Abstract
Erythrocytapheresis, red blood cell (RBC) depletion, and RBC exchange transfusions are apheresis techniques used to rapidly lower the circulating red blood cell mass or to exchange the patient erythrocyte mass with donor red blood cells. Automated RBC exchange is performed using an apheresis device, while manual RBC exchange is based on sequential phlebotomies and isovolemic replacement. The main indication for RBC depletion in hematopoietic stem cell transplantation is the bone marrow processing in major ABO-incompatible transplants. These patients are particularly at risk for immediate posttransplant hemolysis due to preformed circulating isohemagglutinins that lyse the donor erythrocytes in the transplant. RBC depletion is an effective measure to avoid this complication. On the contrary, patients with minor ABO-incompatible HSCT are at risk for developing delayed hemolysis due to a passenger lymphocyte syndrome. Mature donor lymphocytes start to produce isohemagglutinins against recipient’s erythrocytes causing a hemolysis that typically starts 1–2 weeks after the transplant. Reduction of circulating patient’s erythrocytes using RBC exchange transfusions is a possible prophylactic intervention to reduce the risk of this potentially life-threatening hemolysis.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Red blood cell exchange
- Erythrocytapheresis
- RBC depletion
- Hematopoietic stem cell transplantation
- ABO
- Passenger lymphocyte syndrome
- Immediate hemolysis
- Delayed hemolysis
12.1 Introduction
Red blood cell (RBC) exchange is the replacement of patient’s RBC with allogeneic donor RBC and can be performed either manually or automated. It has the advantage over simple transfusions that patient’s RBCs are replaced without increasing the hematocrit or exposing the patient to the risk of fluid overload. RBC depletion describes an ex vivo procedure where RBCs are removed and replaced with crystalloid or colloid solution, when necessary. Typically, RBC depletion is used for bone marrow processing in the context of ABO-incompatible hematopoietic cell transplantation (HCT). This can be performed using different techniques, including sedimentation and apheresis. Erythrocytapheresis is an in vivo procedure in which RBCs are removed from the whole blood of the patient during the apheresis procedure and replaced by crystalloid or colloid solution (Padmanabhan et al. 2019). Although the terms RBC exchange, RBC depletion, and erythrocytapheresis in the medical literature are often used interchangeably, they describe different therapeutic procedures.
Manual RBC exchange implies sequential phlebotomies and isovolemic replacement with crystalloids and/or donor RBC. It has been frequently used in the past. However, with the introduction of automated cell separators, it has lost its importance but still might be applied in selected situations (Kuo et al. 2015; Swerdlow 2006). Automated RBC exchange is based on an apheresis procedure that separates RBCs from other blood components. The RBCs are subsequently selectively removed and replaced with donor RBCs alone and/or crystalloids/colloid solutions (Padmanabhan et al. 2019). Automated apheresis instruments have substantially facilitated the collection and replacement procedures. Based on clinical data such as body weight, height, gender, age, initial and final hematocrit, as well as average replacement fluid hematocrit and the fluid balance, the instruments calculate the exchange volumes. Moreover, automated systems allow to determine the percentage of remaining patient’s erythrocytes (fraction of the remaining cells), which is of particular interest for the calculation of the remaining pathological erythrocytes not only in patients with sickle cell disease but also in malaria and babesiosis. The introduction of automated RBC exchange procedures has substantially improved the standardization and has reduced the manipulations by the operator, and by that, it has become better applicable in clinical routine. Nevertheless, RBC exchange is still associated with some procedural risks as shown in Table 12.1, and the indications should therefore be carefully evaluated.
While plasmapheresis is quite frequently used in allogeneic HCT, there are few indications for RBC exchange or depletion mainly in the context of bone marrow processing. The indication for RBC exchange and depletion will be discussed in the following chapters.
12.2 ABO-Incompatible Hematopoietic Stem Cell Transplantation
Due to the fact that HLA and ABO antigens are independently inherited, 40–50% of all allogeneic HCT are performed across the ABO blood group barrier (Stussi et al. 2006; Klumpp 1991). As shown in Fig. 12.1, three groups of ABO mismatch can be distinguished in HCT: minor, major, and bidirectional ABO incompatibility. Minor ABO incompatibility, e.g., from an O-type donor to an A-type recipient, is characterized by the ability of donor B-lymphocytes to produce anti-recipient isohemagglutinins. In contrast, major ABO-incompatible HCT, e.g., from an A-type donor to an O-type recipient, is characterized by the presence of preformed anti-donor isohemagglutinins. In bidirectional ABO incompatibility, e.g., A-type donor to a B-type recipient, a combination of both the major and minor ABO blood group barriers must be overcome (Holbro and Passweg 2015). Although the overall outcome of patients undergoing ABO-incompatible HCT is not affected, several immunohematological complications such as hemolysis and pure red cell aplasia may arise in the posttransplant course (Worel 2016).
12.3 Hemolysis After Hematopoietic Stem Cell Transplantation
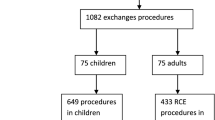
Hemolysis is a frequent complication after allogeneic HCT, but fortunately, most patients present with relatively mild and transient symptoms (Sokol et al. 2002). The most important causes of posttransplant hemolysis are shown in Fig. 12.2. Hemolysis can be classified by the onset of the symptoms into immediate and delayed hemolysis (Holbro and Passweg 2015). Immunological causes should be differentiated from nonimmune causes and microangiopathic hemolytic anemias. A thorough anamnesis including detailed drug history, as well as laboratory analysis to further characterize the nature of the hemolysis, is essential for the correct diagnosis. The Coombs test, elution techniques, and a morphological search for schistocytes on the blood film provide important diagnostic clues and should always be performed in patients presenting with hemolysis after allogeneic HCT.
Immune hematological complications such as antibody-mediated posttransplant hemolysis often, but not always, arise in the context of ABO-mismatched transplantations. Patients with a major ABO barrier are at risk for immediate hemolysis and later on delayed RBC engraftment or pure red cell aplasia, while patients with a minor ABO barrier are at risk for delayed hemolysis due to a passenger lymphocyte syndrome (PLS) (Fig. 12.1).
12.4 Management of Immediate Hemolysis
Acute immune hemolysis arising immediately after the infusion of the stem cell product is caused by preexisting isohemagglutinins of the recipient that bind to and eventually eliminate transplanted donor erythrocytes. Stem cell products collected by peripheral blood apheresis usually contain small amounts of donor erythrocytes, and further processing is recommended only if the erythrocyte content in the product is more than or equal to 20 mL and the isohemagglutinins of the patient are equal to or higher than 1:32 (Fig. 12.3) (Rowley et al. 2011). In contrast, bone marrow-derived stem cell products contain approximately 25–35% donor erythrocytes; thus, prevention of immediate hemolysis is mandatory prior to HCT. Since many products contain 1–1.5 L non-manipulated bone marrow, the equivalent of one RBC unit or even more can be present in the product.
Two strategies can be applied to reduce the risk of acute hemolysis. First, isohemagglutinins can be removed from the recipient prior to HCT by immunoadsorption, plasmapheresis (see also chapter 11), or slow infusions of incompatible donor-type RBC (Stussi et al. 2009). Both methods seem to be equally effective in reducing the isohemagglutinins titers lowering the pretransplant isohemagglutinins by five titer steps.
Center’s experience and patient-related factors, such as difficulties with venous access, anticoagulant toxicity, vascular volume changes, mild platelet depletion, and the risk of infection with plasma exchange or immunoadsorption, might direct physicians rather to the second option, the pretransplant manipulation of the bone marrow product (Daniele et al. 2014) (see also chapter 10). RBC depletion from the stem cell product can be achieved by density centrifugation (sedimentation) and/or by bone marrow processing with a cell separator. While this technology has been used since many years in major ABO-incompatible bone marrow transplant recipients, it has partially lost its importance in the last decade due to the preferential use of peripheral blood stem cell products. However, with the renewed interest for bone marrow stem cell products in the context of haploidentical HCT, the processing of ABO-incompatible bone marrow products will be increasingly used again (Passweg et al. 2017).
Several separation devices and technologies have been applied in the past. For an historical overview of the developments in bone marrow processing of ABO-incompatible stem cell products, we recommend a review by Daniele and colleagues (Daniele et al. 2014). Recently, bone marrow processing with the Amicus, COBE Spectra, and Spectra Optia devices has been published with excellent results regarding RBC depletion. All devices have RBC depletion rates exceeding 90% (Table 12.2) (Sorg et al. 2015; Witt et al. 2011; Kim et al. 2016; Larghero et al. 2006). The loss of stem cells has become less of an issue since the recovery rates for CD34+ positive cells in the newer generation of devices generally are more than 80%, and with the COBE Optia, the CD34+ recovery is more than 90%. Nevertheless, in the context of accreditation, the procedure has to be validated.
The bone marrow processing program on the Spectra Optia was accepted by the FDA in 2015. The advantages of the Spectra Optia are clearly reduced manual handling during the process. A new single bag system for the Spectra Optia bone marrow processing program was developed allowing the bone marrow aspirate to be recirculated during the procedure, thereby eliminating the need for the operator to manually reverse flow multiple times, as required for bone marrow processing procedures on COBE Spectra system. The total number of operator adjustments was reduced from 23 per procedure on the COBE Spectra to four on the Spectra Optia. This led to a higher stability and reproducibility of the procedures.
12.5 Management of Delayed Hemolysis Due to Passenger Lymphocyte Syndrome
Passenger lymphocyte syndrome (PLS) is a rare and unpredictable complication after allogeneic HCT or solid organ transplantation (Hows et al. 1986; Shortt et al. 2008). It is characterized by a delayed hemolysis 1–4 weeks (typically 7–14 days) after minor or bidirectional ABO-incompatible HCT. Pathogenetically, PLS is caused by immunocompetent donor-derived B-lymphocytes that start to produce during the engraftment phase isohemagglutinins against the remaining patient’s erythrocytes (Bolan et al. 2001; Booth et al. 2013). Although rare, it can cause severe hemolysis and may lead to multiorgan failure and eventually death (Watz et al. 2014). Hemolysis persists until the residual recipient RBCs are destroyed or replaced by donor or transfused RBC, which often occurs within few days after the onset of hemolysis. With the introduction of reduced-intensity conditioning regimen, an increased incidence of PLS has been observed. This is likely due to the higher lymphocyte content in the stem cell product and due to the higher percentage of remaining patient’s erythrocytes. Risk factors for PLS include peripheral blood stem cells, a donor with blood group O, a recipient with blood group A, cyclosporine alone as GVHD prophylaxis, and reduced-intensity conditioning (Watz et al. 2014; Gajewski et al. 1992; Worel et al. 2007).
It is recommended that patients with minor ABO barrier should be regularly monitored for signs of hemolysis during the early posttransplant phase; however, there is no generally accepted strategy to prevent PLS. The reduction of remaining patient’s erythrocytes by transfusing O-type RBC or by RBC exchange transfusions theoretically reduces the risk and the severity of delayed hemolysis with a therapeutic aim of less than 30% of residual patient’s RBC. As some transplant centers routinely transfuse O-type and others donor- and/or recipient-type RBC in patients with minor ABO-incompatible HCT, the incidence of delayed hemolysis might be influenced by these different transfusion strategies among transplant centers (Worel et al. 2010). The concept of lowering patient’s RBC content has been tested in a single-center study analyzing minor or bidirectional ABO-incompatible HCT receiving prophylactic RBC exchange transfusions with historical controls (Worel et al. 2007). All patients were transplanted with reduced intensity conditioning and mostly peripheral blood stem cells. To avoid immediate hemolysis, the bone marrow products were plasma depleted. The reason for starting the prophylactic RBC exchange program was that the incidence of PLS in this center among patients with reduced intensity conditioning was high (5/10 patients) with three patients dying of transplant-related mortality during the period of hemolysis. Thus, prophylactic RBC exchange transfusions were started prior to minor or bidirectional ABO-incompatible HCT replacing 1–1.5× the patient blood volume with a median of eight RBC concentrates. By this, the incidence of severe hemolysis and transplant-related mortality was reduced in minor ABO-incompatible HCT undergoing RBC exchange, while there was no difference in the incidence of GVHD and the overall survival.
A second retrospective single-center study analyzed prophylactic RBC exchange transfusion in minor and bidirectional ABO-incompatible HCT (Cunard et al. 2014). In contrast to the previous study, prophylactic RBC exchange was performed at day 4 after allogeneic HCT and only in patients deemed to be high risk according to the presence of predefined risk factors (minor or bidirectional ABO incompatibility, non-myeloablative conditioning, lack of prophylactic B cell-directed therapy (methotrexate)). It is of note that, in the RBC exchange group, a higher number of patients received reduced intensity conditioning regimens due to a change of the transplant practice in this period. The latter study showed a statistically not significant trend toward fewer severe hemolysis in the exchange group, while there was no difference in overall survival. Patients in the RBC exchange group required twice as many RBC transfusions compared to the historical group.
Taking this data together, there is no clear benefit of prophylactic RBC exchange to prevent PLS in patients with minor ABO-incompatible HCT resulting in a weak recommendation for RBC exchange in this clinical setting (2C) (Padmanabhan et al. 2019). Indeed, RBC exchange has not been widely accepted among transplant centers due to practical reasons and the relatively inefficient exchange procedure (Booth et al. 2013).
12.6 RBC Exchange for Treatment of Drug Overdoses
Some case reports have described RBC exchange as a treatment of drug intoxication with cyclosporine, tacrolimus, and sirolimus, alone or in combination with plasma exchange. The rationale for RBC exchange is that many drugs are not only bound to plasma proteins but also in the RBC compartment (Kurokawa et al. 1996; Hinderling 1997). Several case reports were published in patients with solid organ transplantation. In HCT, to the best of our knowledge, only two case reports are published. One case describes the successful treatment of cyclosporine intoxication (Moorman et al. 2011). Using sequential plasmapheresis and RBC exchange transfusions, the cyclosporine levels could be reduced to normal within 16 h. A second case describes the treatment of a sirolimus overdose (Galera et al. 2015). With four sessions of RBC exchange, the drug level could be reduced to normal levels; however, after stopping the RBC exchange, the sirolimus drug level rebounded due to redistribution of the drug from the extravascular compartment and the patient experienced renal failure.
12.7 Expert Point of View
RBC depletion in the context of major ABO-incompatible HCT is a standard procedure of bone marrow processing. The program on the Spectra Optia allows a standardized and efficient RBC depletion with an excellent recovery of CD34+ positive cells. It should be preferred over manual depletion methods, as it requires less operator manipulations with its inherent risks.
The evidence for prophylactic RBC exchange in patients with minor ABO-incompatible HCT as well as in the setting of drug overdosing is insufficient for a general recommendation. Nevertheless, it might be indicated in some clinical high-risk situations. Given the rarity of the indication, it should be done in close collaboration with the apheresis medicine specialist.
References
Bolan CD, Childs RW, Procter JL, Barrett AJ, Leitman SF (2001) Massive immune haemolysis after allogeneic peripheral blood stem cell transplantation with minor ABO incompatibility. Br J Haematol 112(3):787–795
Booth GS, Gehrie EA, Bolan CD, Savani BN (2013) Clinical guide to ABO-incompatible allogeneic stem cell transplantation. Biol Blood Marrow Transplant 19(8):1152–1158
Cunard R, Marquez II, Ball ED et al (2014) Prophylactic red blood cell exchange for ABO-mismatched hematopoietic progenitor cell transplants. Transfusion 54(7):1857–1863
Daniele N, Scerpa MC, Rossi C et al (2014) The processing of stem cell concentrates from the bone marrow in ABO-incompatible transplants: how and when. Blood Transfus 12(2):150–158
Gajewski JL, Petz LD, Calhoun L et al (1992) Hemolysis of transfused group O red blood cells in minor ABO-incompatible unrelated-donor bone marrow transplants in patients receiving cyclosporine without posttransplant methotrexate. Blood 79(11):3076–3085
Galera P, Martin HC, Welch L et al (2015) Automated red blood cell exchange for acute drug removal in a patient with sirolimus toxicity. J Clin Apher 30(6):367–370
Hinderling PH (1997) Red blood cells: a neglected compartment in pharmacokinetics and pharmacodynamics. Pharmacol Rev 49(3):279–295
Holbro A, Passweg JR (2015) Management of hemolytic anemia following allogeneic stem cell transplantation. Hematology Am Soc Hematol Educ Program 2015(1):378–384
Hows J, Beddow K, Gordon-Smith E et al (1986) Donor-derived red blood cell antibodies and immune hemolysis after allogeneic bone marrow transplantation. Blood 67(1):177–181
Kim J, Joseph R, Matevosyan K, Sarode R (2016) Comparison of Spectra Optia and COBE Spectra apheresis systems’ performances for red blood cell exchange procedures. Transfus Apher Sci 55(3):368–370
Klumpp TR (1991) Immunohematologic complications of bone marrow transplantation. Bone Marrow Transplant 8(3):159–170
Kuo KHM, Ward R, Kaya B, Howard J, Telfer P (2015) A comparison of chronic manual and automated red blood cell exchange transfusion in sickle cell disease patients. Br J Haematol 170(3):425–428
Kurokawa N, Kadobayashi M, Yamamoto K et al (1996) In-vivo distribution and erythrocyte binding characteristics of cyclosporine in renal transplant patients. J Pharm Pharmacol 48(6):553–559
Larghero J, Rea D, Esperou H et al (2006) ABO-mismatched marrow processing for transplantation: results of 114 procedures and analysis of immediate adverse events and hematopoietic recovery. Transfusion 46(3):398–402
Moorman MT, Epstein RB, Smith JW, O’Neal C, Holter JL (2011) Management of cyclosporine overdose in a hematopoietic stem cell transplant patient with sequential plasma exchange and red blood cell exchange. J Clin Apher 26(3):156–158
Padmanabhan A, Connelly-Smith L, Aqui N, Balogun RA, Klingel R, Meyer E et al (2019) Guidelines on the use of therapeutic apheresis in clinical practice—evidence-based approach from the Writing Committee of the American Society for Apheresis: the eighth special issue. J Clin Apher 34(3):171–354. https://doi.org/10.1002/jca.21705
Passweg JR, Baldomero H, Bader P et al (2017) Use of haploidentical stem cell transplantation continues to increase: the 2015 European Society for Blood and Marrow Transplant activity survey report. Bone Marrow Transplant 8:1–7
Rowley SD, Donato ML, Bhattacharyya P (2011) Red blood cell-incompatible allogeneic hematopoietic progenitor cell transplantation. Bone Marrow Transplant 46(9):1167–1185
Shortt J, Westall GP, Roxby D et al (2008) A “dangerous” group O donor: severe hemolysis in all recipients of organs from a donor with multiple red cell alloantibodies. Am J Transplant 8(3):711–714
Sokol RJ, Stamps R, Booker DJ et al (2002) Posttransplant immune-mediated hemolysis. Transfusion 42(2):198–204
Sorg N, Poppe C, Bunos M et al (2015) Red blood cell depletion from bone marrow and peripheral blood buffy coat: a comparison of two new and three established technologies. Transfusion 55(6):1275–1282
Stussi G, Halter J, Schanz U, Seebach JD (2006) ABO-histo blood group incompatibility in hematopoietic stem cell and solid organ transplantation. Transfus Apher Sci 35(1):59–69
Stussi G, Halter J, Bucheli E et al (2009) Prevention of pure red cell aplasia after major or bidirectional ABO blood group incompatible hematopoietic stem cell transplantation by pretransplant reduction of host anti-donor isoagglutinins. Haematologica 94(2):239–248
Swerdlow PS (2006) Red cell exchange in sickle cell disease. Hematology 2006(1):48–53
Watz E, Remberger M, Ringdén O et al (2014) Analysis of donor and recipient ABO incompatibility and antibody-associated complications after allogeneic stem cell transplantation with reduced-intensity conditioning. Biol Blood Marrow Transplant 20(2):264–271
Witt V, Beiglböck E, Fritsch G (2011) Bone marrow processing with the AMICUS™ separator system. J Clin Apher 26(4):195–199
Worel N (2016) ABO-mismatched allogeneic hematopoietic stem cell transplantation. Transfus Med Hemother 43(1):3–12
Worel N, Greinix HT, Supper V et al (2007) Prophylactic red blood cell exchange for prevention of severe immune hemolysis in minor ABO-mismatched allogeneic peripheral blood progenitor cell transplantation after reduced-intensity conditioning. Transfusion 47(8):1494–1502
Worel N, Panzer S, Reesink HW et al (2010) Transfusion policy in ABO-incompatible allogeneic stem cell transplantation. Vox Sang 98(3 Pt 2):455–467
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Stussi, G., Buser, A., Holbro, A. (2020). Red Blood Cell Exchange: When and Why?. In: Abutalib, S., Padmanabhan, A., Pham, H., Worel, N. (eds) Best Practices of Apheresis in Hematopoietic Cell Transplantation. Advances and Controversies in Hematopoietic Transplantation and Cell Therapy. Springer, Cham. https://doi.org/10.1007/978-3-319-55131-9_12
Download citation
DOI: https://doi.org/10.1007/978-3-319-55131-9_12
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-55130-2
Online ISBN: 978-3-319-55131-9
eBook Packages: MedicineMedicine (R0)