10.1007/978-3-319-60511-1_2
Published:
Publisher Name: Humana Press, Cham
Print ISBN: 978-3-319-60509-8
Online ISBN: 978-3-319-60511-1
eBook Packages: MedicineMedicine (R0)