Abstract
As the routine use for CT increases, there is an opportunity to increase the detection rate of unsuspected and asymptomatic colorectal cancers. This pictorial essay provides abundant examples of the typical morphologic appearances of colorectal cancer in the unprepared colorectum. Many examples of lesions that were missed in clinical practice are illustrated with lessons on how to avoid these errors. Atypical appearances of colorectal cancer are also illustrated. The overall aim is to increase the detection rate of colorectal cancer at routine CT.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The use of CT for the evaluation of a variety of abdominal symptoms is commonplace [1]. These imaging studies represent an opportunity to diagnose unrecognized colorectal cancer, potentially at an early stage. Previous reports have shown the prospective miss rate of colorectal cancer at CT (49%) and the commonest morphologic appearances of these lesions [2]. The use of routine CT for detecting colorectal cancer has also been described by others [3,4,5].
The objective of this pictorial essay is to provide the radiologist with images of missed colorectal cancers and selected unusual presentations encountered while interpreting a routine CT examination. A variety of techniques were used; however, the majority (87%) were performed with intravenous contrast material. Cases are grouped to illustrate the variable patterns of these lesions to facilitate enhanced detection. Each case includes axial, coronal and sagittal images. The clinical scenario for each patient example is given to provide clinical context and understanding of patient symptoms and the effects of delays in diagnosis and treatment that can occur. The aim is to increase detection of colorectal cancer at routine CT.
Morphologic types and typical appearances
Three main morphologic appearances of colorectal cancer exist including annular (Fig. 1), polypoid (Fig. 2) and asymmetric (Fig. 3) bowel wall thickening. Annular lesions (sometimes referred to as concentric) encircle the bowel lumen, thicken the bowel wall and narrow the lumen of the colon. Polypoid lesions are predominantly intraluminal and present with a soft tissue mass of variable size within the bowel. Asymmetric lesions appear to thicken only a portion of the bowel wall. Awareness of these patterns of colorectal cancer will aid in their detection (Figs. 1, 2 and 3).
Annular colorectal cancer within the right colon. This is the most common morphologic type of colorectal cancer. A Axial CT. Bowel wall thickening (arrow) is present on both sides of the ascending colon. B Coronal CT. Circumferential bowel wall thickening (arrow) is present within the ascending colon. C Sagittal CT. Focal bowel wall thickening is seen on both sides of the bowel wall (arrow)
Polypoid colorectal cancer within the cecum. Soft tissue masses can often be distinguished from stool as it lacks internal air pockets and air bubbles. These lesions can be distinguished from the ileocecal valve because of its large size and the lack of internal fat. The ileocecal valve often contains internal fat attenuation when prominent. A Axial CT. Large mixed attenuation mass (arrow) within and expanding the lumen of the cecum. B Coronal CT. Polypoid soft tissue mass (arrow) is present within the cecum. C Sagittal CT. Soft tissue (arrow) fills the lumen of the cecum
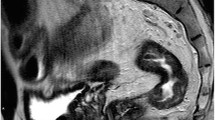
Asymmetric colorectal cancer within the rectum. These lesions are often the most difficult to detect as they are often smaller than annular (concentric) lesions. These images were acquired during the arterial phase of contrast enhancement during a CT angiogram. A Axial CT. Bowel wall thickening is present from the 4 o’clock to the 6 o’clock position in the posterior rectum (arrow). B Coronal CT. Enhancing asymmetric thickening is present along the left wall of the rectum (arrow). Air containing stool fills the remainder of the rectal lumen. C Sagittal CT. Nodular thickening and enhancement is present along the posterior wall of the rectum (arrow)
Lesions that were prospectively missed but identified retrospectively
Many of the lesions that were prospectively missed were performed for indications not specifically related to the colon. Abdominal pain was the commonest indication, but other symptoms or findings like constipation, bleeding or anemia were present in nearly half of patients with colorectal cancers that were missed on the initial interpretation [2]. Missed lesions were of advanced stage and most often located in the ascending colon and rectum [2]. Common radiologic findings among missed lesions were bowel wall thickening (91%), luminal narrowing (73%) and pericolonic soft tissue stranding or prominent pericolonic lymph nodes (35%) [2]. Nearly half of missed colorectal cancers were of concentric morphology, while asymmetric bowel wall thickening and polypoid morphology were each found in approximately 25% of patients [2]. For examples see Figs. 4, 5, 6, 7, 8, 9, 10 and 11.
Missed polypoid lesion in cecum. A 67-year-old male presenting with abdominal pain and a microcytic anemia. No colon lesion was identified at CT. The mass was identified at colonoscopy performed for routine polyp follow-up. At operation (right hemicolectomy) a 3.4-cm invasive well-differentiated, polypoid, adenocarcinoma was found in the ileocecal valve (T1, N0, M0). A Axial CT with contrast material. A soft tissue mass is present within the right colon (arrow). B Coronal CT. The lesion (arrow) is difficult to identify at the level of the ileocecal valve. C Sagittal CT. The collapsed colon lumen makes this lesion (arrow) difficult to identify. A soft tissue mass within the colon lumen, even if only well seen on one projection, should prompt further investigation
Missed polypoid lesion in ascending colon. A 84-year-old male evaluated at CT after a fall without identification of a colon lesion. Two months later the patient developed hematochezia. Colonoscopy identified a mass in the right colon. An invasive 3.2-cm poorly differentiated adenocarcinoma with 2 of 76 lymph nodes involved (T3, N1, M0) was identified following an extended right hemicolectomy. A Axial CT. A subtle intraluminal mass (arrow) is present within the upper ascending colon. B Coronal CT. The lesion (arrow) fills the colon lumen and displaces intraluminal gas medially. C Sagittal CT. An intraluminal soft tissue mass (arrow) is present in the ascending colon. Soft tissue attenuation within the colon lumen should prompt further investigation. Notice how the stool pattern and gas is displaced at the level of the mass
Missed asymmetric wall thickening in the transverse colon. A 79-year-old male with a history of chronic anemia was referred to CT with equivocal findings of pneumoperitoneum on an abdominal plain radiograph. No colon lesions or pneumoperitoneum was identified at CT. Seven months later the patient presents with hematochezia. A 4-cm nonobstructive mass was found in the transverse colon at colonoscopy. Pathologic examination of the biopsy specimen demonstrated an invasive, moderate to poorly differentiated adenocarcinoma. A Axial CT. Within the midtransverse colon there is asymmetric bowel wall thickening (arrow). Note the normal wall thickness in the adjacent colon is imperceptible. B Coronal CT. Asymmetric thickening of the colon wall (arrow), corresponding to the wall thickening on the axial image (A). C Sagittal CT. Asymmetric thickening of a colonic fold within the transverse colon. Comparison of the wall thickness of adjacent bowel is helpful in this case to differentiate normal from abnormal wall thickening. A focal area of bowel wall thickening different than adjacent colon should prompt suspicion of a colon lesion
Missed asymmetric wall thickening in the right colon. A 64-year-old male evaluated at CT for a perirectal abscess. No right colon lesion was identified at CT. Colonoscopy performed 2 months later for anemia and a positive stool DNA test reported a large mass in the cecum. Pathology results following right hemicolectomy reported an invasive 10 cm, poorly differentiated adenocarcinoma in the cecum at the ileocecal valve. Twelve of 43 lymph nodes were positive for metastatic carcinoma. A Axial CT without contrast material. Focal wall thickening (arrow) along the anterior wall of the right colon. B Coronal CT. Irregular wall thickening along the lateral wall of the right colon, just above the ileocecal valve (arrow). C Sagittal CT. Focal wall thickening along the anterior wall of the right colon (arrow). The CT indication of a perirectal abscess may have been a distractor, as the patient did have a large perirectal abscess (not shown). In addition, the lack of IV contrast material may have also contributed to the error
Missed recurrent colon cancer. A 88-year-old female referred to CT for abdominal pain, hypotension and GI bleeding. She had a previous right hemicolectomy for colon cancer and was on chronic anticoagulation. The CT report included a description of the right hemicolectomy, but no mention of a colon lesion. Colonoscopy was not ordered. The patient returned two months later with anemia and weakness. Colonoscopy reported a large mass in the right colon. The patient underwent a transverse colectomy. At pathology, an invasive poorly differentiated adenocarcinoma adjacent to the surgical suture line with anterior abdominal wall invasion was described. One of 5 lymph nodes was positive (T4, N1, M0). A Axial CT. The high attenuation suture line from the prior right hemicolectomy is visible. There is enhancing, circumferential wall thickening (arrows) distal to the anastomotic line. B Coronal CT. Circumferential, enhancing, wall thickening and irregularity (arrow) is present near the hepatic flexure of the colon. C Sagittal CT. Enhancing, wall thickening along the anterior wall of the colon (arrow) is present adjacent to the anastomosis (high attenuation sutures). The tumor is also adjacent to the anterior body wall with loss of the fat plane between the mass and the anterior abdominal wall musculature. An explanation for this error is not clear. The CT scan was interpreted at 7:58 in the evening. Fatigue, high workload, other distractions in the work environment and lack of colon tracking could all have contributed to this oversight
Missed concentric sigmoid mass. A 55-year-old female referred for CT to evaluate for obstruction. The report suggested a sigmoid stricture (no mass was reported) and colonoscopy was recommended. An 8-cm circumferential mass was found at endoscopy. A sigmoid resection was performed. Pathologic examination reported an invasive, well-differentiated adenocarcinoma without nodal involvement (T3, N0, M0). A Axial CT. Dilated, fluid-filled colon is present to the level of sigmoid colon. Bowel wall thickening and luminal narrowing is present at the transition point (arrow). B Coronal CT. Annular narrowing with wall thickening (arrow) is present at the site of colonic obstruction. C Sagittal CT. Dilated colon is seen to the level of the obstructing lesion (arrow). The commonest cause of colonic obstruction is colon cancer. Although a stricture secondary to diverticulitis is possible, no diverticula are present in this region of the colon, and there was no clinical history of diverticulitis. This lesion should not be confused with non-distension as the colon is diffusely dilated upstream from the mass (a finding that would not be present if the narrowing was secondary to transient non-distention)
Missed flat, low attenuation cecal mass. A 86-year-old male referred to CT because of vomiting. CT report did not include any findings related to the colon. The patient was discharged with the diagnosis of gastroenteritis. Fifteen months later he was found to be anemic. Colonoscopy reported a 3-cm mass in the cecum. A right hemicolectomy was performed. Pathologic examination reported a 2.9-cm invasive, moderately well-differentiated adenocarcinoma with a single positive lymph node (T3, N1, M0). A Axial CT. A low attenuation focal region of bowel wall thickening (arrow) is present in the cecum. The surface of the lesion is lobulated. B Coronal CT. Focal enhancement is present at the level of the mass (arrow). No oral contrast material had been administered. C Sagittal CT. The lesion is visible on the posterior wall of the cecum (arrow). The surface of the lesion is enhancing. This lesion is of lower attenuation than expected for a solid mass. This can occur when the lesion contains mucin. In addition, the lesion is flat (wider than it is higher) and appears dependent on the axial image, simulating stool. Stool is usually heterogeneous and contains air bubbles. The enhancement that is present in this lesion should prompt further investigation. Stool never enhances, and nearly all colon neoplasms will enhance
Missed concentric mass. A 85-year-old male with anemia. A colon lesion was not reported at CT. Colonoscopy reported a large mass at the splenic flexure. A transverse colectomy was performed. Pathologic examination revealed a 5.5 cm invasive, well to moderately differentiated mucinous adenocarcinoma (T3, N0, M0). A Axial CT. Partially concentric wall thickening (arrow) in the right transverse colon. Notice how adjacent bowel wall in the mid-transverse colon is of normal thickness. B Coronal CT. Annular wall thickening in the right transverse colon (arrow) with luminal narrowing. C Sagittal CT. Asymmetric thickening (arrow) in the right transverse colon. Bowel wall thickening can often be equivocal if the colon lumen is collapsed or partially distended. Comparison of a region of concerning bowel wall thickening with an adjacent loop that appears thin and nearly imperceptible can help identify a colonic mass. Colonoscopy cannot always locate lesions accurately. In this case the reported lesion in the splenic flexure was near the hepatic flexure
Unusual radiologic appearances of colorectal cancers
Colorectal cancers do not always present as one of the three most common morphologic types. Examples of different presentations to consider are shown in Figs. 12, 13, 14 and 15. These include a mass with a complicating intussusception, a mass with vivid enhancement, a surprisingly large mass with mesenteric and nodal extension, and a perforated carcinoma. Awareness of these variations in presentation can be helpful in arriving at an accurate and timely diagnosis.
Missed polypoid mass, later presenting with intussusception. A 86-year-old female referred for a CT scan for hematuria of unknown cause. The cecal mass was not detected at CT. Three months later the patient presents with abdominal pain and rectal bleeding. CT report includes a description of the intussusception without mention of a lead point mass. The patient underwent a right hemicolectomy. Pathologic report included a 4.2-cm invasive mucinous adenocarcinoma without nodal metastasis (T3, N0, M0). A Axial CT. Soft tissue mass (arrow) fills the cecum. B Coronal CT. The soft tissue mass (arrow) in the cecum expands the colonic lumen. Notice how it differs in appearance from colonic contents containing abundant air in the more distal colon. C Sagittal CT. Heterogeneous, enhancing soft tissue mass (arrow) in the proximal colon. D CT obtained 3 months later revealing an intussusception. Low attenuation, peripherally enhancing mass (arrow) is present in the transverse colon. E Coronal CT. The low attenuation mass (arrow) is identified in the transverse colon with intussuscepting fat visible in the right colon. Mucinous neoplasms can present as low attenuation masses. There is abnormal peripheral enhancement within this mass that excludes stool. An intussusception should always prompt a search for a lead point mass
Unusual cecal mass with huge regional node. A 86-year-old female referred for a CT scan for abdominal pain, abdominal mass and weight loss. CT reported a malignant appearing mass in the cecum with an adjacent mass and other smaller nodules. Pathologic report from a CT guided biopsy of the mesenteric mass reported a moderately to poorly differentiated adenocarcinoma. A Axial CT. A soft tissue mass is present in the cecum with associated soft tissue stranding. There are two adjacent mesenteric soft tissue masses (arrows). B Coronal CT. Soft tissue mass is present in the cecum (arrow). A larger mesenteric mass is located medial to the cecum. Another 1.5-cm lymph node is also visible in the ileocolic lymph node chain. Microscopic metastases from colon cancer to normal-size regional lymph nodes are very common, but they are usually not identified at CT. Enlarged nodes (> 1 cm) can be identified when present. Other diagnostic considerations in this case would include lymphoma or metastases from another source. The finding of extracolonic soft tissue stranding and/or lymph nodes should prompt a careful search of the colon for a mass
A 34-year-old male with a perforated colon cancer. The patient was referred to CT for abdominal pain and an elevated white blood count. There was a strong family history of colon cancer developing at a young age. CT reported a contained perforation of the sigmoid colon with irregular colonic wall thickening. A sigmoid resection was performed. Pathology reported a 6-cm invasive, moderately differentiated sigmoid adenocarcinoma with perforation and adjacent abscess formation. There was invasion of the visceral peritoneum. No lymph node involvement was present. A Axial CT. An irregular circumferential mass is present in the sigmoid colon with extensive soft tissue changes medial to the mass. B Coronal CT. A loculated fluid collection (arrow) and soft tissue stranding are present medial to the sigmoid mass. C Sagittal CT. Circumferential soft tissue mass (arrow) in the sigmoid colon. Diverticulitis can mimic a perforated colon cancer. One helpful feature that favors a diagnosis of carcinoma is the lobular surface and the abrupt wall thickening that is seen in this case (best demonstrated in Fig. 14A). Equivocal cases should be followed by either colonoscopy or repeat CT scan
A 89-year-old female with iron deficiency anemia requiring transfusion. CT enterography was performed to assess for a GI source of bleeding. Diffuse thickening of the cecum was reported at CT. Colonoscopy reported a large mass at the ileocecal valve. Pathologic evaluation of the biopsy material revealed invasive adenocarcinoma, moderately differentiated. A Axial CT—enteric phase of contrast enhancement. Intense enhancement of a circumferential mass in the cecum (arrow). B Coronal CT. Marked enhancement of the soft tissue mass in the cecum (arrow). Normal mucosal enhancement during the enteric phase of contrast enhancement of several small bowel loops. C Sagittal CT. Vivid contrast enhancement of a mass in the cecum (arrow). Colorectal cancer will enhance following intravenous contrast enhancement. The phase of contrast enhancement will determine the intensity of the enhancement. This amount of contrast enhancement during the enteric phase of contrast enhancement could also be seen with a neuroendocrine tumor
Summary
This pictorial essay provides the radiologist with clinical scenarios and examples of the typical appearance of most colorectal cancers, many examples of lesions that were missed in clinical practice, and atypical presentations of colorectal cancers. Radiologists with the knowledge of these tumor patterns combined with an approach to track the colon carefully at CT will identify the majority of colorectal cancers in practice.
Data availability
All relevant data supporting the findings of this study are reported in the article.
Code availability
Not applicable.
Abbreviations
- CT:
-
Computed tomography
- IV:
-
Intravenous
References
Smith-Bindman R, Kwan ML, Marlow EC, Theis MK, Bolch W, Cheng SY, Bowles EJA, Duncan JR, Greenlee RT, Kushi LH, Pole JD, Rahm AK, Stout NK, Weinmann S, Miglioretti DL (2019) Trends in Use of Medical Imaging in US Health Care Systems and in Ontario, Canada, 2000-2016. JAMA 322:843-856. doi:https://doi.org/10.1001/jama.2019.11456
Johnson CD, Flicek KT, Mead-Harvey C, Quillen JK (2023) Strategies for improving colorectal cancer detection with routine computed tomography. Abdom Radiol (NY) 48:1891-1899. doi:https://doi.org/10.1007/s00261-023-03884-3
Klang E, Eifer M, Kopylov U, Belsky V, Raskin S, Konen E, Amitai MM (2017) Pitfalls in diagnosing colon cancer on abdominal CT. Clin Radiol 72:858-863. doi:https://doi.org/10.1016/j.crad.2017.06.007
Ozel B, Pickhardt PJ, Kim DH, Schumacher C, Bhargava N, Winter TC (2010) Accuracy of routine nontargeted CT without colonography technique for the detection of large colorectal polyps and cancer. Dis Colon Rectum 53:911-918. doi:https://doi.org/10.1007/DCR.0b013e3181d5de13
Than M, Witherspoon J, Shami J, Patil P, Saklani A (2015) Diagnostic miss rate for colorectal cancer: an audit. Ann Gastroenterol 28:94-98
Acknowledgements
The authors acknowledge the assistance of Sonia Watson, PhD, in preparation of the manuscript.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Ethical approval
Exempt.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Flicek, K.T., Johnson, C.D. Pictorial essay: improving diagnostic effectiveness of colorectal cancer at CT. Abdom Radiol 49, 2060–2073 (2024). https://doi.org/10.1007/s00261-024-04219-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-024-04219-6