Abstract
Clinical details: A 69-year-old female presented with positive FOB; colonoscopy found impassable stricture at the transverse colon. CT scan demonstrates an approximately 3.5 cm annular lesions within the transverse colon as illustrated below.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
7.1 Case 1: Typical “Apple-Core” Appearance on CT of a Transverse Colon Primary. CT Staging: T3N2M0
Clinical details: A 9-year-old female presented with positive FOB; colonoscopy found impassable stricture at the transverse colon. CT scan demonstrates an approximately 3.5 cm annular lesions within the transverse colon as illustrated below.

Teaching points: CT scan is the primary imaging modality for staging colon cancer, alongside colonoscopy. The typical appearance of a colon cancer is usually described as an “apple core” due to the tumour-associated bowel wall thickening/stricture as illustrated in this case.
7.2 Case 2: Sigmoid Colon Primary. CT Staging: T3N2M0
Clinical details: A 74-year-old male presented with positive FOB; colonoscopy found mass lesion in the sigmoid colon, and biopsy confirmed moderately differentiated adenocarcinoma. CT scan demonstrates an approximately 5 cm annular lesions within the sigmoid colon as illustrated below.

Teaching points: CT scan is the primary imaging modality for staging colon cancer, alongside colonoscopy. The typical appearance of a colon cancer is demonstrated here with circumferential mural thickening of the affected segment of the bowel loop.
7.3 Case 3: Adenocarcinoma Within the Splenic Flexure of the Colon. On CT, the Approximately 5 cm Annular Lesion Is in Close Contact with the Anterior Surface and the Upper Pole of the Left Kidney as Illustrated Below. CT Staging: T4N2M0
Clinical details: A 65-year-old female presented with an acute episode of PR bleeding, and colonoscopy found a mass lesion in the splenic flexure. Histology confirmed moderately differentiated adenocarcinoma. Patient proceeded with neoadjuvant chemotherapy.

Teaching points: CT scan is the primary imaging modality for staging colon cancer, alongside colonoscopy. It is very useful to delineate the extent of colon primary and to assess its relationship with adjacent organs or structures as illustrated in this case.
7.4 Case 4: An Approximately 5 cm Annular Adenocarcinoma Within the Sigmoid Colon with Peri-colonic Extramural Infiltration. CT Staging: T3N1M0
Clinical details: An 83-year-old male presented with lower abdominal pain and bowel obstruction. Histology confirmed moderately differentiated adenocarcinoma (Fig. 7.1).
Teaching points: CT scan is the primary imaging modality for staging colon cancer, alongside colonoscopy. It is very useful to delineate the extent of colon primary and to assess its relationship with adjacent organs, and, in addition to transaxial images, reviewing the lesion using all three dimensions provides useful information as illustrated in this case.
7.5 Case 5: Caecum Primary with Mesenteric Nodal and Extensive Liver Metastases. CT Staging: T3N1M1
Clinical details: An 88-year-old female presented with weight loss and microcytic anaemia. Histology confirmed poorly differentiated adenocarcinoma. Patient was recommended for palliative care (Fig. 7.2).
Teaching points: CT scan is the primary imaging modality for staging colon cancer, alongside colonoscopy. It is very useful to delineate the extent of colon primary and detecting metastases as illustrated in this case.
7.6 Case 6: An Approximately 4 cm Annular Adenocarcinoma Within the Descending Colon with Peri-colonic Nodal Metastases and Adjacent Peritoneal Infiltration. CT Staging: T4N2M0
Clinical details: A 69-year-old male presented with PR bleeding, and colonoscopy found a necrotic mass lesion in the descending colon. Histology confirmed moderately differentiated adenocarcinoma. CT scan demonstrated an approximately 4 cm annular mass in the descending colon with locoregional nodal metastases (Fig. 7.3) and infiltration to the adjacent peritoneum (Fig. 7.3b). Patient proceeded to surgery.
(a) Sagittal image of CT scan demonstrates the colon primary in the descending colon as well as an adjacent nodal metastasis; (b) sagittal image of CT scan in the same patient demonstrates peritoneal thickening, posterior to the colon primary, consistent with disease infiltration and thus T4 disease
Teaching points: CT scan is the primary imaging modality for staging colon cancer, alongside colonoscopy. It is very useful to delineate the extent of colon primary and to assess its relationship with adjacent organs or structures as illustrated in this case.
7.7 Case 7: An Approximately 5 cm Annular Adenocarcinoma Within the Transverse Colon in a Patient with a History of Chronic Lymphocytic Leukaemia (CLL). CT Staging: T3N1M0
Clinical details: An 81-year-old female with a history of CLL for 14 years presented with diarrhoea, thought to be related to chemotherapy for her CLL. Colonoscopy found an annular mass lesion in the transverse colon. Histology confirmed poorly differentiated adenocarcinoma. CT scan demonstrated an approximately 5 cm annular mass in the transverse colon with widespread generalised lymphadenopathy above and below the diaphragm (Fig. 7.4).
Teaching points: CT scan is the primary imaging modality for staging colon cancer, alongside colonoscopy. It is however sometimes difficult to differentiate metastatic lymphadenopathy from underlying haematological proliferative disorders such as low-grade lymphoma or CLL, as illustrated in this case.
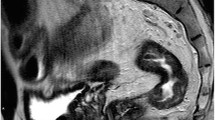
7.8 Case 8: An Approximately 2 cm Semi-annular Adenocarcinoma Within the Rectum. MRI Staging: T2N0M0
Clinical details: A 78-year-old male with known prostate cancer. MRI for prostate found an incidental rectal tumour. Histology confirmed moderately differentiated adenocarcinoma. MRI scan demonstrated an approximately 2 cm semi-annular mass confined to the 2–5 o’clock position as illustrated below.

Teaching points: MRI scan is the primary imaging modality for assessing rectal cancer. It is very useful to delineate the extent of rectal primary and to assess its relationship with adjacent musculature and thus guide surgery.
7.9 Case 9: Moderately Differentiated Adenocarcinoma of the Low Rectum. MRI Staging: T4N2M0
Clinical details: A 31-year-old male presented with a history of rectal bleeding, and flexible sigmoidoscopy showed low rectal cancer extending into the anal canal. MRI scan below demonstrates an annular tumour with extramural spread anteriorly at 1 o’clock position and contacts the posterior surface of the prostate gland.

Teaching points: MRI scan is the primary imaging modality for assessing rectal cancer. It is very useful to delineate the extent of rectal primary and to assess its relationship with adjacent musculature and organs and thus guide the management.
7.10 Case 10: Locally Advanced Adenocarcinoma Within the Rectum Extending for Approximately 7 cm in Craniocaudal Length. MRI Staging: T4N2Mx
Clinical details: A 32-year-old male presented with increased bowel frequency and passing blood. MRI scan demonstrated a locally advanced low rectal tumour with anterior extramural spread and contacts the prostate gland at 9 o’clock as illustrated below. Histology confirmed poorly differentiated adenocarcinoma.

Teaching points: MRI scan is the primary imaging modality for assessing rectal cancer. It is very useful to delineate the extent of rectal primary and to assess its relationship with adjacent musculature and organs and thus guide management.
7.11 Case 11: Locally Advanced Rectal Adenocarcinoma with Multiple Mesorectal Nodal Metastases. FDG-PET/CT Staging: T4N2M0
Clinical details: A 46-year-old male presented with rectal bleeding. Biopsy confirmed poorly differentiated adenocarcinoma. FDG-PET/CT scan demonstrates metabolically active rectal primary coupled with multiple mesorectal nodal metastases as illustrated below.
Teaching points: FDG-PET/CT scan is a very useful tool in assessing colorectal cancer especially in detecting distant metastases. One of the pitfalls is urinary activity in the pelvis like in this case: the rectal primary is strongly FDG avid, so it is the enlarged right-sided mesorectal nodal metastasis (Fig. 7.5a, b), whilst focal increased FDG accumulation is also seen in the left pelvic region (arrowed) but with no corresponding nodal lesion at this site. This is due to urinary activity in the left ureter as better illustrated in the MIP of the study in Fig. 7.5c.

Fig. 7.5
7.12 Case 12: Moderately Differentiated Transverse Colon Cancer with a Solitary Segment VIII Liver Metastasis on Staging CT Scan and Subsequent Liver MRI Scan Was Indeterminate. FDG-PET/CT Staging: T3N1M0
Clinical details: A 71-year-old male presented with anaemia, and colonoscopy confirmed moderately differentiated adenocarcinoma of the transverse colon. The staging CT scan demonstrated T3 N1 transverse primary with a solitary liver metastasis (Fig. 7.6a, arrowed) which was further assessed with a dedicated liver MRI, but this lesion was considered as indeterminate (Fig. 7.6b, arrowed). Subsequent FDG-PET/CT scan demonstrated FDG-avid colon primary (Fig. 7.6c, arrowed), but the concerned liver lesion showed no increased metabolic activity, likely to be a benign lesion.

Fig. 7.6
Teaching points: FDG-PET/CT scan is a useful tool in assessing colorectal cancer especially in characterising indeterminate lesions detected by CT or MRI, as illustrated in this case.
7.13 Case 13: Recurrent Poorly Differentiated Adenocarcinoma of the Rectum 3 Years After Surgery
Clinical details: An 88-year-old male, raising CEA 3 years after anterior resection of rectal primary (T2N0M0 at presentation). FDG-PET/CT scan demonstrates a solitary FDG-avid soft tissue lesion in the right presacral space. Patient proceeded with palliative radiotherapy with subsequent CEA reduction from 15 to 6 (Fig. 7.7).
(a) Fused FDG-PET/CT scan demonstrates the approximately 2.8 × 23 cm FDG-avid presacral soft tissue (yellow arrowed); the lesions can be identified on the corresponding unenhanced CT image (b) (yellow arrowed); this lesion is also identifiable in the lateral view of the MIP image (c) (green arrowed)
Teaching points: FDG-PET/CT scan is a very useful tool in detecting recurrent rectal cancer especially in identifying recurrent disease from postsurgical scarring tissue usually in the presacral space as illustrated in the case.
7.14 Case 14: Recurrent Colon Cancer 8 Years After Surgery
Clinical details: A 67-year-old female with a history of colon cancer (resected 8 years ago) presented with daily central and lower abdominal pain, frequent loose stools. CEA elevated. CT scan showed new soft tissue thickening along the SMA, suspicious for recurrent disease. FDG-PET/CT demonstrated increased metabolic activity. Patient proceeded with chemotherapy (Fig. 7.8).
(a) CT scan demonstrates soft tissue thickening along the SMA (yellow arrowed) which was not present in the previous CT scan 2 years ago (b) on subsequent FDG-PET/CT scan (c); this soft tissue demonstrates increased metabolic activity (green arrowed). (d) is the corresponding unenhanced CT image of the FDG-PET/CT study
Teaching points: FDG-PET/CT scan is a very useful tool in detecting recurrent colorectal cancer especially in identifying recurrent disease at less usual recurrent sites as illustrated in the case.
7.15 Case 15: Further Recurrence in the Right Hilum Following Resection of Solitary Lung Metastasis from a Dukes B Colon Cancer
Clinical details: An 81-year-old female who had anterior resection 3 years ago for a moderately differentiated adenocarcinoma of the sigmoid colon. Had right upper lobectomy a year later for a solitary lung metastasis. Follow-up CT scan 2 years later showed suspicious recurrence in the right hilum. FDG-PET/CT scan demonstrates FDG-avid right hilar soft tissue recurrence. Patient proceeded with cyberknife radiotherapy (Fig. 7.9).
(a) CT scan demonstrates soft tissue thickening at the right anterior hilum (yellow arrowed) which raised suspicion for further recurrent disease at this site. However, due to the previous surgery, it is less certain if this small soft tissue actually reflects recurrent disease. Subsequent FDG-PET/CT study showed significantly increased metabolic activity, (b) fused image, (c) MIP and (d) unenhanced CT image of the PET/CT study
Teaching points: FDG-PET/CT scan is a very useful tool in detecting recurrent colorectal cancer especially in identifying recurrent disease at less usual recurrent sites or postsurgical sites where the normal anatomy was disturbed, as illustrated again in the case.
7.16 Case 16: FDG-PET/CT Has Higher Sensitivity in Detecting Recurrent Colorectal Cancer
Clinical details: A 71-year-old male with a history of sigmoid cancer (resected 3 years ago). Elevated CEA and CT scan showed anastomotic recurrence as well as pelvic nodal metastases. FDG-PET/CT scan demonstrates, in addition, small but FDG-avid extra-pelvic left para-aortic nodal metastases, and as a result, the patient became ineligible for radiotherapy (Fig. 7.10).
(a) CT scan demonstrates anastomotic and other pelvic recurrent lesions including the left common iliac nodal metastasis/recurrence as illustrated in this figure (yellow arrowed), but subsequent FDG-PET/CT scan showed a further small extra-pelvic approximately 7 mm left para-aortic nodal metastasis at the level of L3 (green arrowed) (b–d)
Teaching points: FDG-PET/CT scan has higher specificity and also higher sensitivity in detecting recurrent colorectal cancer as illustrated in the case.
7.17 Case 17: Mucinous Colorectal Tumour Has Low FDG Avidity
Clinical details: A 46-year-old male presented with a mucinous adenocarcinoma of the rectum (T3N2M0) 4 years ago, had chemoradiation and is considered for pelvic exenteration surgery. Restaging CT scan showed a new presacral mass with bony destruction (Fig. 7.11a, yellow arrowed), which raised suspicion of disease infiltration, but this is complicated by the recent chemoradiation. On subsequent FDG-PET/CT scan, this mass demonstrates only very low-grade FDG avidity (Fig. 7.11b, green arrowed). Biopsy confirmed mucinous adenocarcinoma.

Fig. 7.11
Teaching points: Mucinous colorectal adenocarcinoma is known to have low FDG avidity, and thus FDG-PET/CT scans should be interpreted with caution.
7.18 Case 18: Postsurgical Inflammatory Changes Could Remain FDG Avid for a Protracted Time
Clinical details: A 40-year-old male with recurrent adenocarcinoma of the rectum (anastomotic recurrence 4 years after anterior resection). In addition to the known peri-anastomotic recurrence (Fig. 7.12c, green arrowed), the FDG-PET/CT scan also showed an ill-defined area of FDG-avid soft tissue thickening in the left breast (yellow arrowed in Fig. 7.12a–c) which actually corresponds to a port-a-cath removal 9 weeks prior to the PET/CT scan.

Fig. 7.12
Teaching points: Postsurgical inflammatory changes could remain FDG avid for a protracted time. It is always important to correlate imaging findings with clinical information especially when “unusual” findings are seen as illustrated in this case, whereas a left breast “lesion” was seen in a male patient.
7.19 Case 19: MRI in Assessing Response to Neoadjuvant Chemoradiotherapy in Lower Rectal Cancer
Clinical details: A 48-year-old male presented with rectal bleeding, and biopsy demonstrated moderately differentiated adenocarcinoma of the lower rectum. MDT recommended chemoradiation (Fig. 7.13).
(a) Sagittal view of the baseline pelvic MRI scan demonstrates an approximately 4.4 cm annular mass in the lower rectum with its lower edge approximately 1.9 cm above the top of the puborectalis sling (green arrowed, MRI stage: T2N0Mx); (b) is the same view taken 8 weeks after the completion of chemoradiation and demonstrates an excellent response to treatment with an approximately 1.9 cm predominantly residual scarring tissue at the primary disease site (yellow arrowed)
Teaching points: Differing from that of colon cancer, neoadjuvant chemoradiation plays instrumental roles in the treatment of lower rectal cancer. Although no imaging could predict a definite pathological complete remission, both MRI and FDG-PET/CT provide reliable information in assessing response to treatment.
7.20 Case 20: FDG-PET/CT Is a very Useful Tool in Assessing Colorectal Cancer in Response to Chemo- or Radiotherapy
Clinical details: A 50-year-old male presented with a locally advanced rectosigmoid signet ring cell adenocarcinoma. Baseline FDG-PET/CT scan (Fig. 7.14a) demonstrated a strongly FDG-avid rectosigmoid primary (yellow arrowed) and multiple mesorectal nodal metastases (green arrowed); subsequent FDG-PET/CT scan after chemoradiation demonstrated a partial response at the primary site (Fig. 7.14b, yellow arrowed), whilst the previous FDG-avid nodal metastases had mostly resolved.

Fig. 7.14
Teaching points: FDG-PET/CT scan is a very useful tool in assessing colorectal cancer response to treatment. Although low-grade residual FDG uptake could represent either small residual active tumour or post-treatment inflammatory process, focal, high-grade uptake usually reflects residual active disease as illustrated in this case. Also, despite some of the mucinous and signet ring cell adenocarcinomas could demonstrate only very low-grade FDG avidity, this is highly variable sometimes depending on the tumour cellularity and mucin content; as shown in this case, a signet ring cell tumour demonstrates high-grade FDG avidity.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Du, Y. (2017). PET/CT in Colorectal Cancer-Pictorial Atlas. In: Du, Y. (eds) PET/CT in Colorectal Cancer. Clinicians’ Guides to Radionuclide Hybrid Imaging(). Springer, Cham. https://doi.org/10.1007/978-3-319-54837-1_7
Download citation
DOI: https://doi.org/10.1007/978-3-319-54837-1_7
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-54836-4
Online ISBN: 978-3-319-54837-1
eBook Packages: MedicineMedicine (R0)