Abstract
In this chapter, we will describe how infrared thermography (IRT) can help us to prevent and monitor injuries, always based on the use of standardised protocols. We will explain some of the main physiological aspects and will enumerate the main applications, with examples gathered from our research and professional experience with top sport athletes and teams. To summarize, IRT can help us to reduce injury incidence and to increase the performance in a non-invasive, fast and objective way.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
4.1 Introduction: How Can Infrared Thermography Help Us to Prevent/Monitor Injuries?
Despite the improvement of technology in recent decades, injuries are still a huge problem for professional and amateur athletes and sport institutions. Moreover, injuries are not just a health matter, but also an economic problem for the team or athlete [1], and obviously a factor influencing individual and team performance.
Nevertheless, we cannot deny the significant and useful changes that new technologies are bringing to sport professionals in order to reduce the injury incidence. One of the key factors is related to the quantification of training loads: internal and external. We speak about a new perspective that has arisen since the advent of tools that help to control the training loads. On one hand, we have the external loads, such as global positioning systems that calculate distances, acceleration, impacts, and so on. On the other hand, we have the internal loads to quantify the biological responses of each individual according to the type of training. In both cases technological tools have been developed to quantify how the athlete is assimilating the training load .
One of the most significant works about the relationship between the workload and the risk of injuries was made by Gabbett and Jenkins in which they identified how the distribution of internal load affect in the incidence of injuries [2]. This study is a milestone in sports science for determining how stimuli affect training in injury prevention. Some years later, Gabbett exposed the fact that the training-injury prevention paradox is based on situation where a training workload control becomes the main tool for injury prevention [3].
In this context, we found different technologies, tools and methods focused on the injury prevention. Among all of them, we identify infrared thermography (IRT) as one of the most interesting technologies for preventing injuries in humans. In recent years, some authors have described how this old technology can be used as tool for injury prevention [4–9].
IRT is a safe, non-invasive and low-cost technique that allows for the rapid and non-invasive recording of radiating energy that is released from the body. IRT measures skin temperature (Tsk) and has been widely used since the early 1960s in different sectors. During the first decades after its development, research into the use of IRT in humans was mainly focused on its applications as a diagnostic tool. However, IRT was replaced by newer and more accurate technologies (such as X-rays and magnetic resonance imaging). Recent technical advances in infrared cameras have made new human applications of IRT (beyond diagnostic techniques) possible. Among others, the prevention and monitoring of injuries has been shown to be one of the most interesting and useful applications because of its ability to identify changes in body surface temperature, reporting on the metabolism of active muscles and monitoring training workload [10].
It is widely known that there is a correlation between muscle activation and the variation of skin temperature [11]. Depending on the type of exercise and intensity, the area adjacent to the muscles involved in the exercise could experience a decrease or increase of the skin temperature , as result of a combination of factors, such as metabolism, muscle contraction, sweating or skin blood flow [12].
Ideally, our skin is supposed to maintain a constant thermal pattern over time, with the constant aim of keeping the body in thermal balance or “homeothermy” [13]. However, a lot of factors can affect the thermal asymmetry of a person during their lifetime, and most of them are related to pathological reasons such as inflammation or nerve dysfunctions [14].
In this sense, IRT can help us to identify thermal asymmetries by comparing bilateral body areas (e.g., left and right knee, or dominant and non dominant calf) [15, 16]. Thermal asymmetries on those regions of interest (ROIs) may indicate a non pathological pattern (related to dominance factors or ancient injuries or surgeries), but also it could show us a potential injury risk due to an incorrect workload assimilation, excessive activity, asymmetrical exercise execution or muscle overload. Those asymmetries could appear before other indicators as pain, which is extremely useful for implementing preventive strategies before injury occurs. In this way, IRT can be used not only to identify those thermal asymmetries, but above all to identify the reasons for such asymmetry and to modify the training load to come back to the thermal balance.
Moreover, IRT can be also extremely useful once an injury occurs, because we can monitor the thermal asymmetry evolution in order to check if the rehabilitation process is correctly stimulating the areas involved and taking as reference the thermal pattern before the injury [17, 18].
Obviously, there are a lot of factors affecting skin temperature [19], which makes it in some cases impossible to prevent certain injuries. Nevertheless, the frequent record of thermal images allows for an individual comparison of thermal asymmetries over time, providing a reliable database evolution that is a key factor in determining the normal thermal values of a subject, and therefore for individualizing and better understanding any changes to the thermal pattern, and therefore the reasons that may lead to a thermal asymmetry.
To summarize, IRT represents a fast, cheap and useful technique that allows the sport and health professionals to better understand the physiology and health status of a subject. Indeed, if IRT is used following a standardized protocol, with a reliable analysis method or software, and combined with other technologies and the collaboration of different sport professionals, it could really help to decrease the injury incidence [5–9, 20, 21].
4.2 The Protocol: Methodological Aspects and Equipment Requirements
IRT is not a perfect technique. Therefore, the use of a standardized protocol seems to be absolutely essential for ensuring the quality of the thermal results [22].
We are also aware of the differences between using IRT in a scientific context, or facing the reality out of a laboratory. As researchers, we must always try to maintain the protocol quality, nevertheless we should also be able to manage real situations with top elite athletes and institutions where not all the elements are under control, but the results must be still excellent.
In addition to the Chap. 3 of this book, we will enumerate some of the more recognised protocols. Then we will show a synopsis from the TERMOINEF “Protocol for thermographic assessment in humans” [23]. Finally, we will describe the different approaches to analyzing thermal images: qualitative and quantitative analysis.
4.2.1 Thermographic Protocols in the Literature
In recent years, several organisations from the health sector have generated and published their own protocols and quality assurance guidelines . For example, below we list some of the most relevant publications in the last several years:
-
(a)
In 2002, IACT published Standards and Protocols in Clinical Thermographic Imaging, which describes some of the basic requirements for performing an accurate clinical assessment with IRT [24].
-
(b)
In 2004, the International Organisation for Standardisation (ISO) published ISO 9886 focusing on the ergonomic evaluation of thermal strain by physiological measurements [25].
-
(c)
In 2006, Schwartz published a complete guideline prepared by members of the American Academy of Thermology (AAT) [26]. The guide was aimed at neuromuscular thermologists and other interested parties.
-
(d)
Among the large number of academies, associations and societies, the European Association of Thermology (EAT) has been one of the most active institutions in recent years in publishing IRT-related studies. The University of Glamorgan group (recently renamed South Wales University) has worked to better understand the technical factors that affect IRT measurements and to create a strict protocol for reducing errors and increasing the accuracy and the precision of temperature measurements [22, 27–35]. Ring and Ammer published one of the most cited works regarding the requirements for using IRT in the medical sector [34]. Other authors from this active group have noted important factors in quality assurance [32] or specific applications in fever screening [31]. Most of the works are summarized in the Glamorgan Protocol [29].
-
(e)
Most recently, the research group from the Technical University of Madrid, presented during the XIII EAT Congress in 2015 a “Protocol for thermographic assessment in humans” [23], gathering the most recent updates and results from the research and professional experience of the previous years. The report was reviewed by Kurt Ammer and the EAT scientific board.
To summarize, most thermographic guidelines agree on the following items:
-
1.
Location requirements
-
2.
Equipment characteristics
-
3.
Subject/patient information and preparation
-
4.
Subject/patient assessment
-
5.
Processing and presentation of results.
Regardless of the protocol followed, it is clear that it is absolutely necessary to follow standardised guidelines when using IRT in humans to avoid risking the quality and objectivity of our research or professional work on IRT.
4.2.2 The “TERMOINEF” Thermographic Data Collection Protocol
The TERMOINEF protocol aims to integrate and agree on the most important points with other protocols in the literature [23]. In addition to what was described in Chap. 3, TERMOINEF is a general protocol for taking thermal images with humans, but it has been mainly used in the exercise sector with the aim of injury prevention. Below we will summarize some of the most important points from this and other protocols.
-
Considerations Prior to the Assessment
Before the assessment, it is highly recommended to have an informative session with the athlete being assessed or the medical staff and professionals involved if they are not familiar with thermography. In this session, which may be physical or virtual, the subjects will be provided with written information, including information about IRT, the processes to be followed during data collection, the type of information to be provided in the final report, and recommendations to be followed before the thermographic session.
We all know that in some institutions and teams, the access to top elite athletes is restricted, but this information should be provided at least to the medical staff so that they could inform them or at least take into account the following factors before the session:
-
All evaluations of the same subject should be conducted at the same time.
-
No physical activity should be performed for at least 6 h prior to the evaluation (so, ideally before the first training session).
-
Avoid the application of creams, gels or sprays on the skin area to be evaluated
-
Avoid coffee, alcohol or stimulants for 6 h prior to the evaluation.
-
Do not smoke in the 6 h prior to the assessment.
-
Do not receive any treatment or massage (it is especially important to coordinate the session with the physiotherapists, so they do not proceed before the evaluation).
-
Avoid direct sun or UV sessions before evaluation.
-
The previous day (when possible), avoid any drugs or treatment with any substance that may alter the normal thermogram.
-
Avoid taking a shower or bath before the evaluation.
-
Do not alter rest or meal habits.
In addition to that and since not all facilities are perfectly adapted to data collection, it is highly advisable to visit the location before the day, or with enough time to get it adapted. Sometimes, the only place available is some space in the changing room or near to the place the athletes prepare themselves before the training session. We suggest that it should not occur in a place where the humidity of the showers could change the room temperature and humidity.
Likewise, sometimes the acclimatisation period must be reduced in order to get the most of the athletes assessed. In this case and although some authors have demonstrated the importance of having at least 15 min [36], we prefer to get the thermal images without an ideal acclimatisation period rather than having no measurement. Since we take into account this and other potential influence factors, we can afterwards better interpret the results relating to thermal asymmetries, which are theoretically not that influenced because, in most cases, the factors affect the whole body equally. Standarized protcols are very important and we must try to use them always, but in specific cases (which are common with top athletes), it is better to have the thermal images despite not having them.
-
Selection of the Camera
We strongly recommend using a thermal imaging camera with a resolution equal to or greater than 320 (horizontal) × 240 (vertical) pixels, a minimum sensitivity of 65 m K, a measurement range covering the possibilities of the human environment (between 0 and 50 °C), a thermal sensitivity of 0.02 °C or lower, and standard data outputs for a PC. The resolution of the camera is one the most important factors for obtaining a high-quality thermal images. A camera with a high resolution will provide a sharper image and a greater number of pixels of the considered ROI, and will improve the quality and reliability of the results.
In recent years, some camera manufacturers have launched low-cost cameras with attractive prices but poor resolution features. Some authors have already analyzed their performance and concluded that they do not have the minimum technical requirements to perform a reliable analysis [37].
Even if it sounds strange, nowadays, most of thermal cameras used with humans are designed and manufactured for other applications, such as industry, security and construction (there is not a specific need to measure 150 °C when working with human skin). However, the potential for sports and human applications for IRT is such a reality that some companies are already working on specific cameras that may be launched by the end of 2016. The more specific they are for human application, the higher the quality of the results will be.
-
Considerations on the Evaluation Day
On the day of data collection it is necessary to carry out the following steps before starting:
-
The first day, the subject should be briefly informed about the characteristics of thermography, the purpose of the data collection and the data details (including anonymity and data processing).
-
On the first day, subjects have to sign the informed consent.
-
The subject has to undress, staying in underwear (women preferably without bra) for around 10–15 min to acclimate to the temperature of the room, which should be between 18 and 25 °C (ideal: 21 °C).
-
During the acclimatization time, we recommend performing a survey with questions concerning the existence of possible influencing factors such as the previous training session, the intake of medicaments, the application of creams or ice on the skin and other influencing factors gathered in the literature [19].
The technician/researcher
The person charged with carrying out the evaluation must perform the following tasks before starting:
-
To prepare the room at a suitable temperature (between 18 and 25 °C).
-
To turn on the IRT camera at least 20’ before (to avoid calibration problems).
-
To prepare the tripod (if necessary).
-
To locate a step to elevate the subject and isolate the feet from the cold floor. Placing marks on the step will help to standardise the location of the subject’s feet.
-
To prepare roll up (if necessary) or make sure to have a proper and non-reflecting background.
-
To turn on the weather station.
-
To prepare the “black body” or calibration system (if necessary).
-
To check with the IRT camera any radiation source in the room (hot pipes, windows, etc.).
-
To prepare the notebook with questionnaire data collection for each subject or have a software ready to take those data.
-
To turn on the computer, which will be used for transfer and analysis of the photos.
-
To check the card or USB drive (or the connection of the camera to the computer) for the data acquisition.
-
To turn on the computer, which will be used to transfer the photos and to analyze them.
Camera position
This depends on the subject’s height. Normally, it is placed between 2.5 and 3 m (for a subject of 1.70 m height). Regarding the height of the camera, it will be located so that the centre of the image matches the geometric centre of the area to be evaluated (about 65 cm for the lower limbs and 125 cm for the upper body). It is important to keep the IRT camera in a perpendicular angle in relation to the subject. There will be a transparent template to guide the technician on the placement of the subject (see Figs. 4.1, 4.2 and 4.3).
Other protocols, such as the one from Glamorgan [29], have proposed different body views in order to get closer images from the ROIs to be analyzed. Our proposal is based on four thermal images: two from the upper body and two from the lower limb, anterior and posterior views. Obviously, closer perspectives are richer in number of pixels and therefore in objective information, but our proposal is also adapted to specific situations with a lack of time; we can get the whole body from an athlete analyzed with just four images, which is very convenient when we must assess 20 players as fast as possible. We also trust our software analyses and its reliable performance [12] in that the results produced will be good enough to inform decisions and to make a good interpretation.
During the evaluation
Subjects have to follow the following instructions in lower body images (Fig. 4.2):
-
The subject stands on a “step” platform to raise his feet (about 10 cm).
-
Maintaining an anatomical position (upright and symmetrical).
-
Slightly open legs (about 40 cm).
-
Feet straight toward the camera.
-
Looking ahead.
-
Arms crossed or hands behind the head in lower body images.
-
Feet must be clearly distinguishable from the background.
-
Use of the transparent template as a reference:
-
The lower brands are the places where feet should appear.
-
The crossing of the two lines coincides with the abductors area.
-
The highest point on the vertical line must match the navel.
-
In the case of upper body images (Fig. 4.3),
-
The subject stands on a “step” platform to raise his feet (about 10 cm).
-
Maintaining an anatomical position (upright and symmetrical).
-
Same leg position.
-
Looking ahead.
-
Arms relaxed, stretched and slightly supinated so you can see the front or back of the forearm.
-
Both hands with fists clenched.
-
The head and fists must be clearly distinguishable from the background.
-
The transparent template might be used as reference.
-
The temperature bar is just above the knees.
-
The body shape must fit on the image (see Fig. 4.3). That is, the head should be very close to the top edge and the hands to the lateral edges of the image.
-
4.2.3 Thermal Image Analysis
Once the thermal image is taken, the professional has two main ways to analyze the thermograms: qualitative and quantitative methods.
The quality of the qualitative analysis depends on the experience of the thermographer. The image is interpreted by analyzing the color patterns of the thermograms, and a correct analysis depends on the accurate settings of the camera’s temperature ranges. This method can help to identify the most evident asymmetries, but it could be that significant asymmetries are not seen.
The quantitative analysis makes thermography more objective and reliable. It records thermal data (normally maximum, minimum, average and standard deviation) from each ROI by manual or automatic procedures. The thermal results of each ROI can be compared with contralateral or adjacent ROIs of the same subject or with the same ROI of other subjects. In that case, the thermal results for each ROI can be compared with previous thermograms independent of the temperature range settings (Fig. 4.4).
Flow chart of the analysis of thermograms. Figure adapted from Sillero-Quintana et al. [23]
-
Manual
One of the most controversial points regarding IRT applications in humans is the selection of the ROIs . Many IRT studies have developed their own criteria for creating and selecting ROIs.
The controversy around ROI selection is based on the manual procedure that is required to create ROIs. We observed that the reliability of ICC results (intra- and inter-examiner Correlation Coefficient ICC) were often suboptimal, due to factors that depended on the ability of the observer to manually select the ROI [34, 38]. In some cases of specific thermal images (analyzing closer ROI) it could be appropriated, but the fact that the results will be more difficult to compare with time and with other subjects if the observer is different should be taken into account.
-
Automatic
To improve reliability and to open up the possibility of comparing IRT results among studies, we suggest the development of automatic and objective procedures to select the ROI. In this sense, software solutions with automatic ROI selection features would be a first step, such as that proposed by different research groups [6, 39–41].
Among all of them, we highlight ThermoHuman. It is a big data Software as a Service (SaaS) online program that uses an applied automatized computer vision solution to obtain human body thermal data. Day-to-day data points are extracted for monitoring thermal asymmetries to help sports professionals in the objective decision-making process and to help avoid injuries. It uses both thermal and personal variables, such as previous injuries, type of sport, dominance, age, height, weight or body mass index, and offers the chance to filter all this information and correlate variables in order to prevent sport injuries.
The ROIs extracted by ThermoHuman allow the professional to obtain the average, maximum, minimum, standard deviation and, of particular importance for data analysis, the number of pixels from each ROI. Currently, there are four protocols that divide the human body in four regions: upper anterior, upper posterior, lower anterior and lower posterior (Fig. 4.5), but more protocols will be developed in the future.
ThermoHuman uses the same procedure than the previous non-commercial version, Termotracker, which was tested with excellent reliability results [12].
We highly recommend performing the thermographic evaluation before the training session. In those cases, it is especially important to get the results as soon as possible, because one of the most interesting advantages of IRT is to obtain fast and objective results that allows the medical and technical staff to take decisions regarding the adaptation of training if needed, obviously before the session starts. This possibility is only possible by performing an automatic analysis , since manual analysis would not be sufficiently fast to get the outcomes before the training, and, obviously, the results would not be that reliable. In addition to that, automatic analysis helps to compare thermal images of the same subjects or between athletes, so we can get a better and reliable perspective for our athletes and/or team through the time.
Therefore, when using IRT to prevent injuries, it is absolutely necessary to analyze the thermal images with an automatic process (e.g., software ) to get more possibilities for preventing injuries or just to adapt the training based on the physical status the athlete.
4.3 The Athlete: Physiology Concepts: From Thermal Asymmetry to Thermal Pattern
In order to understand how IRT can be used, we must describe some aspects related to the subject of physiology . Concepts such as thermal homeostasis and thermal symmetry/asymmetry are the basis for understanding how can we detect injury risk areas.
Another concept worth highlighting is the thermal profile, or the specialization thermal characteristics derived from a sport discipline or concrete performance.
Finally, it is also worth to summarizing the factors affecting human skin temperature.
4.3.1 Biological Principles
Human skin, with an emissivity (an object’s ability to emit radiation) of 0.98, is almost equal to a black body radiator [42]. The physics of heat radiation and the physiology of thermoregulation in the human body make the reliable and valid interpretation of thermal images difficult. Skin temperature regulation is a complex system that depends on blood-flow rate, local structures of subcutaneous tissues and the activity of the sympathetic nervous system [43]. However, there is evidence that the sympathetic nervous system is the primary regulator of blood circulation in the skin and is, therefore, the primary regulator of thermal emission [44]. Vasoconstriction and vasodilation of the blood vessels function to regulate blood flow in the skin. Thermoreceptors in the skin, also known as Ruffini corpuscles, recognize the ambient temperature. An increased temperature results in vasodilation, leading to increased blood flow to the skin, whereas vasoconstriction occurs by a decrease in temperature and results in reduced blood flow to the skin [45]. These physiological processes combine with heat transfer and thermoregulation in convection, conduction, radiation and sweat evaporation. Heat transfer by radiation is of great value in medicine [46]. To date, the mechanism of thermoregulatory adaption to exercise is complex and not entirely understood.
-
Heat exchange between the human body and environment
In the case of the human body, the high metabolic activity generates a great amount of thermal energy, which must be dissipated to maintain the stability of the physiological processes of the body [47]. The mechanisms used by the human body to transfer the calorific energy are: conduction, convection, radiation and evaporation (see Fig. 4.6).
The heat transfer by emission and absorption of radiation is called thermal transfer by radiation. We invite the reader to consult Chap. 2 of this book and the work of Incropera [48] or any other literature reference belonging to the field of physics in order to deepen their knowledge about the topic of energy transfer by radiation.
Bodies emit thermal radiation due to their temperature: the higher the temperature, the more thermal radiation that is emitted. However, each material has a different emissivity (see Chap. 2 of this book for emissivity values of different materials).
Emissivity is the ability of each object to emit infrared radiation [49]. Not all objects emit 100% of what they should; if they did so, the infrared signal that would be able to pick up a camera would be directly related to the temperature, according to the Stefan-Boltzmann Law, which relates directly to the energy temperature irradiated.
From the amount of energy dissipated by the human skin, approximately 60% is in the form of infrared radiation [47], and the remaining 40% corresponds to convection. Normally, when working with opaque bodies (as human bodies), the transmissivity is equal to “0”, because the radiation is unable to pass through the body. Consequently, the main concepts in working with radiation and human bodies are the emissivity and reflectivity.
4.3.2 Thermal Homeostasis, Thermal Symmetry/Asymmetry and Thermal Profile
Given that certain physiological disorders may influence the local exchange thermal response [21, 50–52], the use of thermography in sports can help to prevent muscle, joint or tendon injuries since, in cases of overuse or overtraining, the local temperature of the affected areas may be increased, compared with other similar areas or to the contralateral body region [7]. IRT can detect thermal asymmetry that could lead to injury, with its consequent impact on performance and health of athletes, team planning and even, in cases of professional sport or high performance, the economic impact for the athlete or club.
With a periodic thermographic monitoring of the athlete, a specific thermal profile of both the subject and the sport discipline or the team can be created; that is, a “map” with the normal thermal characteristics of each ROI, such as the frontal and posterior legs of a soccer player. Thus, any abnormal temperature rise in both legs or in one specific region, or that takes place continuously or more intensely than normal in an athlete can be related to an inflammatory process [21, 51]. This situation may occur as a result of: a load of training above the assimilative capacity of the athlete, being able to produce a risk of damage by overload; or inappropriate development of recovery patterns, such as balanced nutrition, hours of rest or specific physiotherapy treatments. In any case, it will be necessary to evaluate the cause of the thermal alteration before an injury occurs.
Considering the concept of anatomical proportionality, the thermal response between two contralateral body parts is expected to be symmetrical [53, 54]. Thermal monitoring comparing bilateral body parts indicates that differences up to 0.25 °C [53], 0.4 °C [55], 0.5 °C [15], or 0.62 °C [56] are considered as acceptable. However, differences above these values may indicate that the ROI with a higher or lower temperature, contrasted with the individual’s usual thermal profile settings, might have some inflammatory problem (hyperthermia ) or degenerative (hypothermia ) [21, 51, 55, 57].
According to our research and practical experience, we propose a “level of attention” scale to be considered depending on the bilateral temperature differences recorded (Table 4.1).
Based on the table above showing indications for the level of attention, it should be borne in mind that a difference ≤0.4 °C would be considered normal [53–55]. For levels higher than 0.5 °C, the following would be advised: (a) verifying if some external factor could be influencing the result; (b) monitoring the athlete to assess his/her environmental and training conditions; (c) increasing the frequency of monitoring. We never recommend taking drastic decisions after the first negative assessment. In the case that the difference is repeated in the second assessment, an appropriate intervention by the physician, physical therapist or trainer would be recommended, and the intervention should last until the differences come back into an acceptable range considering the normal values of the athlete.
With values classified as “prevention “, an immediate decrease in training load or even training suspension is recommended, since when values are higher than 0.8–1.0 °C the existence of a significant inflammatory process [51] or a risk of injury in an ROI is clearly described, even without prior symptoms of pain, and a medical and/or physiotherapy evaluation of the athlete is recommended. The state of “alarm” imposes an immediate suspension of training and a medical and physiotherapy assessment. The “High Severity” status indicates a difference that may be pathological or a sign of major injury; as in other cases, coordination with the medical team is essential to determine the actual state of the athlete.
However, to properly apply the ranges of severity from Table 4.1, we must always consider the individual thermal profile of the athlete and the sport practiced, since the previous injury of athletes or characteristics of the sport practiced can cause imbalances in the thermal baseline profile that are within normal limits for this specific athlete or discipline, and which could lead the criteria to be applied incorrectly. For example, if the specificity of sport always makes the forearm grip 0.4 °C warmer, it may be normal that one day the athlete has a 0.8 °C imbalance in the forearms, and would not require any special attention.
When significant temperature differences are observed, repetition of the assessment is recommended after 15 min to confirm whether this difference is maintained [55]. Another possibility is to spray the area with an alcohol or convection cooling and wait for five minutes to see the thermal response of the area [55]. This technique is known as dynamic thermography [58].
IRT also allows evaluation of the level of metabolic activity when there is a trauma [21] or after surgery [55]. A regular monitoring during the recovery process allows one to track the evolution of the athlete’s thermal profile prior to his/her normal condition before the injury. In addition, the thermographic monitoring allows assessment of whether the medical and physiotherapy intervention evolves as expected.
4.3.3 Factors Influencing the Application of Infrared Thermograhy on Humans
Working with IRT requires taking into account many factors , which could influence either the evaluation or the interpretation of thermal images [38]. Pretending to control such a quantity of factors could entail an “impossible mission”, but in many cases, just the knowledge of these factors is a first but important step. Fernández-Cuevas and collaborators published a comprehensive classification of factors that could affect the use of IRT in humans [19]. They divided them into three main groups (see Fig. 4.7).
Representation of IRT influence factors classification in humans. Figure obtained from Fernández-Cuevas et al. [19]
-
Environmental factors: Related to the place where the evaluation is made.
-
Individual factors: Those related to the subject assessed and his/her personal characteristics, which could influence skin temperature (Tsk). Those will be divided into intrinsic and extrinsic factors.
-
Technical factors: Linked to the equipment used during the IRT evaluation.
As we described in the previous subchapter about protocols, the best way to be aware of the existence of such factors is to use standardised protocols and surveys, so we can note the existence of some of those factors.
4.4 Main Applications of Infrared Thermography in Sport Injury Detection
Physical activity and exercise are one of the most potentially promising IRT applications. Indeed, technological advances in infrared cameras have allowed for a resurgence of investigation in this sector, enhancing new and old applications , such as the following:
-
The quantification of training workload [10, 12, 20, 59–61].
-
The detection of anatomical and biomechanical imbalances [62, 63].
-
The evaluation of fitness and performance conditions [59, 64–66].
-
The detection of high temperature risk in pregnant women [67].
-
The detection of delayed onset muscle soreness (DOMS) [50].
-
The monitoring of fatigue during exercise [68].
-
The support in screening and early diagnosis in emergencies [69].
-
The evaluation of efficiency levels in some disciplines [66, 70].
-
The detection of the lactate threshold [59].
-
The monitoring of the respiration rate [71].
Of all those applications, the one focused on the prevention and monitoring of injuries is the one really grabbing attention from researchers and professionals. IRT is able to provide an easy way to record non-invasive and momentary information of the athlete’s thermal balance. The objective data given by the thermography expert must be analyzed by the coaching staff (physical trainer, injury therapist, medical staff and coach) in a coordinated way. Therefore, the data will be processed by the sport scientist, who is an expert in thermography and a specialist in research in exercise and sport science and in high performance sport. All of this will positively affect the decrease in the number of injuries and the increase in the team performance, allowing the best players to miss the fewest matches. Based on standardised protocols, IRT will allow us to:
-
(1)
Prevent injuries with the previous training information.
-
(2)
Monitor an injury already started.
-
(3)
Know the answer to the training load.
-
(4)
Have additional information on initial evaluations of athletes.
4.4.1 Injury Prevention
A professional football team has an average of 81 injuries per season [75] and it is expected to have 15 muscle injuries in a 25-player squad [76]. Of those muscle injuries, 92% will impact in four areas: hamstring (37%), adductors (23%), quadriceps (19%) and calf muscle (13%). More than 50% of injuries occur in the muscle and tendon, while two-thirds of them are from muscle fatigue, and the remaining third are from trauma [77]. It is important to categorise the risk depending on the type of injury, the areas that are injured and the total number of days the player misses due to the injuries. Knowing this fact will determine an efficient and concise approach to injury prevention, focusing on areas with the highest incidence and severity.
The use of IRT could save the 7.5 million euros that a Spanish First Division League loses on average due to the injuries [1], if it achieved the reductions of 90% muscles injuries and muscle fatigue in professional football, as suggested by Gomez-Carmona [20]. Then, by continuously monitoring the thermal evolution of the comparison of the dominant and non-dominant members of the football player, we will establish optimal ranges of asymmetry [78] that will allow us to have a standard of care (see Table 4.1, shown in the previous subchapter).
Consequently, when an increase in the thermal imbalance between members (Fig. 4.8) is detected, the technical staff can individualise the training process of that player using the following options:
-
Designing specific protocols for the area with asymmetry.
-
Reducing the volume of individual work.
-
Modifying training tasks to avoid impacting the area with asymmetry.
-
Dealing with the physiotherapist.
-
No training (giving rest to the player).
-
Carrying out additional tests (MRI, X-ray etc.) depending on the severity of the asymmetry.
As mentioned in the previous subchapter, for an optimal tracking of the asymmetries , automatic solutions that quantify the temperature of different ROIs are needed. Using an algorithm for artificial vision, each ROI (muscle areas and/or joint) can automatically be identified and, therefore, comparative reports can be carried out easily between a left–right member or a dominant–non dominant in a scientific way and reliable. This allows us to accumulate and manage the data recorded, establishing thermal evolution of each player, which is essential for assessing individual training load and match response.
One example of how IRT can prevent injuries is the one we experienced with a javelin thrower during our work in Olympiastüztpunkt in Hannover, Germany. We used IRT before starting the physiotherapy session, so we could take the images and analyze them to inform the physiotherapist before he started the session, reporting the main asymmetries.
In that case, the athlete complained about pain in his dominant shoulder. Nevertheless, the thermal images after the training showed a colder asymmetry: his dominant shoulder was 0.4 °C colder than the non-dominant shoulder. We asked him to come before training in order to confirm if this thermal pattern was normal, and before the training, the pattern was different: his right shoulder before training was 0.2 °C warmer. That same day, after the training, the colder asymmetry occurred again. Thanks to this information, the physiotherapist could think about a potential nerve compression , and treat the athlete in this way. Hopefully, some weeks after, the pain disappeared and the pattern was different: before and after training, the dominant shoulder was warmer (Fig. 4.9).
Dynamic thermography involves thermal monitoring after a physical stress (cold, heat, exercise) and can be ideal for monitoring possible alterations that are not visible on a daily basis [58]. This technique is often used on the postgame day, involving immersion in cold water that many professional teams perform. In the example of Fig. 4.10, we can observe how the cold stress on the skin temperature is not symmetrical, and therefore we can identify a warmer area around the individual’s left ankle. This warmer area could be related to an old injury or area that has been abnormally activated or irrigated. In this case, this thermal pattern was reported to the medical staff in order to follow the evolution and to determine if there could be any dysfunction or problem.
4.4.2 Injury Follow-Up
In cases we cannot prevent, when injury occurs, IRT can help in the rehabilitation process quantifying the return to the normal thermal of the player. The degree of asymmetry is recommended for the return to training is still to be defined. For example, it is important to investigate from which thermal asymmetry (1.5 °C, 1 °C or even less) is a player ready to start transition from the process of rehabilitation to training after an anterior cruciate ligament injury operation. This would provide the possibility to individualise rehabilitation and may shorten or lengthen periods in response to the thermal response of each player.
In Fig. 4.11 the evolution of a sprained right ankle over the three weeks of the recovery process of a football player is shown. IRT can help us not just to shorten the recovery process by tracking the thermal asymmetry, but also, to check that the healthy body area (in that example, the left leg) is not getting overloaded and therefore increasing the risk of injury in this area.
Furthermore, Fig. 4.12 shows three stages of evolution of the anterior cruciate ligament injury in the right knee of a judoka with a recovery of several months.
The main problem with thermal monitoring lays in the work of analyzing each muscle area in an isolated way in case there are several injuries that need monitoring. In this case, not only knee cruciate ligament injury, but the response from all the adjoining areas such as the tibial, quadriceps and even popliteal [17]. Therefore, computer applications have been created to automate the identification of muscle areas and extract thermal information referring to each of these areas individually. An example is the software TermoTracker, and its new version ThermoHuman, which identifies 80 ROIs of full body enabling the quick preparation of reports to distribute to the technical or medical staff.
We present an Anterior Cruciate Ligament (ACL) injury evolution in a rugby player: from the day before the injury until the return to play (Fig. 4.13). What makes this case study unique is that during the whole process, the rugby player was monitored by IRT.
Before the surgery (from day 12 to 94), the subject followed a progressive programme five days a week with isometric and concentric exercises to prepare the limb muscles and to maintain the physical condition. After the surgery (from day 111 to 242), the rehabilitation programme consisted of a progressive adaptation to gain range of motion, to reduce the inflammation, to strengthen the muscles, and to gain ability and confidence.
The results can be divided into three phases. Firstly, from the injury to the surgery , we saw a decrease in pain perception and regular ΔT variations, from the biggest (+1.20 °C on day 1) to the smallest difference (+0.08 °C on day 82). Secondly, from the surgery (day 95), we found a similar decrease in the evolution of pain, but a different ΔTsk behaviour, which was maintained during the first weeks of the rehabilitation due to the exercises performed (2). The third phase started some weeks before the return to play (day 175), when the subject again felt a “crack” on his right knee during his first game in a training session. ΔTsk (+1.36 °C) and pain increased but, fortunately, ACL was not torn again. We restarted the rehabilitation, which ended on the 27th June 2012 (day 242) with his first game, and the last one of the season for the team.
In conclusion, IRT results were especially useful regarding the return to play: since Tsk is directly related to the inflammation and muscle activity, it helped both the medical and technical staff to adapt and optimize the rehabilitation process. In addition, the subject described to us how IRT helped him to visualize the evolution, and somehow motivated him to move forward despite the relapse (Fig. 4.13).
4.4.3 Training Load Assimilation
The study of the thermal response to training is one of the most promising fields of IRT. If we are able to predict which areas will be activated depending on the exercise carried out, we will be entering the field of predictive analysis. This thermal information combined with external load indicators such as GPS and internal load indicators such as the subjective perception of the effort or heart rate, can give us a more accurate approach regarding how each individual reacts and assimilate different training loads. It could also help either to predict individual or group response to different training stimulus.
An example would be the realization of high intensity interval training (HIIT), and how its different methods (repeated sprint training, sprint interval training, short bouts or long bouts) [79] impact on one or more muscle areas. If the location and intensity of each of the exercises are known at the thermal level, we will be able to anticipate and individualise what type of training will have less risk for a player.
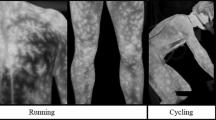
Observing an explosive player profile that has an asymmetry in the hamstring of more than 0.5 °C. During the training and much more in competition, the player will perform a large number of sprints and a very high percentage of high-intensity running, which increases the risk of injury in the most vulnerable areas, such as the hamstring. Considering the thermal asymmetry in the hamstring area, we should avoid HIITs, whose effects can be seen in Fig. 4.14, which increases the effects of the load on that muscle group.
It is not only important to monitor the thermal response immediately after training, but also before starting the session the next day and throughout the week. Sometimes it may appear that residual effects occur, affecting only one of the members, in which localized unilateral temperature patterns are altered (Fig. 4.15) that may constitute a harmful risk if the evolution is not controlled and prevention measures are not taken.
4.4.4 Initial Physical Evaluation
The arrival of a new player to a team involves the medical staff performing a series of tests and evaluations to prove that the player is suitable for physical activity and arrives at the club with a minimum level of fitness. This medical examination includes tests from electrocardiograms to stress tests, but rarely includes tests that reflect vascular alterations as IRT can.
Here is an example of a player in whom a vascular problem was discovered in an initial evaluation in the right lower limb presenting an asymmetry of level four at the knee and thigh. We informed the medical doctor, who transfer the case to the vascular specialist to assess the case and treat the player (Fig. 4.16).
Other thermal changes can also be signs of postural imbalances [62] which, combined with assessments such as tread analysis and manual scan, can increase the success rate in identifying potentially dangerous imbalances for the player.
4.5 Conclusions
IRT has been widely shown to be a tool that can be used by sport professionals with interesting and useful applications. Since IRT is non-invasive, the technology is becoming more accessible in terms of pricing and its results are objective, easy to interpret and fast to get using new software, we strongly believe that IRT will become a commonly used tool, not only by top sport professionals, but also by generic users.
In this sense, our obligation is to highlight the necessity of using IRT with standardised protocols, in order to reduce the influence of factors that can affect the interpretation and results of this technique.
Obviously, IRT is not the final solution for injuries. There is still a lot of research to be performed in order to better understand the human thermoregulation and the skin temperature behaviour. Despite this lack of knowledge, nowadays we can confirm that, based on our research and professional experience in several top sport institutions, IRT is an extremely useful tool to prevent and monitor injuries, and control the individual assimilation of the exercise workload in professional and amateur athletes based on the evolution and asymmetries in skin temperature.
References
Fernández Cuevas I, Gómez Carmon PM, Sillero Quintana M, et al (2010) Economic costs estimation of soccer injuries in first and second spanish division professional teams. In: 15th annual congress of the European college of sport sciences ECSS
Gabbett TJ, Jenkins DG (2011) Relationship between training load and injury in professional rugby league players. J Sci Med Sport 14:204–209. doi:10.1016/j.jsams.2010.12.002
Gabbett TJ (2016) The training—injury prevention paradox: should athletes be training smarter and harder? Br J Sports Med 50:273–280. doi:10.1136/bjsports-2015-095788
Bandeira F, de Moura MAM, de Souza MA et al (2012) Pode a termografia auxiliar no diagnóstico de lesões musculares em atletas de futebol? Rev Bras Med Esporte 18:246–251
Bandeira F, Neves EB, de Moura MAM, Nohama P (2014) A termografia no apoio ao diagnóstico de lesão muscular no esporte. Rev Bras Med Esporte 20:59–64
Barcelos EZ, Caminhas WM, Ribeiro E et al (2014) A combined method for segmentation and registration for an advanced and progressive evaluation of thermal images. Sensors 14:21950–21967. doi:10.3390/s141121950
BenEliyahu DJ (1990) Infrared Thermography in the diagnosis and management of sports injuries: a clinical study and literature review. Chiropr Sports Med 4:41–53
Costello J, Stewart IB, Selfe J et al (2013) Use of thermal imaging in sports medicine research: a short report: short article. Int SportMed J 14:94–98
Tauchmannova H, Gabrhel J, Cibak M (1993) Thermographic findings in different sports, their value in the prevention of soft tissue injuries. Themol Osterr 3:91–95
Čoh M, Širok B (2007) Use of the thermovision method in sport training. Facta Univ-Ser Phys Educ Sport 5:85–94
Kenny GP, Jay O (2007) Sex differences in postexercise esophageal and muscle tissue temperature response. Am J Physiol Regul Integr Comp Physiol 292:R1632–1640. doi:10.1152/ajpregu.00638.2006
Fernández Cuevas I (2012) Effect of endurance, speed and strength training on skin temperature measured by infrared thermography = Efecto del entrenamiento de resistencia, velocidad y fuerza en la temperatura de la piel a través de la termografía infrarroja. Universidad Politécnica de Madrid
Frim J, Livingstone SD, Reed LD et al (1990) Body composition and skin temperature variation. J Appl Physiol Bethesda Md 68:540–543
Ring EFJ (1990) Quantitative thermal imaging. Clin Phys Physiol Meas 11:87. doi:10.1088/0143-0815/11/4A/310
Niu HH, Lui PW, Hu JS et al (2001) Thermal symmetry of skin temperature: normative data of normal subjects in Taiwan. Zhonghua Yi Xue Za Zhi Chin Med J Free China Ed 64:459–468
Uematsu S, Edwin DH, Jankel WR et al (1988) Quantification of thermal asymmetry: part 1: normal values and reproducibility. J Neurosurg 69:552–555
Piñonosa Cano S, Sillero Quintana M, Milanovic L et al (2013) Thermal evolution of lower limbs during a rehabilitation process after anterior cruciate ligament surgery. Kinesiol Zagreb Croat 45:121–129
Piñonosa Cano S (2016) Use of infrared thermography as a tool to monitor skin temperature along the recovery process of an anterior cruciate ligament surgery. Universidad Politécnica de Madrid
Fernández-Cuevas I, Bouzas Marins JC, Arnáiz Lastras J et al (2015) Classification of factors influencing the use of infrared thermography in humans: A review. Infrared Phys Technol 71:28–55. doi:10.1016/j.infrared.2015.02.007
Carmona Gómez P (2012) Influencia de la información termográfica infrarroja en el protocolo de prevención de lesiones de un equipo de fútbol profesional español. (Influence of infrared thermographic information in the injury prevention protocol of a professional spanish footbal team). Universidad Politécnica de Madrid
Hildebrandt C, Raschner C, Ammer K (2010) An overview of recent application of medical infrared thermography in sports medicine in Austria. Sensors 10:4700–4715
Ammer K (2006) Influence of imaging and object conditions on temperature readings from medical infrared images. Pol J Environ Stud (Submitt)
Sillero-Quintana M, Fernández Cuevas I, Arnaiz Lastras J, Bouzas Marins JC (2015) TERMOINEF group: protocol for thermographic assessment in humans
IACT (2002) Thermology guidelines. standards and protocolos in clinical thermography imaging
ISO (2004) Ergonomics—evaluation of thermal strain by physiological measurements. ISO 9886
Schwartz RG (2006) Guidelines for neuromusculoskeletal thermography. Thermol Int 16:5–9
Ammer K (2015) Do we need reference data of local skin temperatures? Thermol Int 25:45–47
Ammer K (2003) Need for standardisation of measurements in thermal imaging. Thermogr Lasers Med Akad Cent Graf-Mark Lodart SA Lodz 13–18
Ammer K (2008) The Glamorgan Protocol for recording and evaluation of thermal images of the human body. Thermol Int 18:125–144
Ammer K, Ring EFJ (2006) Standard procedures for infrared imaging in medicine. In: Biomedical engineering handbook. CRC Press, Boca Raton
Mercer JB, Ring EFJ (2009) Fever screening and infrared thermal imaging: concerns and guidelines. Thermol Int 19:67–69
Plassmann P, Ring EFJ, Jones CD (2006) Quality assurance of thermal imaging systems in medicine. Thermol Int 16:10–15
Ring EFJ, Ammer K (2012) Infrared thermal imaging in medicine. Physiol Meas 33:R33–46. doi:10.1088/0967-3334/33/3/R33
Ring EFJ, Ammer K (2000) The technique of infrared imaging in medicine. Thermol Int 10:7–14
Ring EFJ, Ammer K, Wiecek B et al (2007) Quality assurance for thermal imaging systems in medicine. Thermol Int 17:103–106
Hart J, Owens EF (2004) Stability of paraspinal thermal patterns during acclimation. J Manipulative Physiol Ther 27:109–117. doi:10.1016/j.jmpt.2003.12.006
Vardasca R, Gabriel J (2016) Is the low cost thermal camera FLIR C2 suitable for medical thermal measurements? Thermol Int 26
Zaproudina N, Varmavuo V, Airaksinen O, Närhi M (2008) Reproducibility of infrared thermography measurements in healthy individuals. Physiol Meas 29:515. doi:10.1088/0967-3334/29/4/007
Fernandez Cuevas I, Marins JC, Gomez Carmona PM et al (2012) Reliability and reproductibility of skin temperature of overweight subjects by an infrared thermograpy software designed for human beings. Thermol Int 22:130–137
Fournet D, Redortier B, Havenith G (2012) A method for whole-body skin temperature mapping in humans. Thermol Int 22:157–159
Varajão J, Cunha M, Bjørn-Andersen N et al (2014) Segmentation algorithms for thermal images. Procedia Technol 16:1560–1569. doi:10.1016/j.protcy.2014.10.178
Steketee J (1973) Spectral emissivity of skin and pericardium. Phys Med Biol 18:686
Kellogg DL, Pérgola P (2000) Skin responses to exercise and training. In: Garrett WE, Kirkendall DT (eds) Exercise and sport science. Lippincott-Raven Publishers, Philadelphia, pp 239–250
Charkoudian N (2003) Skin blood flow in adult human thermoregulation: how it works, when it does not, and why. Mayo Clin Proc 78:603–612. doi:10.4065/78.5.603
Wallin BG (1990) Neural control of human skin blood flow. J Auton Nerv Syst 30(Suppl):S185–190
Blatteis CM (1998) Physiology and pathophysiology of temperature regulation. World Scientific, Singapore
Wilmore JH, Costill DL, Kenney WL (2008) Physiology of sport and exercise. Human Kinetics
Incropera FP (1999) Introduction to heat transfer: with brief fluid. Wiley, New York
Anbar M (1987) Computerized thermography. Int J Technol Assess Health Care 3:613–621
Al-Nakhli HH, Petrofsky JS, Laymon MS, Berk LS (2012) The use of thermal infra-red imaging to detect delayed onset muscle soreness. J Vis Exp. doi:10.3791/3551
Hildebrandt C, Zeilberger K, Ring EFJ, Raschner C (2012) The application of medical infrared thermography in sports medicine. Ultrasound 10:2
Zaproudina N, Ming Z, Hänninen OO (2006) Plantar infrared thermography measurements and low back pain intensity. J Manipulative Physiol Ther 29:219–223
Vardasca R (2008) Symmetry of temperature distribution in the upper and lower extremities. Thermol Int 18:154–155
Vardasca R, Ring F, Plassmann P, Jones C (2012) Thermal symmetry of the upper and lower extremities in healthy subjects. Thermol Int 22:53–60
Pichot C (2001) Aplicación de la termografía en el dolor lumbar crónico. Rev Soc Esp Dolor 8:43–47
Feldman F, Nickoloff EL (1984) Normal thermographic standards for the cervical spine and upper extremities. Skeletal Radiol 12:235–249. doi:10.1007/BF00349505
Garagiola U, Giani E (1990) Use of telethermography in the management of sports injuries. Sports Med Auckl NZ 10:267–272
de Weerd L, Mercer JB, Weum S (2011) Dynamic infrared thermography. Clin Plast Surg 38:277–292. doi:10.1016/j.cps.2011.03.013
Akimov EB, Son’kin VD (2011) Skin temperature and lactate threshold during muscle work in athletes. Hum Physiol 37:621–628
Chudecka M, Lubkowska A (2010) Temperature changes of selected body’s surfaces of handball players in the course of training estimated by thermovision, and the study of the impact of physiological and morphological factors on the skin temperature. J Therm Biol 35:379–385
Fernández-Cuevas I, Sillero-Quintana M, Garcia-Concepcion MA et al (2014) Monitoring skin thermal response to training with infrared thermography. New Stud Athl 29:57–71
Abate M, Di Carlo L, Di Romualdo S et al (2009) Postural adjustment in experimental leg length difference evaluated by means of thermal infrared imaging. Physiol Meas 31:35
Koprowski R (2015) Automatic analysis of the trunk thermal images from healthy subjects and patients with faulty posture. Comput Biol Med 62:110–118. doi:10.1016/j.compbiomed.2015.04.017
Abate M, Di Carlo L, Di Donato L et al (2013) Comparison of cutaneous termic response to a standardised warm up in trained and untrained individuals. J Sports Med Phys Fitness 53:209–215
Formenti D, Ludwig N, Gargano M et al (2013) Thermal imaging of exercise-associated skin temperature changes in trained and untrained female subjects. Ann Biomed Eng 41:863–871. doi:10.1007/s10439-012-0718-x
Priego Quesada JI, Carpes FP, Bini RR et al (2015) Relationship between skin temperature and muscle activation during incremental cycle exercise. J Therm Biol 48:28–35. doi:10.1016/j.jtherbio.2014.12.005
Sillero Quintana M, Conde Pascual E, Gómez Carmona PM et al (2012) Effect of yoga and swimming on body temperature of pregnant women. Thermol Int 22:143–149
Hadžić V, Širok B, Malneršič A, Čoh M, Can infrared thermography be used to monitor fatigue during exercise? A case study. J Sport Health Sci. doi:10.1016/j.jshs.2015.08.002
Sillero-Quintana M, Fernández-Jaén T, Fernández-Cuevas I et al (2015) Infrared thermography as a support tool for screening and early diagnosis in emergencies. J Med Imaging Health Inform 5:1223–1228
Bertucci W, Arfaoui A, Janson L, Polidori G (2013) Relationship between the gross efficiency and muscular skin temperature of lower limb in cycling: a preliminary study. Comput Methods Biomech Biomed Engin 16(Suppl 1):114–115. doi:10.1080/10255842.2013.815902
Lewis GF, Gatto RG, Porges SW (2011) A novel method for extracting respiration rate and relative tidal volume from infrared thermography. Psychophysiology 48:877–887. doi:10.1111/j.1469-8986.2010.01167.x
Dotti F, Ferri A, Moncalero M, Colonna M (2016) Thermo-physiological comfort of soft-shell back protectors under controlled environmental conditions. Appl Ergon 56:144–152. doi:10.1016/j.apergo.2016.04.002
Fournet D, Redortier B, Havenith G (2015) Can body-mapped garments improve thermal comfort for sport in the cold? Extreme Physiol Med 4:A74
Fournet D, Ross L, Voelcker T et al (2013) Body mapping of thermoregulatory and perceptual responses of males and females running in the cold. J Therm Biol 38:339–344. doi:10.1016/j.jtherbio.2013.04.005
Salces JN, Quintana MS (2012) Epidemiología de las lesiones en el fútbol profesional español en la temporada 2008–2009. Arch Med Deporte 750–766
Ekstrand J, Hägglund M, Waldén M (2011) Epidemiology of muscle injuries in professional football (soccer). Am J Sports Med 39:1226–1232
Noya Salces J, Gómez-Carmona PM, Gracia-Marco L et al (2014) Epidemiology of injuries in first division Spanish football. J Sports Sci 32:1263–1270
Bouzas Marins JC, de Andrade Fernandes A, Gomes Moreira D et al (2014) Thermographic profile of soccer players’ lower limbs. Rev Andal Med Deporte 7:1–6. doi:10.1016/S1888-7546(14)70053-x
Buchheit M, Laursen PB (2013) High-intensity interval training, solutions to the programming puzzle: part I: cardiopulmonary emphasis. Sports Med Auckl NZ 43:313–338. doi:10.1007/s40279-013-0029-x
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
Fernández-Cuevas, I., Arnáiz Lastras, J., Escamilla Galindo, V., Gómez Carmona, P. (2017). Infrared Thermography for the Detection of Injury in Sports Medicine. In: Priego Quesada, J. (eds) Application of Infrared Thermography in Sports Science. Biological and Medical Physics, Biomedical Engineering. Springer, Cham. https://doi.org/10.1007/978-3-319-47410-6_4
Download citation
DOI: https://doi.org/10.1007/978-3-319-47410-6_4
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-47409-0
Online ISBN: 978-3-319-47410-6
eBook Packages: Physics and AstronomyPhysics and Astronomy (R0)