Abstract
The goal of precision medicine is to tailor treatments to the individual patient’s disease. In radiation oncology, this means tailoring the dose to the boundaries of the tumor, but also to the unique biology of the patient’s disease. In recent years, mathematical modeling has made inroads toward achieving these goals, through the optimization of radiation dose based on radiobiological parameters for individual patients. In this chapter, we review recent literature of mathematical models of tumor growth and response to radiation therapy (RT) and discuss the clinical utility of mathematical models, as well as provide a forward-looking perspective into how mathematical models may enhance patient outcomes through well-designed clinical trials.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction: Rationale for Mathematical Models in Radiation Oncology
Mathematics has played a pivotal role in radiobiology ever since the inception of the field (Hall and Giaccia 2011). Fowler provides an excellent historical account of the trials, tribulations, and challenges of translating laboratory-based radiobiology into the clinic in his 2006 perspective piece published in Physics in Medicine and Biology (Fowler 2006). Over the past 50 years, many experiments have been performed to understand and predict the biological effects of radiation in various dose and fraction schemes. Along with these experiments have come mathematical models of biological response that attempt to provide a mechanistic and predictive component to the observed data.
Despite the enormous variability in experimental conditions and mathematical models, consistent patterns between radiation dose and biological responses have emerged. A critical paradigm in the field is the finding that when the surviving fraction of cells is plotted on a log scale against radiation dose, the trend can be reliably predicted by a quadratic model. This observation led Brenner et al. to demonstrate that several mathematical descriptions (e.g., radiation damage, repair, and response to RT) result in predictions of dose-response relationships similar to this central paradigm (Brenner et al. 1998). Thus, the fundamental linear-quadratic (LQ) dose-response relationship has endured and continues to provide the benchmark assessment of biological response to radiation. The LQ model states that the surviving fraction (SF) of cells after a dose (D) of radiation is given by
where α (1/Gy) and β (1/Gy2) are parameters that determine the shape of the curve. Indeed, a vast literature exists on the mechanistic and empirical history of this famous equation, and entire books have been written about the mathematics of radiobiology (Hall and Giaccia 2011; Dale and Jones 2007).
To underscore the contemporary relevance of mathematical modeling in the spatial and biological optimization of RT, a point-counterpoint piece published in Medical Physics in 2016 (Kim et al. 2016) contends that, “With newly available tools such as functional imaging and mathematical models to better estimate the patient-specific, radiobiological parameters … spatiotemporal optimization will enhance current efforts to find more effective treatment schedules to improve patient outcome.” The argument against the contention only questions the degree of the potential gains with RT optimization alone; suggests that increased use of RT + chemotherapy or RT + radiosensitizers will achieve larger gains; and laments that progress will take at least five years, partially due to the need for validated mathematical models. Both of these arguments are likely true, and both are actually encouraging for the broader view on the role of mathematical modeling in the optimization of RT-based therapies.
Similarly, several authors have previously discussed the clinical and translational relevance of mathematical models to predict tumor growth and response to RT (Yankeelov et al. 2013; Jackson et al. 2014; Baldock et al. 2013; Gallasch et al. 2013). Mathematical models can inform clinical practice in a number of ways: via patient-specific models of tumor growth and response to RT, by guiding the design of preclinical studies to predict radiation sensitivity, by helping select patients for definitive clinical trials on these mathematically-driven treatment enhancements, and ultimately by optimizing radiation dose and treatment planning. The challenges involved with the inter-disciplinary, iterative cycle between development, testing, and application of mathematical models in collaboration with clinicians and experimental biologists, as well as some recent successful examples, are summarized by Michor and Beal (2015).
2 Illustrative Mathematical Models of Cellular- and Tissue-Scale Responses to Radiation
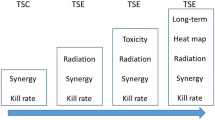
Here we summarize a few tenets and principles of mathematical modeling in radiation oncology. As the intended audience of this review is the clinical radiation oncologist, we omit gratuitous mathematical detail in favor of a more heuristic view, and point the reader to excellent reviews as well as more technical literature for the mathematical details of the models. A schematic overview of mathematical modeling in RT is provided in Fig. 1.
Mathematical models provide a path to precision medicine in radiation oncology through prediction and optimization of response to RT based on an individual patient’s tumor biology. Mathematical models are used to predict cell growth and response to RT, to optimize RT dose, and may also provide biomarkers (metrics) that can be used to identify and predict which patients will respond to a given treatment course
Ultimately, a mathematical model aims to predict response to RT, although the endpoints defining a response may vary from shrinkage in tumor size, to surviving fraction of cells (Powathil et al. 2013; Prokopiou et al. 2015; Rockne et al. 2010), to predictions of overall survival and similar clinical endpoints (Zaw et al. 2014; Baldock et al. 2012). In this section, we survey increasingly complex mathematical models of cellular- and tissue-scale tumor growth and response to RT.
Starting with simple dose-equivalence and dose-response models, the biologically effective dose (BED) and similar concepts date back to the earliest forms of ionizing radiation as a treatment for human maladies. Since then, many mathematical formalisms have been proposed to incorporate additional variables (e.g., cell proliferation, DNA damage, repair, and ultimately the surviving fraction of cells) into a variety of radiation doses and energies. Mathematically, these models tend to take the form of ordinary differential equations that describe the rate of change of the tumor population with and without the effects of radiation, which is described as a negative rate of change. Tumor doubling time (td), which is nominally incorporated in the basic LQ model, is a simplistic interpretation of these concepts. The concept of tumor control, and tumor control probability (TCP), given by
where N is the number of tumor cells, and SF is the surviving fraction, can be used as a simple measure to evaluate the success of a given treatment protocol. Several different formalisms for evaluating TCP have been proposed, which vary in complexity (Gong et al. 2013).
2.1 Tumor Growth Laws
Tumor cell growth laws often come in variations of a few archetypes: exponential growth, volume-limited logistic growth, or growth rate-limited Gompertzian growth. One or more of these growth models are then paired with mathematical models of response to RT, often based on the LQ model; this subject is thoroughly reviewed with mathematical details by Enderling et al. (2010) and O’Rourke et al. (2009). However, it is debated whether the LQ model is appropriate to describe biological responses to high dose per fraction treatments such as radiosurgery, which can involve doses of up to 20 Gy in a single fraction (Kirkpatrick et al. 2009). As a result, more complex mathematical models have been proposed to account for potentially different biological effects of high dose RT, which include mechanisms of DNA damage and repair kinetics (Siam et al. 2016; Tariq et al. 2015; Watanabe et al. 2016).
2.2 More Complex Multiscale Models
Mathematical models can also include multiple scales in space and time. Models that include cell motility, surrounding tissues, and spatial variations in radiation dose, for example, often take the form of partial differential equations (Stamatakos et al. 2006; Ribba et al. 2006; Powathil et al. 2007) or agent-based models (Scott et al. 2016). These spatial models may include biophysical forces between the tumor and the surrounding tissue, which may influence cell response to radiation-induced damage (Angeli and Stylianopoulos 2016). In addition, environmental factors that influence response to RT can be included in mathematical models. For example, hypoxia, or lack of oxygen, mediates production of DNA-damaging oxygen free radical species in response to radiation. Thus, changes in the spatial and temporal distribution of hypoxia within the tissue can affect cell kill. A number of groups have incorporated hypoxia into both tumor growth and response to RT models (Scott et al. 2016; Malinen et al. 2006; Titz and Jeraj 2008; Jeong et al. 2013; Rockne et al. 2015).
2.3 Pros and Cons of Model Complexity
Although a variety of mathematical models of tumor growth and response to RT exist, a philosophical argument must be considered regarding model complexity and the ability of the model to be parameterized, and to reasonably provide predictive value. In this way, the number of parameters, often a measure of a model’s complexity, is weighed relative to the biological assumptions in the model. For instance, models that include environmental factors such as hypoxia tend to be more complex, and involve more equations, more parameters, and more specific assumptions. In contrast, simpler models often involve fewer, but broader, assumptions, and also fewer parameters. Such models can more easily be adapted to individual patient data to make patient-specific models and predictions.
Considering the spectrum of model complexity, along with ease-of-use, and evaluating potential utility in the clinical setting, is a challenge for several reasons. One reason is that complex models are difficult to communicate to non-mathematicians, and are difficult to interpret, even by the mathematicians who craft them. An additional concern is that metrics used for decision-making derived from complex models may be sensitive to small changes in the model’s parameters, making the decision-making less robust to variations seen in real data. Finally, more complicated models are not necessarily more effective, as many complicated models make predictions similar to simple models, as shown by Gong et al. (2013).
Simple models, on the other hand, may not include mechanisms or biological detail satisfying to a biologist or clinician, and may miss important features that determine optimal treatment planning, but have the value of being relatively clear to communicate. This highlights just some of the hurdles that support the earlier contention that, even with the ongoing effort in the field, definitive studies on the use of these more complex mathematical models that customize RT to the patient and the patient’s disease will most likely not be completed within five years.
3 Personalized Models
Patient-specific mathematical models provide one means of approaching the ultimate goal of precision medicine: to tailor the treatment to the individual patient’s disease. Baldock et al. provide a roadmap for translating patient-specific models into precision medicine (Baldock et al. 2013), and describe the application of mathematical models to address a variety of clinical questions, such as prediction of surgical outcomes and response to RT. These applications of patient-specific mathematical modeling are connected to the goals of precision medicine, in that biological characteristics of each patient’s disease are incorporated into a tailor-made mathematical model that can provide predictions of response for that individual patient. These predictions can then be used to both better select patients for clinical trials of novel approaches and define cases in which treatment can be rationally modified. In settings with a high cure rate, such as head and neck sarcoma, conventional RT approaches with mathematical models may have a limited value. However, in settings in which the response rate is low or highly variable, personalized mathematical models may provide a means to select patients for a clinical trial, or perhaps modify the treatment plan.
Several methods have been proposed to personalize mathematical models for individual patients. The most common approach is to fit a model to patient data by adjusting parameters in a fixed model. This can be done through a variety of methods, with Bayesian inference (Hawkins-Daarud et al. 2013; Tariq et al. 2016) and model-data fitting procedures (Rockne et al. 2010; Hathout et al. 2015a; Colombo et al. 2015) being two of the most prevalent methods in recent years. For model-fitting algorithms, the most common forms of input are tumor volume and shape characteristics obtained from magnetic resonance imaging (MRI) (Rockne et al. 2010; Neal et al. 2013; Hathout et al. 2015b), positron emission tomography (PET) (Rockne et al. 2015; Mz et al. 2013), or computed tomography (CT) (Prokopiou et al. 2015; Belfatto et al. 2015). These approaches estimate parameters in the model(s) that correspond to biological characteristics of the tumor, such as cell doubling time, proliferation rate, and rate of migration into the surrounding tissue.
3.1 Proliferation Saturation Index
Prokopiou et al. (2015) have derived a proliferation saturation index (PSI) from a model of tumor cell growth and response to RT with a simple logistic growth law, given by
where PSI is the tumor volume-to-carrying capacity ratio (V/K). Radiation response is determined by the LQ model and is given by
The authors provide a novel perspective on the famous logistic growth equation by using the PSI as a predictive variable for RT response. The patient-specific parameter, PSI, is estimated using regression to fit the logistic growth equation, using data derived from two pre-treatment CT scans. The authors show that PSI correlates with RT response, defined by the post-treatment CT scan, and use their model to simulate different treatment and fractionation schemes that show improved response and tumor control for the individual patient.
3.2 Estimating Radiobiological Parameters
A popular formalism for modeling tumor proliferation, migration, and response to RT takes the form of a partial differential equation to incorporate spatial and temporal variations in the tumor growth, radiation delivery, and radiation response. Although many other models have been proposed, the following model for glioblastoma response to RT provides a means to estimate the LQ radiobiological parameters for individual patients using tumor volume data before and after treatment (Rockne et al. 2009, 2010). The model is given by
where the tumor cell density (c(x, t)) is a function of space (x) and time (t), and its rate of change is determined by random Brownian motion in the form of diffusion, with migration rate Φ, and logistic growth with proliferation rate ρ. The parameters of this model can be estimated using serial MRI data prior to treatment (Rockne et al. 2010). The delivery and response to RT is given by the term R(c, t, D), where D is the dose of radiation, and the instantaneous rate of cell kill from radiation is given by (1 − SF), where SF is the surviving fraction determined by the LQ model, as follows:
Holding the α/β ratio constant, this model may be fitted to tumor volume data to obtain patient-specific estimates of radiation sensitivity, quantified by the LQ parameter α, as we have shown in Rockne et al. (2010). Moreover, a positive correlation is found between the tumor proliferation rate and radiation sensitivity. This correlation provides a prediction of response to RT, since the proliferation rate is calculated with pre-treatment imaging data. This approach enables patient-specific simulations of alternate RT plans that use response to conventional treatment as a reference. Although approaches for estimating patient-specific radiobiological parameters from imaging data have been criticized for being ill-posed (Chvetsov et al. 2015), the technique is formally no different than a parameter estimation algorithm. In this case, the patient-specific radiobiological parameter α may be used to identify patients likely to respond to RT and that may also be validated in observational studies, used in optimization algorithms, and used to select patients for clinical trials, all of which can potentially lead to advances in patient outcome.
4 Treatment Optimization
A logical extension of personalized models of tumor growth and response to RT is optimization of treatment for the patient. Model-based biomarkers may be included along with dose constraints as inputs to algorithms that can maximize response while minimizing dose to normal tissue. Despite the development of patient-specific cell lines and preclinical animal studies, translating in vitro cell survival curves parameterized by the LQ or other mathematical models into optimized RT for individual patients remains problematic. To overcome this, recent literature in radiation treatment optimization has focused on themes of optimizing radiation dose distributions, biological response, and target volume delineation.
4.1 Spatial Dose and Fractionation Optimization
In order to optimize radiation dose, in addition to existing clinical treatment planning which conforms the dose to the target volume, organs at risk (OARs) are identified, and dose to normal tissue is constrained. These spatial optimizations are incremental advances over the routine conformal or intensity-modulated radiation therapy (IMRT) practices currently standard in clinical radiation oncology. Multi-objective evolutionary algorithms (MOEAs) take OARs and normal tissue doses as constraints into the clinical problem of dosimetry, while also maximizing TCP to the target volume (Holdsworth et al. 2010; Kim et al. 2012). These algorithms can also include objectives to be maximized, such as tumor size or cell kill (Corwin et al. 2013). Groups have already demonstrated the feasibility of implementing spatial optimization of dose using multi-objective evolutionary algorithm methods into a clinical workflow (Kim et al. 2015; Smith et al. 2016). The incorporation of patient-specific tumor growth and response models into this paradigm is a reasonable goal.
The temporal optimization of RT through fractionation attempts to minimize normal tissue complications and incorporate cell repair from radiation damage into the mathematical models. Fractionation schemes are often compared with dose equivalence calculations that are typically based upon the LQ model (Holloway and Dale 2013). In addition to BED- and LQ-based calculations of dose equivalence, tumor growth models can be incorporated into optimization algorithms that explicitly model changes in tumor volume. This enables adaptive fractionation schemes that are tailored to the response of the tumor (Unkelbach et al. 2014b) or that include dose to multiple normal tissues (Saberian et al. 2016). Badri et al. (2015) have taken this approach to apply a mathematical optimization for glioblastoma and demonstrate improved tumor control after mathematical model-predicted improved response to an alternative treatment regime in which the treatment fractions were temporally optimized to minimize toxicity to early and late responding normal tissues. The treatment plans suggested by Badri et al. were also constrained by the 8 a.m.–5 p.m. clinical workday, to provide a practical dosing schedule that could be performed in the clinic.
4.2 Tumor Biology Optimization
Perhaps an obvious goal of RT optimization is to maximize tumor cell kill (Zaider and Hanin 2011). In order to tailor optimized RT treatment plans to the biology of the individual patient’s tumor, whether that be a genomically adjusted dose as suggested by Alomari et al. (2014), or dynamic biologically conformal radiation therapy (DBCRT) (Kim et al. 2012), one must identify appropriate biological targets. A systems oncology perspective incorporates multiple scales of tumor biology, including proliferation rate, cell signaling, DNA damage repair rate, and organ-level responses as biological targets for optimization (Powathil et al. 2015). Cell phenotypes within the tumor, such as cancer stem cells, and their associated differential responses to RT have also been incorporated into mathematical models and used as biological endpoints for optimization (Leder et al. 2014; Gao et al. 2013).
4.3 Target Volume Delineation
CT imaging is used for dose planning and target volume delineation. However, many cancers are locally invasive, and a portion of the cells beyond the frank lesion are not identified on imaging. This is a particular challenge in glioblastoma, a highly invasive primary brain tumor. In this setting, mathematical models have been used to predict tumor cell invasion not visible with CT or MRI, and have thus improved target delineation (Unkelbach et al. 2014a; Hathout et al. 2016) by including this invisible portion of disease. Mathematical models have also been proposed to adjust target volumes, based on hypoxia predicted within and around the tumor by models and/or inferred from PET imaging (Rockne et al. 2015; Moghaddasi et al. 2016).
4.4 Patient-Specific Optimization
The penultimate optimization is a combination of each of the previously described aspects of RT endpoints—spatial dose distribution, temporal fractionation, normal tissue toxicity, tumor biology, and target volume delineation—on a patient-specific basis. Only a few groups have achieved this penultimate combination of mathematical modeling that incorporates tumor growth rates derived from individual patient’s clinical data and adapted to exploit tumor response and treatment. For example, our own work (Rockne) leverages multi-objective optimization, tumor growth and response models, and personalization of model parameters. We use these criteria to suggest, and test, optimal treatment plans for individual patients, and then compare these plans to the standard of care using mathematical model simulations (Corwin et al. 2013). This work demonstrates an improved therapeutic ratio and tumor burden (volume) reduction compared to conventional 2 Gy/day treatment plans. Although these results are purely in silico, they give hope for the continued pursuit of mathematical models to reach the ultimate goal of personalized medicine. In order to translate these studies into patients, the model must be tested in animal systems and in observational clinical trials.
5 Future Directions
Most of the mathematical approaches described in this chapter are focused on the cell and tissue level, with some multi-scale models. An enormous literature in the systems biology field applies mathematical modeling to describe subcellular processes, including cell signaling (McMahon et al. 2013) and DNA repair kinetics (Carlson et al. 2008). Indeed, Craft argues that a more comprehensive, multiscale (subcellular, cell, and tissue level) understanding of radiation response is needed to fully optimize and personalize RT (Kim et al. 2016).
5.1 Combination Therapy and Novel Radiotherapies
The synergy of combining RT with novel therapies, particularly anti-angiogenic therapies, which may impact the tumor microenvironmental variables of hypoxia and blood perfusion, has shown mixed effects in patients. Mathematical models provide a means to interrogate and characterize the hypothetical subset of patients that may benefit from the combination therapy (Hawkins-Daarud et al. 2015). Mathematical models incorporating tumor growth and normal tissue toxicity-related side effects also predict patients that could most benefit from novel RT modalities, such as proton irradiation (Langendijk et al. 2013), particularly for “kill painting” of dose in hypoxic tumors (Tinganelli et al. 2015).
Mathematical models also show promise as tools to investigate the potential roles of phenomena that may be difficult to quantify in a clinical setting, such as the bystander and abscopal effects, in which cells in tissues not directly exposed to ionizing radiation demonstrate behaviours similar to cells that are directly irradiated (Powathil et al. 2016; Poleszczuk et al. 2016). In these cases, mathematical models and simulations can provide novel hypotheses and insights that could be investigated in controlled settings. In this way, models may also provide a bridge between preclinical studies and clinical observations, by providing a mechanistic and general explanation for observations.
5.2 Computational Trials
Mathematical models have also been used to perform “computational trials” which interrogate the impact that varying biological parameters may have in determining outcomes for a given treatment regimen (Raman et al. 2016). In particular, Raman et al. use a mathematical model of glioblastoma growth and response to treatment to quantify motility phenotypes, patterns of progression, and treatment scenarios for various in silico patients that are hypothetically treated. This “phase i” style computational trial—a phrase coined by Jacob G. Scott in the Lancet in 2012 (Scott 2012)—offers a potential application for mathematical models to optimize the efficiency of RT-based clinical trials before they even begin.
5.3 Testing Mathematical Model-Based Biomarkers in Clinical Trials
Although we are not aware of any ongoing prospective clinical studies predicated on mathematical models other than the LQ model (Jones and Dale 2000), these applications are on the horizon. For mathematical models to truly make inroads toward clinical adaptation, a convincing demonstration of the model’s utility is needed. Ultimately, there are two ways mathematical models in RT can enhance patient outcomes, the direct and the indirect. The direct means is the simplest to test. A select subset of patients who are eligible for RT in some setting (alone or in combination) are randomized to standard RT planning versus RT planning guided by the addition of a new mathematical model that likely incorporates individual patient and tumor differences obtained from a variety of pre-treatment assessments, and may suggest changes during RT as well. Successful demonstration of utility would be based on outcomes such as response, local disease-free survival, progression-free survival, or overall survival, with the latter being more convincing. If patient benefit is associated with the use of a mathematical model, this would be the clearest and most direct demonstration of the utility of a new mathematical approach. There are, however, other ways in which mathematical models can demonstrate clinical utility. These indirect methods include (1) enhancing our understanding of biology through testing mathematical models that capture our current understanding, and (2) providing a risk stratification of patients. For the latter, there is a large literature on the use of risk scoring and nomograms to help select patients for more aggressive therapy, or to qualify for a clinical trial. These mathematical models can be used in such a scoring system to help characterize patient responsiveness to the standard of care RT-based therapy. This type of biomarker development and use is established by both retrospective and prospective studies, and can lead to innovative prospective studies such as the TAILORx study (clinicaltrials.gov identifier NCT00310180), a Trial Assigning IndividuaLized Options for treatment (Rx).
6 Summary
Mathematical modeling has played an important role in radiation biology and physics for decades. Similarly, mathematical models have been used to study tumor growth and response to cancer treatments for over a century. Recent advancements in mathematical models have brought these fields together to optimize and improve RT. As summarized in this chapter, models that allow for personalization of tumor growth and response predictions, along with methods to incorporate novel approaches into radiation treatment optimization algorithms, have advanced the role and increased the value of mathematical modeling in clinical radiation oncology. Indeed, as predictive models allow us to to tailor treatments to the individual patient’s disease, and provide model-derived biomarkers that may be tested in clinical trials, we move closer to the goal of precision medicine. In radiation oncology, this means not only tailoring the dose to the boundaries of the tumor, but also to the unique biology and stage of the patient’s disease. Thus, we believe that mathematical modeling will continue to be a critical element that enables the goal of designing the majority of RT schedules using spatiotemporal optimization “within the next five years …” (2016) (Kim et al. 2016).
Abbreviations
- BED:
-
Biologically equivalent dose
- CT:
-
Computed tomography
- DBCRT:
-
Dynamic biologically conformal radiation therapy
- IMRT:
-
Intensity modulated radiation therapy
- LQ:
-
Linear-quadratic
- MOEA:
-
Multi-objective evolutionary algorithm
- MRI:
-
Magnetic resonance imaging
- OAR:
-
Organ at risk
- PET:
-
Positron emission tomography
- RT:
-
Radiation therapy
- SF:
-
Surviving fraction
- TCP:
-
Tumor control probability
References
Alomari A, Rauch PJ, Orsaria M, Minja FJ, Chiang VL, Vortmeyer AO (2014) Radiologic and histologic consequences of radiosurgery for brain tumors. J Neurooncol [Internet] 117(1):33–42, March 2014. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24442402
Angeli S, Stylianopoulos T (2016) Biphasic modeling of brain tumor biomechanics and response to radiation treatment. J Biomech [Internet] 49(9):1524–1531. Elsevier. Available from: http://dx.doi.org/10.1016/j.jbiomech.2016.03.029
Badri H, Pitter K, Holland EC, Michor F, Leder K (2015) Optimization of radiation dosing schedules for proneural glioblastoma. J Math Biol [Internet]. Springer, Berlin, Heidelberg. Available from: http://springerlink.bibliotecabuap.elogim.com/10.1007/s00285-015-0908-x
Baldock AL, Anh S, Rockne R, Neal M, Clark-Swanson K, Sterin G et al (2012) Patient-specific invasiveness metric predicts benefit of resection in human gliomas. Neuro Oncol [Internet] 14:131. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4211670/
Baldock AL, Rockne RC, Boone AD, Neal ML, Hawkins-Daarud A, Corwin DM et al (2013) From patient-specific mathematical neuro-oncology to precision medicine. Front Oncol [Internet] 3:62, 2013/04/09 ed. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23565501
Belfatto A, Riboldi M, Ciardo D, Cecconi A, Lazzari R, Jereczek-Fossa B et al (2015) Adaptive mathematical model of tumor response to radiotherapy based on CBCT data. IEEE J Biomed Heal Informatics [Internet] 2194(c):1–1. Available from: http://ieeexplore.ieee.org/lpdocs/epic03/wrapper.htm?arnumber=7153523
Brenner DJ, Hlatky LR, Hahnfeldt PJ, Huang Y, Sachs RK (1998) The linear-quadratic model and most other common radiobiological models result in similar predictions of time-dose relationships. Radiat Res [Internet] 150(1):83–91. Available from: http://www.ncbi.nlm.nih.gov/pubmed/9650605
Carlson DJ, Stewart RD, Semenenko VA, Sandison GA (2008) Combined use of Monte Carlo DNA damage simulations and deterministic repair models to examine putative mechanisms of cell killing. Radiat Res [Internet] 169(4):447–459, 2008/03/28 ed. Available from: http://www.ncbi.nlm.nih.gov/pubmed/18363426
Chvetsov AV, Sandison GA, Schwartz JL, Rengan R (2015) Ill-posed problem and regularization in reconstruction of radiobiological parameters from serial tumor imaging data. Phys Med Biol [Internet] 60(21):8491–8503. IOP Publishing
Colombo MC, Giverso C, Faggiano E, Boffano C, Acerbi F, Ciarletta P (2015) Towards the personalized treatment of glioblastoma: integrating patient-specific clinical data in a continuous mechanical model. PLoS One [Internet] 10(7):e0132887. Available from: http://dx.plos.org/10.1371/journal.pone.0132887
Corwin D, Holdsworth C, Rockne RC, Trister AD, Mrugala MM, Rockhill JK et al (2013) Toward patient-specific, biologically optimized radiation therapy plans for the treatment of glioblastoma. PLoS One [Internet] 8(11):e79115, Jan 2013 [cited 22 Nov 2014]. Available from: http://www.pubmedcentral.nih.gov/pubmed/3827144
Dale RG, Jones B (2007) British Institute of Radiology. Radiobiological modelling in radiation oncology. British Institute of Radiology, 292 p
Enderling H, Chaplain MA, Hahnfeldt P (2010) Quantitative modeling of tumor dynamics and radiotherapy. Acta Biotheor [Internet] 58(4):341–353. Available from: http://www.ncbi.nlm.nih.gov/pubmed/20658170
Fowler JF (2006) Development of radiobiology for oncology-a personal view. Phys Med Biol [Internet] 51(13):R263–R286, 7 July 2006. Available from: http://www.ncbi.nlm.nih.gov/pubmed/16790907
Gallasch R, Efremova M, Charoentong P, Hackl H, Trajanoski Z (2013) Mathematical models for translational and clinical oncology. J Clin Bioinf [Internet] 3(1):23. BioMed Central Ltd, 7 Jan 2013. Available from: http://www.jclinbioinformatics.com/content/3/1/23
Gao X, McDonald JT, Hlatky L, Enderling H (2013) Acute and fractionated irradiation differentially modulate glioma stem cell division kinetics. Cancer Res [Internet]. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23269274
Gong J, Dos Santos MM, Finlay C, Hillen T (2013) Are more complicated tumour control probability models better? Math Med Biol 30:1–19
Hall EJ, Giaccia AJ (2011) Radiobiology for the radiologist [Internet], 7th edn. Lippincott Williams & Wilkins, Philadelphia, ix, 546 p. Available from: http://www.loc.gov/catdir/toc/ecip063/2005031128.html
Hathout L, Ellingson B, Cloughesy T, Pope W (2015a) Patient-specific characterization of the invasiveness and proliferation of low-grade gliomas using serial MR imaging and a mathematical model of tumor growth. Oncol Rep [Internet] 2883–2888. Available from: http://www.spandidos-publications.com/10.3892/or.2015.3926
Hathout L, Pope WB, Lai A, Nghiemphu PL, Cloughesy TF, Ellingson BM (2015b) Radial expansion rates and tumor growth kinetics predict malignant transformation in contrast-enhancing low-grade diffuse astrocytoma. CNS Oncol 4:247–256
Hathout L, Patel V, Wen P (2016) A 3-dimensional DTI MRI-based model of GBM growth and response to radiation therapy. Int J Oncol [Internet] 1–7. Available from: http://www.spandidos-publications.com/10.3892/ijo.2016.3595
Hawkins-Daarud A, Prudhomme S, van der Zee KG, Oden JT (2013) Bayesian calibration, validation, and uncertainty quantification of diffuse interface models of tumor growth. J Math Biol 67(6–7):1457–1485
Hawkins-Daarud AJ, Rockne RC, Corwin D, Anderson AR, Kinahan PE, Swanson KR (2015) In silico analysis suggests differential response to bevacizumab and radiation combination therapy in newly diagnosed glioblastoma. J R Soc Interface [Internet] 12(20150388). Available from: http://dx.doi.org/10.1098/rsif.2015.0388
Holdsworth C, Kim M, Liao J, Phillips MH (2010) A hierarchical evolutionary algorithm for multiobjective optimization in IMRT. Med Phys [Internet] 37(9):4986–4997. Available from: http://www.ncbi.nlm.nih.gov/pubmed/20964218
Holloway RP, Dale RG (2013) Theoretical implications of incorporating relative biological effectiveness into radiobiological equivalence relationships. Br J Radiol [Internet] 86(1022):20120417, 2013/02/07 ed. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23385996
Jackson T, Komarova N, Swanson K (2014) Mathematical oncology: using mathematics to enable cancer discoveries. Am Math Mon 121(November):1–17
Jeong J, Shoghi KI, Deasy JO (2013) Modelling the interplay between hypoxia and proliferation in radiotherapy tumour response. Phys Med Biol [Internet] 58(14):4897–4919, 21 July 2013. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23787766
Jones B, Dale RG (2000) Radiobiological modeling and clinical trials. Int J Radiat Oncol Biol Phys 48(1):259–265
Kim M, Ghate A, Phillips MH (2012) A stochastic control formalism for dynamic biologically conformal radiation therapy. Eur J Oper Res [Internet] 219(3):541–556. Elsevier B.V. Available from: http://dx.doi.org/10.1016/j.ejor.2011.10.039
Kim M, Stewart RD, Phillips MH (2015) A feasibility study: Selection of a personalized radiotherapy fractionation schedule using spatiotemporal optimization. Med Phys [Internet] 42(11):6671–6678. Available from: http://scitation.aip.org/content/aapm/journal/medphys/42/11/10.1118/1.4934369
Kim M, Craft DL, Orton CG (2016) Within the next five years, most radiotherapy treatment schedules will be designed using spatiotemporal optimization. Med Phys [Internet] 43(5):2009–2012. Available from: http://scitation.aip.org/content/aapm/journal/medphys/43/5/10.1118/1.4943383
Kirkpatrick JP, Brenner DJ, Orton CG (2009) Point/Counterpoint. The linear-quadratic model is inappropriate to model high dose per fraction effects in radiosurgery. Med Phys [Internet] 36(8):3381–3384, 2009/09/15 ed. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19746770
Langendijk JA, Lambin P, De Ruysscher D, Widder J, Bos M, Verheij M (2013) Selection of patients for radiotherapy with protons aiming at reduction of side effects: the model-based approach. Radiother Oncol [Internet] 107(3):267–273, July 2013. Elsevier Ireland Ltd. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23759662
Leder K, Pitter K, Laplant Q, Hambardzumyan D, Ross BD, Chan TA et al (2014) Mathematical modeling of PDGF-driven glioblastoma reveals optimized radiation dosing schedules. Cell [Internet] 156(3):603–616, 30 Jan 2014. Elsevier. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24485463
Malinen E, Søvik A, Hristov D, Bruland ØS, Olsen DR (2006) Adapting radiotherapy to hypoxic tumours. Phys Med Biol [Internet] 51(19):4903–4921, 7 Oct 2006. Available from: http://www.ncbi.nlm.nih.gov/pubmed/16985278
McMahon SJ, Butterworth KT, Trainor C, McGarry CK, O’Sullivan JM, Schettino G et al (2013) A kinetic-based model of radiation-induced intercellular signalling. PLoS ONE 8(1):15–18
Michor F, Beal K (2015) Improving cancer treatment via mathematical modeling: surmounting the challenges is worth the effort. Cell [Internet] 163(5):1059–1063. Elsevier Inc. Available from: http://dx.doi.org/10.1016/j.cell.2015.11.002
Moghaddasi L, Bezak E, Harriss-Phillips W (2016) Monte-Carlo model development for evaluation of current clinical target volume definition for heterogeneous and hypoxic glioblastoma. Phys Med Biol [Internet] 61(9):3407–3426. IOP Publishing
Mz H, Petitjean C, Ruan S, Vera P, Dubra B (2013) Predicting lung tumor evolution during radiotherapy from PET images using a patient specific model. IEEE 10th international symposium on biomedical imaging: from nano to macro, San Francisco, CA, pp 1404–1407
Neal ML, Trister AD, Ahn S, Baldock A, Bridge CA, Guyman L et al (2013) Response classification based on a minimal model of glioblastoma growth is prognostic for clinical outcomes and distinguishes progression from pseudoprogression. Cancer Res [Internet] 73(10):2976–2986, 2013/02/13 ed., 15 May 2013. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23400596
O’Rourke SFC, McAneney H, Hillen T (2009) Linear quadratic and tumour control probability modelling in external beam radiotherapy. J Math Biol 58(4–5):799–817
Poleszczuk JT, Luddy KA, Prokopiou S, Robertson-Tessi M, Moros EG, Fishman M et al (2016) Abscopal benefits of localized radiotherapy depend on activated T-cell trafficking and distribution between metastatic lesions. Cancer Res 76(5):1009–1018
Powathil G, Kohandel M, Sivaloganathan S, Oza A, Milosevic M (2007) Mathematical modeling of brain tumors: effects of radiotherapy and chemotherapy. Phys Med Biol [Internet] 52(11):3291–3306. Available from: http://www.ncbi.nlm.nih.gov/pubmed/17505103
Powathil GG, Adamson DJA, Chaplain MAJ (2013) Towards predicting the response of a solid tumour to chemotherapy and radiotherapy treatments: clinical insights from a computational model. PLoS Comput Biol 9(7)
Powathil GG, Swat M, Chaplain MAJ (2015) Systems oncology: towards patient-specific treatment regimes informed by multiscale mathematical modelling. Semin Cancer Biol [Internet] 30C:13–20, Feb 2015. Elsevier Ltd. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24607841
Powathil GG, Munro AJ, Chaplain MAJ, Swat M (2016) Bystander effects and their implications for clinical radiation therapy: insights from multiscale in silico experiments. J Theor Biol [Internet] 401:1–14. Elsevier. Available from: http://dx.doi.org/10.1016/j.jtbi.2016.04.010
Prokopiou S, Moros EG, Poleszczuk J, Caudell J, Torres-Roca JF, Latifi K et al (2015) A proliferation saturation index to predict radiation response and personalize radiotherapy fractionation. Radiat Oncol [Internet] 10(1):159. Available from: http://www.ro-journal.com/content/10/1/159
Raman F, Scribner E, Saut O, Wenger C, Colin T, Fathallah-Shaykh HM (2016) Computational trials: unraveling motility phenotypes, progression patterns, and treatment options for glioblastoma multiforme. PLoS One [Internet] 11(1):e0146617. Available from: http://dx.plos.org/10.1371/journal.pone.0146617
Ribba B, Colin T, Schnell S (2006) A multiscale mathematical model of cancer, and its use in analyzing irradiation therapies. Theor Biol Med Mod 3(7)
Rockne R, Alvord EC, Rockhill JK, Swanson KR, Alvord Jr EC, Rockhill JK et al (2009) A mathematical model for brain tumor response to radiation therapy. J Math Biol [Internet] 58(4–5):561–578, April 2009. Available from: http://www.ncbi.nlm.nih.gov/pubmed/18815786
Rockne R, Rockhill JK, Mrugala M, Spence AM, Kalet I, Hendrickson K et al (2010) Predicting efficacy of radiotherapy in individual glioblastoma patients in vivo: a mathematical modeling approach. Phys Med Biol [Internet] 55(12):3271–3285. Available from: http://www.ncbi.nlm.nih.gov/pubmed/20484781
Rockne RC, Trister AD, Jacobs J, Hawkins-daarud AJ, Neal ML, Hendrickson K et al (2015) A patient-specific computational model of hypoxia-modulated radiation resistance in glioblastoma using 18F-FMISO-PET. J R Soc Interface [Internet] 12. Available from: http://classic.rsif.royalsocietypublishing.org/content/12/103/20141174.short
Saberian F, Ghate A, Kim M (2016) Optimal fractionation in radiotherapy with multiple normal tissues. Math Med Biol 33:211–252
Scott J (2012) Phase i trialist. Lancet Oncol [Internet] 13(3):236, March 2012. Elsevier. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22489289
Scott JG, Fletcher AG, Anderson ARA, Maini PK (2016) Spatial metrics of tumour vascular organisation predict radiation efficacy in a computational model. PLoS Comput Biol 12(1):1–24
Siam FM, Grinfeld M, Bahar A, Rahman HA, Ahmad H, Johar F (2016) A mechanistic model of high dose irradiation damage. Math Comput Simul [Internet]. Elsevier B.V. Available from: http://linkinghub.elsevier.com/retrieve/pii/S0378475416000562
Smith WP, Kim M, Holdsworth C, Liao J, Phillips MH (2016) Personalized treatment planning with a model of radiation therapy outcomes for use in multiobjective optimization of IMRT plans for prostate cancer. Radiat Oncol [Internet] 11(1):38. Available from: http://ro-journal.biomedcentral.com/articles/10.1186/s13014-016-0609-7
Stamatakos GS, Antipas VP, Uzunoglu NK, Dale RG (2006) A four-dimensional computer simulation model of the in vivo response to radiotherapy of glioblastoma multiforme: studies on the effect of clonogenic cell density. Brit J Radiol 79:389–400
Tariq I, Humbert-Vidan L, Chen T, South CP, Ezhil V, Kirkby NF et al (2015) Mathematical modelling of tumour volume dynamics in response to stereotactic ablative radiotherapy for non-small cell lung cancer. Phys Med Biol [Internet] 60(9):3695–3713. Available from: http://iopscience.iop.org/0031-9155/60/9/3695/
Tariq I, Chen T, Kirkby NF, Jena R (2016) Modelling and Bayesian adaptive prediction of individual patients’ tumour volume change during radiotherapy. Phys Med Biol [Internet] 61(5):2145–2161. IOP Publishing. Available from: http://stacks.iop.org/0031-9155/61/i=5/a=2145?key=crossref.511fc11bdea8efaa5a2bdcb3669ad645
Tinganelli W, Durante M, Hirayama R, Krämer M, Maier A, Kraft-Weyrather W et al (2015) Kill-painting of hypoxic tumours in charged particle therapy. Sci Rep [Internet] 5:17016. Nature Publishing Group. Available from: http://www.nature.com/articles/srep17016
Titz B, Jeraj R (2008) An imaging-based tumour growth and treatment response model: investigating the effect of tumour oxygenation on radiation therapy response. Phys Med Biol [Internet] 53(17):4471–4488, 7 Sept 2008. Available from: http://www.pubmedcentral.nih.gov/pubmed/2819145
Unkelbach J, Menze B, Konukoglu E, Dittmann F, Ayache B, Shih H (2014a) Radiotherapy Planning for Glioblastoma Based on a Tumor Growth Model: improving Target Volume Delineation. Phys Med Biol 59(3):771–789
Unkelbach J, Craft D, Hong T, Papp D, Ramakrishnan J, Salari E et al (2014b) Exploiting tumor shrinkage through temporal optimization of radiotherapy. Phys Med Biol [Internet] 59(12):3059–79, 21 June 2014. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24839901
Watanabe Y, Dahlman EL, Leder KZ, Hui SK (2016) A mathematical model of tumor growth and its response to single irradiation. Theor Biol Med Model [Internet] 13(1):6. Available from: http://www.tbiomed.com/content/13/1/6
Yankeelov TE, Atuegwu N, Hormuth D, Weis JA, Barnes SL, Miga MI et al (2013) Clinically relevant modeling of tumor growth and treatment response. Sci Transl Med [Internet] 5(187):187ps9, 2013/05/31 ed. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23720579
Zaider M, Hanin L (2011) Tumor control probability in radiation treatment. Med Phys [Internet] 38(2):574 [cited 14 Jan 2015]. Available from: http://scitation.aip.org/content/aapm/journal/medphys/38/2/10.1118/1.3521406
Zaw TM, Pope WB, Cloughesy TF, Lai A, Nghiemphu PL, Ellingson BM (2014) Short-interval estimation of proliferation rate using serial diffusion MRI predicts progression-free survival in newly diagnosed glioblastoma treated with radiochemotherapy. J Neurooncol [Internet] 116(3):601–608, Feb 2014. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24395348
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
Rockne, R.C., Frankel, P. (2017). Mathematical Modeling in Radiation Oncology. In: Wong, J., Schultheiss, T., Radany, E. (eds) Advances in Radiation Oncology. Cancer Treatment and Research. Springer, Cham. https://doi.org/10.1007/978-3-319-53235-6_12
Download citation
DOI: https://doi.org/10.1007/978-3-319-53235-6_12
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-53233-2
Online ISBN: 978-3-319-53235-6
eBook Packages: MedicineMedicine (R0)