Abstract
Purpose of the review
Heart failure is very prevalent and exercise intolerance is one of its main symptoms. Various studies and meta-analysis have provided scientific evidence regarding the improvement of functional capacity and quality of life in patients with heart failure who undertake a cardiac rehabilitation program. This paper reviews the evidence published in recent years regarding the efficacy and safety of physical exercise, as well as the different exercise modalities that should be a part of the treatment of heart failure patients.
Recent findings
Exercise training in heart failure is safe and effective. High-intensity interval training, especially when associated with strength exercises and inspiratory muscle training, offers the most benefits compared with the traditional continuous training of moderate intensity. It is also better tolerated in heart failure patients and this increases adherence. However, we are in need of a big randomized study in patients with heart failure in order to fully establish the best exercise modality in these patients.
Summary
Patients with heart failure should be referred to a multidisciplinary Cardiac Rehabilitation program and receive an individual exercise prescription based on risk stratification, exercise capacity, and patient’s preference. There is no single exercise training program that covers all the individual patients’ needs. Therefore, in most cases, a combination of exercise programs, such as aerobic interval or continuous training, strength exercise, and inspiratory muscle training, is needed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The guidelines of the European Society of Cardiology define heart failure (HF) as an abnormality of cardiac structure or function leading to failure of the heart to deliver oxygen at a rate commensurate with the requirements of the metabolizing tissues, despite normal filling pressures or only at the expense of increased filling pressures. Regular aerobic exercise increases the ability of the body to use that oxygen [1].
Up to 2 % of the adult population in Europe and the United States (U.S.) has HF. It is the first cause of hospital admission in people above 65 years old, contributing to an increasing use of medical resources [2]. During 2012, there were more than 1 million hospitalizations in the U.S. with estimated direct and indirect costs of 40 billion dollars [3]. Identifying the etiology of HF is fundamental in order to offer the most adequate treatment for the patient. Physical training is beneficial for HF patients with ischemic and nonischemic cardiomyopathies, although cardiac adaptation is best in HF patients with nonischemic etiology [4].
Until the nineties, rest and restrain in physical activity were recommended as a part of the treatment of HF. Currently, both the European and the American guidelines highlight the importance of regular aerobic physical activity in the treatment of HF patients, with a class IA level of recommendation to improve functional capacity and reduce morbidity and mortality [5••].
Exercise Training in Heart Failure
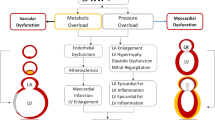
Intolerance to physical exercise is one of the main symptoms in patients with HF, either with reduced or preserved left ventricular ejection fraction (LVEF). This exercise intolerance is strongly correlated with prognosis and a reduced quality of life [6•, 7]; however, it does not correlate with LVEF [8•].. Exercise intolerance can be quantified as a reduction in peak oxygen consumption (VO2) of about 40 % during maximal exercise compared with controls of similar age and sex. This reduction of peak VO2 can be due to cardiac abnormalities such as diminished cardiac output (CO) and chronotropic incompetence but also to abnormalities in peripheral vessels and muscles [7].
As exercise intolerance is multifactorial, we will briefly review the physiopathology behind the central and peripheral mechanisms in patients with HF:
-
(1)
Cardiac alterations lead to systolic or diastolic dysfunction, which in turn lead to diminished systolic volume, increase in filling pressures, mitral regurgitation, and right ventricular dysfunction. In patients with reduced LVEF, the diminished CO at submaximal and peak exercise is the result of reduced systolic volume, together with the reduction in heart rate reserve. Ventricular filling during exercise is also altered secondary to diastolic dysfunction and this increase filling pressures, which are responsible for the increase in pulmonary capillary pressure and dyspnea. Diastolic dysfunction of the left ventricle is an independent predictor of reduced exercise capacity in patients with preserved LVEF [9].
-
(2)
Patients with HF have vascular abnormalities such as endothelial dysfunction secondary to diminished Nitric Oxide availability and an increase of reactive oxygen species that lead to vasoconstriction and a reduced vasodilatory capacity during exercise [7].
-
(3)
Patients with HF have changes in the skeletal muscles that include a reduction in muscle mass, changes of the muscle fibers from type I to type IIb, and a reduction of type IIa muscle fibers in comparison with type IIb fibers. There is also an altered metabolism of these skeletal muscles with a reduction in the oxidative capacity and generation of ATP (diminished function, density, size, and enzymes in the mitochondria that lead to a delay in the synthesis of high-energy components) [9]. Although it is clear that there is an induced myopathy secondary to the state of HF and chronic hypoperfusion documented in some studies, it has been shown that the mitochondrial dysfunction could be the consequence of diminished use of the peripheral muscles and deconditioning [8•].
-
(4)
Respiratory abnormalities in HF patients are due to a mismatch in ventilation/perfusion, pulmonary edema, damage of the pulmonary vasculature, fibrosis, increase of the minute ventilation, and reduced diaphragmatic strength. As opposed to the changes seen in the skeletal muscle, in the diaphragm of patients with HF there is a change from type IIb to type I fibers, probably as an adaptation mechanism to the increase workload of the diaphragm [10•].
-
(5)
The neurohormonal abnormalities that occur during HF imply an increase in sympathetic activity and a decrease in vagal activity, activating the renin-angiotensin-aldosterone system that leads to tachycardia, chronotropic incompetence, vasoconstriction, increase in reactive oxygen species, and proinflammatory cytokines that lead to fibrosis and increased muscular catabolism [9].
It is important to note that the biggest contributors to the increase in peak VO2 achieved by patients with HF after physical training are the peripheral factors above mentioned [7]. The biggest part of the oxygen consumption during the transition from rest to exercise occurs in the active skeletal muscles of the periphery. Therefore, an abnormality in the metabolism of these muscles has a deep impact in the exercise intolerance of patients with HF. In this transition, the increase of blood flow to the muscles is due to the activation of the sympathetic nervous system together with the metabolically mediated vasodilatation that occurs in the muscles that are being exercised. Changes in the central and peripheral arterial function in patients with HF result in an inefficient distribution of the CO to the active skeletal muscles and contribute to exercise intolerance. Although CO can be normal at rest in patients with HF, there is an insufficient capacity to increase CO during mild exercise, leading to an insufficient increase in perfusion of active muscles that could cause an early switch to anaerobic metabolism, with the consequent increase in lactate production, increase of inadequate muscle strength, and finally muscle fatigue. This is why lactate levels correlate well with peak exercise capacity [9].
It is well proven that physical exercise can improve physical capacity (an important prognostic marker in HF patients [11]), heart and vascular function [12], depression [13], and quality of life [14, 15••]. This increase in quality of life also may have a higher impact in patients below 60 years old [16•].
In systolic HF, aerobic training offers an improvement of systolic and diastolic function with beneficial effects in ventricular work. It improves arterial function, measured as a decrease in pulse wave velocity and an increase of the augmentation index [17•]. Aerobic exercise also improves prognostic markers such as the natriuretic peptides and the ventilatory equivalent of carbon dioxide (VE/VCO2 slope) in patients with systolic HF [18].
Physical training with or without strength exercises is an effective treatment to improve exercise tolerance and quality of life in patients with stable HF and reduced LVEF (level of evidence B) [6•, 7]. It can improve peak VO2 and hemodynamics, reduces chronotropic incompetence, and improves the function of the skeletal muscle and peripheral vasculature [9]. Peak VO2 increased between 18 and 25 % and the duration of exercise between 18 and 34 % in the published studies [9]. Subjective symptoms, functional class, and quality of life all improved after exercise training [9].
Flow-mediated vasodilatation and arterial elasticity are reduced in patients with advanced age, and they are critical components in the response to exercise. Physical exercise in patients with HF increases peak VO2 without influencing the flow-mediated arterial vasodilation or arterial elasticity; therefore, the adaptations at the level of the microcirculation and skeletal muscle that increase the transport and utilization of oxygen by the active muscles may be the mechanisms contributing to the increase in peak VO [19, 25].
Most of the studies regarding exercise training in HF have been performed in chronic patients with functional class II–III of the New York Heart Association (NYHA). The biggest study was the HF-ACTION [20••], a randomized and controlled trial that analyzed the effects of physical exercise in 2331 patients with HF in functional class II–III of the NYHA and a LVEF <35 %. One group was randomized to supervised physical exercise that consisted of 36 sessions of aerobic exercise at 60–70 % of the heart rate reserve during 15–35 min, followed by a home exercise program of 40 min, five times per week. The control group received usual care (recommendations to do regular exercise at moderate intensity but without structured sessions or supervision). The primary outcome was death or all-cause hospitalization, and there was a tendency to favor the exercise group but it was not statistically significant (HR 0.93; p = 0.13) after 30 months of follow-up. In a prespecified analysis, adjusting for variables that strongly predicted outcomes such as the cardiopulmonary exercise duration, LVEF, the Beck II depression score ,and atrial fibrillation or flutter, exercise was associated with a significant reduction of the primary outcome of 11 % (p = 0.03). A significant improvement in the quality of life at 3 months was also seen in the exercise group [21••]. However, the benefits of exercise training in patients with systolic HF may have been underestimated due to the following factors: (1) At randomization, 55 % of patients assigned to the control group were not satisfied with the assigned treatment. (2) There was an important crossover rate, as 22–28 % of the control group performed exercise regularly. (3) Adherence in the exercise group diminished gradually from 95 min per week at 4–6 months to 74 min per week at 10–12 months after starting the program.
Many of the published studies, including HF-ACTION, excluded patients with decompensated HF or those who have been hospitalized in the previous 4–6 weeks [22], needing a stabilization period prior to starting a Cardiac Rehabilitation (CR) program. Although the indication for exercise training is more limited in patients with acute HF, the published studies showed a benefit of a protocolized exercise program initiated during the hospitalization. The majority of patients hospitalized for acute HF are older, with multiple comorbidities and deficits in mobility, strength, and balance that can worsen during hospitalization, and all this is associated with increased risk of adverse events such as rehospitalization and death [23]. Exercise training of certain muscles such as the knee extensor during 2 months can be very beneficial to improve diffusive O2 transport in patients with HF and could be very useful in severely deconditioned patients with minimal reserves [24•].
Exercise Training Protocols in Heart Failure
The prescription of an exercise program must be individualized, and the type and intensity of the exercise must be tailored to each case in order to obtain the maximum benefit with the minimum risk. To do this, we must perform an individual clinical evaluation, be aware of the physical and social situation of our patient as well as their personal preferences in order to improve adherence to the therapeutic program. To stratify risk, we recommend risk models that include functional parameters such as the Heart Failure Survival Score or the Metabolic Exercise and Cardiac, and Kidney Indexes (MECKI) [25] that includes the peak VO2 and the VE/VCO2 slope, respectively. The VE/VCO2 slope indexed for the VO2 or the respiratory oscillation index has also been shown to have a role in risk stratification [26].
There are multiple training protocols: Aerobic continuous exercise, interval training alone or combined with strength, and/or respiratory exercises. All of them include a warming-up phase and a cooling-down phase. Also, these programs can be supervised or not and they can be done in hospitals, primary health care centers, sports facilities, or at home. Table 1 describes the training programs of most of the referenced studies, and we will briefly review the different types of exercise protocols and the evidence behind them.
Intermittent Versus Continuous Aerobic Training
Some studies have shown intermittent or interval training (IT) exercise programs to be superior to continuous training (CT) in patients with chronic HF.
Smart et al. [27••] performed a meta-analysis of studies comparing IT with CT in patients with chronic HF, and they concluded that the optimal exercise protocol to improve peak VO2 y VE/VCO2 slope would be an IT of 4 min of work at 90–95 % of the peak heart rate followed by 3 min of recovery at 50–70 % of the peak heart rate during 38 min, three times per week. With the same energy consumption, adding strength exercises seemed to improve the changes in peak VO2, which are associated with good prognosis.
Haykiwsky et al. [28] in another meta-analysis found a higher increase in peak VO2 with IT in comparison with CT of moderate intensity in patients with stable chronic HF and reduced LVEF, although the duration and intensity of exercise in the different studies analyzed were different.
An increase in peak VO2 and CO with IT versus CT was also found by Fleg et al. [6•] after 3 months of training. Fu et al. [29•] also found that IT was associated with a better physical condition, cardiovascular function, and quality of life compared with CT [30].
Other studies published in recent years did not find this superiority of IT versus CT [31, 32, 33•]. The study by Nathalie et al. [34•] found that after 24 sessions of training, both the IT and CT group had significant improvements in physical condition, maximal work load, peak VO2, oxygen uptake at the anaerobic threshold, and peak O2 pulse. There were no changes in cardiovascular structure or in quality of life (SF-36, Minnesota) in any of the groups. Aksoy et al. [35•] also found that both types of exercise protocols reduced serum markers of adhesion molecules associated with endothelial dysfunction (a noninvasive biomarker used to identify high-risk patients) [36].
Short-Duration Interval Training
The majority of studies on cardiac rehabilitation in patients with HF have been performed with CT of moderate intensity (50–70 % of peak VO2), but more recently, high-intensity interval training (HIT) at 80–95 % of peak VO2 during 2–5 min alternating with resting periods have been tested [37, 38]. A recent study by Chrysohoou et al. [17•] evaluated the effect of HIT combined with strength exercise on left ventricular function and aortic elastic properties in patients with chronic HF. Compared with control patients, there was a significant reduction in the pulse wave velocity of 9 % and in the augmentation index of 29 %. They found an increase of peak oxygen uptake of 28 %, peak power of 25 %, peak heart rate of 25 %, and a decrease of the VE/VC02 slope. There was also an improvement in diastolic function with significant decreases in the E/A and E/E′ ratios. All these changes were accompanied by improved quality of life of 66 %, as measured by the Minnesota living with heart failure questionnaire, improved depression score of 19 %, and an increase of the 6-min walking test (6MWT) of 13 % in the intervention group versus the control.
Interval Training at Different Intensities
Hashbullah et al. [38•] published a meta-analysis comparing the effect of different exercise intensities on peak VO2, adherence to treatment and adverse effects in patients with HF. They observed an improvement in peak VO2 in the HIT group as the intensity of the exercise program increased from 4 to 52 weeks and from 45 to 200 min/week. The improvements that they found in the low intensity and control group were attributed to the pharmacological treatment. They did not find significant differences between vigorous exercise and controls regarding cardiac events or mortality, although rehospitalizations were 15 % lower in the vigorous exercise group. When they compared vigorous-intensity exercise with high-intensity exercise, there was a tendency to diminish mortality. Both exercise regimens were better tolerated if rest intervals were used, compared with CT. HIT programs can also increase adherence as the time and frequency of sessions are reduced.
Inspiratory Muscle Training
Inspiratory muscular training (IMT) improves functional capacity and quality of life, especially in patients with an increased weakness of these muscle groups and in association with aerobic exercise. Stamatis et al. [39••] obtained significant benefits in inspiratory muscle work capacity, quality of life, and dyspnea, and a reduction of C-reactive protein and natriuretic peptides in patients with HF that performed aerobic exercise associated with IMT in comparison with those that only did aerobic exercise. They found a significant increase in both groups in maximal inspiratory pressure, peak VO2, and LVEF after training.
Other authors also confirmed the benefit of IMT, showing that its performance during 4 weeks could improve aerobic capacity and peripheral changes [40•].
An exercise program that combines HIT with strength training and IMT showed benefits in the function of the skeletal and respiratory muscles, the cardiopulmonary index, dyspnea, and quality of life compared with a traditional aerobic exercise training program [10].
Benefits of Aerobic Exercise Training in Patients with Preserved LVEF
Most of the studies of exercise training in patients with HF have been performed in those with reduced LVEF, and the effects of HIT in patients with HF and preserved LVEF are less well studied. Siddhartha et al. [41] studied patients with HF and preserved LVEF, and they found that patients that performed HIT had significant improvements in peak VO2, parameters of diastolic dysfunction of the left ventricle, and a reduced diastolic arterial pressure compared with CT. However, there were no changes in endothelial function, maybe because they found no changes in the vasodilatory function among patients with preserved LVEF compared with those with reduced LVEF. Although it was a small study with very few women included, the intensity of HIT recommended (see Table 1) is in accordance with recent recommendations, and it may be an optimal exercise prescription for patients with HF and preserved LVEF.
Ambarish et al. [42] in a recent meta-analysis of patients with HF and a LVEF >45 % observed a significant improvement of cardiorespiratory function and quality of life in the exercise group versus the control, although they did not find significant changes in systolic or diastolic function. Therefore, the improvement in cardiorespiratory function may be mediated through mechanisms independent of the left ventricular function.
Kitzman et al. [19•] demonstrated an improvement in exercise tolerance, systolic and diastolic function, quality of life, and left ventricular dimensions in patients with HF and preserved LVEF after a supervised exercise training program. It was hypothesized that increased arterial stiffness and endothelial dysfunction could contribute to the exercise intolerance observed in patients with HF and preserved LVEF and that this could be improved by means of exercise training programs. However, in this study, they did not find an improvement in endothelial function and arterial stiffness. Other possible mechanisms for the improvement in exercise tolerance could be peripheral factors such as a better extraction of oxygen by the active skeletal muscles or physiological remodeling and associated improvement in stroke volume and cardiac output.
Benefits of Aerobic Exercise Training in Women
There is less evidence of the benefit of physical exercise in women with HF due to the lower number of these patients included in most studies. Piña et al. [43] observed increased benefit for the combined objectives of mortality and hospitalization for any cause in women compared with men. This improvement was primarily driven by a lower hospitalization rate with similar mortality rate. Adherence was similar between women and men and they found similar small increases in peak VO2 with exercise training.
The contribution of hormones to exercise intolerance has not been shown in women with HF, but we do now that estrogen diminishes with age and this could be associated with diminished endothelial dysfunction. Further studies to evaluate this hypothesis are needed, and if this is the case, evaluation of hormonal intervention in older women and men could be beneficial in patients with HF.
Adherence to a Physical Exercise Training Programs
Adherence has been the Achilles heel of most of the Cardiac Rehabilitation programs; especially in the medium–long term. Home-based exercise programs were introduced to improve access and patient participation. A Cochrane review [15••] included 17 randomized controlled studies comparing home-based exercise with supervised exercise training in a center (hospital, gym, or sport center) in HF patients. After 12 months of follow-up, they did not observe any differences in mortality, cardiac events, exercise capacity, quality of life, costs or modifiable risk factors such as Total and LDL Cholesterol, systolic blood pressure, and smoking habits. There were small differences in favor of the center-supervised program regarding HDL Cholesterol, Triglycerides, and diastolic blood pressure. The home-based programs had better adherence and could be beneficial, depending on patient’s preference, in low-risk patients after myocardial infarction, coronary revascularization, or in HF patients.
Lauren et al. [44••] described the association between social support and barriers to participate in an exercise program of 3 to 12 months duration, with adherence and clinical results. Higher exercise time correlated with a higher Perceived Social Support Score (PSSS) and a lower Barriers to Exercise Score (BTES) (p < 0.005). In the HF-ACTION study [20••], from 2331 patients that started the study, 2279 (1090 in the exercise group) completed it. A lower adherence was found in women with younger age, black race, higher body mass index, lower exercise capacity, lower quality of life, and higher depression scores and who were single. There was no association between the baseline PSSS or BTES and peak VO2 at 12 months. Social support was not associated with mortality or cardiovascular or all-cause hospitalization.
Although physical limitations and decreased social support can diminish the adherence to an exercise program, it is important to remember that there are studies that show that even low levels of exercise are better than none [45, 46]. To increase adherence to cardiac rehabilitation programs, life-style interventions can be useful, as well as psychosocial, socioeconomic, educational, and biological factors. There are a few studies on the predictors of behavior regarding physical exercise, including genetic markers [6•], although we need more studies regarding what interventions could improve the adherence to exercise programs in patients with chronic HF. The use of new technologies such as telemedicine using smartphones and internet could facilitate follow-up and adherence in some patient groups [47, 48].
New Horizons
In the future we need to perform more studies on the efficacy of exercise training programs in less-studied patient groups with heart failure such as older and frailer patients with increased comorbidities, women, patients with recently decompensated HF, and patients with HF and preserved LVEF.
HIT seems to be the best exercise training protocol in HF patients as it has been shown to be as safe as CT and more efficacious; however, physicians still hesitate to prescribe this type of exercise programs in HF patients as the existing studies have different exercise protocols with mostly soft outcomes. Therefore, a big randomized controlled trial of HIT combined with IMT and possibly strength exercises compared with CT and with a control group would seem appropriate in order to fully establish this therapy in HF patients.
Another great challenge is to increase the inclusion and adherence of patients with HF to Cardiac Rehabilitation programs. Home-based training programs can overcome geographical access and timetable incompatibilities with similar results to the center-based programs. Also, telemedicine can improve adherence, motivation, and long-term follow-up of the exercise training program by means of smartphone applications that record exercise activity, video conferences, audio tapes for relaxation, or chats. These new approaches to cardiac rehabilitation need to be evaluated in order to establish their safety and efficacy.
Conclusions
Exercise training in HF is safe and effective. HIT, especially when associated with strength exercises and IMT, offers the most benefits compared with the traditional CT of moderate intensity. It is also better tolerated in HF patients and this increases adherence. However, we are in need of a big randomized study in patients with HF in order to fully establish the best exercise modality in patients with HF.
We need multidisciplinary Cardiac Rehabilitation programs to make an individual exercise prescription based on risk stratification, exercise capacity, and patient’s preference. There is no single exercise training program that covers all the individual patients’ needs. Therefore, in most cases, a combination of exercise programs such as aerobic interval training or CT, strength exercise and IMT are needed.
And lastly, we must not forget that the Cardiac Rehabilitation Program in HF patients not only includes exercise training but must work side by side with the multidisciplinary heart failure units. Cardiovascular risk factor control, optimization of medical, surgical, and device treatment, psychosocial support, health and self-care education are important in the management of the patient and must be addressed adequately in order to improve the outcomes and quality of life of our HF patients.
References
Recently published papers of particular interest have been highlighted as: • Of importance •• Of major importance
Vogiatzis I, Zakinthinos SG. The physiological basis of rehabilitation in chronic heart and lung disease. J Appl Physiol. 2013;115(1):16–21.
Sayago-Silva I, García-López F, Segovia-Cubero J. Epidemiology of heart failure in Spain over the last 20 years. Rev Esp Cardiol Engl Ed. 2013;66(8):649–56.
Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics-2013 update: a report from the American Heart Association. Circulation. 2013;127(1):e6–245.
Koukoui F, Desmoulin F, Lairy G, et al. Benefits of cardiac rehabilitation in heart failure patients according to etiology. Medicine. 2015;94(7):e544.
•• McMurray JJ, Adamopoulos S, Ander SD, et al. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: the task force for the diagnosis and treatment of acute and chronic heart failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail. 2012;33(14):1787–847. Provides a good overview on how to diagnose and treat heart failure and the evidence available.
• Fleg JL, Cooper LS, Borlaug BA, Haykowsky MJ, et al. Exercise training as therapy for heart failure: current status and future directions. Circ Heart Fail. 2015;8(1):209–20. Good review on the evidence for using exercise training as a therapy for heart failure.
Haykowsky MJ, Kitzman DW. Exercise physiology in heart failure and preserved ejection fraction. Heart Fail Clin. 2014;10(3):445–52.
• Southern WM, Ryan TE, Kepple K, Murrow JR, Nilsson KR, Mc Cully KK. Reduced skeletal muscle oxidative capacity and impaired training adaptations in heart failure. Physiol Rep. 2015;3(4):e12353. Good review of the peripheral mechanisms that impact impaired exercise capacity in heart failure patients.
Downing J, Balady GJ. The role of exercise training in heart failure. J Am Coll Cardiol. 2011;56(6):561–9.
• Loutaris ID, Adamopoulos S, Manginas A, et al. Benefits of combined aerobic/resistance/inspiratory training in patients with chronic heart failure. A complete exercise model? A prospective randomized study. Int J Cardiol. 2013;167:1967–72. Randomized study on diferent exercise modalities in heart failure.
Cahalin LP, Chase P, Arena R, Myers J, et al. A meta-analysis of the prognostic significance of cardiopulmonary exercise testing in patients with heart failure. Heart Fail Rev. 2013;18(1):79–94.
Green DJ, Eijsvogels T, Bouts YM, Maiorana AJ, et al. Exercise training and artery function in humans: nonresponse and its relationship to cardiovascular risk factors. J Appl Physiol. 2014;117(4):345–52.
Tu R-H, Zeng Z-Y, Zhong G-Q, et al. Effects of exercise training on depression in patients with heart failure: a systematic review and meta-analysis of randomized controlled trials. Eur J Heart Fail. 2014;16(7):749–57.
Lavie CJ, Arena R, Swift DL, et al. Exercise and the cardiovascular system: clinical science and cardiovascular outcomes. Circ Res. 2015;117:207–19.
•• Taylor RS, Sagar VA, Davies EJ, Briscoe S, Coats AJ, Dalai H, Lough F, Rees K, Singh S. Exercise based rehabilitation for heart failure. Cochrane Database Syst Rev. 2014;4:CD003331. Cochrane review on the evidence behind exercise based rehabilitation in heart failure.
• Chrysohoou C, Tsitsinakis G, Vogiatzis I, Cherouveim E, et al. High intensity, interval exercise improves quality of life of patients with chronic heart failure: a randomized controlled trial. QJM. 2014;107(1):25–32. Interesting trial regarding the use of HIT.
• Chrysohoou C, Angelis A, Tsitsinakis G, et al. Cardiovascular effects of high-intensity interval aerobic training combined with strength exercise in patients with chronic heart failure. A randomized phase III clinical trial. Int J Cardiol. 2015;20(179):269–74. Interesting trial regarding the use of HIT.
Cipriano G Jr, Cipriano VT, da Silva VZ, Cipriano GF, Chiappa GR, de Lima AC, Cahalin LP, Arena R. Aerobic exercise effect on prognostic markers for systolic heart failure patients: a systematic review and meta-analysis. Heart Fail Rev. 2014;19(5):655–67.
• Kitzman DW, Brubaker PH, Herrington DM, Morgan TM, et al. Effect of endurance exercise training on endothelial function and arterial stiffness in older patients with heart failure and preserved ejection fraction: a randomized, controlled, single-blind trial. J Am Coll Cardiol. 2013;62(7):584–92. Interesting study that studies the effects of exercise training in endothelial function in patients with heart failure and preserved ejection fraction
•• O´Connor CM, Whellan DJ, Lee KL, et al. Efficacy and safety of exercise training in patients with chronic heart failure: HF-ACTION randomized controlled trial. JAMA. 2009;301(14):1439–50. The largest and most important randomized trial regarding the use of exercise as treatment for heart failure.
•• Mentz RJ, Schulte PJ, Fleg JL et al. Clinical characteristics, response to exercise training, and otcomes in patients with heart failure and chornic obstructive pulmonary disease: findings from Heart Failure an A Controlled Trial Investigating (HF.Action). Am heart J. 2013;165(2): 193–9. The largest and most important randomized trial regarding the use of exercise as treatment for heart failure
Ades PA, Keteyian SJ, Balady GJ, et al. Cardiac rehabilitation exercise and self-care for chronic heart failure. JACC Heart Fail. 2013;1(6):540–7.
Krumholz HM. Post-hospital syndrome-an acquired, transient condition of generalized risk. N Engl J Med. 2013;368(2):100–2.
• Esposito F, Reese V, Shabetai R, Wagner PD, Richardson RS. Isolated quadriceps training increases maximal exercise capacity in chronic heart failure: the role of skeletal muscle convective and diffusive oxygen transport. J Am Coll Cardiol. 2011;58(13):1353–62. Interesting mechanistic study
Pg Agostoni, Corrà U, Cattador G, et al. Metabolic exercise test data combined with cardiac and Kidney indexes, the MECKI score: a multiparametric approach to heart failure prognosis. Int J Cardiol. 2013;167(6):2710–8.
Corrà U, Fiepoli MF, Adamopoulos S, et al. Cardiopulmonary exercise testing in systolic heart failure in 2014: the evolving prognostic role. A position paper from the Committee on Exercise Physiology and Training of the Heart Failure Association of the ESC. Eur J Heart Fail. 2014;16(9):929–41.
•• Smart NA, Dieberg G, Giallauria F. Intermittent versus continuous exercise training in chronic heart failure: a meta-analysis. Int J Cardiol. 2013;166(2):352–8. Meta-analysis that includes all the recently published studies regarding intermittent versus continuous exercise training.
Haykowsky MJ, Timmons MP, Kruger C, et al. Meta-analysis of aerobic interval training on exercise capacity and systolic function in patients with heart failure and reduced ejection fractions. Am J Cardiol. 2013;111(10):1466–9.
• Fu TC, Wang CH, Lin PS, Hsu CC, et al. Aerobic interval training improves oxygen uptake efficiency by enhancing cerebral and muscular hemodynamics in patients with heart failure. Int J Cardiol. 2013;167(1):41–50. Interesting mechanistic study on the benefits of aerobic interval training
Ramos JS, Dalleck LC, Tjonna AE, et al. The impact of high-intensity interval training versus moderate-intensity continuous training on vascular function: a systematic review and meta-analysis. Sports Med. 2015;45(5):679–92.
Iellamo F, Caminiti G, Sposato B, et al. Effect of high-intensity interval training versus moderate continuous training on 24 h blood pressure profile and insulin resistance in patients with chronic heart failure. Intern Emerg Med. 2014;9(5):547–52.
Iellamo F, Manzi V, Camininti G, et al. Matched dose interval and continuous exercise training induce similar cardiorespiratory and metabolic adaptations in patients with heart failure. Int J Cardiol. 2013;167(6):2561–5.
• Koufaki P, Mercer TH, George KP, Nolan J. Low-volume high-intensity interval training vs continuous aerobic cycling in patients with chronic heart failure: a pragmatic randomized clinical trial of feasibility and effectiveness. J Rehabil Med. 2014;46(4):348–56. Study comparing different exercise modalities
• Benda NM, Seeger JP, Stevens GG, Hijimans-Kersten BT, et al. Effects of high-intensity interval training versus continuous training on physical fitness, cardiovascular function and quality of life in heart failure patients. PLoS ONE. 2015;10(10):e0141256. Study comparing different exercise modalities
• Aksoy S, Findikoglu G, Ardic F, et al. Effect of 10-week supervised moderate-intensity intermittent vs. continuous aerobic exercise programs on vascular adhesion molecules in patients with heart failure. Am J Phys Med Rehabil. 2015;94(10 Suppl 1):898–911. Study comparing different exercise modalities
Skaug EA, Aspenes ST, Oldervoll L, et al. Age and gender differences of endothelial function in 4739 healthy adults: the HUNT3 Fitness Study. Eur J Prev Cardiol. 2013;20(4):531–40.
Arena R, Myers J, Forma DE, et al. Should high-intensity-aerobic interval training become the clinical standard in heart failure? Heart Fail Rev. 2013;18(1):95–105.
• Ismail H, McFarlane JR, Nojoumian AH, et al. Clinical outcomes and cardiovascular responses to different exercise training intensities in patients with heart failure: a systematic review and meta-analysis. JACC Heart Fail. 2013;1(6):514–22. Good review on the benefits of different training intensities.
•• Adamopoulos S, Schmid JP, Dendale P, et al. Combined aerobic/inspiratory muscle training vs. aerobic training in patients with chronic heart failure. The Vent-HeFT trial: a European prospective multicentre randomized trial. Eur J Heart Fail. 2014;16:574–82. Randomized study comparing the benefits of adding inspiratory muscle training to aerobic training.
• Marco E, Ramirez-Sarmiento AL, Coloma A, et al. High-intensity vs sham inspiratory muscle training in patients with chronic heart failure: a prospective randomized trial. Eur J Heart Fail. 2013;15(8):892–901. Randomized study comparing the benefits of inspiratory muscle training
Angadi SS, Mookadam F, Lee CD, et al. High-intensity interval training vs. moderate-intensity continuous exercise training in heart failure with preserved ejection fraction: a pilot study. J Appl Physiol. 2015;119(6):753–8.
Pandey A, Parashar A, Kumbhami DJ, et al. Exercise training in patients with heart failure and preserved ejection fraction. Meta-analysis of randomized control trials. Circ Heart Fail. 2015;28(1):33–40.
Piña IL, Bittner V, Clare RM, et al. Effects of exercise training on outcomes in women with heart failure: analysis of HF-ACTION by sex. JACC Heart Fail. 2014;2(2):180–6.
•• Cooper LB, Mentz RJ, Sun J-L, et al. Psychosocial factors, exercise adherence, and outcomes in heart failure patients. Insights from heart failure: a controlled trial investigating outcomes of exercise training (HF-ACTION). Circ Heart Fail. 2015;8(6):1044–51. Important sub-study of the HF-ACTION trial regarding adherence, psychosocial factors and outcomes
Sparling PB, Howard BJ, Dunstan DW, Owen N. Recommendations for physical activity in older adults. BMJ. 2015;350:h100.
Zhao G, Chaoyang L, Ford ES, et al. Leisure-time aerobic physical activity, muscle-strengthening activity and mortality risks among US adults: the NHANES linked mortality study. Br J Sports Med. 2014;48:244–9.
Turk-Adawi K, Grace SL. Smartphone-based cardiac rehabilitation. Heart. 2014;100:1737–8.
Lear SA, Singer J, Banner-Lukaris D, et al. Randomized trial of a virtual cardiac rehabilitation program delivered at a distance via the internet. Circ Cardiovasc Qual Outcomes. 2014;7(6):952–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Marta Gómez-Cuba, Ana Perreau de Pinninck-Gaynés, Rosa Planas-Balagué, Nicolás Manito, and José González-Costello declare that they have no conflict of interest
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical collection on Cardiopulmonary Rehabilitation.
Rights and permissions
About this article
Cite this article
Gómez-Cuba, M., Perreau de Pinninck-Gaynés, A., Planas-Balagué, R. et al. Rehabilitation in Heart Failure: Update and New Horizons. Curr Phys Med Rehabil Rep 4, 208–215 (2016). https://doi.org/10.1007/s40141-016-0125-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40141-016-0125-6