Abstract
Physical activity counselling and individually prescribed and supervised exercise training are core components of a comprehensive cardiac rehabilitation (CR) program, The primary objective of an exercise-based training intervention in cardiac rehabilitation is to positively influence disease progression and prognosis and to improve symptom limited exercise tolerance and overall quality of life. Within a large meta-analysis exercise based cardiac rehabilitation have been shown to reduce overall and cardiovascular mortality rate as well as hospital admissions rate. The safety and efficiency of aerobic endurance and dynamic resistance exercise in to improve exercise capacity and quality of life in cardiac patients is well established and international guidelines recommend its implementation in cardiac rehabilitation programs. This chapter give detailed evidence based practical recommendation how to set up an effective and save exercise training in cardiac rehabilitation.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Exercise Training
- Resistance Training
- Resistance Exercise
- Cardiac Rehabilitation
- Coronary Heart Disease Patient
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
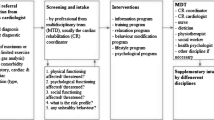
Physical activity counseling and individually prescribed and supervised exercise training are core components of a comprehensive cardiac rehabilitation (CR) program, compromising 30–50 % (up to >70 %) of all cardiac rehabilitation activities. This applies to phase II as well as to phase III cardiac rehabilitation for patients post-acute coronary syndrome and post-primary coronary angioplasty (PCI), post-cardiac surgery (coronary artery bypass, valve heart surgery, cardiac transplantation), as well as in chronic heart failure patients.
Within a large meta-analysis of Cochrane database, exercise-based cardiac rehabilitation has been shown to reduce overall mortality rate by 13 %, cardiovascular mortality rate by 26 %, and hospital admission rate by 18–31 % in patients with coronary heart disease (CHD) [1–3]. Moreover meta-analysis has revealed CR programs with exercise training interventions as only content to be even more effective, demonstrating exercise only to reduce overall mortality rate by 27–28 %, mortality rate due to cardiovascular disease by 31 % (Fig. 4.1), and the re-infract rate by 43 % [3–5]. These results emphasize the impact of exercise interventions as a core component of CR program. However, so far epidemiological studies have not been able to provide sufficient statistically significant evidence linking the incidence of nonfatal heart attacks and sudden cardiac death to exercise training-based rehabilitation measures [1–5].
Effectiveness of exercise only or exercise as part of a comprehensive cardiac rehabilitation program on all-cause mortality and cardiac mortality (According to Jolliffe et al. [3])
1 Definition of Terms
Any muscle contraction resulting in an energy metabolism above basal metabolic rate is characterized as physical activity [6]. Exercise or exercise training is any physical activity that is planned, structured, performed repeatedly, and specifically aimed at improving the physical fitness level [6]. Physical fitness comprises the ability of performance including cardiopulmonary endurance, muscle strength, flexibility, and coordination [6, 7]. Cardiorespiratory fitness is determined by the maximal cardiovascular exercise capacity and is dependent on oxygen transport via lung diffusion, cardiocirculation to the muscle fiber, where it is used in the mitochondria for energy production (ATP synthase). Assessment of maximal oxygen uptake (VO2peak/max) is the gold standard for evaluating cardiorespiratory fitness, typically assessed during a maximal exercise tolerance test performed on a bicycle or treadmill ergometer [8]. Maximal exercise capacity is the highest power output a person can sustain during an exercise tolerance [8]. Exercise tolerance is defined as the highest power output possible before any pathological symptoms and/or medical indications occur [9]. In a healthy person both terms can be used interchangeably, but in a patient the range can differ substantially [8]. For the definition of the amount of physical activity or exercise, the interrelation between the total dose of activity and the intensity at which the activity is performed have to be considered (volume of exercise = duration × intensity). While the dose refers to the total energy expended, intensity reflects to the rate of energy expenditure during the physical activity. Absolute intensity reflects the rate of energy expenditure during exercise, usually expressed in metabolic equivalent tasks (MET). One MET is the energy expenditure or oxygen consumption (VO2) measured during sitting, which equals 3.5 mL O2 kg−1 min−1. MET-hours are the product of exercise intensity and exercise time [6]. Relative intensity refers to the percent of aerobic power utilized during exercise. It is expressed as percent of maximal heart rate or percent of VO2peak. In this context, activities performed at a relative intensity of <40 % VO2peak are considered to be of light intensity, those performed at 40–60 % VO2peak to be of moderate intensity, and those performed at relative intensity of >60 % VO2peak to be of vigorous intensity [6]. For the estimation of intensity, the person’s individual premises have to be taken into account. For example, brisk walking at 4.8 km h−1 has an absolute intensity of ~4 MET. For a young and healthy person, this intensity is low in relative terms, but represents a vigorous intensity for an 80-year-old person.
Exercise therapy “is medically indicated and prescribed exercise, planned and dosed by therapists, controlled together with the physician and carried out with the patient either alone or in a group” [10]. Sport and exercise therapy “is an exercise based therapeutic measure which compensates for destroyed physical, mental and social functions with suitable sports remedies, regenerates, guards against secondary damage and supports health oriented behaviour. Sport therapy is based on biological principles; especially includes physiological, medical, pedagogic-psychological as well as social therapeutic elements and attempts to create enduring health competence” [10].
2 Objective of Exercise-Based Training Intervention
The primary objective of an exercise-based training intervention in cardiac rehabilitation is to positively influence disease progression and prognosis. This is most successfully achieved in coronary heart disease (CHD) and its pathological consequences (acute coronary syndrome, sudden death, ischemic heart failure) and in nonischemic chronic heart failure [1, 2, 6, 11–17]. The main secondary objectives are an improvement in the symptom-free exercise tolerance and overall quality of life [6, 12–14]. Further secondary objectives are overcoming cardiovascular and musculoskeletal limitations caused by inactivity (in particular in chronic heart failure and after open-heart surgery), as well as to improve mobility, independence, psychological well-being, social and occupational reintegration, and cardiovascular risk factors and thereby reduce the need for future home care, enhance participation, and enable the patient to take up his further life. In order to achieve these objectives, an extensive physical activity counseling including individual instructions is of crucial importance, in addition to the supervised exercise training [6, 11, 12, 14, 16–19].
Individual objectives should be based on the patient’s cardiac diagnosis, exercise capacity, possible exercise-limiting comorbidities, age, gender, exercise experience, as well as the patient’s motivation, personal exercise goals, and preferences. Respecting somatic, psychosocial, and educative objectives, they should aim to support the patient’s health-oriented behavior, to create his/her persistent health competence, and to improve his/her self-efficacy (Table 4.1 and Fig. 4.2).
3 How to Set Up an Exercise Training Program in Cardiac Rehabilitation
Exercise training in cardiac rehabilitation should be medically supervised and led by an experienced exercise therapist (or physiotherapist). During the initial phase after an acute event, the exercise program should be started under careful medical supervision. The supervision should include physical examination, monitoring of heart rate, blood pressure, and rhythm before, during, and after the exercise training [12, 14, 17]. A careful supervision allows to verify individual responses and tolerability, clinical stability, and promptly identifying signs and symptoms indicating necessary modification or termination of the program. The supervision should be prolonged in patients with high risk of cardiovascular events (severe coronary heart disease, heart failure NYHA III, ventricular arrhythmias, implantable cardioverter defibrillator (ICD), heart transplantation). In these patients an inpatient cardiac rehabilitation setting is recommended [12].
Exercise training in cardiac rehabilitation should be prescribed on an individualized approach after a careful clinical evaluation including: risk stratification, symptom-limited exercise testing (either on bicycle or on treadmill), assessment of possible exercise-limiting comorbidities, assessment of functional capacity (especially in groups at risk to have reduced functional capacity, e.g., older patients, females, and/or heart failure patients), assessment of behavioral characteristics (movement and exercise experiences, physical activity level, readiness to change behavior, self-confidence, barriers to increase physical activity, as well as social support in making positive changes), and patient’s personal goals and exercise preferences. The type and severity of the disease also have to receive similar attention such as personal characteristics like age and gender [12, 14, 17] (Fig. 4.3).
Exercise training in cardiac rehabilitation should be based on aerobic endurance training. On its basis, further components such as resistance exercise and gymnastics including exercises for coordination (inclusive balance and sensorimotoric), flexibility, agility, and strength as well as perceptional training, are to be added. In frail and older patients, special exercise elements for preventing falls should be a part of the exercise program (Fig. 4.4).
Based on the results of the clinical evaluation, every person should receive individualized exercise training recommendations containing the following information [14] (Fig. 4.5):
-
Exercise training goals (i.e., improvement of exercise capacity, muscular strength)
-
Exercise training mode (i.e., aerobic endurance training, moderate resistance training)
-
Exercise training content, with reference to the preferred type of exercise (i.e., bicycle ergometer, treadmill, walking, Nordic walking, etc.; resistance training using weight machines, elastic bands, etc.)
-
Exercise training method (steady-state training, interval training, etc.)
-
Exercise training intensity (i.e., % HRpeak, % VO2peak, % of one repetition maximum)
-
Exercise training duration (duration of the individual training unit [i.e., 30–60 min] and the supervised training program [i.e., 3–6 months])
-
Exercise training frequency (i.e., 3–7 exercise units per week) [12]
Exercise training duration, intensity, and frequency should start at a low level and be increased incrementally. Especially in patients taking up an exercise training after a long period of inactivity, it is important to pay close attention to the variation in time each organ system needs in order to adapt to the training process. While the cardiovascular and muscular systems show a fast adaptation, bones, tendons, ligaments, and joints adapt very slowly. The primary goal should be to increase training duration and frequency [12]. If these are well tolerated, then the intensity can also be increased.
Exercise training should be planned in three stages: initial stage, improvement stage, and maintaining stage (Fig. 4.6) [12, 14, 17].
The objectives of the initial stage are to prepare the patient for the exercise training and to verify the individual response and tolerability to a low-intensity exercise program. This phase also includes improvement of coordination and flexibility as well as developing the patient’s perception for exercise intensity. Previously physically inactive people and older patients have to receive special attention. In the initial stage the intensity of exercise should be kept at a low level. According to perceived symptoms and clinical status, the duration of the exercise unit can be prolonged (i.e., from 15 to 30 min). The duration of the initial stage depends on the patient’s clinical status and exercise tolerance, but should not exceed 4–6 exercise units during 1–2 weeks, respectively.
The objectives of the improvement stage are to gradually increase exercise capacity and other components of physical fitness such as coordination, flexibility, muscular strength, and endurance capacity. During this stage, the exercise intensity should be gradually increased according to the patient’s exercise prescription and exercise goals. Likewise, each exercise session can be prolonged up to 30–60 min and even beyond as well as exercise frequency can be increased up to daily sessions. However, this has to be adapted to the patient’s objective medical status and subjective health status.
The objectives of the maintenance stage are to stabilize and preserve the improvements achieved as well as extend them over a long period of time. Exercise intensity, exercise duration, and exercise frequency can be gradually increased if tolerated. In this stage, special attention has to be paid to the patient’s motivation as well as education to increase and or stabilize adherence to regular physical activity and exercise training. It is mandatory to provide the patient with the necessary practical skills of self-control and adequate handling during physical activity and/or exercise training. Careful instruction about the impact and health benefits of regular physical activity and exercise training might be helpful to improve his/her adherence to a physically active lifestyle.
Overall, during cardiac rehabilitation the individual exercise training recommendations have to be adapted individually and reevaluated after change of medical status, change of medication, hospitalization, or other illnesses.
4 Physical Activity Counseling: Motivation to a Physically Active Lifestyle
Provided they are performed on a regular and a long-term basis, physical activity and exercise training are valuable sources of multiple health benefits. The patient’s motivation to take up an active lifestyle and start regular exercise training on a sustained basis is therefore an important goal of the cardiac rehabilitation program. Investigations have shown that the patient’s thorough information and motivation provided by the attending physician is the most effective instrument to achieve such behavioral changes [21]. Based on this initial encouragement by the physician, the motivation achieved has to be stabilized and augmented through individual as well as group counseling during the rehabilitation process.
The primary preventive role of regular physical activity is well established by large epidemiological studies. Results of meta-analyses demonstrate regular physical activity compared with sedentary behavior to be associated with reduction of overall mortality rate by 22–36 % and reduction of cardiovascular mortality rate by 25–35 % [22–25]. The impact of regular physical activity in the secondary prevention of CHD is less well established. The results of smaller prospective studies demonstrate the prognostic importance of regular physical activities after diagnosis of the CHD, showing regular physical activity to be associated with a relative risk reduction of overall mortality by 19–58 % and cardiovascular mortality and/or morbidity by 20–62 % [26–35]. These prospective cohort studies [27, 32] also showed that it is never too late to take up an active lifestyle. They found reduced overall mortality rate by 29–50 % in former inactive CHD patients that increased their activity levels after the diagnosis of the disease [27, 32]. A relative reduction for overall mortality by 34–79 % was found in anciently physically active patients that maintained active, compared to those who were sedentary before and after the diagnosis of the disease [27, 32]. These results have to be established by studies with greater cohorts. Thereby in cardiac rehabilitation, it is important to emphasize sedentary lifestyle as an independent risk factor and explain the health benefits achieved by any increase in physical activity to the patients. However, the exercise therapist should keep in mind that it is not sufficient to inform the patient about the achievable health benefits. During the rehabilitation process, the patient’s perceptions, attitude, and health esteem regarding physical activity and exercise training have to be influenced positively. It is important that he/she experiences the exercise training provided during cardiac rehabilitation as a convenient task that he/she can cope with as well as an activity that is associated with well-being, fun, and social contacts. On a long-term basis, the patient will only integrate physical activity and exercise training into his/her daily life, if medical benefits are associated with personal values. The motivation to be physically active for health benefits usually only lasts for few months [36]. It is essential to change the patient’s secondary motivation (exercise training for health) into a primary motivation (e.g., I like exercise training, it is associated with fun, well-being, and/or meeting friends); otherwise he/she will return to his/her inactive lifestyle within a short period of time.
During the cardiac rehabilitation program, the patient should receive individual advices and exercise prescription for his/her physical activity and exercise training after the termination of the program and get the opportunity to put those into practice under supervision. These individual advises should take into consideration the patient’s age, gender, past habits, comorbidities, preferences, and goals. The patient’s readiness to change behavior, his/her self-confidence, and/or social support in making positive changes as well as possible barriers to increase and take up independent exercise training should be addressed. The participation in long-term maintenance programs like heart groups should be recommended if available.
5 Perception Training, Body Awareness, and Practical Skills of Self-Control
After an acute cardiac event (acute coronary syndrome, PCI, or cardiac surgery), most of the patients are uncertain regarding physical activity overall and, particularly, how much physical stress they are able to tolerate and what kind of physical activity they are allowed to perform. This uncertainty in combination with the experience of the vulnerability of the heart results in the avoidance of any physical strain and foster physical inactivity. Other patients rather tend to mentally suppress the cardiac event that might assimilate a danger of overload. During the exercise training, the patient has to learn the limit of his/her exercise tolerance and his/her exercise limits. The goal is to achieve the patient’s realistic judgment as well as his/her acceptance of the often considerable reduced exercise tolerance. The exercise training is an optimal instrument to improve the patient’s body awareness and perception. The experience of subjective and objective symptoms that occur during exercise training should be used to help the patient to recognize such symptoms as well as estimate their relevance for the load achieved. Improving body awareness and perception should therefore be an integral component of each exercise training, explaining the exercise procedure and its beneficial as well as possible adverse effects on the body to the patient. Through the exercise training, the patient should learn to perceive and observe his/her local and systemic reactions (i.e., increased heart rate, respiration, level of exertion of the muscle, subjective well-being, etc.) and to interconnect them to the objective exertion performed. By gradually increased exercise intensity, the patient should perceive the limit of his/her exercise tolerance in order to be able to recognize it. The exercise therapist should communicate with the patient asking him/her to prescribe his/her perceptions of objective and subjective symptoms during exercise. These practical skills of self-control are the fundamental instruments for the patient’s safe and effective approach to physical activity and training. This will reduce anxiety and improve a certainty regarding physical exertion during occupation, recreation, or daily life (Fig. 4.7).
6 Aerobic Endurance Training
Oxygen consumption (VO2peak) assessed by means of cardiopulmonary exercise testing is one of the strongest predictors of disease prognosis in patients with coronary artery disease and chronic heart failure [36–42] (Fig. 4.8). In CHD patients every 1.0 ml/kg1 min1 increase in VO2peak is associated with 15 % decrease in risk of death, 14 % (in women) and 17 % (in men) decrease in risk of overall mortality, and 10–14 % (in women) and 9–16 % (in men) decrease in risk of cardiovascular mortality [42]. Martin et al. [43] demonstrated in a retrospective analysis of a cohort of 5641 CHD patients that improvements in VO2peak achieved during cardiac rehabilitation have prognostic value. They found every increase in exercise capacity in one MET achieved during 12-week CR to be associated with 13 % reduction of overall mortality. In patients who started the CR program in the lowest fitness group, the benefit on exercise capacity was even of greater value. In this group an increase in one MET was associated with 30 % reduction of overall mortality.
The relative risk of death from any cause according to quintile of exercise capacity among subjects with and without cardiovascular disease (According to Myers et al. [41])
A systematically carried out aerobic endurance exercise program leads to an increase in exercise capacity and symptom-free exercise tolerance [13, 42–46]. In patients with cardiovascular disease, the increase in exercise capacity gained has been reported to range between 11 and 36 % [13, 45, 46] depending on the patient’s exercise tolerance, clinical status, as well as intensity and dose of the exercise training [13, 47–49]. Sedentary untrained and deconditioned patients have been shown to achieve the greatest benefits [13, 47–49]. In addition, long-term regular aerobic endurance training positively influences well-known cardiovascular risk factors such as hypertension, type 2 diabetes mellitus, dyslipidemia, and abdominal obesity [50–59] (Fig. 4.9).
6.1 Exercise Prescription and Definition of Individual Exercise Intensity
Based on careful clinical evaluation and risk stratification, including symptom-limited exercise testing, aerobic endurance training can be performed in a safe and an effective manner [3, 4, 46].
In addition to the maximal achieved exercise capacity, the intensity that the patient is able to tolerate without any pathology (exercise tolerance) is to be well defined and taken into account when exercise prescription is given.
Absolute contraindications to aerobic endurance training are summarized in Table 4.2 [14].
6.1.1 How to Define Exercise Intensity
Training intensity should be established and controlled based on the results of a maximal exercise stress test done on a bicycle/treadmill ergometer including ECG and blood pressure monitoring. This should yield maximal heart rate, maximal exercise load in watts, possible ischemic threshold, and blood pressure response to exercise. These data will form the basis for determining the individual training load and training heart rate. Additional cardiovascular examinations or improvement of therapy has to be included, if cardiac complaints and/or symptoms arise during the exercise stress test. If complaints or symptom limitations persist, despite maximal therapeutic efforts, it is advised to keep the exercise load at a level free of symptoms and ischemia. It is generally recommended that the training intensity should be clearly below the ischemic threshold [11–13, 17].
The heart rate is an objective, easily determined parameter used to regulate and control exercise load in cardiac rehabilitation. The maximal heart rate (HR peak ) is the highest heart rate achieved prior to termination of an incremental exercise tolerance test due to subjective exhaustion or objective indications [8]. The training heart rate can be determined as percent of maximal heart rate (HRpeak). In cardiac rehabilitation a training heart rate of 65–75 % (if tolerated 80–85 %) HRpeak is recommended [17]. It is important to keep in mind that only the heart rate response to an exercise stress test performed under the patients actual medication can be used for exercise prescription. This applies especially to the use of ß-receptor blockers (Fig. 4.10).
The training heart rate can also be determined mathematically by using the Karvonen formula, in which the heart rate reserve (HRR) is calculated. The heart rate reserve is the difference between maximal heart rate and resting heart rate, as determined in maximal exercise stress test (Fig. 4.11).
In cardiac patients training heart rate of 40–60 % (if tolerated 65–70 %) of heart rate reserve is recommended [17]. The heart rate reserve method should especially be used in patients with chronotropic incompetence. The training heart rate should always be determined clearly below the ischemic threshold (i.e., 10 beats/min).
Maximal exercise capacity measured in watt is a reliable and reproducible parameter in order to regulate exercise training performed on a bicycle ergometer [11]. In cardiac rehabilitation exercise intensity at 40–60 % (if tolerated up to 70–80 %) of maximal load (watt) achieved in a symptom limited exercise test is recommended [17]. In patients with very low exercise tolerance, very low heart rate reserve, as well as with the inability of the sinus node to react adequately to exercise stress by increasing heart rate (i.e., patients with chronotropic incompetence, atrial fibrillation, pacemakers, and post-heart transplant), training intensity should be controlled according to exercise load in watts and by using the Borg scale.
The Borg scale (rate of perceived exertion (RPE)) is used to subjectively assess how the individual perceives the intensity of the performed exercise on a scale from 6 to 20 points [60] (Fig. 4.12). It is not advisable, however, to solely rely on the Borg scale to advise on training load as it contains too many influencing factors from the patient’s perspective (i.e., unfamiliar method, poor body awareness, over motivation, and peer pressure) [61]. The Borg scale can be used as a supplement to other training regulation options, as well as to facilitate developing body awareness to the exercise load. Target values are RPE 11–14, comparable to light to moderate exercise intensity [17].
The maximal oxygen consumption (VO 2peak ) reached during an exercise stress test and the oxygen consumption at the anaerobic threshold (VO2-AT) are meaningful parameters in regulating exercise load during training [62]. The latter can also be determined during submaximal exercise testing, independent of the individual’s motivation level [63]. If a cardiopulmonary exercise test is used to determine aerobic training intensity then 40–70 % of VO2peak (up to 80 % if tolerated) should be targeted, close to the individual’s anaerobic threshold (1st VAT) [17, 64] (Fig. 4.13).
6.1.2 Aerobic Endurance Training Duration and Frequency
Health benefits can only be reached and maintained with long-term aerobic endurance training done on a regular basis. Aerobic endurance training should be performed for ≥30 min 3–5 times per week, preferably everyday, resulting in a total exercise time of ≥150 min per week (or 21/2 h/week). Ideally, exercise time should be around 3–4 h/week. The initial aerobic endurance exercise phase should last around 5–10 min in untrained individuals and gradually increase to ≥30 min per training session during the course of the training program. Low-intensity physical activities, such as walking in plane, can and should be done on a daily basis (preferably more than once a day) [12, 14, 17].
6.1.3 How to Perform Aerobic Exercise Training
The most common training forms used in cardiac rehabilitation to improve aerobic endurance are ergometer training on a cycle or treadmill. Additional common aerobic exercise modes include walking, Nordic walking, and biking. Jogging may be performed in those with good exercise capacity. This holds also true for swimming, as only those with stable cardiac condition without ischemia or potential for life-threatening should perform swimming. The decisive factors in choosing an appropriate training form in cardiac rehabilitation should be the ability to exactly dose, control, and gradually increase the appropriate exercise intensity, and the availability to monitor vital parameters (i.e., ECG, heart rate, blood pressure) is necessary.
When choosing a training form, an individual’s baseline characteristics (such as age, gender, exercise experience, exercise tolerance, and concomitant diseases) as well as preference and motivation must be considered. For overweight and obese individuals, non-weight-bearing exercise modes should be chosen (i.e., biking, bicycle ergometer training, and swimming). Walking and Nordic walking can be considered, if there are no pre-existing joint problems.
6.1.3.1 Aerobic Endurance Training on a Cycle Ergometer
In phase II of cardiac rehabilitation, aerobic endurance training on a cycle ergometer is recommended as standard procedure. The advantages of this training form are that it is non-weight bearing and enables the exercise load to be precisely dosed, independent of the patient’s body weight. Moreover, the minimal upper body motion enables blood pressure and ECG to be monitored at a high-quality standard during exercise. This type of exercise can be performed in an upright or supine position, and special safety equipment is available to facilitate patients with special needs, for example, extremely obese subjects, elderly insecure patients, or patients with history of stroke (Fig. 4.14). Computer-controlled cycle ergometer training and monitoring systems, specially designed for the use in cardiac rehabilitation, are available. Cycle ergometry can be performed as group training or at an individual basis. Training should be performed on an electrically braked cycle ergometer 3–5 times per week. If possible, it should be taken advantage of everyday the cardiac rehabilitation program is offered.
Endurance training (i.e., 10–30 min) is the most effective method to improve aerobic endurance capacity. Every exercise unit on the cycle ergometer should be constructed in four phases (Table 4.3 and Fig. 4.15).
Table 4.4 shows the recommendation for the implementation of moderate-intensity-continuous-endurance training in cardiac rehabilitation [17].
The safety and efficiency of moderate-intensity-continuous-aerobic training in patients with cardiac diseases is well established and therefore recommended as a standard training modality in cardiac rehabilitation in international guidelines and position papers. In primary prevention it is well known that higher exercise volume aerobic exercise training is more effective to improve exercise capacity and to reduce overall mortality. On the other hand by increasing the intensity similar effects can be achieved by shorter exercise boots [66]. Results of a meta-analyses [22] demonstrate an inverse relationship between exercise intensity and overall mortality, which was independent of age and gender. The question is if vigorous aerobic exercise training is also safe, effective, and well tolerated in cardiac patients. An interval-training mode would allow to exercise with at least short high-intensity bouts alternating to bouts of low or moderate intensity. In fact in the last decade, some studies with high-intensity interval training (HIIT) in cardiac patients have been carried out. The results prove HIIT to be beneficial [67, 68] and safe [69] in CHD patients [67–75] as well as in patients with markedly reduced exercise capacity (i.e., severe chronic heart failure) [76–80]; however long-term effects are still equivocal. In cardiac rehabilitation mainly two types of interval trainings protocols have been in focus of science and implementation: sprint or short-term interval training and high-intensity interval training (HIIT).
The type of sprint or short (term) interval training mostly used in cardiac rehabilitation is characterized by alternating short bouts of high-intensity exercise (20–30s) followed by a long recovery phase at minimal load typically twice the length of the exercise bout (ratio of exercise time: recovery time = 1:2) (Fig. 4.16 and Table 4.5). The advantage of this type of training is that the short bout of high-intensity exercise stimulates peripheral adaptations in the leg muscles to take place without compromising an overload in central mediation. The exercise intensity can be determined as a percentage of maximum load (wattpeak) achieved during a symptom-limited exercise stress test. An intensity as high as 85–90 % of wattpeak is usually recommended. Conclusive evidence base concerning the safety and efficiency of this type of training is only preliminary and must be confirmed by randomized controlled studies [14, 17].
Within the last few years, the safety and the efficacy of the 4 × 4 min high-intensity interval training protocol (HIIT) (Table 4.5 and Fig. 4.17) has been in the scientific focus for its use in cardiac rehabilitation. Meta-analysis including the results of few small, randomized controlled studies comparing the efficacy of HIIT to moderate-intensity-continuous-endurance training has revealed HIIT to be more effective in improving exercise capacity measured as a VO2peak. A meta-analysis of nine studies (206 CHD patients) [67] revealed HIIT to increase VO2peak a 1.60 mL/kg−1/min−1 more than moderate continuous training. High-intensity interval training resulted in a significant larger benefit in VO2peak compared to moderate continuous training (MCT) in patients with CHD (HIIT 20.5 % vs. MCT 12.8 %; p < 0.001). A second meta-analysis of six studies (229 CHD patients; EF < 40; 99 were randomized to HIIT) confirms these results [68]. Patients in the HIIT group improved their VO2peak by 1.53 mL/kg−1/min−1 more than those in the MCT group. The authors point out that small sample sizes and the large inconsistency and heterogeneity between the study results in the included studies limit the informational value of this meta-analysis. On the other hand, a recently published larger randomized controlled study (200 CHD patients; EF > 40 %) comparing HITT versus MCT does not confirm these results [74]. The results show no advantage for one of the exercise modalities (HIIT: 23.5 ± 5.7 vs. 28.6 ± 6.9 mL/kg−1/min−1; +22.7 %; MCT: 22.4 ± 5.6 vs. 26.8 ± 6.7 mL/kg−1/min−1; +20.3 %; p (time) =0.001; p (interaction) = ns) [74]. Both 12-week interventions equally improved VO2peak, peripheral endothelial function, as well as quality of life in CHD patients. Both programs seem to be safe for CHD patients, and no adverse events were reported during the exercise sessions. The authors’ experience was that the implementation of the 4 × 4 HIIT protocol with the target intensity of 90–95 % of HRpeak is hardly feasible in CHD patients. The mean intensity achieved in the HIIT group was 88 % of HRpeak compared to mean intensity of 80 % HRpeak in MCT group. These results demonstrate the impact of sufficient training intensity in continuous exercise training, which may, if tolerated, be more than the generally recommended 65–75 % of the HRpeak. Rogmore et al. [69] evaluated the risk of cardiovascular events during organized high-intensity interval exercise training (HIIT 85–95 % HRpeak) and moderate-intensity training (MCT 60–70 % HRpeak) among 4846 patients, primary with coronary heart disease. The results indicate that the risk of a cardiovascular event is overall low during both high-intensity exercise and moderate-intensity exercise in a cardiovascular rehabilitation setting (MCT, one fatal cardiac arrest (1 per 129,456 exercise hours); HIIT, two nonfatal cardiac arrests (1 per 23,182 exercise hours)). In a recently published study, a significant correlation between the changes in physical fitness during the intervention and the physical activity levels after the 1-year follow-up was found, indicating that patients who improved their physical fitness more had a higher motivation to adopt a physically active lifestyle following cardiac rehabilitation [80, 81].
A meta-analysis of seven randomized trials comparing the results of HIIT vs. MCT in heart failure patients (mean LVEF 32 % ) showed high-intensity interval training (HIIT) to be more effective for improving VO2peak than traditionally prescribed moderate-intensity continuous aerobic training (MCT) (WMD 2.14 mL VO2/kg/min, 95 % CI 0.66–3.63). The comparison of the effects on the left ventricular ejection fraction (LVEF) at rest revealed inconclusive results (HIIT vs. MCT: WMD 3.3 %, 95 % CI −0.7–7.3 %) [79]. An interesting meta-analysis stratified aerobic exercise studies in heart failure patients by activity intensity [80]. The results revealed the magnitude of improvements in cardiorespiratory fitness to be greater with increasing intensity, unrelated to baseline fitness levels or exercise volume. The largest improvement in VO2peak was observed with high-intensity training (23 %) showing a linear decrease in effect size with decreasing exercise intensity (vigorous intensity 16 %, moderate intensity 13 %, low intensity 7 %, respectively). Exercising with high or vigorous intensity seems to be well tolerated in heart failure patients, especially if interval protocol is used. Furthermore studies of continuous exercise training used a greater volume (duration) of exercises and some of them multiple daily sessions. In high-intensity exercise programs, the volume of work is completed in shorter time and may therefore require shorter session duration and lower exercise frequency that might influence the patient’s adherence to the exercise program [80]. Moreover this analysis also demonstrated exercising with higher intensity in heart failure patients to be safe, showing no increased risk of death, adverse events, or hospitalization in the high- and vigorous-intensity exercise groups [80]. These interesting results must be confirmed by more prospective randomized controlled studies, with greater cohorts and longer follow-up period, though, before definite recommendations can be given [14, 17]. Furthermore until now the prognostic value of high-intensity interval training have not yet been evaluated neither in CHD nor in heart failure patients.
For the implementation in cardiac rehabilitation, the more scientific discussion of intensity and exercise mode allows to derive the knowledge that aerobic exercise of any intensity of continuous or interval mode seems to be effective to improve exercise capacity in cardiac patients. Exercising with high or vigorous intensity leads to greater improvements than exercising with moderate or low intensity. Higher intensity seems to be better tolerated, if the exercise training is carried out with an interval mode, which allows resting periods between the high or vigorous exercise bouts. In the general praxis of cardiac rehabilitation, it is in the responsibility of the exercise therapist in agreement with the CR physician to decide, which exercise intensity and exercise mode fits best for the individual patient. Rigid interval protocols might not be optimal for every patient. The exercise specialist should consider modification in order to adapt the program to the individual capability of the patient.
Thus high-intensity interval training is not an alternative for continuous aerobic exercise training but could be an effective and well-tolerated supplementary approach for aerobic endurance training in cardiac rehabilitation.
6.1.3.2 Other Forms of Aerobic Endurance Training in Cardiac Rehabilitation
To further improve aerobic endurance, other forms of exercise such as walking, Nordic walking, slow jogging, and cycling can be added to the individual’s training program depending on the patient’s preference and exercise tolerance. This also applies to phase II of cardiac rehabilitation.
Endurance training in form of walking improves the physical fitness and has a positive influence on numerous cardiovascular risk factors [83–85]. Going for a walk or walking in general (brisk walking with deliberate arm movement) are ideal types of aerobic endurance exercise for getting started for unfit individuals, the elderly, and/or postmenopausal women, without risking an overload of the cardiopulmonary system.
Organized rehabilitation programs should provide the opportunity for all patients to take part in supervised walks and walking programs provided that patients meet necessary exercise tolerance criteria and are without adverse comorbidities. The walking terrain, walking pace, and duration should be tailored to the needs of the participating patients. The benefit of walking programs is their applicability in everyday life, which makes them ideal to motivate patients to increase their daily physical activity. They also offer an excellent opportunity to improve the patient’s body perception and self-awareness. By becoming familiar with exercise parameters like heart rate, breathing frequency, well-being, and level of exhaustion, the individual can translate this experience into his/her every day activities. Exercise intensity can be controlled by the target heart rate for aerobic endurance training. This approach is applicable to most types of endurance exercise.
The use of walking poles (“Nordic walking”) can somehow increase exercise intensity by increasing muscle recruitment. This translates into higher oxygen uptake (up to + 4.4 ml.kg−1.min−1) and overall energy expenditure (up to +1.5 kcal.min−1) [86]. Further advantages of Nordic walking include a reduction in weight bearing on the joints and an increase in body stabilization due to the walking poles (especially during downhill walking) [87, 88]. During recent years Nordic walking has become extremely popular and is well tolerated especially by elderly and female patients. To utilize the advantages of this exercise form, correct technique should be emphasized. Exercise intensity can be controlled by means of target heart rate for aerobic endurance training [88] (Fig. 4.18).
Biking is an ideal endurance and recreational sport for persons of all age groups. Organized rehabilitation programs typically provide biking tours and can be applied in cardiac rehabilitation as well. Special attention should be paid to the suitability of the bike (i.e., touring bike with many gears, e-bike, good transmission, suspension, and a comfortable saddle), the terrain (solid leveled surface), as well as the safety (helmet). The experience gained from supervised biking tours during the rehabilitation program can be motivating to the patient in order to implement this activity into his/her everyday life. Biking on a solid leveled surface is a non-weight-bearing activity and is well suited for patients with low exercise tolerance. Alternatively, a motor-assisted pedal cycle can be used; however lower exercise intensity has to be taken into account. Exercise intensity can be controlled by the target heart rate for aerobic endurance training.
In patients with very good exercise tolerance, endurance running (jogging) is one option to improve aerobic endurance capacity and to positively influence cardiovascular risk factors. Even this mode of exercise can be modified regarding intensity from slow to rather fast jogging, the former also termed “wogging.” Maximal adaptations can be achieved with minimal efforts during this type of exercise [8]. Exercise intensity can be controlled by the target heart rate for aerobic endurance training.
7 Resistance Exercise Training
The objective of resistance exercise training is to increases muscular strength by performing static or dynamic muscle contractions. While dynamic (isotonic) exercise is performed by movement of the joint, static (isometric) exercise does not result in movement of the joint. Most physical activities comprise both dynamic and static contractions and are therefore classified based on their dominant characteristics.
In cardiac rehabilitation resistance training programs include primarily dynamic repetitions with both concentric (muscle shortening) and eccentric (muscle lengthening) muscle actions. Isometric muscle actions play a secondary role [89].
Muscular hypertrophy is defined as the increase in total muscle mass. Hypertrophy training is intensity dependent and dominated by isometric contractions (muscle contraction without changes in muscle length), which is not in focus in cardiac rehabilitation. Muscular endurance is the ability to sustain muscular strength over an extended period of time with minimal decrease in power output and is composed of dynamic contractions [8].
The exercise intensity of dynamic resistance training is determined using the one-repetition maximum (1-RM) method [90], often not assessing 100 % but rather submaximal values in cardiac patients (Sect. 4.7.5).
7.1 The Impact of Resistance Exercise in Cardiac Rehabilitation
Resistance exercise can lead to an increase in muscular strength and muscular endurance by increasing muscle mass and/or improving coordination and muscle metabolism [91–93]. It is known to have diversified health benefits, i.e., reduced loss in muscle mass and strength associated with heart disease or old age, as well as increased exercise and functional capacity, to positively influence several cardiovascular risk factors, to improve mobility, participation, and quality of life [17] (Table 4.6).
In many cases (especially in elderly patients) the loss in muscle mass and strength is associated with heart disease or old age, the essential reason for reduced everyday activity levels, mobility, and participation. Thus in these patients the improved ability to develop muscular strength can influence the quality of life decisively. Adequate individualized resistance training positively influences the ability to carry out everyday activity; improve the patient’s self-confidence, independency, and psychosocial well-being; as well as avert or reduce the need of nursing care. Improved proprioception mediated by adequate resistance training positively influence coordination and balance. Combined resistance and balance training improve stability and gait ability, enhance security of movement, and thus play a major role in preventing falls [92, 98].
Individualized and adequately dosed dynamic resistance training has been demonstrated to be safe and effective in cardiac patients and is encouraged by the current recommendations on exercise training in cardiac rehabilitation [1–13, 17, 49] (Fig. 4.19). This particularly applies to patients with coronary artery disease who possess good exercise tolerance and preserved left ventricular function. The results of a meta-analysis evaluating the efficacy of aerobic endurance training compared to combined programs of aerobic and resistance training in CHD patients revealed combined programs to be more effective in improving lower and upper body strength, body composition (decreased percent body fat and trunk fat and increased fat-free mass), and peak working capacity [99].
Blood pressure response during Valsalva maneuver (modified according to Graf [125])
Resistance training has also been shown to be well tolerated and effective in the elderly and/or female patients [108–112].
The efficacy and safety of resistance exercise in high-risk patients, that is, patients with chronic heart failure, has remained an ongoing discussion over the last decade. Numerous studies have been conducted exploring this topic, most of them including only a small cohort differing markedly in their research approach and research question. However, none of these previous studies has shown any increased cardiac risk associated with resistance training, which has proven overall effective. According to new scientific evidence, supervised individualized dynamic resistance exercise training at low-to-moderate intensity is a safe and effective training mode and should be prescribed in addition to aerobic exercise training. This helps to counteract muscle atrophy and peripheral changes typically seen in heart failure patients [17, 113–117].
It has to be noted though that only aerobic endurance training has shown to improve clinical prognosis. Comparable prospective studies focusing on surrogate endpoints do not exist for resistance exercise [17, 118]. In cardiac rehabilitation the implementation of adequately dosed resistance training is recommended to compliment aerobic endurance exercise training [17, 49] (Fig. 4.20). Absolute contraindications to resistance training are the same as absolute contraindications for aerobic endurance training (Table 4.2).
7.2 Blood Pressure Response During Resistance Exercise
It is well known that resistance exercise can result in an extreme increase in blood pressure, but it is also recognized that this does not necessarily have to be the case, if an appropriate training volume (weight, number of repetitions, sets) is chosen. It should be taken into account, when prescribing exercise, that the actual blood pressure response to resistance exercise is dependent on the amount of static (isometric) muscle contraction, the actual load (% of individual’s 1-RM) [119, 120], and the amount of muscle mass involved [121]. Blood pressure response is also dependent on the number of repetitions and total duration of muscular contraction [122] as well as repetition speed and rest periods [122]. The highest blood pressure response is reached, when multiple repetitions are performed at 70–95 % of 1-RM to exhaustion, since it is equally affected by both intensity and duration. Exercise load below 70 % of 1RM as well as duration of muscular contraction above 95 % of 1-RM are insufficient to elicit a significant rise in blood pressure response [124].
A dynamic resistance training with low-to-moderate intensity allows a high number of repetitions (muscular endurance training (15–30 reps), moderate hypertrophy training (10–15 reps)) without evoking any major rise in blood pressure. The blood pressure response during this type of training is lower compared to the increase in blood pressure seen during moderate endurance training.
If the Valsalva maneuver (a forced expiration is invoked against the closed glottis) is carried out during resistance exercise, the rise in blood pressure is more pronounced. The Valsalva maneuver leads to an increase in intrathoracic pressure, which, in turn, leads to a decrease in venous return and potentially reduction in cardiac output [124]. The physiological response includes an increase in heart rate to maintain cardiac output and peripheral vasoconstriction to maintain blood pressure, which otherwise may decrease with decreasing cardiac output. Once the imposed strain is released, there is a dramatic increase in venous return and subsequently an increase in cardiac output being forced through a constricted arterial vascular system. The dramatic rise and drop in blood pressure can limit myocardial oxygen delivery resulting in potentially dangerous arrhythmias and/or reduced perfusion of the coronary arteries leading to ischemia [124]. A rapid fall in blood pressure after straining at maximal workload sometimes results in syncope even in healthy persons [125] (Fig. 4.21).
Special attention should be paid to the Valsalva maneuver during resistance exercise training. Before starting the resistance exercise program, the patient should be educated about the complications potentially associated with the Valsalva maneuver. He/she should learn to pay attention to his/her breathing while exercising and learn to combine exercise and breathing in a way that enables him/her to avoid Valsalva maneuver. This should be a part of the preparation in the initial exercise stage.
7.3 Implementation of Resistance Training in Cardiac Rehabilitation
Exercise training in cardiac rehabilitation should be started by means of aerobic endurance training. Resistance training may be considered in phase II and phase III cardiac rehabilitation, but is contraindicated in phase I (hospital phase). Resistance training should be implemented as an alternative training mode, supplementary to aerobic exercise, and can be integrated into the training program after one or two sessions of continuous endurance trainings at the earliest.
In the absence of any adverse comorbidity, moderate-intensity dynamic resistance training is recommended for all low-risk patients with stable cardiovascular disease and good exercise tolerance (including myocardial infarction and/or interventional revascularization), moderate to good left ventricular function, no clinical signs of heart failure, and without symptoms of angina pectoris or ischemic ST segment depression during exercise stress test. Low-intensity resistance exercise training should not be started earlier than 2 weeks post-myocardial infarction and/or 7 days post-interventional revascularization. Combined endurance and resistance training (up to 60 % of 1-RM), delivered early after myocardial infarction, does not induce negative left ventricular remodeling and is associated with an increase in VO2peak and muscle strength [126].
In women with CHD, both aerobic endurance training and resistance training delivered within a cardiac rehabilitation program improve physical quality of life and VO2peak. However, within 1 year of follow-up, physical quality of life is significantly higher in women who participated in a combined training regime [127].
In patients recovering from coronary artery bypass surgery (CABG) and other open-heart surgery, exercise capacity can be extremely limited. After a thoracotomy and/or saphenectomy, the wound healing takes approximately 4–6 weeks. Physical exercise inducing tangential vector forces in or around the sternum (pressure or sheer stress) should be avoided for at least 3 months postoperatively. Before resistance training is started, the treating physician must confirm that the sternum is stable. If there are no complications during the postoperative course and the patient has a good exercise tolerance, a low-intensity resistance exercise training for the lower limbs can be carried out earlier, provided a stable trunk positioning is ensured. This may also be true for selected exercises of the upper body.
In heart transplant recipients, the continuous immunosuppressive therapy including cortisone often leads to muscle atrophy and decrease in bone mass. In addition, these patients usually have a poor musculoskeletal structure due to the long history of preceding severe cardiac disease and subsequent inactivity. Resistance exercise training has been demonstrated to show good effects in these patients [97, 98]. In clinically stable patients, individualized moderate dynamic resistance training should be started as soon as possible in the postoperative phase and should be continued on a long-term basis, to counteract the negative side effects associated with immunosuppressive therapy.
In patients with stable chronic heart failure, left ventricular function remains stable during moderate-intensity resistance training [128]. In these patients, the amount of exercise intolerance does not correlate with the degree of left ventricular dysfunction. It is well recognized that the reduction in exercise tolerance is also related to morphological, metabolic, and functional changes in the patient’s peripheral musculature. Several studies have demonstrated that adequate dynamic resistance training with low-to-moderate intensity may help to counteract the muscle atrophy typically associated with chronic heart failure. In stable patients with chronic heart failure (NYHA I-III), adequate resistance training is recommended in addition to aerobic endurance training [17, 113–117].
7.4 How to Perform Resistance Exercise Training
In cardiac rehabilitation resistance training should be medically supervised and led by an experienced exercise therapist/physiotherapist. Objective training goals should be modulated for each patient individually. The use of elastic exercise bands and/or small weights for resistance training is very suitable. This equipment is easy to use and allows individually tailored resistance training as well as group training. Further advantages are the easy storage and their low costs. However, particularly the use of elastic exercise bands must be carefully instructed to each patient to ensure that they are used in a safe manner.
More precise training with less risk of overloading can be achieved through the use of weight machines. They allow for higher precision in implementing individualized training programs and safe movement execution. For this type of training individual supervision is mandatory.
Resistance training is prescribed according to dosage parameters such as intensity (resistance), number of repetition, volume, frequency, and duration as well as rate of progression [89]. A lower repetition range with a heavier weight/resistance may better optimize strength and power, while a higher repetition range with a lighter weight/resistance may better enhance muscular endurance. Weight loads that permit 8–15 repetitions will generally facilitate improvements in muscular strength and endurance [124].
Table 4.7 shows recommendations for the implementation of resistance training in cardiac rehabilitation.
In the initial stage all patients should start training at very low intensity (< 30 % 1-RM) to learn and practice correct movement execution (familiarization). In the improvement stage I, the load should be increased gradually from 30 to 50 %. While elderly patients and/or patients with low exercise tolerance (i.e., heart failure patients) should start training at very low intensity (< 30 % 1-RM), trained patients with good exercise tolerance can start training at moderate intensity (50 % 1-RM), increasing first the number of repetitions and series and thereafter the intensity. In the improvement stage II, the load should be gradually increased (30–50 %1-RM and further up to 60 % 1-RM) based on the patient’s exercise tolerance and response to the resistance training. Higher training intensities (stage III) may be considered in well-trained patients with good exercise tolerance and low cardiac risk, who have already completed a 4–6 week resistance exercise training program [17, 124, 130].
After each set of exercises, a resting time of at least 1 min should be implemented [122]. In novice a frequency of three sessions per week is considered most effective. Once trained, and in order to maintain the desired level of strength, frequency can be reduced to two sessions per week [130, 131]. Between each session, there should be 1 day of abstinence from resistance training.
7.5 How to Determine the Appropriate Load of Resistance Training
The evaluation of muscle strength is indicated to prescribe individualized safe and effective resistance training intensities, to track the progress of an individual, as well as to evaluate the efficacy of resistance training regime. A number of methods for determining the intensity for resistance training exist. Laboratory-based methods include the use of isometric dynamometers and isokinetic dynamometers. In chronic heart failure patients, the use of isokinetic versus one-repetition maximum strength assessment has been demonstrated to be more accurate to assess changes in muscular strength with exercise training [132]. On the other hand, these methods require sophisticated laboratory equipment and personal trained in their use and in addition are not very specific for the types of movement patterns commonly used in typical cardiac rehabilitation regimes. The one repetition maximum test has been shown to be reliable for various populations, also in untrained middle-aged as well as old individuals [90]. The one repetition maximum is defined as “the maximum amount of weight/resistance that can be performed for only a single repetition for a given exercise, with a proper lifting technique, without compensatory movements and without breath holding” [90]. The evaluation of the 1-RM is the gold standard in dynamic resistance exercise testing. This method is comparatively simple and requires relatively inexpensive non-laboratory equipment (Table 4.8). The 1-RM test can be performed using the same patterns as those undertaken by the exercising individuals during their normal training. Numerous studies have reported that the 1-RM method to assess muscle strength is safe for patients with cardiovascular diseases [133, 134].
The maximum strength a person can produce, the maximum weight a person can lift (i.e., the one repetition maximum), is not an absolute value and can be influenced by several factors, i.e., by psychological factors (i.e., motivation and/or external encouragement) and the testing protocol (i.e., with or without familiarization). The result may further be influenced by the quality of the test execution (proper lifting technique, range of motion, speed of movement, control for compensatory movements and breath holding, rest periods, and more) as well as the testing possibilities and equipment used [89, 133, 135]. Thus, it has to be kept in mind that the testing of 1-RM may have significant practical problems, making results unreliable. Many cardiac patients are old and weak. Thus the equipment used needs to have a low starting load and options for small increments in order to be able to test this population at all. It must also be considered that different types (manufacturer) of machines/equipment show variable results due to differences in the load transmission. Measured results on the one type of equipment cannot be transferred to training performed on another. Therefore it is strongly recommended always to perform the 1-RM test using the same equipment to be used for resistance training. A familiarization process prior to 1-RM strength testing is essential to avoid injury, for ensuring reliable test results, and minimize learning effect or systematic bias. This includes teaching (and practicing) correct lifting and breathing technique at very low load and/or using submaximal loads. In younger and experienced individuals, one session is sufficient; in older and/or inexperienced patients, multiple sessions are often necessary. Without a familiarization process prior to strength testing, there is a significant increase in the expression of muscle strength between two consecutive strength tests performed a few days apart [133]. Furthermore familiarization may reduce the risk of injury especially in patients, who have no previous lifting experience.
The results of one repetition maximum test can be used to determine the appropriate exercise load for resistance exercise training in cardiac patients. The intensity of training is specified according to a percentage of the one repetition maximum (1-RM).
An alternative, often used in cardiac patients, is the evaluation of a predictive one repetition maximum (testing 10 or fewer repetitions to fatigue) using the Brzycki’s equation to determine max load [136]. The use of a prediction equation for older adults appears also to be a valid measure of 1-RM. In older patients, the prediction equation have been shown to underestimate the actual 1-RM, but the error is small [133]. The use of the indirect method to estimate 1-RM is practical and safe and may even produce more accurate result especially in older unexperienced cardiac patients.
To avoid a maximal strength test (1-RM), which might lead to Valsalva maneuver and blood pressure evaluation, the correct intensity can also be found by using a graded exercise testing. Here, the patient begins with very low intensity that does not require much effort, and the resistance load is gradually increased to the point at which the patient can maximally achieve 10–15 repetitions in a correct manner without abdominal strain and symptoms [129]. The Borg scale can be used to assess the patient’s perceived exertion in addition to measuring objective physiologic parameters. In patients with moderate risk, perceived exertion (RPE) should be 12–13, not exceeding 15 (Table 4.9; Fig. 4.22).
In summary in exercise-based cardiac rehabilitation, the therapists do not need absolute maximal values of muscular strength, but need reliable values of strength performance to be able to set up an individualized safe and effective resistance exercise program.
8 Additional Contents of Exercise Training Program in Cardiac Rehabilitation
Physical exercises to improve flexibility, agility, coordination balance, muscular strength, and endurance should be an essential part of all comprehensive exercise training program in cardiac rehabilitation. The main objectives are to provide the premises for effective exercise training and prevent musculoskeletal injuries. Balance is required in many activities of daily living as well as recreational physical activities. Exercises to improve balance, kinesthetic differentiation ability, as well as other coordinative skills are of special importance to prevent falls in the elderly as well as in untrained individuals that are starting exercise after a long period of physical inactivity. Complimentary to resistance training especially balance training for static and dynamic balance is recommended. The balance training should be adapted to the patient’s abilities, starting with low levels of difficulty and include various progressions. The different level of difficulty and progression can be achieved by modifying the exercises used, for instance, as follows: decrease/increase the base of support (three separate stances: double leg, single leg, tandem), use different surfaces (ueven and/or uneven surface and medium density balance pad with even and or uneven surfache, etc.), use instable surfaces (use of tilt boards), modify optical control (eyes are open/eyes are closed), prevent the use of arms to help balance (arms crossed), and do supplementary task while balancing (i.e., catching ball).
To prevent overload and the risk of musculoskeletal injury, special attention should be paid to the appropriate exercise choices as well as to correct movement execution. All exercises performed have to be individually dosed and controlled by the exercise therapist. As the determination of the right exercise intensity is far more difficult in these exercises than in aerobic exercise, when the exercise therapist can use heart rate monitoring to control intensity, improving the patient’s body perception and awareness is of particular importance. For the supervision a careful control of adequate respiration and observation of symptoms of overload (i.e., exudation, blushing, incorrect execution of the exercise) as well as the use of subjective perceived rate of exertions (Borg scale) in combination with communication between patient and therapist are the instruments of choice. The avoidance of Valsalva maneuver is mandatory to prevent dangerous elevations in blood pressure.
The patient should be integrated into therapy groups according to their exercise tolerance, physical condition, existence of relevant exercise and/or mobility limitations, and/or comorbidities, age, and experience with physical activity and exercise.
According to the exercise tolerance, most rehabilitation centers differentiate at least between so-called chair groups (>0.3–0.5 watt/kg body weight), low-intensity exercise group (>0.5–1.0 watt/kg body weight), and moderate-intensity exercise group (>1.0 watt/kg body weight). In larger centers more distinctive differentiation according to exercise tolerance and rehabilitation indication, age, and gender groups can be followed.
In special indications, i.e., in patients after a thoracotomy and/or saphenectomy, special groups for the treatment of the postoperative consequences are needed. This special program should include breathing exercises and careful mobilization of the thorax to avoid and work against reliving postures and improve breathing quality as well as exercises to improve venous return. Physical exertion which causes tangential vector forces in the sternal area (pressure or sheering stress, i.e., caused by dissymmetric exercises) should be avoided. Due to the limited physical activity early after heart surgery, these exercises are usually performed in seated position.
Exercise intensity can be differentiated by changing individual speed of motion, exercise duration, muscle mass involved, amplitude of the movement, and the flexibility, strength, and coordination demand necessary to perform the exercise in an adequate and correct manner (Table 4.10).
To enhance motivation and interaction within the therapy group, the integration of modified movement games and team games into the exercise program is to be recommended. Small movement games with simple modifiable rules, which can be played in small groups with low organizational demand, are appropriate. If modified team games are to be integrated, games played on separated playing fields are most suitable. Due to the separate radius of activity, the exercise intensity as well as the risk of injury can be reduced. In general the intensity of movement and team games can be modified by changing the rules, reducing/increasing the playground, changing the number of players, reducing/increasing the distances to overcome, reducing/increasing the speed of movement, varying play equipments, etc. This allows adapting the game to the premises of the group and to integrate the playing activities into the exercise program without danger of overload. Because of the inadequate possibility to control the intensity, movement games with higher demand of muscular strength or aerobic endurance are unsuitable (Fig. 4.23).
9 Patient–Therapist Relationship
Exercise therapy is a core component of the cardiac rehabilitation process that usually is led by a specially educated therapist. He/she works with the patient at every visit to the rehabilitation center, often for several hours every week. Thus, of all therapists he/she learns to know the patient best during the rehabilitation phase. While exercising together a special patient–therapist relationship can be established. This opens the opportunities for informal talks about familiar and/or occupational pleasures and/or problems. The patients do not seldom open themselves to the exercise therapist about his/her problems coping with the disease, his/her insecurity, anxiety, motivation, preferences for lifestyle changes, as well as problems and barriers he/she experiences to fulfill the demands of the CR and lifestyle changes he/she is confronted with during CR program. Furthermore, the supervision of the exercise intervention gives the therapist the best opportunity to observe how the patient reacts. Is the program meeting his/her needs, interests, preferences, and/or motivation? Is he/she enjoying the participation, having fun? Is he/she relaxed, anxious, or depressed? Is the exercise intensity, volume, as well as the contents of the exercise program adequate? Do any symptoms, i.e., arrhythmia, ischemia, musculoskeletal problems, and problems related to comorbidities during exercise occur? Thus the exercise therapist captures a special role within the interdisciplinary cardiac rehabilitation team and can serve as an important connector between the patient and other members of the team, including the CR physician. As a “person of trust,” his information and “diagnosis” should be considered invaluable (Fig. 4.24).
In summary the therapist responsible for exercised-based intervention for cardiac rehabilitation has to keep in mind that exercise training is more than a matter of evidence-based medicine, endurance and/or resistance training, intensity, and volume of exercise. On a long-term basis, the benefit strived for will only be achieved if the rehabilitation team manages to motivate the patient to change her/his attitude and take up a regular physical activity and exercise training and optimally to continue this lifelong. In this regard the precondition for a self-controlled exercise training and the basic for the patient’s health competence are the improved patient’s body awareness and his/her practical skills of self-control. During the rehabilitation process, the patient’s perceptions, attitude, and health esteem regarding physical activity and exercise training have to be influenced positively. It is important that he/she experiences the exercise training provided during cardiac rehabilitation as a convenient task that he/she can cope with as well as an activity that is associated with well-being, fun, and social contacts. On a long-term basis, the patient will only integrate physical activity and exercise training into his/her daily life, if medical benefits are associated with personal values.
References
Heran BS, Chen JM, Ebrahim S, Moxham T, Oldridge N, Rees K, DR T, RS T. Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane Database Syst Rev. 2011;(8):CD001800.
Anderson L, Oldridge N, Thompson DR, Zwisler AD, Rees K, Martin N, Taylor RS. Exercise-based cardiac rehabilitation for coronary heart disease cochrane systematic review and meta-analysis. J Am Coll Cardiol. 2016;67:1–12.
Jolliffe JA, Rees K, Taylor RS, Thompson D, Oldridge N, Ebrahim S. Exercise-based rehabilitation for coronary heart disease. Cochrane Database Syst Rev Update. 2001;(1):CD001800. Update Software.
Taylor RS, Brown A, Ebrahim S, Jolliffe J, Noorani H, Rees K, Skidmore B, Stone JA, Thompson DR, Oldridge N. Exercise-based rehabilitation for patients with coronary heart disease: systematic review and meta-analysis of randomized controlled trials. Am J Med. 2004;116:682–92.
Clark AM, Hartling L, Vandermeer B, McAlister FA. Meta-analysis: secondary prevention programs for patients with coronary artery disease. Ann Intern Med. 2005;143:659–72.
Thompson PD, Buchner D, Pina IL, Balady GJ, Williams MA, Marcus BH, Berra K, Blair SN, Costa F, Franklin B, et al. Exercise and physical activity in the prevention and treatment of atherosclerotic cardiovascular disease: a statement from the Council on Clinical Cardiology (Subcommittee on Exercise, Rehabilitation, and Prevention) and the Council on Nutrition, Physical Activity, and Metabolism (Subcommittee on Physical Activity). Circulation. 2003;107:3109–16.
U.S. Department of Health and Human Services, Rdt. Physical activity and health: a report of the surgeon general. Atlanta: U.S Department of Health and Human Services. Centers for Disease Control and Prevention National Center for Chronic Disease and Health Promotion; 1996.
Hollmann W, Hettinger TH. Sportmedizin. Grundlagen für Arbeit, Training und Präventivmedizin, völlig neu bearbeitete und erweiterte Auflage ed, vol. 4. Stuttgart/New York: Schattauer; 2000.
Gielen S, Hambrecht R. Trainingstherapie – Theoretische Grundlagen und Evidenz. In: Rauch B, Middeke M, Bönner G, Karoff M, Held K, editors. Kardiologische rehabilitation. Stuttgart: Thieme; 2007. p. 70–8.
Deutcher Verband für Gesundheitssport und Sporttherapie. www.dvgs.de. [Web Page] 2016.
Balady GJ, Williams MA, Ades PA, Bittner V, Comoss P, Foody JM, Franklin B, Sanderson B, Southard D. Core components of cardiac rehabilitation/secondary prevention programs: 2007 update: a scientific statement from the American Heart Association Exercise, Cardiac Rehabilitation, and Prevention Committee, the Council on Clinical Cardiology; the Councils on Cardiovascular Nursing, Epidemiology and Prevention, and Nutrition, Physical Activity, and Metabolism; and the American Association of Cardiovascular and Pulmonary Rehabilitation. Circulation. 2007;115:2675–82.
Piepoli MF, Corra U, Benzer W, Bjarnason-Wehrens B, Dendale PAC, Gaita D, McGee H, Mendes M, Niebauer J, Olsen-Zwisler AD, Schmid JP. Secondary prevention trough cardiac rehabilitation. 2008. Update. From knowledge to implementation. A position paper from the cardiac rehabilitation section of the European Association of Cardiac Rehabilitation and Prevention. Eur J Cardiovasc Prev Rehabil. 2010;17:1–17.
Leon AS, Franklin BA, Costa F, Balady GJ, Berra KA, Stewart KJ, Thompson PD, Williams MA, Lauer MS. Cardiac rehabilitation and secondary prevention of coronary heart disease : an American Heart Association scientific statement from the Council on Clinical Cardiology (Subcommittee on Exercise, Cardiac Rehabilitation, and Prevention) and the Council on Nutrition, Physical Activity, and Metabolism (Subcommittee on Physical Activity), in collaboration with the American association of Cardiovascular and Pulmonary Rehabilitation. Circulation. 2005;111:369–76.
Bjarnason-Wehrens B, Schulz O, Gielen S, Halle M, Dürsch M, Hambrecht R, Lowis H, Kindermann W, Schulze R, Rauch B. Leitlinie körperliche Aktivität zur Sekundärprävention und Therapie kardiovaskulärer Erkrankungen. Clin Res Cardiol. 2009;4(Suppl. 3):1–44.
Sagar VA, Davies EJ, Briscoe S, Coats AJS, Dalal HM, Lough F, Rees K, Singh S, Taylor RS. Exercise-based rehabilitation for heart failure: systematic review and meta-analysis. Open Heart. 2015;2:e000163. doi:10.1136/openhrt-2014-000163.
Bjarnason-Wehrens B, Held K, Hoberg E, Karoff M, Rauch B. Deutsche Leitlinie zur Rehabilitation von Patienten mit Herz-Kreislauferkrankungen (DLL-KardReha). Clin Res Cardiol. 2007;(Suppl 2):III/1–III/54.
Vanhees L, Rauch B, Piepoli M, van Buuren F, Takken T, Börjesson M, Bjarnason-Wehrens B, Doherty P, Dugmore D, Halle M and (on behalf of the writing group of the EACPR). Importance of characteristics and modalities of physical activity and exercise in the management of cardiovascular health in individuals with cardiovascular disease (Part III). Eur J Prev Cardiol 2012;19:1326–1332.
Corra U, Giannuzzi P, Adamopoulos S, Bjornstad H, Bjarnason-Weherns B, Cohen-Solal A, Dugmore D, Fioretti P, Gaita D, Hambrecht R, et al. Executive summary of the Position Paper of the Working Group on Cardiac Rehabilitation and Exercise Physiology of the European Society of Cardiology (ESC): core components of cardiac rehabilitation in chronic heart failure. Eur J Cardiovasc Prev Rehabil. 2005;12:321–5.
Pina IL, Apstein CS, Balady GJ, Belardinelli R, Chaitman BR, Duscha BD, Fletcher BJ, Fleg JL, Myers JN, Sullivan MJ. Exercise and heart failure: a statement from the American Heart Association Committee on exercise, rehabilitation, and prevention. Circulation. 2003;107:1210–25.
Bjarnason-Wehrens B. Trainingsmaßnahmen. Rauch B, Middeke M, Bönner G, Karoff M, Held K. (Edt.). Kardiologische rehabilitation. Stuttgart: Thieme; 2007. p. 78–89.
Eden KB, Orleans CT, Mulrow CD, Pender NJ, Teutsch SM. Does counseling by clinicians improve physical activity? A summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med. 2002;137:208–15.
Löllgen H, Böckenhoff A, Knapp G. Physical activity and all-cause mortality: An updated meta-analysis with different intensity categories. Int J Sports Med. 2009;30:213–24.
Nocon M, Hiemann T, Muller-Riemenschneider F, Thalau F, Roll S, Willich SN. Association of physical activity with all-cause and cardiovascular mortality: a systematic review and meta-analysis. Eur J Cardiovasc Prev Rehabil. 2008;15:239–46.
Samitz G, Egger M, Zwahlen M. Domains of physical activity and all-cause mortality: systematic review and dose-response meta-analysis of cohort studies. Int J Epidemiol. 2011;40:1382–400.
Löllgen H, Löllgen D. Risikoreduktion kardiovaskulärer Erkrankungen durch körperliche Aktivität. Internist. 2011;53:20–9.
Blumenthal JA, Babyak MA, Carney RM, Huber M, Saab PG, Burg MM, et al. Exercise, depression, and mortality after myocardial infarction in the ENRICHD trial. Med Sci Sports Exerc. 2004;746-755 doi:10.1249/01.MSS.0000125997.63493.13.
Wannamethee SG, Shaper AG, Walker M. Physical activity and mortality in older men with diagnosed coronary heart disease. Circulation. 2000;102:1358–63.
Janssen I, CJ J. Influence of physical activity on mortality in elderly with coronary artery disease. Med Sci Sports Exerc. 2006:418–23.
Al-Khalili F, Janszky I, Andersson A, Svane B, Schenck-Gustafsson K. Physical activity and exercise performance predict long-term prognosis in middle-aged women surviving acute coronary syndrome. J Intern Med. 2007;261:178–87.
Moholdt T, Wisløff U, Nilsen TIL, Slørdahl SA. Physical activity and mortality in men and women with coronary heart disease: a prospective population-based cohort study in Norway (the HUNT study). Eur J Cardiovasc Prev Rehabil. 2008;15:639–45.
Apullan FJ, Bourassa MG, Tardif JC, Fortier A, Gayda M, Nigam A. Usefulness of self-reported leisure-time physical activity to predict long-term survival in patients with coronary heart disease. Am J Cardiol. 2008;102:375–9.
Gerber Y, Myers V, Goldbourt U, Benyamini Y, Scheinowitz M, Drory Y. Long-term trajectory of leisure time physical activity and survival after first myocardial infarction: a population-based cohort study. Eur J Epidemiol. 2011;26:109–16.
Mons U, Hahmann H, Brenner H. A reverse J-shaped association of leisure time physical activity with prognosis in patients with stable coronary heart disease: evidence from a large cohort with repeated measurements. Heart. 2014;100:1043–9.
Yu C, Li LS, Ho HH, Lau C. Long-term changes in exercise capacity, quality of life, body anthropometry, and lipid profiles after a cardiac rehabilitation program in obese patients with coronary heart disease. Am J Cardiol. 2003;91:321–5.
Shibata Y, Hayasaka S, Yamada T, Ojima T, Ishikawa S, et al. Physical activity and risk of fatal or non-fatal cardiovascular disease among CVD survivors – the JMS cohort study. Circ J. 2011;75:1368–72.
Godin G, Desharnais R, Jobin J, Cook J. The impact of physical fitness and health-age appraisal upon exercise intentions and behavior. J Behav Med. 1987;10:241–50.
Kavanagh T, Mertens DJ, Hamm LF, Beyene J, Kennedy J, Corey P, Shephard RJ. Prediction of long-term prognosis in 12 169 men referred for cardiac rehabilitation. Circulation. 2002;106:666–71.
Valeur N, Clemmensen P, Saunamaki K, Grande P. The prognostic value of pre-discharge exercise testing after myocardial infarction treated with either primary PCI or fibrinolysis: a DANAMI-2 sub-study. Eur Heart J. 2005;26:119–27.
Lund LH, Aaronson KD, Mancini DM. Validation of peak exercise oxygen consumption and the Heart Failure Survival Score for serial risk stratification in advanced heart failure. Am J Cardiol. 2005;95:734–41.
O'Neill JO, Young JB, Pothier CE, Lauer MS. Peak oxygen consumption as a predictor of death in patients with heart failure receiving beta-blockers. Circulation. 2005;111:2313–8.
Myers J, Prakash M, Froelicher V, Do D, Partington S, Atwood JE. Exercise capacity and mortality among men referred for exercise testing. N Engl J Med. 2002;346:793–801.
Keteyian SJ, Brawner CA, Savage PD, Ehrman JK, Schairer J, Divine G, Aldred H, Ophaug K, Ades PA. Peak aerobic capacity predicts prognosis in patients with coronary heart disease. Am Heart J. 2008;156:292–300.
Martin BJ, Arena R, Haykowsky M, Hauer T, Austford LD, Knudtson M, Aggarwal S, Stone JA, for the APPROACH Investigators. Cardiovascular fitness and mortality after contemporary cardiac rehabilitation. Mayo Clin Proc. 2013;88:455–63.
Ades PA, Savage PD, Brawner CA, Lyon CE, Ehrman JK, Bunn JY, Keteyian SJ. Aerobic capacity in patients entering cardiac rehabilitation. Circulation. 2006;113:2706–12.
Karmisholt K, Gotzsche PC. Physical activity for secondary prevention of disease. Systematic reviews of randomised clinical trials. Dan Med Bull. 2005;52:90–4.
Rees K, Taylor RS, Singh S, Coats AJ, Ebrahim S. Exercise based rehabilitation for heart failure. Cochrane Database Syst Rev. 2004;(4):CD003331.
Ades PA. Cardiac rehabilitation and secondary prevention of coronary heart disease. N Engl J Med. 2001;345:892–902.
Wenger NK, Froelicher ES, Smith LK, Ades PA, Berra K, Blumenthal JA, Certo CM, Dattilo AM, Davis D, DeBusk RF, et al. Cardiac rehabilitation as secondary prevention. Agency for Health Care Policy and Research and National Heart, Lung, and Blood Institute. Clin Pract Guidel Quick Ref Guide Clin. 1995;17:1–23.
Piepoli MF, Corrà U, Adamopoulos S, Benzer W, Bjarnason-Wehrens B, et al. Secondary prevention in the clinical management of patients with cardiovascular diseases. Core components, standards and outcome measures for referral and delivery: A Policy statement from the cardiac rehabilitation section of the European Association for Cardiovascular Prevention & Rehabilitation. Endorsed by the Committee for Practice Guidelines of the European Society of Cardiology. Eur J Prev Cardiol. 2012;21:664–81.
Cornelissen V, Smart NA. Exercise training for blood pressure: a systematic review and meta- analysis. J Am Heart Assoc. 2013;2:e004473. doi:10.1161/JAHA.112.004473.
Pan XR, Li GW, Hu YH, Wang JX, Yang WY, An ZX, Hu ZX, Lin J, Xiao JZ, Cao HB, et al. Effects of diet and exercise in preventing NIDDM in people with impaired glucose tolerance. The Da Qing IGT and Diabetes Study. Diabetes Care. 1997;20(4):537–44.
Tuomilehto J, Lindstrom J, Eriksson JG, Valle TT, Hamalainen H, Ilanne-Parikka P, Keinanen-Kiukaanniemi S, Laakso M, Louheranta A, Rastas M, et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med. 2001;344:1343–50.
Boule NG, Haddad E, Kenny GP, Wells GA, Sigal RJ. Effects of exercise on glycemic control and body mass in type 2 diabetes mellitus: a meta-analysis of controlled clinical trials. JAMA. 2001;286:1218–27.
Kodama S, Tanaka S, Saito K, Shu M, Sone Y, Onitake F, Suzuki E, Shimano H, Yamamoto S, Kondo K, et al. Effect of aerobic exercise training on serum levels of high-density lipoprotein cholesterol: a meta-analysis. Arch Intern Med. 2007;167:999–1008.
Halverstadt A, Phares DA, Wilund KR, Goldberg AP, Hagberg JM. Endurance exercise training raises high-density lipoprotein cholesterol and lowers small low-density lipoprotein and very low-density lipoprotein independent of body fat phenotypes in older men and women. Metabolism. 2007;56(4):444–50.
Kelley GA, Kelley KS. Aerobic exercise and HDL2-C: a meta-analysis of randomized controlled trials. Atherosclerosis. 2006;184:207–15.
Kelley GA, Kelley KS, Franklin B. Aerobic exercise and lipids and lipoproteins in patients with cardiovascular disease: a meta-analysis of randomized controlled trials. J Cardpulm Rehabil. 2006;26:131–9.
DiPietro L. Physical activity in the prevention of obesity: current evidence and research issues. Med Sci Sports Exerc. 1999;31(11 Suppl):S542–6.
Garrow JS, Summerbell CD. Meta-analysis: effect of exercise, with or without dieting, on the body composition of overweight subjects. Eur J Clin Nutr. 1995;49:1–10.
Borg G. Perceived exertion as an indicator of somatic stress. Scand J Rehabil Med. 1970;2:92–8.
Ilarraza H, Myers J, Kottman W, Rickli H, Dubach P. An evaluation of training responses using self-regulation in a residential rehabilitation program. J Cardpulm Rehabil. 2004;24:27–33.
Wassermann K, Hansen JE, Sue DY, Casaburi R, BJ W. Principles of exercise testing ind interpretation. 3rd ed. Lippincott Williams & Wikins: Baltimore; 1999.
Gitt AK, Wasserman K, Kilkowski C, Kleemann T, Kilkowski A, Bangert M, Schneider S, Schwarz A, Senges J. Exercise anaerobic threshold and ventilatory efficiency identify heart failure patients for high risk of early death. Circulation. 2002;106:3079–84.
Mezzani A, Hamm LF, Jones AM, McBride PE, Moholdt T, Stone JA, Urhausen A, Williams MA, European Association for Cardiovascular Prevention and Rehabilitation; American Association of Cardiovascular and Pulmonary Rehabilitation; Canadian Association of Cardiac Rehabilitation. Aerobic exercise intensity assessment and prescription in cardiac rehabilitation: a joint position statement of the European Association for Cardiovascular Prevention and Rehabilitation, the American Association of Cardiovascular and Pulmonary Rehabilitation, and the Canadian Association of Cardiac Rehabilitation. J Cardiopulm Rehabil Prev. 2012;32:327–50.
Dubach P, Sixt S, Myers J. Exercise training in chronic heart failure: why, when and how. Swiss Med Wkly. 2001;131:510–4.
Wen CP, Wai JPM, Tsai MK, Yang YC, Cheng TYD, Lee M, et al. Minimum amount of physical activity for reduced mortality and extended life expectancy: a prospective cohort study. Lancet. 2011;378:1244–53.
Pattyn N, Coeckelberghs E, Buys R, Cornelissen VA, Vanhees L. Aerobic interval training vs. moderate continous training in coronary artery disease patients: a systematic review and meta-analysis. Sports Med. 2014;44:687–700.
Elliott AD, Rajopadhyaya K, Bentley DJ, Beltrame JF, Aromataris EC. Interval training versus continuous exercise in patients with coronary artery disease a meta-analysis. Heart Lung Circ. 2015;24:149–57.
Rognmo O, Moholdt T, Bakken H, Hole T, Mølstad P, Myhr NE, Grimsmo J, Wisløff U. Cardiovascular risk of high- versus moderate-intensity aerobic exercise in coronary heart disease patients. Circulation. 2012;126:1436–40.
Moholdt T, Amundsen BH, Rustad LA, Løvø KT, Gullikstad LR, Bye A, Skogvoll E, Wisløff U, Slørdahl SA. Aerobic interval training versus continuous moderate exercise after coronary artery bypass surgery: a randomized study of cardiovascular effects and quality of life. Am Heart J. 2009;158:1031–7.
Munk PS, Butt N, Larsen AI. High-intensity interval exercise training improves heart rate variability in patients following percutaneous coronary intervention for angina pectoris. Int J Cardiol. 2009;145:312–4.
Rognmo O, Hetland E, Helgerud J, Hoff J, Slørdahl SA. High intensity aerobic interval exercise is superior to moderate intensity exercise for increasing aerobic capacity in patients with coronary artery disease. Eur J Cardiovasc Prev Rehabil. 2004;11:216–22.
Warburton DE, McKenzie DC, Haykowsky MJ, Taylor A, Shoemaker P, Ignaszewski AP, Chan SY. Effectiveness of high-intensity interval training for the rehabilitation of patients with coronary artery disease. Am J Cardiol. 2005;95:1080–4.
Conraads VM, Pattyn N, De Maeyer C, Beckers PJ, Coeckelberghs E, Cornelissen VA, Denollet J, Frederix G, Goetschalckx K, Hoymans VY, Possemiers N, Schepers D, Shivalkar B, Voigt JU, Van Craenenbroeck EM, Vanhees L. Aerobic interval training and continuous training equally improve aerobic exercise capacity in patients with coronary artery disease; The SAINTEX-CAD study. Int J Cardiol. 2015;179:203–10.
Hofmann R, Gogol C, Karoff M Bjarnason-Wehrens B. Impact of continuous exercise intensity versus high intensity interval exercise training on endurance capacity in coronary artery disease patients with preserved left ventricular function. Abstract P181, EuroPRevent 2014, Amsterdam.
Nechwatal RM, Duck C, Gruber G. Physical training as interval or continuous training in chronic heart failure for improving functional capacity, hemodynamics and quality of life – a controlled study. Z Kardiol. 2002;91:328–37.
Wisloff U, Stoylen A, Loennechen JP, Bruvold M, Rognmo O, Haram PM, Tjonna AE, Helgerud J, Slordahl SA, Lee SJ, et al. Superior cardiovascular effect of aerobic interval training versus moderate continuous training in heart failure patients: a randomized study. Circulation. 2007;115:3086–94.
Smart NA, Dieberg G, Giallauria F. Intermittent versus continuous exercise training in chronic heart failure: a meta-analysis. Int J Cardiol. 2013;186:352–8.
Haykowsky MJ, Timmons MP, Kruger C, McNeely M, Taylor DA, Clark AM. Meta-analysis of aerobic interval training on exercise capacity and systolic function in patients with heart failure and reduced ejection fractions. Am J Cardiol. 2013;111:1466–9.
Ismail H, McFarlane JR, Nojoumian AH, Dieberg G, Smart NA. Clinical outcomes and cardiovascular responses to different exercise training intensities in patients with heart failure. J Am Coll Cardiol Heart Fail. 2013;1:514–22.
Pattyn N, Vanhees L, Cornelissen VA, Coeckelberghs E, De Maeyer C, Goetschalckx K, Possemiers N, Wuyts K, Van Craenenbroeck EM, PJ B. The long-term effects of a randomized trial comparing aerobic interval versus continuous training in coronary artery disease patients: 1-year data from the SAINTEX-CAD study. Eur J Prev Cardiol. 2016;23:1154–64. doi:10.1177/2047487316631200.
Meyer K, Samek L, Schwaibold M, Westbrook S, Hajric R, Beneke R, Lehmann M, Roskamm H. Interval training in patients with severe chronic heart failure: analysis and recommendations for exercise procedures. Med Sci Sports Exerc. 1997;29(3):306–12.
Kelley GA, Kelley KS, Tran ZV. Walking and resting blood pressure in adults: a meta-analysis. Prev Med. 2001;33:120–7.
Kelley GA, Kelley KS, Tran ZV. Walking and non-HDL-C in adults: a meta-analysis of randomized controlled trials. Prev Cardiol. 2005;8:102–7.
Murphy MH, Nevill AM, Murtagh EM, Holder RL. The effect of walking on fitness, fatness and resting blood pressure: a meta-analysis of randomised, controlled trials. Prev Med. 2007;44:377–85.
Church TS, Earnest CP, Morss GM. Field testing of physiological responses associated with Nordic Walking. Res Q Exerc Sport. 2002;73:296–300.
Willson J, Torry MR, Decker MJ, Kernozek T, Steadman JR. Effects of walking poles on lower extremity gait mechanics. Med Sci Sports Exerc. 2001;33:142–7.
Schwameder H, Roithner R, Muller E, Niessen W, Raschner C. Knee joint forces during downhill walking with hiking poles. J Sports Sci. 1999;17:969–78.
Kraemer WJ, Ratamess NA, French DN. Resistance training for health and performance. Curr Sports Med Rep. 2002;1:165–71.
Kraemer WJ, Ratamess NA, Fry AC, French DN. Strength testing: development and evaluation of methodology. In: Maud PJ, Foster C, editors. Physiological assessment of human fitness. 2nd ed. Champaign: Human Kinetics; 2006. p. 119–50.
Narici MV, Reeves ND, Morse CI, Maganaris CN. Muscular adaptations to resistance exercise in the elderly. J Musculoskelet Neuronal Interact. 2004;4:161–4.
Latham NK, Bennett DA, Stretton CM, Anderson CS. Systematic review of progressive resistance strength training in older adults. J Gerontol A Biol Sci Med Sci. 2004;59:48–61.
Latham N, Anderson C, Bennett D, Stretton C. Progressive resistance strength training for physical disability in older people. Cochrane Database Syst Rev. 2003;(2):CD002759.
Pu CT, Johnson MT, Forman DE, Hausdorff JM, Roubenoff R, Foldvari M, Fielding RA, Singh MA. Randomized trial of progressive resistance training to counteract the myopathy of chronic heart failure. J Appl Physiol. 2001;90:2341–50.
Williams AD, Carey MF, Selig S, Hayes A, Krum H, Patterson J, Toia D, Hare DL. Circuit resistance training in chronic heart failure improves skeletal muscle mitochondrial ATP production rate – a randomized controlled trial. J Card Fail. 2007;13:79–85.
Braith RW, Magyari PM, Pierce GL, Edwards DG, Hill JA, White LJ, Aranda Jr JM. Effect of resistance exercise on skeletal muscle myopathy in heart transplant recipients. Am J Cardiol. 2005;95:1192–8.
Braith RW, Magyari PM, Fulton MN, Aranda J, Walker T, Hill JA. Resistance exercise training and alendronate reverse glucocorticoid-induced osteoporosis in heart transplant recipients. J Heart Lung Transplant. 2003;22:1082–90.
Gillespie LD, Gillespie WJ, Robertson MC, Lamb SE, Cumming RG, Rowe BH. Interventions for preventing falls in elderly people. Cochrane Database Syst Rev. 2003;(4):CD000340.
Marzolini Oh PI, Brooks D. Effect of combined aerobic and resistance training versus aerobic training alone in individuals with coronary artery disease: a meta-analysis. Eur J Prev Cardiol. 2012;19:81–94.
Hwang CL, Chien CL, Wu YT. Resistance training increases 6-minute walk distance in people with chronic heart failure: a systematic review. J Physiother. 2010;56:87–96.
Hunter GR, Treuth MS, Weinsier RL, Kekes-Szabo T, Kell SH, Roth DL, Nicholson C. The effects of strength conditioning on older women’s ability to perform daily tasks. J Am Geriatr Soc. 1995;43:756–60.
Hunter GR, Wetzstein CJ, Fields DA, Brown A, Bamman MM. Resistance training increases total energy expenditure and free-living physical activity in older adults. J Appl Physiol. 2000;89:977–84.
Banz WJ, Maher AM, Thompson WG, Bassett DR, Moore W, Ashraf M, Keefer DJ, Zemel MB. Effects of resistance versus aerobic training on coronary artery disease risk factors. Exp Biol Med. 2003;228:434–40.
Brooks N, Layne JE, Gordon PL, Roubenoff R, Nelson ME, Castaneda-Sceppa C. Strength training improves muscle quality and insulin sensitivity in Hispanic older adults with type 2 diabetes. Int J Med Sci. 2007;4:19–27.
Kim HJ, Lee JS, Kim CK. Effect of exercise training on muscle glucose transporter 4 protein and intramuscular lipid content in elderly men with impaired glucose tolerance. Eur J Appl Physiol. 2004;93:353–8.
Holten MK, Zacho M, Gaster M, Juel C, Wojtaszewski JF, Dela F. Strength training increases insulin-mediated glucose uptake, GLUT4 content, and insulin signaling in skeletal muscle in patients with type 2 diabetes. Diabetes. 2004;53:294–305.
Castaneda C, Layne JE, Munoz-Orians L, Gordon PL, Walsmith J, Foldvari M, Roubenoff R, Tucker KL, Nelson ME. A randomized controlled trial of resistance exercise training to improve glycemic control in older adults with type 2 diabetes. Diabetes Care. 2002;25:2335–41.
Fiatarone MA, Marks EC, Ryan ND, Meredith CN, Lipsitz LA, Evans WJ. High-intensity strength training in nonagenarians. Effects on skeletal muscle. JAMA. 1990;263:3029–34.
King PA, Savage P, Ades PA. Home resistance training in an elderly woman with coronary heart disease. J Cardpulm Rehabil. 2000;20:126–9.
Brochu M, Savage P, Lee M, Dee J, Cress ME, Poehlman ET, Tischler M, Ades PA. Effects of resistance training on physical function in older disabled women with coronary heart disease. J Appl Physiol. 2002;92:672–8.
Ades PA, Savage PD, Brochu M, Tischler MD, Lee NM, Poehlman ET. Resistance training increases total daily energy expenditure in disabled older women with coronary heart disease. J Appl Physiol. 2005;98:1280–5.
Ades PA, Savage PD, Cress ME, Brochu M, Lee NM, Poehlman ET. Resistance training on physical performance in disabled older female cardiac patients. Med Sci Sports Exerc. 2003;35:1265–70.
Lee IM, Hsieh CC, Paffenbarger Jr RS. Exercise intensity and longevity in men. The Harvard Alumni Health Study. JAMA. 1995;273:1179–84.
Volaklis KA, Tokmakidis SP. Resistance exercise training in patients with heart failure. Sports Med. 2005;35:1085–103.
Benton MJ. Safety and efficacy of resistance training in patients with chronic heart failure: research-based evidence. Prog Cardiovasc Nurs. 2005;20:17–23.
Bartlo P. Evidence-based application of aerobic and resistance training in patients with congestive heart failure. J Cardiopulm Rehabil Prev. 2007;27:368–75.
Piepoli MF, Conraads V, Corrà U, Dickstein K, Francis DP, Jaarsm T, McMurray J, Pieske B, Piotrowicz E, Schmid JP, Anker SD, Solal AC, Filippatos GS, Hoes AW, Gielen S, Giannuzzi P, Ponikowsk PP. Exercise training in heart failure: from theory to practice. A consensus document of the Heart Failure Association and the European Association for Cardiovascular Prevention and Rehabilitation. Eur J Heart Fail. 2011;13:347–57.
Braith RW, Stewart KJ. Resistance exercise training: its role in the prevention of cardiovascular disease. Circulation. 2006;113:2642–50.
Lind AR, McNicol GW. Muscular factors which determine the cardiovascular responses to sustained and rhythmic exercise. Can Med Assoc J. 1967;96:706–15.
Sale DG, Moroz DE, McKelvie RS, MacDougall JD, McCartney N. Comparison of blood pressure response to isokinetic and weight-lifting exercise. Eur J Appl Physiol Occup Physiol. 1993;67:115–20.
Mitchell JH, Payne FC, Saltin B, Schibye B. The role of muscle mass in the cardiovascular response to static contractions. J Physiol. 1980;309:45–54.
Lamotte M, Fleury F, Pirard M, Jamon A, de Borne P v. Acute cardiovascular response to resistance training during cardiac rehabilitation: effect of repetition speed and rest periods. Eur J Cardiovasc Prev Rehabil. 2010;17:329–36.
Fleck S, Falkel J, Harman E. Cardiovascular responses during resistance training. Med Sci Sports Excerc. 1989;21:114.
Williams MA, Haskell WL, Ades PA, Amsterdam EA, Bittner V, Franklin BA, Gulanick M, Laing ST, Stewart KJ. Resistance exercise in individuals with and without cardiovascular disease: 2007 update: a scientific statement from the American Heart Association Council on Clinical Cardiology and Council on Nutrition, Physical Activity, and Metabolism. Circulation. 2007;116:572–84.
Graf C, Rost R. Herz und Sport. Balingen: Spitta Verlag; 2001.
Schmid JP, Anderegg M, Romanens M, Morger C, Noveanu M, Hellige G, Saner H. Combined endurance/resistance training early on, after a first myocardial infarction, does not induce negative left ventricular remodeling. Eur J Cardiovasc Prev Rehabil. 2008;15:341–6.
Arthur HM, Gunn E, Thorpe KE, Ginis KM, Mataseje L, McCartney N, McKelvie RS, Ginis KM, Mataseje L, McCartney N, McKelvie RS. Effect of aerobic versus combined aerobic-strength training on 1-year, post-cardiac rehabilitation outcomes in woman after a cardiac event. J Rehabil Med. 2007;39:730–5.
Karlsdottir AE, Foster C, Porcari JP, Palmer-McLean K, White-Kube R, Backes RC. Hemodynamic responses during aerobic and resistance exercise. J Cardpulm Rehabil. 2002;22:170–7.
Bjarnason-Wehrens B, Mayer-Berger W, Meister ER, Baum K, Hambrecht R, Gielen S. Recommendations for resistance exercise in cardiac rehabilitation. Recommendations of the German Federation for Cardiovascular Prevention and Rehabilitation. Eur J Cardiovasc Prev Rehabil. 2004;11:352–61.
Braith RW, Graves JE, Pollock ML, Leggett SL, Carpenter DM, Colvin AB. Comparison of 2 vs 3 days/week of variable resistance training during 10- and 18- week programmes. Int J Sports Med. 1989;10:450–4.
Rhea MR, Alvar BA, Burkett LN, Ball SD. A meta-analysis to determine the dose response for strength development. Med Sci Sports Exerc. 2003;35:456–64.
Feiereisen P, Vaillant M, Eischen D, Delagardelle C. Isokinetic versus one-repetition maximum strength assessment in chronic heart failure. Med Sci Sports Exerc. 2010;42:2156–63.
Levinger I, Goodman C, Hare DL, Jerums G, Toia D, Selig S. The reliability of the 1RM strength test for untrained middle-aged individuals. J Sci Med Sport. 2009;12:310–6.
Barnard KL, Adams KJ, Swank AM, Mann E, Denny DM. Injuries and muscle soreness during the one repetition maximum assessment in a cardiac rehabilitation population. J Cardpulm Rehabil. 1999;19:52–8.
Schroeder ET, Wang Y, Castaneda-Sceppa C, Cloutier G, Vallejo AF, Kawakubo M, Jensky NE, Coomber S, Azen SP, Sattler FR. Reliability of maximal voluntary muscle strength and power testing in older men. J Gerontol A Biol Sci Med Sci. 2007;62:543–9.
Brzycki M. Strength testing-Prediction a one-rep max from reps-to-fatique. JOPERD. 1993;68:88–90.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
Bjarnason-Wehrens, B., Halle, M. (2017). Exercise Training in Cardiac Rehabilitation. In: Niebauer, J. (eds) Cardiac Rehabilitation Manual. Springer, Cham. https://doi.org/10.1007/978-3-319-47738-1_4
Download citation
DOI: https://doi.org/10.1007/978-3-319-47738-1_4
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-47737-4
Online ISBN: 978-3-319-47738-1
eBook Packages: MedicineMedicine (R0)