Abstract
The advent of improved cancer therapies has increased patient survivorship and with it the need to better understand the long-term sequelae of cancer and cancer therapies. As the number of survivors increases, so does our awareness of the long-term neurological complications of cancer treatments. Neurotoxicity can be particularly severe and impact quality of life and overall functioning. This chapter will focus on several common long-term neurological side effects of cancer and cancer treatments, with some emphasis on CNS toxicity in long-term survivors of pediatric cancers. Some of the most common CNS complications to be discussed below include impaired cognition, seizures, cerebrovascular events, and peripheral neuropathy.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Long-term cancer survival
- Sequelae
- Cancer treatments
- Cancer therapies
- Neurotoxicity
- Seizures
- Impaired cognition
- Peripheral neuropathy
- Cerebrovascular events
- CNS
- Complications
- Pediatric population
Introduction
The advent of improved cancer therapies has increased patient survivorship and with it the need to better understand the long-term sequelae of cancer and cancer therapies . With earlier detection methods and improved treatments, the number of cancer survivors by the year 2020 is estimated to reach approximately 20 million [1]. As this number increases, so does our awareness of the long-term neurological complications of cancer treatments. Among several cancer treatment -related side effects, neurotoxicity can be particularly severe and impact quality of life and overall functioning [2,3,4]. Given the inherent susceptibility of the developing nervous system to toxicity and an estimated high survival rates of up to 80% [5, 6], survivors of childhood cancers are affected disproportionately. Much of what we know about the long-term neurological complications of cancer and cancer therapies has been learned from research on survivors of childhood cancers.
This chapter will focus on several common long-term neurological side effects of cancer and cancer treatments , with some emphasis on CNS toxicity in long-term survivors of pediatric cancers. Some of the most common CNS complications to be discussed below include impaired cognition , seizures, cerebrovascular events, and peripheral neuropathy. A discussion of these complications in acute and subacute treatment settings can be found in earlier chapters of this text.
Cognitive Impairment
Cognitive impairment is a potentially long-lasting and late side effect of cancer and cancer treatments that can greatly impact quality of life and overall functioning [7]. Pediatric oncology patients are particularly vulnerable to the damaging effects of radiation and chemotherapy on the developing brain, and cognitive dysfunction has been reported in up to 40% of childhood cancer survivors. Neurocognitive difficulties have also been reported in adult cancer survivors [8,9,10,11,12,13,14,15,16]. Various cognitive domains can be impacted including attention, memory, and processing speed [17, 18].
Cognition in Survivors of Pediatric CNS Tumors
About 20% of pediatric tumors arise in the CNS. The 5-year overall survival of pediatric primary brain tumor patients has been estimated at more than 75% [5], with many survivors at risk of pervasive neurocognitive impairment decades after diagnosis and treatment [19,20,21,22,23,24,25,26,27]. Pediatric brain tumor patients experience up to a 20-fold increased frequency of severe impairment compared to the general population 20 years after diagnosis [28], and cognitive declines of 20–40 IQ points are not uncommon [20, 23, 29]. Importantly, subjective cognitive complaints do not mirror objective declines in cognition, despite significant functional implications. In one study, fewer than 10% of survivors reported severe cognitive impairment despite 50% being severely impaired in performance-based measures [28], highlighting the need for clinical assessment in addition to patient-reported outcomes when assessing cognition in this population. Despite subjective awareness of deficits, the functional implications of severe cognitive decline are tremendous, with observed reduced attainment of expected adult developmental milestones including education, employment, independent living [28], and possibly a lower socioeconomic attainment [20].
Cranial and craniospinal irradiation have been a well-known risk factor for impairment in cognition in children and adult survivors of pediatric brain tumors [5, 24, 30,31,32,33], particularly in areas of memory and executive functioning [34,35,36,37]. There is a correlation between radiation dose and IQ [38, 39]. Moreover, it is estimated that, when irradiated at age less than 7 years, nearly 100% of children require special education; after 7 years of age approximately 50% of children require special education [33]. The temporal lobe is particularly vulnerable to effects of radiation; higher dose levels to this region are associated with higher risk for memory impairment [21]. Newer treatment techniques have been aimed at minimizing dose and target volume, though the long-term benefit of these techniques has yet to be established.
While the precise mechanisms underlying radiation-induced cognitive dysfunction remain elusive, damage to hippocampal neurogenesis may be involved. Studies in animal models have demonstrated that therapeutic doses of cranial irradiation virtually ablate neurogenesis and that this inhibition of neurogenesis correlates with impaired performance on hippocampal-dependent memory tests [33, 40, 41]. Surprisingly, irradiation does not simply deplete the stem cell population, but rather disrupts the microenvironment that normally supports hippocampal neurogenesis [40, 42]. This microenvironmental perturbation is due largely to irradiation-induced microglial inflammation and anti-inflammatory therapy with the non-steroidal anti-inflammatory agent indomethacin partially restores hippocampal neurogenesis and function in rodents [42]. Additional possible mechanisms underlying radiation-induced cognitive dysfunction include white matter dysfunction, altered regional blood flow due to microvascular disease and acute and chronic oxidative stress and inflammatory responses [43,44,45].
Cognition in pediatric brain tumor survivors is also affected by factors other than radiation. In survivors with no exposure to radiation, there exists a 17-fold increase in the prevalence of impaired cognitive flexibility, and a fivefold increase in the prevalence of impairments in short- and long-term memory. Additionally, up to 37% of these survivors are severely impaired on at least one measure of processing speed [28].
Treatment of pediatric brain tumors may include cranial irradiation and/or cytotoxic chemotherapy; both have been implicated in the pathophysiology of cancer treatment-induced cognitive decline. Additional factors that have been associated with neurocognitive outcome include tumor site [46], age at diagnosis [47], history of seizures and hydrocephalus with shunt placement [20, 28]. After adjustment for exposure to cranial irradiation, Brinkman and colleagues found that seizures conferred a 50% increase in the risk of cognitive impairment [28]. This may be related to the use of anticonvulsant medications or the cumulative neurobiological and physiologic consequences of recurrent seizures. Likewise, the same group reported that a history of hydrocephalus with shunt placement conferred 40% increased risk of memory impairment [28], possibly related to hippocampal vulnerability to hydrocephalus [48].
Cognition in Survivors of Non-CNS Pediatric Cancers
Pediatric survivors of non-CNS cancers are also at risk of developing clinically significant impairment in neurocognitive functioning [6]. The incidence of impairment in at least one cognitive domain has been reported as high as 21% [49]. Most of these data have been derived from studies on survivors of childhood leukemias [50,51,52,53,54,55,56] and lymphomas. These studies suggest that cranial irradiation, chemotherapy (in particular high dose systemic and intrathecal) [57], stem cell transplant [58], and other treatments such as corticosteroids [55, 58] may be involved in the etiology of cognitive dysfunction in these patients. Additional factors associated with neurocognitive outcome in this patient population include age at diagnosis and female sex [49, 57, 59,60,61,62].
Acute lymphoblastic leukemia (ALL) represents the largest diagnostic group of survivors of childhood cancers, and the best studied. Neurocognitive impairment in this population is pervasive and long lasting, being reported up to 26 years after diagnosis, well into adulthood [53, 63]. Deficits in attention, memory, intelligence, processing speed, and executive functioning have been reported [53, 59, 64,65,66]. Until recently, these impairments had been largely attributed to prophylactic cranial irradiation [50, 53].
Cranial irradiation affects cognition in a dose-dependent manner [53], and, in this population, dose thresholds remain debatable. Recent reports suggest that a dose of less than 18 Gy may reduce risk [31, 67]. Withholding radiation and treating with chemotherapy alone may further reduce risk [31, 67] and has been an impetus for the omission of radiation therapy for most patients with childhood ALL. Instead, systemic and intrathecal chemotherapy is used to establish CNS prophylaxis.
Chemotherapy also has a significant impact on cognition in this population [6, 18, 60, 68,69,70,71,72]. Krull et al. [53] recently demonstrated that significant cognitive impairments were common among survivors of childhood ALL treated with chemotherapy only. Likewise, a recent meta-analysis assessing long-term neurocognitive functioning after chemotherapy-only regimens among survivors of childhood ALL revealed significant moderate impairment across multiple neurocognitive domains, with intelligence most affected [56]. Additional information is needed on the functional implications of these impairments though certainly patient and families should be provided with appropriate educational planning and surveillance.
Imaging correlates to neurocognitive outcomes in ALL survivors have been discovered, providing an understanding of some of the mechanistic underpinnings of late cognitive deficits and suggesting a role of white matter changes in neurocognitive changes secondary to cancer treatments. Specifically, smaller brain white matter volumes have been associated with larger deficits in attention, memory, intelligence, and academic achievement [73,74,75]. Additionally, fractional anisotropy (a measure related to degree of myelination) has been associated with IQ in childhood survivors of ALL.
Though limited, additional data exist to suggest that cognition is affected in childhood survivors of other non-CNS cancers. Intriguingly, some of these reports suggest that cognition can be affected by indirect mechanisms of treatment and not by direct CNS toxicity. Krull et al. [76] reported that adult long-term survivors of pediatric Hodgkin disease (HD) were at significant risk for neurocognitive decline. Importantly, this finding was associated with cardiopulmonary dysfunction attributable to standard care treatment with thoracic radiation and anthracyclines or bleomycin. Cardiopulmonary morbidity was further linked with cerebrovascular pathology as evidenced by multifocal leukoencephalopathy and hemosiderin deposits in the brain. This notable CNS finding was sixfold higher in HD survivors than in comparable cohorts and suggests a mechanism whereby pulmonary and cardiac dysfunction may lead to cognitive decline in this population. Primary prevention strategies have been sought and include reduction or omission of mantle field radiation, though these patients likely remain at risk given known cardiopulmonary side effects of anthracyclines and bleomycin.
Cognitive outcomes in long-term survivors of childhood osteosarcoma have also been evaluated [77]. Pediatric osteosarcoma has a 70% survival rate, largely due to advances in treatment including adjuvant chemotherapy with intravenous methotrexate. In addition, historical treatment regimens have incorporated anthracyclines, bleomycin, and alkylating agents, all chemotherapies known to affect cardiopulmonary function. The prevalence of cognitive decline in this population was found to be high, and this was not completely related to treatment with methotrexate. Maximum plasma concentrations, median clearance, and median/cumulative exposure to systemic methotrexate were not associated with cognitive impairment. Instead, any grade 3 or 4 adverse chronic conditions such as cardiac, pulmonary, or endocrine dysfunction were associated with poorer memory and slower processing speed. These results suggest that chronic health conditions related to cancer and cancer treatment can have a significant impact on cognition, in some cases more so that direct toxicity from treatment itself.
Cognition in Survivors of Adult Cancers
The incidence of post-treatment cognitive impairment in survivors of adult cancers ranges from 15 to 61% [78] and may be among the most frequently reported post-treatment symptoms of cancer survivors [79]. Effects can be worse immediately after treatment with some improvement over time [78] or with little recovery, leading to long-lasting impairment [10, 16, 80, 81]. Alternatively, patients may develop symptoms months to years following treatment [14]. Deficits in memory, executive function, processing speed, and attention appear most frequently [82]. Age [83, 84] and baseline cognitive reserve [83] have been identified as risk factors to neurotoxic effects of chemotherapy.
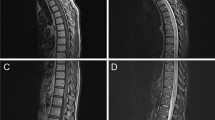
The mechanisms underlying effects of chemotherapy on the brain remain elusive, but may involve direct neurotoxic injury of hippocampal progenitor cells [85,86,87]. Such effects on hippocampal neurogenesis may help explain the delayed impact of treatment on cognition. Chemotherapy-induced increases in oxidative stress [88], white matter damage [86, 89], and reduced brain vascularization [78] may also be involved. Imaging studies have provided additional information about the structural and functional pathology associated with chemotherapy exposure. Reductions in hippocampal and frontal white and gray matter have been documented in cancer patients treated with chemotherapy [90, 91]. Advanced imaging studies using functional MRI, PET, and diffusion tensor MRI have provided additional albeit limited understanding of the pathophysiology of cognitive changes associated with chemotherapy [78].
Cerebrovascular Events
Numerous studies have shown that cancer survivors are at increased risk for stroke. The potential consequences of a stroke can be devastating leading to overt physical and cognitive disabilities, but can also be subtle and worsen cognitive impairment related to other factors. Cranial irradiation, in a dose-dependent fashion, is a particularly strong predictor of stroke risk [92,93,94,95,96,97]. The cumulative stroke risk in survivors treated with 50+ Gy has been estimated at 12% between 10 and 30 years of post-diagnosis [96]. Importantly, the elevated stroke risk conferred by cranial irradiation in childhood persists into early adulthood and continues to increase decades after treatment [96, 98, 99].
Radiation increases risk of arteriopathies such as moyamoya. Arteriopathies can lead to small and large vessel necrosis and has been identified as the most common risk factor for recurrent stroke in cancer survivors [100]. They typically occur shortly after completion of radiation, with one report estimating a median of 55 months from the time of radiation to discovery [101]. Since stroke risk persists decades after treatment, a second mechanism for delayed arteriopathy may exist.
Atherosclerosis is a more common cause of stroke in all comers and has also been linked with radiation [102,103,104,105]. The cumulative risk of stroke in survivors of childhood cancer treated with cranial irradiation increases fourfold for patients with additional atherosclerotic risk factors such as hypertension, diabetes, or black race [96], but is not solely dependent on these additional factors. A better understanding of the role of arteriopathy and atherosclerosis in the mechanism of stroke in cancer survivors would have significant implication for primary prevention, in particular in childhood cancer survivors. As it stands, the increased risk of stroke in cancer survivors suggests that frequent screening for modifiable stroke risk factors needs to be considered.
Seizures
Seizures are a common occurrence in both adults and children with brain tumors with an incidence near 30% [2]. The incidence of ongoing seizures in long-term survivors of pediatric brain tumors is as high as 14–25% [19, 106]. Seizures in this population are recognized as one of the most significant neurological complications of childhood brain tumors as they can occur frequently and at any time from diagnosis to years later. Moreover, they negatively impact quality of life [107]. Tumor pathology, extent of tumor resection and tumor recurrence are all risk factors [106]. In addition, treatment such as surgery, radiation, and chemotherapy can increase risk for seizures. In an analysis of a large cohort of survivors through the Childhood Cancer Survivor Study, patients with a history of radiation dose greater than 30 Gy to a cortical region of the brain had twofold risk of developing seizure as a late effect of treatment [19]. In this population, concurrent use of medications such as antidepressants and antibiotics, as well secondary medical complications such as infection or bleeding, can also lower seizure thresholds and increase risk [106].
Survivors of pediatric non-CNS cancers are likewise at increased risk for seizure as reported in a study assessing neurological morbidity in survivors of childhood ALL, which reported seizures in 11% of study participants [4]. History of CNS involvement of disease was associated with seizures, but additional factors such as cranial irradiation and chemotherapy likely also played a role [4].
Seizures themselves can be quite burdensome to cancer survivors, limiting functionality and quality of life in many cases, and affecting brain function in some. Moreover, additional side effects from the treatment of seizures with antiepileptic drugs (AEDs) can be equally as disturbing. Many of these agents have been associated with fatigue, and cognitive impairment, in addition to many non-neurological side effects. Thus, even infrequent seizures can impact overall medical health and quality of life.
Peripheral Neuropathy
Chemotherapy-Induced Peripheral Neuropathy
In comparison with the central nervous system, the peripheral nervous system (PNS) has better regeneration capacity. Notwithstanding, peripheral nerve toxicity, typically related to chemotherapy (chemotherapy-induced peripheral neuropathy, CIPN), can be debilitating, long lasting, and sometimes permanent [108, 109]. Until recently, this type of toxicity had remained an underestimated and under-recognized clinical problem in cancer survivors [110], perhaps because the accepted paradigm was that of a reversible condition. The evidence of long-term persistence of symptoms is now clear, in part due to the availability of large cancer registries such as Patient-Reported-Outcomes Following Initial Treatment of Long Term Evaluation of Survivorship (PROFILES) [110]. This has led to increased attention to this topic, so much so that the National Comprehensive Cancer Network recently expanded its guidelines for survivorship to address CIPN [111]. The hope is that with the increased attention, research in this field will continue to expand.
Most of the evidence supporting long-term CIPN in cancer survivors comes from studies of patient with breast, colorectal, and ovarian cancers who are typically exposed to neurotoxic agents. In one study of patients treated with oxaliplatin, 79% reported ongoing peripheral neuropathy after a median of 29 months from treatment [112]. Another study reported that over 25% of patients treated with oxaliplatin had NCI-CTC grade 3 symptoms 2 years after treatment. More compelling have been results from analysis of PROFILES data that revealed the persistence of CIPN up to 11 years post-treatment [113]. Cumulative dose was associated with worse outcomes [114].
Additional reports have revealed that CIPN can result in functional impairment. In a recent study, 89% of cancer survivors treated with oxaliplatin reported at least one symptom of neuropathy at 7 years from completion of therapy [115]. Importantly, due to their peripheral nerve symptoms, up to 24% of these survivors had difficulties driving, and 60% reported difficulties with exercise [115]. Functional consequences are further evidenced by reports that reveal an increased propensity to falls, with some series reporting up to 20% of patients with cancer and CIPN reporting falls [116, 117]. Motor neuropathy associated with taxanes use in breast cancer has been most strongly associated with increased propensity for falls [117]. Importantly, while clearly prevalent in cancer survivors, CIPN remains underreported by patients [118], suggesting that practitioners must be vigilant for symptoms and be educated to recognize early signs of the condition.
CIPN is also prevalent in adult survivors of pediatric cancers. In patients treated with either vinca alkaloids or platinum agents, the prevalence at a median of 25 years from diagnosis can be as high as 20 and 17.5% for long-term motor and sensory impairments, respectively [119]. In platinum-treated testicular cancer survivors, 22% had detectable peripheral neuropathy 23–33 years after therapy, and 6% had disabling neuropathy up to 22 and 15 years out from treatment, respectively [120, 121]. Clinical evidence for peripheral neuropathy as measured by EMG/NCS has also been reported in nearly 30% of survivors of childhood ALL at a mean of 7.4 years post-treatment [122]. CIPN in this population likely increases the risk for functional performance limitations, as evidenced by objective decreases in mobility and poor performance on a walk test and a timed “up and go” test [119].
Unfortunately, there are no proven preventive therapies for CIPN. There are data to support the role of duloxetine in the treatment of neuropathic pain related to CIPN, though relief is typically incomplete. No convincing data exist to support the use of other agents such as tricyclic antidepressants, gabapentine, or topical lidocaine, despite data supporting their utility in other neuropathic nerve conditions. Practitioners will often try these agents regardless of their success in these other conditions. Additional research with these agents is needed. Although no protective or curative agents exist, early detection of symptoms is important, in particular for children, as rehabilitative services and equipment may improve symptoms and provide strengthening and joint protection which in the long run could minimize functional limitations. For a compete discussion of CIPN including pathogenesis, clinical features, and evidence for treatment, please refer to Chap. 15 of this text.
Radiation-Induced Peripheral Neuropathy (RIPN)
Radiation-induced peripheral neuropathy (RIPN) is a less well-recognized, studied phenomenon, largely because it is more rare than its counterpart CIPN. The functional implications, however, can be equally severe [123]. RIPN has long been considered irreversible [124] and is associated with fibrotic changes to the nerves. The pathogenesis may be related to progressive fibrosis driven by reactive oxidative species and inflammatory mediators, ultimately resulting in demyelination, direct axonal injury, and nerve ischemia [125, 126].
A classic example of this type of neuropathy is a brachial plexopathy that can occur when radiation is directed at the chest, axillary region, thoracic outlet, or neck [127]. The incidence has decreased over the past six decades due impart to better radiation techniques and decreased doses. In the 1950s, the incidence was close to 65%, while now the incidence is only 1–2% [125], with 40–75% of cases resulting from radiation for breast cancer [128, 129]. Timing of symptom presentation varies widely, ranging anywhere from one year to decades after completion of treatment [130]. Presentation also varies ranging from mild sensory symptoms to debilitating pain and motor dysfunction. For a complete discussion of RIPN including pathogenesis, clinical features, and evidence for treatment, please refer to Chap. 14 of this text.
Summary
Neurological complications of cancer and cancer therapies are common in survivors of both adult and childhood cancers. Common complications often include cognitive deficits, strokes, seizures, and peripheral neuropathy. Importantly, these side effects are often associated with limitations in normal functioning, and impairment in quality of life. Much remains to be learned about the pathophysiology underlying many of these complications. This knowledge will ideally aid in the discovery of preventive and curative strategies, where currently there are none. Early recognition of these complications and risk for complications is crucial to provide both functional and psychological support to survivors and their families.
References
Jemal A, et al. Cancer statistics, 2009. CA: A Cancer J Clin. 2009;59(4):225–49.
Liigant A, et al. Seizure disorders in patients with brain tumors. Eur Neurol. 2001;45(1):46–51.
Luyken C, et al. The spectrum of long-term epilepsy-associated tumors: long-term seizure and tumor outcome and neurosurgical aspects. Epilepsia. 2003;44(6):822–30.
Khan RB, et al. Neurologic morbidity and quality of life in survivors of childhood acute lymphoblastic leukemia: a prospective cross-sectional study. J Cancer Surviv. 2014;8(4):688–96.
Howlander N, Krapcho M, et al. SEER Cancer statistics review, 1975–2011. Bethesda, MD: National Cancer Institute; 2011.
Anderson FS, Kunin-Batson AS. Neurocognitive late effects of chemotherapy in children: the past 10 years of research on brain structure and function. Pediatr Blood Cancer. 2009;52(2):159–64.
Mitby PA, et al. Utilization of special education services and educational attainment among long-term survivors of childhood cancer: a report from the childhood cancer survivor study. Cancer. 2003;97(4):1115–26.
van Dam FS, et al. Impairment of cognitive function in women receiving adjuvant treatment for high-risk breast cancer: high-dose versus standard-dose chemotherapy. J Natl Cancer Inst. 1998;90(3):210–8.
Schagen SB, et al. Cognitive deficits after postoperative adjuvant chemotherapy for breast carcinoma. Cancer. 1999;85(3):640–50.
Brezden CB, et al. Cognitive function in breast cancer patients receiving adjuvant chemotherapy. J Clin Oncol. 2000;18(14):2695–701.
Hurria A, et al. Cognitive function of older patients receiving adjuvant chemotherapy for breast cancer: a pilot prospective longitudinal study. J Am Geriatr Soc. 2006;54(6):925–31.
Ahles TA, Saykin A. Cognitive effects of standard-dose chemotherapy in patients with cancer. Cancer Investig. 2001;19(8):812–20.
Schagen SB, et al. Late effects of adjuvant chemotherapy on cognitive function: a follow-up study in breast cancer patients. Ann Oncol. 2002;13(9):1387–97.
Wefel JS, et al. The cognitive sequelae of standard-dose adjuvant chemotherapy in women with breast carcinoma: results of a prospective, randomized, longitudinal trial. Cancer. 2004;100(11):2292–9.
Schagen SB, et al. Change in cognitive function after chemotherapy: a prospective longitudinal study in breast cancer patients. J Natl Cancer Inst. 2006;98(23):1742–5.
Weis J, Poppelreuter M, Bartsch HH. Cognitive deficits as long-term side-effects of adjuvant therapy in breast cancer patients: ‘subjective’ complaints and ‘objective’ neuropsychological test results. Psycho-oncology. 2009;18(7):775–82.
Campbell LK, et al. A meta-analysis of the neurocognitive sequelae of treatment for childhood acute lymphocytic leukemia. Pediatr Blood Cancer. 2007;49(1):65–73.
Moleski M. Neuropsychological, neuroanatomical, and neurophysiological consequences of CNS chemotherapy for acute lymphoblastic leukemia. Arch Clin Neuropsychol. 2000;15(7):603–30.
Packer RJ, et al. Long-term neurologic and neurosensory sequelae in adult survivors of a childhood brain tumor: childhood cancer survivor study. J Clin Oncol. 2003;21(17):3255–61.
Ellenberg L, et al. Neurocognitive status in long-term survivors of childhood CNS malignancies: a report from the childhood cancer survivor study. Neuropsychology. 2009;23(6):705–17.
Armstrong GT, et al. Region-specific radiotherapy and neuropsychological outcomes in adult survivors of childhood CNS malignancies. Neuro Oncol. 2010;12(11):1173–86.
Anderson NE. Late complications in childhood central nervous system tumour survivors. Curr Opin Neurol. 2003;16(6):677–83.
Mulhern RK, et al. Late neurocognitive sequelae in survivors of brain tumours in childhood. Lancet Oncol. 2004;5(7):399–408.
Mulhern RK, et al. Neurocognitive consequences of risk-adapted therapy for childhood medulloblastoma. J Clin Oncol. 2005;23(24):5511–9.
Mabbott DJ, et al. Core neurocognitive functions in children treated for posterior fossa tumors. Neuropsychology. 2008;22(2):159–68.
Nagel BJ, et al. Early patterns of verbal memory impairment in children treated for medulloblastoma. Neuropsychology. 2006;20(1):105–12.
Ris MD, et al. Intellectual outcome after reduced-dose radiation therapy plus adjuvant chemotherapy for medulloblastoma: a Children’s Cancer Group study. J Clin Oncol. 2001;19(15):3470–6.
Brinkman TM, et al. Long-term neurocognitive functioning and social attainment in adult survivors of pediatric CNS tumors: results from the St Jude lifetime cohort study. J Clin Oncol. 2016;34(12):1358–67.
Ellenberg L, et al. Factors affecting intellectual outcome in pediatric brain tumor patients. Neurosurgery. 1987;21(5):638–44.
Smibert E, et al. Risk factors for intellectual and educational sequelae of cranial irradiation in childhood acute lymphoblastic leukaemia. Br J Cancer. 1996;73(6):825–30.
Spiegler BJ, et al. Change in neurocognitive functioning after treatment with cranial radiation in childhood. J Clin Oncol. 2004;22(4):706–13.
Palmer SL, et al. Predicting intellectual outcome among children treated with 35–40 Gy craniospinal irradiation for medulloblastoma. Neuropsychology. 2003;17(4):548–55.
Monje M. Cranial radiation therapy and damage to hippocampal neurogenesis. Dev Disabil Res Rev. 2008;14(3):238–42.
Jain N, et al. Neuropsychological outcome following intensity-modulated radiation therapy for pediatric medulloblastoma. Pediatr Blood Cancer. 2008;51(2):275–9.
Palmer SL, Reddick WE, Gajjar A. Understanding the cognitive impact on children who are treated for medulloblastoma. J Pediatr Psychol. 2007;32(9):1040–9.
Dennis M, et al. Neuropsychological sequelae of the treatment of children with medulloblastoma. J Neurooncol. 1996;29(1):91–101.
Aarsen FK, et al. Cognitive deficits and predictors 3 years after diagnosis of a pilocytic astrocytoma in childhood. J Clin Oncol. 2009;27(21):3526–32.
Grill J, et al. Long-term intellectual outcome in children with posterior fossa tumors according to radiation doses and volumes. Int J Radiat Oncol Biol Phys. 1999;45(1):137–45.
Kieffer-Renaux V, et al. Patterns of neuropsychological deficits in children with medulloblastoma according to craniospatial irradiation doses. Dev Med Child Neurol. 2000;42(11):741–5.
Monje ML, et al. Irradiation induces neural precursor-cell dysfunction. Nat Med. 2002;8(9):955–62.
Raber J, et al. Radiation-induced cognitive impairments are associated with changes in indicators of hippocampal neurogenesis. Radiat Res. 2004;162(1):39–47.
Monje ML, Toda H, Palmer TD. Inflammatory blockade restores adult hippocampal neurogenesis. Science. 2003;302(5651):1760–5.
Zhao W, Diz DI, Robbins ME. Oxidative damage pathways in relation to normal tissue injury. Br J Radiol. 2007;80(1):S23–31.
Lee WH, et al. Irradiation induces regionally specific alterations in pro-inflammatory environments in rat brain. Int J Radiat Biol. 2010;86(2):132–44.
Soussain C, et al. CNS complications of radiotherapy and chemotherapy. Lancet. 2009;374(9701):1639–51.
Mulhern RK, et al. Neuropsychological status of children treated for brain tumors: a critical review and integrative analysis. Med Pediatr Oncol. 1992;20(3):181–91.
Sands SA, et al. Long-term quality of life and neuropsychologic functioning for patients with CNS germ-cell tumors: from the first international CNS germ-cell tumor study. Neuro Oncol. 2001;3(3):174–83.
Savolainen S, et al. MR imaging of the hippocampus in normal pressure hydrocephalus: correlations with cortical Alzheimer’s disease confirmed by pathologic analysis. AJNR Am J Neuroradiol. 2000;21(2):409–14.
Kadan-Lottick NS, et al. Neurocognitive functioning in adult survivors of childhood non-central nervous system cancers. J Natl Cancer Inst. 2010;102(12):881–93.
Ochs J, et al. Comparison of neuropsychologic functioning and clinical indicators of neurotoxicity in long-term survivors of childhood leukemia given cranial radiation or parenteral methotrexate: a prospective study. J Clin Oncol. 1991;9(1):145–51.
Mahoney DH Jr, et al. Acute neurotoxicity in children with B-precursor acute lymphoid leukemia: an association with intermediate-dose intravenous methotrexate and intrathecal triple therapy—a Pediatric Oncology Group study. J Clin Oncol. 1998;16(5):1712–22.
Cousens P, et al. Cognitive effects of cranial irradiation in leukaemia: a survey and meta-analysis. J Child Psychol Psychiatry. 1988;29(6):839–52.
Krull KR, et al. Neurocognitive outcomes decades after treatment for childhood acute lymphoblastic leukemia: a report from the St Jude lifetime cohort study. J Clin Oncol. 2013;31(35):4407–15.
Mulhern RK, et al. Memory function in disease-free survivors of childhood acute lymphocytic leukemia given CNS prophylaxis with or without 1,800 cGy cranial irradiation. J Clin Oncol. 1988;6(2):315–20.
Waber DP, et al. Cognitive sequelae in children treated for acute lymphoblastic leukemia with dexamethasone or prednisone. J Pediatr Hematol Oncol. 2000;22(3):206–13.
Iyer NS, et al. Chemotherapy-only treatment effects on long-term neurocognitive functioning in childhood ALL survivors: a review and meta-analysis. Blood. 2015;126(3):346–53.
Langer T, et al. CNS late-effects after ALL therapy in childhood. Part III: neuropsychological performance in long-term survivors of childhood ALL: impairments of concentration, attention, and memory. Med Pediatr Oncol. 2002;38(5):320–8.
Wefel JS, Witgert ME, Meyers CA. Neuropsychological sequelae of non-central nervous system cancer and cancer therapy. Neuropsychol Rev. 2008;18(2):121–31.
Copeland DR, et al. Neuropsychological sequelae of childhood cancer in long-term survivors. Pediatrics. 1985;75(4):745–53.
Brown RT, et al. Cognitive and academic late effects among children previously treated for acute lymphocytic leukemia receiving chemotherapy as CNS prophylaxis. J Pediatr Psychol. 1998;23(5):333–40.
Waber DP, et al. Late effects of central nervous system treatment of acute lymphoblastic leukemia in childhood are sex-dependent. Dev Med Child Neurol. 1990;32(3):238–48.
von der Weid N, et al. Intellectual outcome in children and adolescents with acute lymphoblastic leukaemia treated with chemotherapy alone: age- and sex-related differences. Eur J Cancer. 2003;39(3):359–65.
Krull KR, et al. Reliability and validity of the childhood cancer survivor study neurocognitive questionnaire. Cancer. 2008;113(8):2188–97.
Giralt J, et al. Long-term neuropsychologic sequelae of childhood leukemia: comparison of two CNS prophylactic regimens. Int J Radiat Oncol Biol Phys. 1992;24(1):49–53.
Kingma A, et al. Academic career after treatment for acute lymphoblastic leukaemia. Arch Dis Child. 2000;82(5):353–7.
Meadows AT, et al. Declines in IQ scores and cognitive dysfunctions in children with acute lymphocytic leukaemia treated with cranial irradiation. Lancet. 1981;2(8254):1015–8.
Kadan-Lottick NS, et al. Comparison of neurocognitive functioning in children previously randomly assigned to intrathecal methotrexate compared with triple intrathecal therapy for the treatment of childhood acute lymphoblastic leukemia. J Clin Oncol. 2009;27(35):5986–92.
Mahone EM, et al. Motor and perceptual timing deficits among survivors of childhood leukemia. J Pediatr Psychol. 2007;32(8):918–25.
Espy KA, et al. Chemotherapeutic CNS prophylaxis and neuropsychologic change in children with acute lymphoblastic leukemia: a prospective study. J Pediatr Psychol. 2001;26(1):1–9.
Hill DE, et al. Visual and verbal short-term memory deficits in childhood leukemia survivors after intrathecal chemotherapy. J Pediatr Psychol. 1997;22(6):861–70.
Copeland DR, et al. Neuropsychologic effects of chemotherapy on children with cancer: a longitudinal study. J Clin Oncol. 1996;14(10):2826–35.
Kingma A, et al. No major cognitive impairment in young children with acute lymphoblastic leukemia using chemotherapy only: a prospective longitudinal study. J Pediatr Hematol Oncol. 2002;24(2):106–14.
Reddick WE, et al. Smaller white-matter volumes are associated with larger deficits in attention and learning among long-term survivors of acute lymphoblastic leukemia. Cancer. 2006;106(4):941–9.
Carey ME, et al. Reduced frontal white matter volume in long-term childhood leukemia survivors: a voxel-based morphometry study. AJNR Am J Neuroradiol. 2008;29(4):792–7.
Lesnik PG, et al. Evidence for cerebellar-frontal subsystem changes in children treated with intrathecal chemotherapy for leukemia: enhanced data analysis using an effect size model. Arch Neurol. 1998;55(12):1561–8.
Krull KR, et al. Neurocognitive function and CNS integrity in adult survivors of childhood hodgkin lymphoma. J Clin Oncol. 2012;30(29):3618–24.
Edelmann MN, et al. Neurocognitive and patient-reported outcomes in adult survivors of childhood osteosarcoma. JAMA Oncol. 2016;2(2):201–8.
Ahles TA, Root JC, Ryan EL. Cancer- and cancer treatment-associated cognitive change: an update on the state of the science. J Clin Oncol. 2012;30(30):3675–86.
Boykoff N, Moieni M, Subramanian SK. Confronting chemobrain: an in-depth look at survivors’ reports of impact on work, social networks, and health care response. J Cancer Surviv Res Pract. 2009;3(4):223–32.
Ahles TA, et al. Neuropsychologic impact of standard-dose systemic chemotherapy in long-term survivors of breast cancer and lymphoma. J Clin Oncol. 2002;20(2):485–93.
Schagen SB, et al. Neurophysiological evaluation of late effects of adjuvant high-dose chemotherapy on cognitive function. J Neurooncol. 2001;51(2):159–65.
Janelsins MC, et al. An update on cancer- and chemotherapy-related cognitive dysfunction: current status. Semin Oncol. 2011;38(3):431–8.
Ahles TA, Fau-Saykin AJ, et al. Longitudinal assessment of cognitive changes associated with adjuvant treatment for breast cancer: impact of age and cognitive reserve. J Clin Oncol. 2010;28(29):4434–40.
Kesler SR, Kent JS, O’Hara R. Prefrontal cortex and executive function impairments in primary breast cancer. Arch Neurol. 2011;68(11):1447–53.
Dietrich J, et al. CNS progenitor cells and oligodendrocytes are targets of chemotherapeutic agents in vitro and in vivo. J Biol. 2006;5(7):22.
Han R, et al. Systemic 5-fluorouracil treatment causes a syndrome of delayed myelin destruction in the central nervous system. J Biol. 2008;7(4):12.
Hyrien O, Dietrich J, Noble M. Mathematical and experimental approaches to identify and predict the effects of chemotherapy on neuroglial precursors. Can Res. 2010;70(24):10051–9.
Konat GW, et al. Cognitive dysfunction induced by chronic administration of common cancer chemotherapeutics in rats. Metab Brain Dis. 2008;23(3):325–33.
Ahles TA, Saykin AJ. Candidate mechanisms for chemotherapy-induced cognitive changes. Nat Rev Cancer. 2007;7(3):192–201.
McDonald BC, et al. Gray matter reduction associated with systemic chemotherapy for breast cancer: a prospective MRI study. Breast Cancer Res Treat. 2010;123(3):819–28.
Deprez S, et al. Longitudinal assessment of chemotherapy-induced structural changes in cerebral white matter and its correlation with impaired cognitive functioning. J Clin Oncol. 2012;30(3):274–81.
Haddy N, et al. Relationship between the brain radiation dose for the treatment of childhood cancer and the risk of long-term cerebrovascular mortality. Brain. 2011;134(Pt 5):1362–72.
Bowers DC, et al. Stroke as a late treatment effect of Hodgkin’s disease: a report from the Childhood Cancer Survivor Study. J Clin Oncol. 2005;23(27):6508–15.
Harrington CB, et al. It’s not over when it’s over: long-term symptoms in cancer survivors—a systematic review. Int J Psychiatry Med. 2010;40(2):163–81.
van den Beuken-van Everdingen MH, et al. Prevalence of pain in patients with cancer: a systematic review of the past 40 years. Ann Oncol. 2007;18(9):1437–49.
Mueller S, et al. Radiation, atherosclerotic risk factors, and stroke risk in survivors of pediatric cancer: a report from the childhood cancer survivor study. Int J Radiat Oncol Biol Phys. 2013;86(4):649–55.
Amir Z, Neary D, Luker K. Cancer survivors’ views of work 3 years post diagnosis: a UK perspective. Eur J Oncol Nurs. 2008;12(3):190–7.
Bowers DC, et al. Late-occurring stroke among long-term survivors of childhood leukemia and brain tumors: a report from the childhood cancer survivor study. J Clin Oncol. 2006;24(33):5277–82.
Mueller S, et al. Risk of first and recurrent stroke in childhood cancer survivors treated with cranial and cervical radiation therapy. Int J Radiat Oncol Biol Phys. 2013;86(4):643–8.
Fullerton HJ, et al. Recurrent stroke in childhood cancer survivors. Neurology. 2015;85(12):1056–64.
Ullrich NJ, et al. Moyamoya following cranial irradiation for primary brain tumors in children. Neurology. 2007;68(12):932–8.
Plummer C, et al. Ischemic stroke and transient ischemic attack after head and neck radiotherapy: a review. Stroke. 2011;42(9):2410–8.
Dorresteijn LD, et al. Increased carotid wall thickening after radiotherapy on the neck. Eur J Cancer. 2005;41(7):1026–30.
Meeske KA, et al. Premature carotid artery disease in pediatric cancer survivors treated with neck irradiation. Pediatr Blood Cancer. 2009;53(4):615–21.
Cavaletti G, Marmiroli P. Chemotherapy-induced peripheral neurotoxicity. Nat Rev Neurol. 2010;6(12):657–66.
Ullrich NJ, et al. Incidence, risk factors, and longitudinal outcome of seizures in long-term survivors of pediatric brain tumors. Epilepsia. 2015;56(10):1599–604.
Sato I, et al. Impact of late effects on health-related quality of life in survivors of pediatric brain tumors: motility disturbance of limb(s), seizure, ocular/visual impairment, endocrine abnormality, and higher brain dysfunction. Cancer Nurs. 2014;37(6):E1–14.
Mols F, et al. Chemotherapy-induced neuropathy and its association with quality of life among 2- to 11-year colorectal cancer survivors: results from the population-based PROFILES registry. J Clin Oncol. 2013;31(21):2699–707.
Beijers A, et al. Chemotherapy-induced peripheral neuropathy and impact on quality of life 6 months after treatment with chemotherapy. J Community Support Oncol. 2014;12(11):401–6.
Cavaletti G, Alberti P, Marmiroli P. Chemotherapy-induced peripheral neurotoxicity in cancer survivors: an underdiagnosed clinical entity? Am Soc Clin Oncol Educ Book. 2015;35:e553–60.
Kvale E, Urba SG. NCCN guidelines for survivorship expanded to address two common conditions. J Natl Compr Canc Netw. 2014;12(5 Suppl):825–7.
Park SB, et al. Long-term neuropathy after oxaliplatin treatment: challenging the dictum of reversibility. Oncologist. 2011;16(5):708–16.
Mols F, et al. Chemotherapy-induced peripheral neuropathy and its association with quality of life: a systematic review. Support Care Cancer. 2014;22(8):2261–9.
Beijers AJ, et al. Peripheral neuropathy in colorectal cancer survivors: the influence of oxaliplatin administration. Results from the population-based PROFILES registry. Acta Oncol. 2015;54(4):463–9.
Tofthagen C, et al. Oxaliplatin-induced peripheral neuropathy’s effects on health-related quality of life of colorectal cancer survivors. Support Care Cancer. 2013;21(12):3307–13.
Tofthagen C, Visovsky C, Berry DL. Strength and balance training for adults with peripheral neuropathy and high risk of fall: current evidence and implications for future research. Oncol Nurs Forum. 2012;39(5):E416–24.
Gewandter JS, et al. Falls and functional impairments in cancer survivors with chemotherapy-induced peripheral neuropathy (CIPN): a University of Rochester CCOP study. Support Care Cancer. 2013;21(7):2059–66.
Armes J, et al. Patients’ supportive care needs beyond the end of cancer treatment: a prospective, longitudinal survey. J Clin Oncol. 2009;27(36):6172–9.
Ness KK, et al. Chemotherapy-related neuropathic symptoms and functional impairment in adult survivors of extracranial solid tumors of childhood: results from the St. Jude lifetime cohort study. Arch Phys Med Rehabil. 2013;94(8):1451–7.
Glendenning JL, et al. Long-term neurologic and peripheral vascular toxicity after chemotherapy treatment of testicular cancer. Cancer. 2010;116(10):2322–31.
Strumberg D, et al. Evaluation of long-term toxicity in patients after cisplatin-based chemotherapy for non-seminomatous testicular cancer. Ann Oncol. 2002;13(2):229–36.
Ramchandren S, et al. Peripheral neuropathy in survivors of childhood acute lymphoblastic leukemia. J Peripher Nerv Syst. 2009;14(3):184–9.
Pradat PF, Delanian S. Late radiation injury to peripheral nerves. Handb Clin Neurol. 2013;115:743–58.
Gillette EL, et al. Late radiation injury to muscle and peripheral nerves. Int J Radiat Oncol Biol Phys. 1995;31(5):1309–18.
Delanian S, Lefaix JL, Pradat PF. Radiation-induced neuropathy in cancer survivors. Radiother Oncol. 2012;105(3):273–82.
Brown MR, Ramirez JD, Farquhar-Smith P. Pain in cancer survivors. Br J Pain. 2014;8(4):139–53.
Chen AM, et al. Brachial plexus-associated neuropathy after high-dose radiation therapy for head-and-neck cancer. Int J Radiat Oncol Biol Phys. 2012;84(1):165–9.
Kori SH, Foley KM, Posner JB. Brachial plexus lesions in patients with cancer: 100 cases. Neurology. 1981;31(1):45–50.
Fathers E, et al. Radiation-induced brachial plexopathy in women treated for carcinoma of the breast. Clin Rehabil. 2002;16(2):160–5.
Johansson S. Radiation induced brachial plexopathies. Acta Oncol. 2006;45(3):253–7.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG
About this chapter
Cite this chapter
Arrillaga, I. (2018). Neurological Complications of Cancer and Cancer Therapies in Long-Term Survivors. In: Schiff, D., Arrillaga, I., Wen, P. (eds) Cancer Neurology in Clinical Practice. Springer, Cham. https://doi.org/10.1007/978-3-319-57901-6_34
Download citation
DOI: https://doi.org/10.1007/978-3-319-57901-6_34
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-57899-6
Online ISBN: 978-3-319-57901-6
eBook Packages: MedicineMedicine (R0)