Abstract
Biliary diseases represent an important group of inborn and acquired diseases of the intra- and extrahepatic bile ducts with severe morbidity and mortality due to the development of biliary type of liver fibrosis, liver cirrhosis, and eventually cholangiocarcinoma [1]. The spectrum of cholangiopathies is heterogeneous with respect to underlying mechanisms, clinical course, and presentation. However, these liver diseases share a common target: the cholangiocyte. These diseases include immune-mediated, idiopathic cholangiopathies, such as primary biliary cholangitis (previously known as primary biliary cirrhosis) and primary sclerosing cholangitis, biliary atresia, as well as graft-versus-host disease. The difficulties in studying the complex nature of cholangiocyte injury in humans as well as the currently limited treatment options stress the need for reliable, well-defined, and reproducible animal models in order to gain insights into the pathophysiology and to test novel therapies. The aim of this chapter is to critically discuss the characteristics and limitations of rodent models of biliary diseases for primary biliary cholangitis, primary sclerosing cholangitis, biliary atresia, graft-versus-host disease, as well as cholangiocarcinoma.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Animal model
- Biliary atresia
- Biliary type of liver fibrosis cholangiocarcinoma
- Cholangiopathies
- Graft-versus-host disease
- Primary biliary cirrhosis
- Primary sclerosing cholangitis
-
The term biliary disease includes a diverse spectrum of liver diseases, which however share the same primary pathogenetic target: the cholangiocyte.
-
The etiology of biliary diseases is unknown, and the use of rodent models is valuable to understand their pathogenesis as well as for testing new drugs.
-
A major limitation of the use of animal models is the species differences between rodents and humans.
-
Several animal models exhibit comparable characteristics of different biliary diseases.
-
There is no “perfect model” that mirrors human biliary disease characteristics making the task of understanding the underlying pathogenetic mechanisms hard. Various aspects of different models might be required to study particular pathogenetic steps.
4.1 Introduction
Biliary disease represents an umbrella term for numerous complex liver diseases which share the primary pathogenetic target within extra- or intrahepatic bile ducts, including primary biliary cholangitis (PBC) (previously known as primary biliary cirrhosis), primary sclerosing cholangitis (PSC), biliary atresia (BA), graft-versus-host disease (GvHD), and cholangiocarcinoma (CCA). However, they differ significantly in regard to their etiopathogenesis, symptoms and clinical course, liver phenotype, gender predominance, and concomitant diseases [1]. The etiology of these diseases still remains only partly understood, but their pathogenesis has become somehow clearer [1–3].
The main advantages for the use of rodent (especially mouse) models are – compared to other mammalians – low costs, the ability for high-throughput studies, ease of handling and breeding, and the possibility of genetic manipulation in mice. Mouse models enable us also to test new drugs and genetic or surgical manipulation within reasonable time frames because of their low life span [4]. However, despite undoubtedly significant research progress, each animal model still harbors its own and important limitations [4]. Such limitations include substantial species differences between rodents and humans in regard to (1) immune and inflammatory responses [5], (2) hepatic and intestinal nuclear receptor expression [6], (3) bile acid metabolism and pool composition [7], and (4) gut microbiota [8] to name only few. In addition, some models exhibit comparable characteristics of different biliary diseases with underlying shared mechanisms of immune-mediated cholangiocyte injury and biliary type of liver fibrosis, and one specific model may consequently mirror different aspects of several cholangiopathies [9]. However, for clarity reasons we would like to provide the characteristics for each model discussed. Due to limitations of space, we focus exclusively on available mouse models for PBC, PSC, BA, GvHD, and CCA. We would also ask our colleges for pardon, since due to the limitation of references, numerous important publications in this research area could not be cited adequately.
4.2 Primary Biliary Cholangitis (PBC)
The identification of anti-mitochondrial antibodies (AMA) directed against the major mitochondrial antigen pyruvate dehydrogenase complex E2 (PDC-E2) detectable in over 95% of patients leading to consecutive destruction of interlobular bile ducts was a milestone in understanding the autoimmune-mediated nature of PBC [10–12]. Accordingly, PBC represents a classical autoimmune disorder with clear female predominance. Histologically, PBC is characterized by chronic nonsuppurative inflammation with so-called florid duct lesions consisting of epithelioid cell granulomas surrounding small bile ducts eventually progressing to segmental vanishing of bile ducts and ultimately to the biliary type of liver fibrosis and in some patients to liver cirrhosis. Thus, the main attributes of a candidate PBC model include a clear female predominance, presence of AMA in more than 90% and presence of antinuclear antibodies (ANA) in 50–80%, chronic inflammation of small bile ducts with focal duct obliteration and epithelioid cell granuloma formation, chronicity and slow progression of disease with vanishing of bile ducts, biliary type of liver fibrosis with CD4 T cells in liver and hilar lymph nodes, as well as PDC-E2-specific autoreactive CD8 T cells in liver [2].
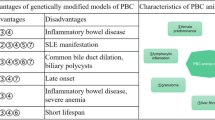
Animal models for PBC can be subdivided into (1) spontaneous models utilizing genetic modification in mice, (2) neonatally thymectomized mice, (3) inducible models with the use of xenobiotics harboring structural similarities to PDC-E2, and (4) infectious-induced PBC-like phenotype. A list of animal models for PBC is given in Table 4.1. Due to limitations of space, we will focus here on genetically modified mice.
4.2.1 dnTGFβRII Mice
Transforming growth factor-beta (TGF-β) has pleiotropic effects on cell growth and immunological control with a promoting effect on the development of the regulatory T-cell compartment [13]. Overexpression of a dominant negative form of the TGF-β promoter leads to development of PBC-like features with lymphoid cell infiltration of portal fields as well as colitis with 100% AMA positivity [14, 15]. The adoptive transfer of CD8+ cells from these animals into immunodeficient Rag1 −/− mice underlined the importance of CD8+ cells, since these mice developed similar histopathology to human PBC; however, CD4+ T-cell transfer had no effect on the liver phenotype but worsened colitis [16]. Further studies with an anti-CD20 antibody in young dnTGFβRII showed complete loss of serum AMA positivity and decreased liver inflammation, but were ineffective when initiated in mice with established disease [17]. A central role for natural killer T (NKT) cells in PBC pathogenesis is supported by the generation of CD1d−/−-dnTGFβRII mice, in which reduced NKT function caused ameliorated inflammation, bile duct damage, mild ductopenia, cholestasis, and biliary fibrosis [18]. IL-12, consisting of a p40 and a p35 subunit, was studied by generating an IL-12p35 −/− and IL-12p40 −/− mouse strain on the dnTGFβRII background [19]. Whereas the IL-12p40 −/−mice were protected from liver inflammation, in IL-12p35 −/− mice, liver inflammation with similar severity but delayed onset compared to the parental dnTGFβRII mice was detected [19]. In addition, the deletion of IL-12p35 subunit from dnTGFβRII mice leads to frequent development of liver fibrosis with numerous immunological and histological features similar to human PBC [19]. To further characterize this interesting and promising mouse model, it will be crucial to study the effect of the different cytokines, including IL-12, -23, and -35 on liver phenotypes and on fibrotic changes via cytokine administration or cytokine-neutralizing antibodies [20].
4.2.2 IL-2Rα−/− Mice
Mice with genetic IL-2 receptor deficiency show 100% AMA positivity, lymphocytic portal inflammation, as well as CD4+ and CD8+ lymphocytes infiltrating the bile duct epithelium of intralobular bile ducts [21]. Interestingly, these animals show concomitant severe intestinal inflammation, which is usually not seen in PBC but PSC patients. No hepatic granuloma formation is seen in this mouse model [21]. In addition, there is no information on serum markers for cholestasis and whether also large bile ducts are involved.
Questioning the role of IL-12 in PBC triggered the generation of double knockouts via crossing IL-2Rα −/− and IL-12p40 −/− mice [22]. IL-2Rα −/− IL-12p40 −/− double-knockout mice show exacerbated autoimmune cholangitis, higher degree of liver fibrosis, and ameliorated colitis compared to IL-2Rα −/− single-knockout mice [22]. For more detailed characterization of cholestasis in this interesting mouse model, serum bile acid and alkaline phosphatase levels are awaited [22]. In addition, it would also be important to know whether IL-2Rα −/− IL-12p-40 −/− mice develop large duct disease.
4.2.3 NOD.c3c4 Mice
The introgression of large genetic intervals on chromosomes 3 and 4 in nonobese diabetic (NOD) mouse strain leads to the development of NOD.c3c4 mice [23, 24]. On histological examination, in a high percentage, eosinophilic infiltration of bile ducts and autoreactivity against the PDC-E2 component are seen. To lower extend destructive cholangitis and granuloma formation can be observed. Whereas these animals show high seropositivity for AMA and ANA (80–90%), unfortunately, we do not have any information on cholestasis parameters of these animals. Intriguingly, extrahepatic bile duct disease is observed in NOD.c3c4 mice – a feature that would better fit to PSC rather than PBC – with development of cystic dilations of bile ducts, partial exfoliation of the biliary epithelium, and dense neutrophil-granulocytic infiltration [23]. The underlying mechanisms, however, for this peculiar phenotype is not clear and deserves detailed time-course studies (e.g., cholangiography or bile duct plastination for better characterization of large duct disease, characterization of the inflammatory infiltrate). The pronounced neutrophil-granulocytic infiltration of bile ducts could be, at least in part, a secondary phenomenon due to dilatation and secondary ascending cholangitis. Consequently bile culture studies should also be of interest. Interestingly however, treatment of NOD.c3c4 mice with a monoclonal antibody directed against CD3 protected these mice from cholangitis [23]. In general, due to the complex morphological changes in NOD.c3c4 mice, this mouse model may serve as a model for different cholangiopathies, including also several important aspects of PSC pathogenesis.
4.2.4 Ae2a,b−/− Mice
The observations that anion exchanger 2 (AE2) is downregulated in the liver and lymphocytes of PBC patients and that ursodeoxycholic acid restores AE2 expression and stimulates biliary bicarbonate secretion partially by activation of hepatic AE2 [25–27] were the trigger to generate Ae2a,b−/− mice. This mouse model shares some immunologic and hepatobiliary features with PBC [28]. Histologically, mild to severe portal inflammation with high interindividual variations in regard to the liver phenotype is observed. In addition, the defective Treg cell function and CD8+ T-cell expansion seen in these mice could be due to the AE2 dysfunction, which seems to be critically involved also in the homeostasis of the immune system. However, so far a detailed characterization of this model in regard to investigation of large ducts and in regard to potential biliary fibrosis has been not performed. One major limitation of the model may lie within the fact that this mouse strain seems to be very difficult to breed (personal communication Juan Medina, Pamplona, Spain).
4.2.5 Scurfy Mice
Scurfy mice with a selective loss of the transcription factor Fox-P3 (forkhead box P3, also known as scurfin) resulting in a functional deficiency of Treg cells show serological and morphological features of immune-mediated cholangitis, including severe bile duct injury [29, 30]. However, serum bile acid and alkaline phosphatase levels are not reported in these mice. Findings in scurfy mice underline the potential importance of Treg cells for the pathogenesis of PBC. One of the major limitations of this model is based on an extremely short life span of these mice of about 4 weeks, which seriously limits their use for longitudinal studies (e.g., disease progress, drug testing).
4.2.6 MRL/lpr Mice
MRL/lpr mice with the lymphoproliferative gene lpr (also known as MRL/MP-lpr/lpr) spontaneously develop severe autoimmune-mediated disorders, such as vasculitis, glomerulonephritis, inflammation of salivary glands, interstitial pneumonia and plasma-cellular infiltration of portal fields with biliary injury, and development of AMA [31]. The relatively low percentage, about 50% of mice showing PBC-like features, critically limits the usefulness of these mice as a PBC model.
Currently no “ideal PBC model” exists among the available mouse models. Although an enormous progress has been achieved in the last decades in the generation of different model systems that show astonishing similarities with human PBC, concerning immunological and histological characteristics, each model harbors still its specific limitations. As PBC represents a chronic cholangiopathy with slow progression to biliary fibrosis and cirrhosis, long-term studies with detailed characterization of the cholestatic phenotype would be of major interest and urgent need for these models.
4.3 Primary Sclerosing Cholangitis (PSC)
PSC leads to irregular scarring of the biliary tree causing bile duct strictures and dilatation-affecting intra- and extrahepatic bile ducts and may finally lead to biliary cirrhosis and liver failure. PSC primarily affects young men and is frequently associated with inflammatory bowel disease with specific clinical features including rectal sparing, right-sided disease, and backwash ileitis (i.e., PSC-IBD) [32]. The main attributes of an ideal PSC model therefore include the following clinicopathological features: male predominance, progressive fibrous-obliterative cholangitis of medium-sized and large bile ducts, onionskin-type-like periductal fibrosis, biliary type of liver fibrosis, concomitant predominantly right-sided mild colitis or pancolitis, and the high risk for CCA.
Animal models for (primary) sclerosing cholangitis [(P)SC] arbitrarily can be clustered into six different groups [33]: chemically induced cholangitis, knockout mouse models, cholangitis induced by infectious agents, models of experimental biliary obstruction, models involving enteric bacterial cell-wall components or colitis, and models of primary biliary epithelial and endothelial cell injury. Subtypes of models, their respective characteristics, and according references are summarized in Table 4.2. Due to limitations of space, we have to focus on only a few of them.
4.3.1 Mdr2 (Abcb4) Gene Knockout Mice
Mdr2 −/− mice show key features of human SC with development of cholangitis and onionskin-type periductal fibrosis similar to human PSC with strictures and dilatations of bile ducts and biliary type of liver fibrosis. Pathogenetically, the lack of biliary phospholipid secretion and increased concentration of free non-micellar-bound bile acids cause damage of bile duct epithelial cells [61] due to regurgitation of bile into the portal tracts leading to inflammation and fibrosis [58, 62]. However, the pathogenetic cause of disease still has to be determined in more detail, especially in regard to the specific role of bile acids. The Mdr2 −/−mouse model proved to be useful to test novel treatment strategies for (P)SC and liver fibrosis of the biliary type. Hence, this model is increasingly used [39–43, 58, 63–66]. Since the fibrotic response is strongly influenced by the genetic background and varies, it will be interesting to determine the potential effects of mouse genetic background on liver fibrosis degree in Mdr2 −/− mice. Only male mice should be used for modeling PSC, since female Mdr2 −/− mice develop gall stone disease already at young age, which is not a common feature in PSC patients and would also lead to significant variations in the cholestatic phenotype of animals [67]. One of the major limitations of this model, however, is the fact that there is insufficient evidence for the impact of MDR3 mutations/dysfunction or low biliary phospholipid output in PSC pathogenesis [68]. In addition, Mdr2 −/− mice do not develop colitis (at least in the genetic backgrounds tested already) or CCA but hepatocellular neoplastic nodules, which is unusual in PSC patients [69].
4.3.2 Mice Harboring a Mutation of Exon 10 of the Cystic Fibrosis (CF) Transmembrane Conductance Regulator Gene Knockout Mice (Cftr −/− Mice)
Cftr −/− mice develop focal cholangitis with inspissated bile and bile duct proliferation, resulting in biliary cirrhosis. Since CFTR gene mutations may play a pathogenetic role in PSC [70], Cftr −/− mice proved useful in the study of PSC development, since CFTR gene mutations may play a pathogenetic role in PSC although being not entirely clear so far [47]. A major limitation of this specific mouse model is that the genetic background strongly determines liver and/or intestinal phenotype [48–51].
4.3.3 Mice with a Point Mutation in the Ferrochelatase Gene (fch/fch) and Mice Fed the Porphyrinogenic Substance 3,5-Dietoxycarbonyl-1,4-Dihydrochollidine (DDC)
Both mice show sclerosing cholangitis and pronounced biliary fibrosis paralleled by ductular proliferation and portoportal bridging within weeks [34–36]. However, neither strictures nor dilations of the large duct system despite showing definite histological features of typical periductal fibrosis in PSC are seen which takes 4–8 weeks after DDC feeding depending on DDC-diet concentration and the mouse strain used [34]. The pathogenetic cause of disease is most likely linked to the biliary excreted DDC metabolite protoporphyrin IX and resulting ductal porphyrin plugs [34]. In addition, a link between DDC feeding and interference with biliary phospholipid secretion has been described [37]. The main advantages of this model include high reproducibility, high suitability for pathophysiological studies on the mechanisms of cholangitis, ductular reaction, and biliary type of liver fibrosis. However, the use for testing of treatment strategies for SC is limited due to the fixed liver phenotype and possible drug-drug interactions.
Taken together similar to PBC, currently there is no “ideal PSC model” available [63, 71, 72]. Since PSC represents a long-standing disease with complex underlying pathogenetic mechanisms, in which endogenous and exogenous factors are involved, it seems not likely that one single model will perfectly mirror PSC, but we will rather need various aspects of different models to study particular pathogenetic steps of PSC.
4.4 Graft-Versus-Host Disease (GvHD)
Bile ducts are major targets in acute and chronic GvHD representing a common complication and limiting factor of an allogeneic tissue and bone marrow transplantation. In humans, acute GvHD occurs within 100 days of transplant, and chronic GvHD (cGvHD) typically develops 100 days after transplantation. In mice, this temporal classification is not necessarily seen, since disease manifestation can differ in time of onset and is mainly defined by the clinical phenotype. Thus, chronic GvHD develops within weeks after transplantation in most mouse models [73]. Pathogenetically, cholangiocytes of small- to medium-caliber bile ducts are the major targets of T-cell-mediated destruction, causing apoptotic cell death and ultimately ductopenia [74]. So far, the detailed pathomechanism of GvHD is not clear.
In mice, GvHD across minor histocompatibility antigens can be induced experimentally by injection of spleen and bone marrow cells of congenic B10.D2 mice into sublethally irradiated BALB/c mice [60]. Bile ducts develop severe cholangitis with predominate lymphocytic inflammatory infiltrates 2–3 weeks after transplantation, and later on periductal fibrosis is observed. The major limitations of this mouse model are that neither loss of intrahepatic small bile ducts nor progression to liver cirrhosis during an observation period of 14 month is observed [60]. Generally speaking, factors confounding the translation of findings in mouse models to the human disease lie behind the fact that in humans acute GvHD typically precedes the chronic form, although in some cases chronic GvHD can occur without the occurrence of clinically obvious acute GvHD [73]. In addition, most patients are given immunosuppressive therapy to prevent acute GvHD influencing the development of chronic GvHD and further complicating modeling human GvHD in animals.
4.5 Biliary Atresia (BA)
BA is the most frequent identifiable cause of neonatal cholestasis, and most patients require early liver transplantation [75]. To date, the underlying pathophysiological mechanisms are unknown, although a pivotal role for a dysregulation of cellular and humoral immunity, viral, toxic, and genetic factors are considered [75]. To date, different model systems for BA have been established, including young lambs and calves [76], sea lampreys [77, 78], zebrafish [79] and mice [79–83]. In newborn BALB/c mice, infection with rhesus rotavirus type A (RRV) in the first 2 days of life leads to liver disease with development of hepatobiliary injury and cholestasis within 1 week of infection [82, 83] mimicking human BA in several aspects [82–84]. Intriguingly, this mouse model shares major clinicopathological features with the human disease, including a time-restricted susceptibility of bile duct injury to the early postnatal period, acholic stools, bile duct proliferation, and portal inflammation as well as type 1 rich inflammatory infiltrate in the liver and bile ducts [84–90]. However, one of the main limitations of this mouse model is the high mortality rate of mice.
4.6 Cholangiocarcinoma (CCA)
CCA is an epithelial biliary malignancy that originates from oncogenic transformation of cholangiocytes. Depending on the anatomic site, they may originate from different cell types, including intrahepatic biliary epithelial cells, hepatic progenitor cells, or mucin-producing cuboidal cholangiocytes of the extrahepatic biliary epithelium and peribiliary glands [91]. The identification of cellular origin in different subtypes may represent a prerequisite for effective therapy, but its impact on prognosis remains uncertain. CCA carcinogenesis is not entirely clear; however, well-known risk factors include the presence of PSC, liver fluke infections, hepatolithiasis or chronic hepatitis C, cirrhosis and toxins sharing induction of chronic cholestasis, and biliary and/or liver inflammation [92–95]. In the last years, several rodent models of CCA have been developed, including mice with xenograft and orthotopic tumors [96–102], genetically modified CCA models [103–105], and carcinogen-induced CCA models [106, 107]. Although these models provide adequate tools to gain insights into the pathophysiology of CCA development and to test new potential therapeutic agents in a preclinical setting, they harbor important limitations and difficulties discussed below (summarized in Table 4.3).
4.6.1 Xenograft and Orthotopic Models
In xenograft models, CCA cell lines are implanted into nude or severe combined immunodeficiency (SCID) mice. In 1985, the first study of CCA was developed by injecting a cell line derived from a human CCA metastasis subcutaneously into the flank of nude mice [108]. This model has not only been used for performing time-course and pathophysiological studies in regard to tumor growth, but also a high number of potential antitumor agents, including caffeic acid, tamoxifen, melatonin, and clobenpropit, have been tested [110–112]. Currently, although being not entirely clear so far, there is increasing evidence for a pivotal role of MicroRNAs (miRNAs) in cholangiocarcinogenesis with miR-26a and miR-494 known to promote tumor growth via targeting Wnt signaling pathway or modulation of the cell cycle [100, 113]. The informative value of studying interactions between cancer and peritumoral stroma cells in these mice, however, is limited, since tumor growth strongly depends on the species-specific microenvironment which is critically different from the tumor developing within the liver [91, 114]. Alternatively, CCA cells may be directly implanted into the bile duct of rodents that enables the study of organotypical interactions between tumor cells and surrounding stroma [115, 116]. In general, it has been shown that orthotopic CCA models are better predictors of drug efficacy and of potentially higher clinical relevance than xenograft models [114]. However, this approach has obvious limitations in the bile duct size of mice being far more time-consuming and technically difficult and therefore more expensive than conventional xenograft models [114].
4.7 Genetically Engineered Mice
4.7.1 p53 Knockout Mice Fed with Carbon Tetrachloride (CCl4)
Four months administration of CCl4 in mice harboring a deletion in the p53 gene leads to development of progressive liver injury and fibrosis paralleled by bile duct proliferation [109]. In accordance with the human CCA, p53 gene mutations are frequently observed [117]. Over time, these mice show tumors mimicking human CCA with atypical, infiltrating keratin 19-positive ducts and tubules with a dense collagenous stroma [109]. Similar to the human situation, this mouse model shows CCA development based on a combination of genetic susceptibility with a toxic chronic liver injury [114]. However, this mouse model is not very practicable; since the duration of time needed for tumor development is quite long (29–52 weeks) [114].
4.7.2 Smad4-Pten Knockout Mice
Smad4-Pten knockout mice, harboring a Cre-mediated deletion of phosphatase and tensin homolog (Pten) and SMAD family member 4 (Smad4), a tumor suppressor gene frequently altered in CCA [118] develop tumors histologically similar to intrahepatic CCA [104]. The authors crossbred mice carrying the Smad4 conditional allele (Smad4 Co) and/or the Pten conditional allele (Pten Co) which were crossed with albumin-Cre mice (Alb-Cre). After 2–3 months of age, biliary epithelial hyperplasia is observed, and at 4–7 months, mice show CCAs in all the animals followed by a progressive increase of tumoral intrahepatic nodules. This model is of major relevance for the understanding of the genetic and molecular mechanisms underlying disease development. In accordance with the human situation, PTEN loss has been linked to human CCA development by activation of the pro-proliferative and antiapoptotic PI3K pathway [93, 119]. Although this mouse model enables the investigation of intrahepatic CCA similar to the human situation already at 4–5 months of age, without any necessary further manipulation, limitations of this model include the absence of chronic liver injury and inflammation, the absence of metastases (even in older animals), and the concomitant development of tumors of the salivary glands [93].
4.7.3 The “DEN-Left Median Bile Duct Ligation” Model
Repeated intraperitoneal injection of diethyl-nitrosamine (DEN) in young Balb/c mice, following left median bile duct ligation and oral gavage of DEN, leads to the development of CCA [93, 107]. After 8 weeks, livers showed multifocal cystic hyperplasia of the intrahepatic bile ducts and multifocal cyst formation. At week 12, the biliary epithelium of the hyperplastic foci and the epithelium lining the cysts showed elongated nuclei. After 16 weeks bile duct tumors develop with full development of CCA in these areas at week 28. Despite its complexity requiring technically demanding bile duct surgery and long-term challenge with DEN, it represents the only known non-engineered mouse for CCA development [93].
Over the last few years, a number of HCC and CCA rodent models have been developed, many of them representing valuable tools for investigating some pathophysiological aspects of cancer development. However, due to the complexity of carcinogenesis per se, it is difficult to determine to what extent a single mouse model reproduces the human disease.
Conclusions
Biliary diseases are complex liver diseases in which extra- or intrahepatic bile ducts are affected. Significant research progress has been made the last years to develop animal models that will help understand their pathogenesis. Several limitations however exist which result in no “perfect model” that mirrors human disease. The use of various aspects of different models might be the way forward to study particular pathogenetic steps in biliary disease.
References
Lazaridis KN, LaRusso NF. The Cholangiopathies. Mayo Clin Proc. 2015;90(6):791–800.
Hirschfield GM, Gershwin ME. The immunobiology and pathophysiology of primary biliary cirrhosis. Ann Rev Phathol. 2013;24(8):303–30.
Hirschfield GM, Karlsen TH, Lindor KD, Adams DH. Primary sclerosing cholangitis. Lancet. 2013;382(9904):1587–99.
Fickert P, Pollheimer MJ, Beuers U, Lackner C, Hirschfield G, Housset C, Keitel V, Schramm C, Marschall HU, Karlsen TH, Melum E, Kaser A, Eksteen B, Strazzabosco M, Manns M, Trauner M, International PSC Study Group (IPSCSG). Characterization of animal models for primary sclerosing cholangitis (PSC). J Hepatol. 2014;60(6):1290–303.
Seok J, Warren HS, Cuenca AG, Mindrinos MN, Baker HV, Xu W, Richards DR, McDonald-Smith GP, et al.; Inflammation and Host Response to Injury, Large Scale Collaborative Research Program. Genomic responses in mouse models poorly mimic human inflammatory diseases. Proc Natl Acad Sci U S A 2013;110(9):3507–12.
Goodwin B, Watson MA, Kim H, Miao J, Kemper JK, Kliewer SA. Differential regulation of rat and human CYP7A1 by the nuclear oxysterol receptor liver X receptor-alpha. Mol Endocrinol. 2003;17(3):386–94.
Chiang JY. Bile acids: regulation of synthesis. J Lipid Res. 2009;50(10):1955–66.
Nguyen TL, Vieira-Silva S, Liston A, Raes J. How informative is the mouse for human gut microbiota research? Dis Model Mech. 2015;8(1):1–16.
Liu Y, Meyer C, Xu C, Weng H, Hellerbrand C, ten Dijke P, Dooley S. Animal models of chronic liver diseases. Am J Physiol Gastrointest Liver Physiol. 2013;304(5):G449–68.
Leung PS, Chuang DT, Wynn RM, Cha S, Danner DJ, Ansari A, Coppel RL, Gershwin ME. Autoantibodies to BCOADC-E2 in patients with primary biliary cirrhosis recognize a conformational epitope. Hepatology. 1995;22(2):505–13.
Moteki S, Leung PS, Dickson ER, Van Thiel DH, Galperin C, Buch T, Alarcon-Segovia D, Kershenobich D, Kawano K, Coppel RL, et al. Epitope mapping and reactivity of autoantibodies to the E2 component of 2-oxoglutarate dehydrogenase complex in primary biliary cirrhosis using recombinant 2-oxoglutarate dehydrogenase complex. Hepatology. 1996;23(3):436–44.
Van de Water J, Ansari A, Prindiville T, Coppel RL, Ricalton N, Kotzin BL, Liu S, Roche TE, Krams SM, Munoz S, Gershwin ME. Heterogeneity of autoreactive T cell clones specific for the E2 component of the pyruvate dehydrogenase complex in primary biliary cirrhosis. J Exp Med. 1995;181(2):723–33.
Massagué J. TGF-beta signal transduction. Annu Rev Biochem. 1998;67:753–91.
Tsuneyama K, Moritoki Y, Kikuchi K, Nakanuma Y. Pathological features of new animal models for primary biliary cirrhosis. Int J Hepatol. 2012:403954.
Oertelt S, Lian ZX, Cheng CM, Chuang YH, Padgett KA, He XS, Ridgway WM, Ansari AA, Coppel RL, Li MO, Flavell RA, Kronenberg M, Mackay IR, Gershwin ME. Anti-mitochondrial antibodies and primary biliary cirrhosis in TGF-beta receptor II dominant-negative mice. J Immunol. 2006;177(3):1655–60.
Yang GX, Lian ZX, Chuang YH, et al. Adoptive transfer of CD8(+) T cells from transforming growth factor beta receptor type II (dominant negative form) induces autoimmune cholangitis in mice. Hepatology. 2008;47:1974–82.
Moritoki Y, Lian ZX, Lindor K, Tuscano J, Tsuneyama K, Zhang W, Ueno Y, Dunn R, Kehry M, Coppel RL, Mackay IR, Gershwin ME. B-cell depletion with anti-CD20 ameliorates autoimmune cholangitis but exacerbates colitis in transforming growth factor-beta receptor II dominant negative mice. Hepatology. 2009;50(6):1893–903.
Chuang YH, Lian ZX, Yang GX, et al. Natural killer T cells exacerbate liver injury in a transforming growth factor beta receptor II dominant-negative mouse model of primary biliary cirrhosis. Hepatology. 2008;47:571–80.
Tsuda M, Zhang W, Yang GX, Tsuneyama K, Ando Y, Kawata K, et al. Deletion of interleukin (IL)-12p35 induces liver fibrosis in dominant-negative TGFβ receptor type II mice. Hepatology. 2013;57:806–16.
Popov Y. Mouse model of primary biliary cirrhosis with progressive fibrosis: are we there yet? Hepatology. 2013;57(2):429–31.
Wakabayashi K, Lian ZX, Moritoki Y, et al. IL-2 receptor alpha(−/−) mice and the development of primary biliary cirrhosis. Hepatology. 2006;44:1240–9.
Yao Y, Yang W, Yang YQ, Ma HD, Lu FT, Li L, Tao YY, Tsuneyama K, Zhang W, Friedman S, Gershwin ME, Lian ZX. Distinct from its canonical effects, deletion of IL-12p40 induces cholangitis and fibrosis in interleukin-2Rα(−/−) mice. J Autoimmun. 2014;51:99–108.
Irie J, Wu Y, Wicker LS, Rainbow D, Nalesnik MA, Hirsch R, Peterson LB, Leung PS, Cheng C, Mackay IR, Gershwin ME, Ridgway WM. NOD.c3c4 congenic mice develop autoimmune biliary disease that serologically and pathogenetically models human primary biliary cirrhosis. J Exp Med. 2006;203(5):1209–19.
Koarada S, Wu Y, Fertig N, Sass DA, Nalesnik M, Todd JA, Lyons PA, Fenyk-Melody J, Rainbow DB, Wicker LS, Peterson LB, Ridgway WM. Genetic control of autoimmunity: protection from diabetes, but spontaneous autoimmune biliary disease in a nonobese diabetic congenic strain. J Immunol. 2004;173(4):2315–23.
Melero S, Spirlì C, Zsembery A, Medina JF, Joplin RE, Duner E, et al. Defective regulation of cholangiocyte Cl−/HCO3(−) and Na+/H+ exchanger activities in primary biliary cirrhosis. Hepatology. 2002;35:1513–21.
Prieto J, García N, Martí-Climent JM, Peñuelas I, Richter JA, Medina JF. Assessment of biliary bicarbonate secretion in humans by positron emission tomography. Gastroenterology. 1999;117:167–72.
Medina JF, Martínez-Ansó, Vazquez JJ, Prieto J. Decreased anion exchanger 2 immunoreactivity in the liver of patients with primary biliary cirrhosis. Hepatology. 1997; 25:12–7.
Salas JT, Banales JM, Sarvide S, Recalde S, Ferrer A, Uriarte I, et al. Ae2a,b-deficient mice develop antimitochondrial antibodies and other features resembling primary biliary cirrhosis. Gastroenterology. 2008;134:1482–93.
Brunkow ME, Jeffery EW, Hjerrild KA, Paeper B, Clark LB, Yasayko SA, Wilkinson JE, Galas D, Ziegler SF, Ramsdell F. Disruption of a new forkhead/winged-helix protein, scurfin, results in the fatal lymphoproliferative disorder of the scurfy mouse. Nat Genet. 2001;27(1):68–73.
Zhang W, Sharma R, Ju ST, He XS, Tao Y, Tsuneyama K, et al. Deficiency in regulatory T cells results in development of antimitochondrial antibodies and autoimmune cholangitis. Hepatology. 2009;49:545–52.
Ohba K, Omagari K, Murase K, Hazama H, Masuda J, Kinoshita H, et al. A possible mouse model for spontaneous cholangitis: serological and histological characteristics of MRL/lpr mice. Pathology. 2002;34:250–6.
Loftus Jr EV, Harewood GC, Loftus CG, Tremaine WJ, Harmsen WS, Zinsmeister AR, Jewell DA, Sandborn WJ. PSC-IBD: a unique form of inflammatory bowel disease associated with primary sclerosing cholangitis. Gut. 2005;54(1):91–6.
Pollheimer MJ, Halilbasic E, Fickert P, Trauner M. Pathogenesis of primary sclerosing cholangitis. Best Pract Res Clin Gastroenterol. 2011;25(6):727–39.
Fickert P, Stöger U, Fuchsbichler A, Moustafa T, Marschall HU, Weiglein AH, Tsybrovskyy O, Jaeschke H, Zatloukal K, Denk H, Trauner M. A new xenobiotic-induced mouse model of sclerosing cholangitis and biliary fibrosis. Am J Pathol. 2007;171(2):525–36.
Meerman L, Koopen NR, Bloks V, Van Goor H, Havinga R, Wolthers BG, Kramer W, Stengelin S, Müller M, Kuipers F, Jansen PL. Biliary fibrosis associated with altered bile composition in a mouse model of erythropoietic protoporphyria. Gastroenterology. 1999;117(3):696–705.
Libbrecht L, Meerman L, Kuipers F, Roskams T, Desmet V, Jansen P. Liver pathology and hepatocarcinogenesis in a long-term mouse model of erythropoietic protoporphyria. J Pathol. 2003;199(2):191–200.
Lyoumi S, Abitbol M, Rainteau D, Karim Z, Bernex F, Oustric V, Millot S, Lettéron P, Heming N, Guillmot L, Montagutelli X, Berdeaux G, Gouya L, Poupon R, Deybach JC, Beaumont C, Puy H. Protoporphyrin retention in hepatocytes and Kupffer cells prevents sclerosing cholangitis in erythropoietic protoporphyria mouse model. Gastroenterology. 2011;141(4):1509–19, 1519.e1–3.
Fickert P, Fuchsbichler A, Marschall HU, Wagner M, Zollner G, Krause R, et al. Lithocholic acid feeding induces segmental BD obstruction and destructive cholangitis in mice. Am J Pathol. 2006;168:410–22.
Halilbasic E, Fiorotto R, Fickert P, Marschall HU, Moustafa T, Spirli C, et al. Side chain structure determines unique physiologic and therapeutic properties of norursodeoxycholic acid in Mdr2−/− mice. Hepatology. 2009;49:1972–81.
Baghdasaryan A, Claudel T, Kosters A, Gumhold J, Silbert D, Thüringer A, Leski K, Fickert P, Karpen SJ, Trauner M. Curcumin improves sclerosing cholangitis in Mdr2−/− mice by inhibition of cholangiocyte inflammatory response and portal myofibroblast proliferation. Gut. 2010;59(4):521–30.
Baghdasaryan A, Claudel T, Gumhold J, Silbert D, Adorini L, Roda A, et al. Dual farnesoid X receptor/TGR5 agonist INT-767 reduces liver injury in the Mdr2-/- (Abcb4-/-) mouse cholangiopathy model by promoting biliary HCO-3 output. Hepatology. 2011;54:1303–12
Moustafa T, Fickert P, Magnes C, Guelly C, Thueringer A, Frank S, Kratky D, Sattler W, Reicher H, Sinner F, Gumhold J, Silbert D, Fauler G, Höfler G, Lass A, Zechner R, Trauner M. Alterations in lipid metabolism mediate inflammation, fibrosis, and proliferation in a mouse model of chronic cholestatic liver injury. Gastroenterology. 2012;142(1):140–51.e12.
Ehlken H, Kondylis V, Heinrichsdorff J, Ochoa-Callejero L, Roskams T, Pasparakis M. Hepatocyte IKK2 protects Mdr2−/− mice from chronic liver failure. PLoS One. 2011;6(10):e25942.
Fickert P, Zollner G, Fuchsbichler A, Stumptner C, Weiglein AH, Lammert F, et al. Ursodeoxycholic acid aggravates bile infarcts in BD-ligated and Mdr2 knockout mice via disruption of cholangioles. Gastroenterology. 2002;123:1238–51.
Fickert P, Fuchsbichler A, Wagner M, Zollner G, Kaser A, Tilg H, et al. Regurgitation of bile acids from leaky BDs causes sclerosing cholangitis in Mdr2 (Abcb4) knockout mice. Gastroenterology. 2004;127:261–74.
Popov Y, Patsenker E, Fickert P, Trauner M, Schuppan D, et al. Mdr2 (Abcb4)−/− mice spontaneously develop severe biliary fibrosis via massive dysregulation of pro- and antifibrogenic genes. J Hepatol. 2005;43:1045–54.
Henckaerts L, Jaspers M, Van Steenbergen W, Vliegen L, Fevery J, Nuytten H, Roskams T, Rutgeerts P, Cassiman JJ, Vermeire S, Cuppens H. Cystic fibrosis transmembrane conductance regulator gene polymorphisms in patients with primary sclerosing cholangitis. J Hepatol. 2009;50(1):150–7.
Snouwaert JN, Brigman KK, Latour AM, Malouf NN, Boucher RC, Smithies O, Koller BH. An animal model for cystic fibrosis made by gene targeting. Science. 1992;257(5073):1083–8.
Dorin JR, Dickinson P, Alton EW, Smith SN, Geddes DM, Stevenson BJ, Kimber WL, Fleming S, Clarke AR, Hooper ML, et al. Cystic fibrosis in the mouse by targeted insertional mutagenesis. Nature. 1992;359(6392):211–5.
Colledge WH, Abella BS, Southern KW, Ratcliff R, Jiang C, Cheng SH, MacVinish LJ, Anderson JR, Cuthbert AW, Evans MJ. Generation and characterization of a delta F508 cystic fibrosis mouse model. Nat Genet. 1995;10(4):445–52.
Zeiher BG, Eichwald E, Zabner J, Smith JJ, Puga AP, McCray Jr PB, Capecchi MR, Welsh MJ, Thomas KR. A mouse model for the delta F508 allele of cystic fibrosis. J Clin Invest. 1995;96(4):2051–64.
Stephens J, Cosyns M, Jones M, Hayward A. Liver and bile duct pathology following Cryptosporidium parvum infection of immunodeficient mice. Hepatology. 1999;30:27–35.
Ungar BL, Burris JA, Quinn CA, Finkelman FD. New mouse models for chronic Cryptosporidium infection in immunodeficient hosts. Infect Immun. 1990;58:961–9.
Mead JR, Arrowood MJ, Sidwell RW, Healey MC. Chronic Cryptosporidium parvum infections in congenitally immunodeficient SCID and nude mice. J Infect Dis. 1991;163:1297–304.
Ponnuraj EM, Hayward AR. Requirement for TNF-Tnfrsf1 signalling for sclerosing cholangitis in mice chronically infected by Cryptosporidium parvum. Clin Exp Immunol. 2002;128:416–20.
Ward JM, Anver MR, Haines DC, Benveniste RE. Chronic active hepatitis in mice caused by Helicobacter hepaticus. Am J Pathol. 1994;145:959–68.
Avenaud P, Le Bail B, Mayo K, Marais A, Fawaz R, Bioulac-Sage P, et al. Natural history of Helicobacter hepaticus infection in conventional A/J mice, with special reference to liver involvement. Infect Immun. 2003;71:3667–72.
Fickert P, Wagner M, Marschall HU, Fuchsbichler A, Zollner G, Tsybrovskyy O, Zatloukal K, Liu J, Waalkes MP, Cover C, Denk H, Hofmann AF, Jaeschke H, Trauner M. 24-norUrsodeoxycholic acid is superior to ursodeoxycholic acid in the treatment of sclerosing cholangitis in Mdr2 (Abcb4) knockout mice. Gastroenterology. 2006;130(2):465–81.
Georgiev P, Jochum W, Heinrich S, Jang JH, Nocito A, Dahm F, et al. Characterization of time-related changes after experimental bile duct ligation. Br J Surg. 2008;95:646–56.
Nonomura A, Kono N, Minato H, Nakanuma Y. Diffuse biliary tract involvement mimicking primary sclerosing cholangitis in an experimental model of chronic graft-versus-host disease in mice. Pathol Int. 1998;48(6):421–7.
Smit JJ, Schinkel AH, Oude Elferink RP, Groen AK, Wagenaar E, van Deemter L, et al. Homozygous disruption of the murine mdr2 P-glycoprotein gene leads to a complete absence of phospholipid from bile and to liver disease. Cell. 1993;75:451–62.
Ernst TM, Schwinge D, Raabe N, Daubmann A, Kaul MG, Adam G, Schramm C, Ittrich H. Imaging of the murine biliopancreatic tract at 7 Tesla: technique and results in a model of primary sclerosing cholangitis. J Magn Reson Imaging. 2014;40(6):1355–64.
Trauner M, Fickert P, Baghdasaryan A, Claudel T, Halilbasic E, Moustafa T, Wagner M, Zollner G. New insights into autoimmune cholangitis through animal models. Dig Dis. 2010;28(1):99–104.
Barikbin R, Neureiter D, Wirth J, Erhardt A, Schwinge D, Kluwe J, Schramm C, Tiegs G, Sass G. Induction of heme oxygenase 1 prevents progression of liver fibrosis in Mdr2 knockout mice. Hepatology. 2012;55(2):553–62.
Strack I, Schulte S, Varnholt H, Schievenbusch S, Töx U, Wendland K, Steffen HM, Drebber U, Dienes HP, Odenthal M. β-Adrenoceptor blockade in sclerosing cholangitis of Mdr2 knockout mice: antifibrotic effects in a model of nonsinusoidal fibrosis. Lab Investig. 2011;91(2):252–61.
Blaas L, Kornfeld JW, Schramek D, Musteanu M, Zollner G, Gumhold J, van Zijl F, Schneller D, Esterbauer H, Egger G, Mair M, Kenner L, Mikulits W, Eferl R, Moriggl R, Penninger J, Trauner M, Casanova E. Disruption of the growth hormone--signal transducer and activator of transcription 5 – insulinlike growth factor 1 axis severely aggravates liver fibrosis in a mouse model of cholestasis. Hepatology. 2010;51(4):1319–26.
Lammert F, Wang DQ, Hillebrandt S, Geier A, Fickert P, Trauner M, Matern S, Paigen B, Carey MC. Spontaneous cholecysto- and hepatolithiasis in Mdr2−/− mice: a model for low phospholipid-associated cholelithiasis. Hepatology. 2004;39(1):117–28.
Trauner M, Fickert P, Wagner M. MDR3 (ABCB4) defects: a paradigm for the genetics of adult cholestatic syndromes. Semin Liver Dis. 2007;27(1):77–98.
Katzenellenbogen M, Mizrahi L, Pappo O, Klopstock N, Olam D, Jacob-Hirsch J, Amariglio N, Rechavi G, Domany E, Galun E, Goldenberg D. Molecular mechanisms of liver carcinogenesis in the mdr2-knockout mice. Mol Cancer Res. 2007;5(11):1159–70.
Pollheimer MJ, Trauner M, Fickert P. Will we ever model PSC? – "it’s hard to be a PSC model!". Clin Res Hepatol Gastroenterol. 2011;35(12):792–804.
Vierling JM. Animal models for primary sclerosing cholangitis. Best Pract Res Clin Gastroenterol. 2001;15(4):591–610.
Pollheimer MJ, Fickert P. Animal models in primary biliary cirrhosis and primary sclerosing cholangitis. Clin Rev Allergy Immunol. 2015;48(2–3):207–17.
Schroeder MA, DiPersio JF. Mouse models of graft-versus-host disease: advances and limitations. Dis Model Mech. 2011;4(3):318–33.
Vierling JM, Hreha G, Wang H, Braun M. The role of biliary epithelial cells in the immunopathogenesis of non-suppurative destructive cholangitis in murine hepatic graft-versus-host disease. Trans Am Clin Climatol Assoc. 2011;122:326–35.
Mack CL. What causes biliary atresia? Unique aspects of the neonatal immune system provide clues to disease pathogenesis. Cell Mol Gastroenterol Hepatol. 2015;1(3):267–74.
Harper P, Plant JW, Unger DB. Congenital biliary atresia and jaundice in lambs and calves. Aust Vet J. 1990;67(1):18–22.
Cai SY, Lionarons DA, Hagey L, Soroka CJ, Mennone A, Boyer JL. Adult sea lamprey tolerates biliary atresia by altering bile salt composition and renal excretion. Hepatology. 2013;57(6):2418–26.
Yeoh EJ, Ross ME, Shurtleff SA, Williams WK, Patel D, Mahfouz R, Behm FG, Raimondi SC, Relling MV, Patel A, Cheng C, Campana D, Wilkins D, Zhou X, Li J, Liu H, Pui CH, Evans WE, Naeve C, Wong L, Downing JR. Classification, subtype discovery, and prediction of outcome in pediatric acute lymphoblastic leukemia by gene expression profiling. Cancer Cell. 2002;1(2):133–43.
Bangaru B, Morecki R, Glaser JH, Gartner LM, Horwitz MS. Comparative studies of biliary atresia in the human newborn and reovirus-induced cholangitis in weanling mice. Lab Invest. 1980;43(5):456–62.
Szavay PO, Leonhardt J, Czech-Schmidt G, Petersen C. The role of reovirus type 3 infection in an established murine model for biliary atresia. Eur J Pediatr Surg. 2002;12(4):248–50.
Wilson GA, Morrison LA, Fields BN. Association of the reovirus S1 gene with serotype 3-induced biliary atresia in mice. J Virol. 1994;68(10):6458–65.
Petersen C, Biermanns D, Kuske M, Schäkel K, Meyer-Junghänel L, Mildenberger H. New aspects in a murine model for extrahepatic biliary atresia. J Pediatr Surg. 1997;32(8):1190–5.
Riepenhoff-Talty M, Schaekel K, Clark HF, Mueller W, Uhnoo I, Rossi T, Fisher J, Ogra PL. Group A rotaviruses produce extrahepatic biliary obstruction in orally inoculated newborn mice. Pediatr Res. 1993;33(4 Pt 1):394–9.
Asai A, Miethke A, Bezerra JA. Pathogenesis of biliary atresia: defining biology to understand clinical phenotypes. Nat Rev Gastroenterol Hepatol. 2015;12(6):342–52.
Shivakumar P, Campbell KM, Sabla GE, Miethke A, Tiao G, McNeal MM, Ward RL, Bezerra JA. Obstruction of extrahepatic bile ducts by lymphocytes is regulated by IFN-gamma in experimental biliary atresia. J Clin Invest. 2004;114(3):322–9.
Carvalho E, Liu C, Shivakumar P, Sabla G, Aronow B, Bezerra JA. Analysis of the biliary transcriptome in experimental biliary atresia. Gastroenterology. 2005;129(2):713–7.
Leonhardt J, Stanulla M, von Wasielewski R, Skokowa J, Kübler J, Ure BM, Petersen C. Gene expression profile of the infective murine model for biliary atresia. Pediatr Surg Int. 2006;22(1):84–9.
Mack CL, Tucker RM, Sokol RJ, Kotzin BL. Armed CD4+ Th1 effector cells and activated macrophages participate in bile duct injury in murine biliary atresia. Clin Immunol. 2005;115(2):200–9.
Shivakumar P, Sabla GE, Whitington P, Chougnet CA, Bezerra JA. Neonatal NK cells target the mouse duct epithelium via Nkg2d and drive tissue-specific injury in experimental biliary atresia. J Clin Invest. 2009;119(8):2281–90.
Shivakumar P, Sabla G, Mohanty S, McNeal M, Ward R, Stringer K, Caldwell C, Chougnet C, Bezerra JA. Effector role of neonatal hepatic CD8+ lymphocytes in epithelial injury and autoimmunity in experimental biliary atresia. Gastroenterology. 2007;133(1):268–77.
Rizvi S, Gores GJ. Pathogenesis, diagnosis, and management of cholangiocarcinoma. Gastroenterology. 2013;145(6):1215–29.
Yamamoto S, Kubo S, Hai S, Uenishi T, Yamamoto T, Shuto T, Takemura S, Tanaka H, Yamazaki O, Hirohashi K, Tanaka T. Hepatitis C virus infection as a likely etiology of intrahepatic cholangiocarcinoma. Cancer Sci. 2004;95(7):592–5.
De Minicis S, Kisseleva T, Francis H, Baroni GS, Benedetti A, Brenner D, Alvaro D, Alpini G, Marzioni M. Liver carcinogenesis: rodent models of hepatocarcinoma and cholangiocarcinoma. Dig Liver Dis. 2013;45(6):450–9.
Khan SA, Thomas HC, Davidson BR, Taylor-Robinson SD. Cholangiocarcinoma. Lancet. 2005;366(9493):1303–14.
Blechacz B, Gores GJ. Cholangiocarcinoma: advances in pathogenesis, diagnosis, and treatment. Hepatology. 2008;48(1):308–21.
Meng F, Yamagiwa Y, Ueno Y, Patel T. Over-expression of interleukin-6 enhances cell survival and transformed cell growth in human malignant cholangiocytes. J Hepatol. 2006;44(6):1055–65.
Fava G, Marucci L, Glaser S, Francis H, De Morrow S, Benedetti A, Alvaro D, Venter J, Meininger C, Patel T, Taffetani S, Marzioni M, Summers R, Reichenbach R, Alpini G. gamma-Aminobutyric acid inhibits cholangiocarcinoma growth by cyclic AMP-dependent regulation of the protein kinase A/extracellular signal-regulated kinase 1/2 pathway. Cancer Res. 2005;65(24):11437–46.
Pawar P, Ma L, Byon CH, Liu H, Ahn EY, Jhala N, Arnoletti JP, McDonald JM, Chen Y. Molecular mechanisms of tamoxifen therapy for cholangiocarcinoma: role of calmodulin. Clin Cancer Res. 2009;15(4):1288–96.
Tang T, Zheng JW, Chen B, Li H, Li X, Xue KY, Ai X, Zou SQ. Effects of targeting magnetic drug nanoparticles on human cholangiocarcinoma xenografts in nude mice. Hepatobiliary Pancreat Dis Int. 2007;6(3):303–7.
Zhang J, Han C, Wu T. MicroRNA-26a promotes cholangiocarcinoma growth by activating β-catenin. Gastroenterology. 2012;143(1):246–56.e8.
Olaru AV, Ghiaur G, Yamanaka S, Luvsanjav D, An F, Popescu I, Alexandrescu S, Allen S, Pawlik TM, Torbenson M, Georgiades C, Roberts LR, Gores GJ, Ferguson-Smith A, Almeida MI, Calin GA, Mezey E, Selaru FM. MicroRNA down-regulated in human cholangiocarcinoma control cell cycle through multiple targets involved in the G1/S checkpoint. Hepatology. 2011;54(6):2089–98.
Zhang K, Chen D, Wang X, Zhang S, Wang J, Gao Y, Yan B. RNA interference targeting slug increases cholangiocarcinoma cell sensitivity to cisplatin via upregulating PUMA. Int J Mol Sci. 2011;12(1):385–400.
Zender S, Nickeleit I, Wuestefeld T, Sörensen I, Dauch D, Bozko P, El-Khatib M, Geffers R, Bektas H, Manns MP, Gossler A, Wilkens L, Plentz R, Zender L, Malek NP. A critical role for notch signaling in the formation of cholangiocellular carcinomas. Cancer Cell. 2013;23(6):784–95.
Xu X, Kobayashi S, Qiao W, Li C, Xiao C, Radaeva S, Stiles B, Wang RH, Ohara N, Yoshino T, LeRoith D, Torbenson MS, Gores GJ, Wu H, Gao B, Deng CX. Induction of intrahepatic cholangiocellular carcinoma by liver-specific disruption of Smad4 and Pten in mice. J Clin Invest. 2006;116(7):1843–52.
Farazi PA, Zeisberg M, Glickman J, Zhang Y, Kalluri R, DePinho RA. Chronic bile duct injury associated with fibrotic matrix microenvironment provokes cholangiocarcinoma in p53-deficient mice. Cancer Res. 2006;66(13):6622–7.
Fava G, Alpini G, Rychlicki C, Saccomanno S, DeMorrow S, Trozzi L, Candelaresi C, Venter J, Di Sario A, Marzioni M, Bearzi I, Glaser S, Alvaro D, Marucci L, Francis H, Svegliati-Baroni G, Benedetti A. Leptin enhances cholangiocarcinoma cell growth. Cancer Res. 2008;68(16):6752–61.
Yang H, Li TW, Peng J, Tang X, Ko KS, Xia M, Aller MA. A mouse model of cholestasis-associated cholangiocarcinoma and transcription factors involved in progression. Gastroenterology. 2011;141(1):378–88, 388.e1–4.
Hudd C, Euhus DM, LaRegina MC, Herbold DR, Palmer DC, Johnson FE. Effect of cholecystokinin on human cholangiocarcinoma xenografted into nude mice. Cancer Res. 1985;45(3):1372–7.
Farazi PA, Zeisberg M, Glickman J, Zhang Y, Kalluri R, DePinho RA. Chronic bile duct injury associated with fibrotic matrix microenvironment provokes cholangiocarcinoma in p53-deficient mice. Cancer Res. 2006;66(13):6622–7.
Wang M, Xiao J, Shen M, Yahong Y, Tian R, Zhu F, Jiang J, Du Z, Hu J, Liu W, Qin R. Isolation and characterization of tumorigenic extrahepatic cholangiocarcinoma cells with stem cell-like properties. Int J Cancer. 2011;128(1):72–81.
Lu D, Han C, Wu T. Microsomal prostaglandin E synthase-1 inhibits PTEN and promotes experimental cholangiocarcinogenesis and tumor progression. Gastroenterology. 2011;140(7):2084–94.
Jing G, Yuan K, Turk AN, Jhala NC, Arnoletti JP, Zhang K, McDonald JM, Chen Y. Tamoxifen enhances therapeutic effects of gemcitabine on cholangiocarcinoma tumorigenesis. Lab Invest. 2011;91(6):896–904.
Yamanaka S, Campbell NR, An F, Kuo SC, Potter JJ, Mezey E, Maitra A, Selaru FM. Coordinated effects of microRNA-494 induce G2/M arrest in human cholangiocarcinoma. Cell Cycle. 2012;11(14):2729–38.
Ko KS, Peng J, Yang H. Animal models of cholangiocarcinoma. Curr Opin Gastroenterol. 2013;29(3):312–8.
Campbell DJ, Dumur CI, Lamour NF, Dewitt JL, Sirica AE. Novel organotypic culture model of cholangiocarcinoma progression. Hepatol Res. 2012;42(11):1119–30.
Noda T, Shimoda M, Ortiz V, Sirica AE, Wands JR. Immunization with aspartate-β-hydroxylase-loaded dendritic cells produces antitumor effects in a rat model of intrahepatic cholangiocarcinoma. Hepatology. 2012;55(1):86–97.
Furubo S, Harada K, Shimonishi T, Katayanagi K, Tsui W, Nakanuma Y. Protein expression and genetic alterations of p53 and ras in intrahepatic cholangiocarcinoma. Histopathology. 1999;35(3):230–40.
Kang YK, Kim WH, Jang JJ. Expression of G1-S modulators (p53, p16, p27, cyclin D, Rb) and Smad4/Dpc4 in intrahepatic cholangiocarcinoma. Hum Pathol. 2002;33(9):877–83.
Tanno S, Yanagawa N, Habiro A, Koizumi K, Nakano Y, Osanai M, Mizukami Y, Okumura T, Testa JR, Kohgo Y. Serine/threonine kinase AKT is frequently activated in human bile duct cancer and is associated with increased radioresistance. Cancer Res. 2004;64(10):3486–90.
Aisaka Y, Watanabe Y, Kamiyasu M, Masanaga T, Tsuji K, Nakanishi T, Kajiyama G, Gershwin ME. Immune-mediated cholangiohepatitis in neonatally thymectomized mice: the role of T cells and analysis of T-cell receptor Vbeta usage. J Autoimmun. 2000;14:239–46.
Wakabayashi K, Yoshida K, Leung PS, et al. Induction of autoimmune cholangitis in non-obese diabetic (NOD).1101 mice following a chemical xenobiotic immunization. Clin Exp Immunol. 2008;155:577–86.
Ambrosini YM, Yang GX, Zhang W, Tsuda M, Shu S, Tsuneyama K, et al. The multi-hit hypothesis of primary biliary cirrhosis: polyinosinic-polycytidylic acid (poly I:C) and murine autoimmune cholangitis. Clin Exp Immunol. 2011;166:110–20.
Ide T, Sata M, Suzuki H, Uchimura Y, Murashima S, Shirachi M, et al. An experimental animal model of primary biliary cirrhosis induced by lipopolysaccharide and pyruvate dehydrogenase. Kurume Med J. 43:185–8.
Mattner J, Savage PB, Leung P, Oertelt SS, Wang V, Trivedi O, et al. Liver autoimmunity triggered by microbial activation of natural killer T cells. Cell Host Microbe. 2008;3:304–15.
Wang JJ, Yang GX, Zhang WC, Lu L, Tsuneyama K, Kronenberg M, Véla JL, Lopez-Hoyos M, He XS, Ridgway WM, Leung PS, Gershwin ME. Escherichia coli infection induces autoimmune cholangitis and anti-mitochondrial antibodies in non-obese diabetic (NOD).B6 (Idd10/Idd18) mice. Clin Exp Immunol. 2014;175(2):192–201.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
Pollheimer, M.J., Fickert, P. (2017). Animal Models of Biliary Disease: Current Approaches and Limitations. In: Hirschfield, G., Adams, D., Liaskou, E. (eds) Biliary Disease. Springer, Cham. https://doi.org/10.1007/978-3-319-50168-0_4
Download citation
DOI: https://doi.org/10.1007/978-3-319-50168-0_4
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-50166-6
Online ISBN: 978-3-319-50168-0
eBook Packages: MedicineMedicine (R0)