Abstract
The article describes the process of the development of an app to support people in lifelong secondary prevention, e.g. after a heart attack or with chronic diseases. The goal of this app-guide, called the HealthNavigator, is to coach people walking on leisure paths through guidance, motivation, and better understanding of physical abilities (body awareness). There were three development cycles, each one followed by a demonstrator test with health professionals and patients. The outcomes of these tests were taken into account for the following development cycle. Focus was placed on how to motivate people to exercise regularly and in a healthy manner. The evaluations showed that HealthNavigator was found to be usable tool for teaching body awareness and making users feel safe, while motivating them to take walks in the open air.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Regular physical activity has nothing but positive effects on the human body. There is one main premise for this: the activity must be exercised individually within an optimal range and at optimal intensity in order to avoid overexertion, injury, and physical problems, such as circulatory or coronary disorders. A moderate aerobic activity of 30 min per day reduces the risk of coronary heart disease [1], and, carried out regularly, it enhances the subjective quality of life [2]. An ideal endurance activity in a moderate range can be performed through taking walks—hiking, trekking, strolling—which can be done by anyone and anywhere in the open air. Controlling intensity while performing endurance activity in an outdoor setting can be difficult, especially for people with little or no experience in this. Control requires objective parameters, such as heart rate, and subjective parameters, such as self-assessment in order for the walker to be coached regarding individual optimal walking intensity. To this end, an app-guide, called HealthNavigator, was developed to coach people during walking on leisure pathways (e.g., streets with sites of historic or cultural interest, paved or unpaved paths in parks, country roads, forest paths). The app provides route guidance, motivation stimulus, and real-time body awareness. The HealthNavigator is an app-guide for people who want to improve their physical condition by hiking outdoors in nature; it can also be used, for example, by persons with cardiovascular diseases, who do not take any medication (e.g. ß-blockers) to regulate heart rate. In that sense, potential users are persons in the phase of lifelong secondary prevention or in the final phase of rehabilitation. Caveat: HealthNavigator is part of a research project, not a medical device in the legal sense.
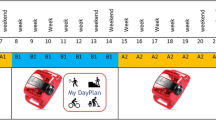
HealthNavigator consists of an app on a smartphone, an app on a smartwatch, and a belt with an integrated ECG. The system should encourage users to optimize their performance and impart confidence in respect to physical capabilities by displaying physical parameters, monitoring self-estimated exertion by the Borg-Scale [3], and providing individual feedback. Due to simultaneous detection of objective and subjective conditions of the user, the HealthNavigator is able to recommend user-tailored load profiles and suggest optimal walking routes. To motivate the user to go for a walk, HealthNavigator provides information on points of interest (such as historical buildings, memorials, and museums in towns or villages), rest areas (such as restaurants or sitting areas with attractive panoramas).
An iterative approach was followed in developing the HealthNavigator, with several cycles building on each other. There were three main iterations, each one consisting of a requirements analysis, system-development, and evaluation. These will be discussed in the sections to follow. Comments from users and professionals helped in adapting the system to achieve steady improvement towards the final demonstration model.
2 Requirements
Although the number of applications and telemedicine systems is rapidly evolving, many of such initiatives do not reach an operational phase. Insufficient technical performance and low usability are considered to be among the major barriers for successful implementation [4]. Involvement of patients and professionals in the requirements analysis and the design process is crucial for adjusting its utilization in the user’s daily routine and for successful implementation. Therefore, for developing the requirements of HealthNavigator, we chose an iterative, user-centered design approach. It considers the user as the basis for the design and involves him/her in the evaluation of design choices [5].
A scenario was developed following the PACT approach (People, Activity, Context and Technology) related to patients using a technology in their daily life within a certain (medical) context. Incorporating the principles of evidence-based medicine into PACT scenario development provides starting points for more effective and efficient design of such applications [6]. We studied the literature documenting state-of-the-art research, and we assessed the user’s medical knowledge and needs by means of PACT tables and expert interviews. By means of open interviews, medical experts were asked about the target users. The developers provided feedback by proposing FICS extensions to the scenario. (FICS stands for Function and events, Interactions and usability issues, Content and structure, Style and aesthetics, related to system use.) The scenario was updated, containing PACT elements combined with FICS elements (Fig. 1).
The HealthNavigator’s user-centered design approach (reproduced with permission from [4])
After elicitation of the requirements in focus groups with medical experts and patients, the functional requirements were prioritized following MoSCoW (Must have, Should have, Could have, Wouldn’t have). Table 1 shows the Must haves (M) and the Should haves (S). Mock-ups were created and evaluated with the patients and specialists. In addition, a field study was performed with the users, to evaluate simple navigation techniques on a smartphone.
3 HealthNavigator
3.1 Concept
The HealthNavigator application combines two main support systems. First, there is health status monitoring, which is realized by measuring heart rate, but also by letting the users reflect their perceived exertion. The information measured by and entered into the system is then used to give users advice for walking faster or slower according to their goals. Second is the navigation system, which includes points of interest. It helps users to navigate on previously defined routes and to adapt the route according to user needs. It also supports navigation back to the starting point (e.g., a healthcare facility) using the shortest route (which may be different from the predefined routes).
While both systems work together, we carefully separated them by using different devices. The navigation system works on the smartphone, since it is not necessary all the time, because walking routes tend to be straight for a longer time, and the smartphone provides a big enough screen with high resolution for getting a clear overview of the map for the route. Health status is constantly monitored. Interaction with the user should be easy, fast, and not distracting. Thus, we decided to use a smartwatch for this interaction.
3.2 Health Status Monitoring
The navigation of the HealthNavigator also focuses on the user’s exertion level. Health status monitoring is supposed to keep the exertion of users within appropriate limits. In the HealthNavigator, this is achieved by measuring heart rate and querying the perceived user exertion. The perceived exertion can be measured using the Borg-RPE-Scale [4], which allows the rating from 6 (no exertion at all) to 20 (maximum exertion). In the beginning, the users have to define their target exertion level. In the HealthNavigator, users were able to choose between four different levels: low, medium, high and very high (see Fig. 2a). Additionally, the fitness level and the age have to be entered by the users.
The HealthNavigator uses the perceived exertion as the main parameter for health status monitoring. The heart rate is used as a supportive parameter. This means that if the system measures exertion different from what the user entered, the perceived exertion is considered to be correct and the system will adapt to that. The goal of this behavior is to cultivate body awareness in the user. We created an algorithm, visualized in Fig. 3.
The algorithm uses the target rating of perceived exertion (RPE) to compute estimated heart rate corridors. The HealthNavigator uses five heart rate corridors: one optimal corridor, two warning corridors, and two alarming corridors. The corridors are estimated based on the user’s the age, the target exertion level, and the maximum heart rate of the user, all of which is estimated by the popular formula 210–age. The HealthNavigator then utilizes the measured heart rate to estimate whether the users are within their desired load limits. If the heart rate is within the estimated optimal heart rate corridor, the HealthNavigator assumes that the user has obtained the desired load and only asks about perceived exertion every ten minutes. If the heart rate lies outside the optimal corridor, the system will shorten this interval. If the deviation is only small (low and/or high corridors), the interval is lowered to three minutes. If the deviation is high (too low and/or too high corridors), the interval is lowered to one minute. This way, the users won’t be asked for perceived exertion too often if it is very likely that they are within their desired limits.
Just as the correlation between the heart rate and the RPE can be high for everyone, since each person reacts differently to physical activity, the interpretation of the RPE levels is also very individual and can differ, too. To address these issues, the algorithm uses the regularly user-entered RPE values to adjust the estimated heart rate corridors, and in conjunction, the interval of user queries for the RPE. This calibration is made if the actual RPE that the user entered equals the target RPE that the user entered at the beginning. In this case, the user has obviously reached his/her defined target intensity—which is the overall goal. If the estimated heart rate corridors do not reflect this, they must be adjusted. The algorithm does this slowly in order to avoid too great adjustments caused by temporal effects, such as a briefly elevated heart rate not caused by physical activity or by short elevations of the exertion level due to geography (for instance, slopes). We chose to adjust the estimated heart rate corridors by a maximum of 5 beats per minute per adjustment. By way of example: let the target be RPE 12 and the estimated heart rate corridor between 110 and 130 beats per minute. If the heart rate is 100 and the user enters 12 as the current RPE, the algorithm will adjust the estimated heart rate corridor to 105 and 125 beats per minute. This will not change the query interval the first time; but the second time, the heart rate corridor will be reduced to 100 and 120, respectively, and match the actual heart rate. The navigation of the HealthNavigator also focuses on the exertion of the user. When the desired exertion level is selected (Fig. 2a), the user can also select how exhausting the path for the hike should be.
The requirements analysis showed that patients in cardiac rehabilitation consider it important to be able to monitor their heart rate. Since entering the perceived exertion is not necessary all the time, the smart watch shows feedback about the heart rate when no user input is required. Figure 2b and c show both smartwatch views used in the HealthNavigator.
Another important element of the requirements analysis is that the system can provide feedback about the user’s optimal performance. Therefore, we have developed a decision support system so the HealthNavigator can provide feedback to help the user achieve the desired exertion level: sending the user messages about walking pace (for example, “Decrease your pace,” when, based on the system input, exertion becomes too high). This feature of HealthNavigator is under development and has not yet been fully evaluated.
3.3 Touristic Navigation
In addition to selecting the desired exertion level (Fig. 2), the user can also select how exhausting the path for the walk should be. The HealthNavigator then locates them and downloads available routes from Open Street Maps. These routes were entered beforehand by experts and contain a necessary rating of the route and possible shortcuts in case users feel over-exerted during the hike. The system then shows available paths to the user and colors them according to the previously entered desired exertion level. Routes that fully meet this requirement are marked green, and routes that are too easy are colored yellow. Routes that are too difficult are colored red and display an additional warning symbol to alert the user against choosing a route that is too hard (Fig. 4).
After choosing a route, the HealthNavigator displays the navigation view (Fig. 5). It consists of a self-rendered map based on Open Street Map data. This data is downloaded as soon as the route is known. During the walk, this allows the HealthNavigator to always guide the user back to the starting point through the shortest path, even if the mobile data connection fails. The navigation itself is realized using a highlighted blue path displayed on the map. The user can zoom in and out to get a better overview of where the path leads. A dialog for showing the expected amount of time to arrival can be opened and closed by the user.
Every route has a predefined shortcut. When it is reached, the HealthNavigator opens a dialog informing the user about both possible ways to continue. The user can then decide whether he/she would like to walk the original route as planned or take the shortcut (due to overexertion, time planning, or other reasons). The user can always activate the navigation back to the starting point by choosing this option from the application menu.
4 Evaluation
Evaluations have been conducted annually, which allows for incorporating the respective partial results into each iteration of the HealthNavigator. Similarly, the usability of the HealthNavigator has been evaluated by various user tests in several separate studies. The design of the HealthNavigator was set based on these results. Final evaluation of the HealthNavigator was performed under real conditions, such as the handling and using of the device by the test participants. A standardized protocol was used at two testing stagess, consisting of a pre-interview, a field study, and a post-interview.
Participating in the study was a total of 12 subjects (5 in group 1 and 7 in group 2),with a mean age of 56.3 ± 8.7 years (group 1: 48.6 ± 6.9 years; group 2: 61.9 ± 4.7 years) with a range of 42 years to 68 years (group 1: 42–57 years; group 2: 56–68 years). Group 1 consisted of healthy people (four of whom were healthcare professionals) and group 2 consisted of persons undergoing physiotherapy. The subgroups differed significantly in age.
HealthNavigator received a good usability rating (SUS score: 71.0 ± 22.3) based on [7, p. 118]. The majority of the participants (83.3 %) believed that their body awareness will increase by using the HealthNavigator system frequently (group 1: 80 %; group 2: 85.7 %). Healthcare professionals explained that this is the case because dyspnea (i.e., difficult breathing) and other symptoms could be diagnosed. The user will become more aware of his/her body condition and learn about his/her capacity. Nine of all participants (75 %) felt safe and confident with the HealthNavigator system (group 1: 60 %; group 2: 85.7 %); and six participants (50 %) thought that the HealthNavigator system can remove anxiety over exercising (group 1: 60 %; group 2: 42.9 %). Four of the seven patients voiced their intention to use HealthNavigator once it becomes available.
The health status monitoring (entering the Borg) was rated the most important current feature of the HealthNavigator, together with the feedback provided. This may be due to the fact that the HealthNavigator is a device with new features, in contrast to the sport navigation devices currently on the market.
The results regarding the features of the HealthNavigator show that the (heart rate) feedback, the tourist information, and the selectable routes are the main motivational functions. The results show that the users are intrinsically motivated to use HealthNavigator to improve their physical condition, to explore the surroundings, and to learn something about the surroundings, while they find the opinions of others regarding the device of less importance.
5 Discussion
With the HealthNavigator, a new method was implemented to help patients regarding lifelong secondary prevention and for healthy people who want to increase their physical condition. The HealthNavigator combines tourist navigation, health status monitoring, and feedback in order to increase body awareness and to coach users in walking on scenic and tourist routes. Evaluations show that the HealthNavigator is user friendly, can teach body awareness, and makes users feel safe, while motivating them to walk and hike outdoors.
The need for people in general and especially for patients to maintain an active and healthy lifestyle was the original impetus behind the project and was closely related to experiences of project partners with patients in current healthcare. The result—the combination of the measured exertion and perceived exertion—is from a technical and medical point of view, new and opens broad prospects for follow up.
We designed a technical system that the target groups find usable and understandable. To achieve ease of usability, we ourselves designed the routing, which allowed us to take the individual preferences of older people into account. There are, of course, improvements to be made for further development of the HealthNavigator. For example, to explain the system to a larger audience, a manual is needed. Also more effort needs to be put into the user interface and the integration of sensors in order to obtain better view of the patient while walking.
With the automatic determination of heart rate corridors and the algorithmic verification of heart rate matching the rating of perceived exertion (RPE), we offer the user a unique possibility to control him- or herself and to learn what his or her individual thresholds are. Very interesting would be to further develop the feedback of the HealthNavigator system for increased guidance regarding navigation and health status monitoring. The decision support that provides feedback and coaches the user to acquire the best walking pace is largely developed, but should be precisely evaluated regarding safety, effects on walking behavior, and motivational influence. In respect to the navigation, currently the user receives a message when an alternative route is available; a future system should automatically coach the user to alternative routes when the input data requires doing so. In light of the recent unobtrusive sensors that are becoming more and more available, together with available context information, the system could be extended through more input data (e.g., physical activity, weather), to make the automatic routing and decision support feedback as accurate and tailored to the user as possible.
The testing with two groups (healthcare professionals and potential users in secondary prevention) delivered two different viewpoints: one from the actual user and another from the persons who are likely to recommend and explain the system to the user. Both views are important when you think in terms of market introduction and operational conditions. We received valuable feedback from professionals and patients, who were mainly positive. Physiotherapists from the Netherlands were willing to test the system and prompted its usefulness for their daily work, as well as patients and practitioners from Germany, who were assured that the HealthNavigator would be of great benefit. However, first we need to perform larger scale trials in order to investigate the effects on the walking behavior and quality of life of the users, and the added value for daily practice. And in terms of market introduction, a closer look at the needs of practitioners and general rehabilitation processes must be taken so that HealthNavigator can be incorporated into regular (care) programs.
References
Balady, G., et al.: Core components of cardiac rehabilitation/secondary preventionprograms: 2007 update. Circulation 115(20v), 2675–2682 (2007)
Bjarnason-Wehrens, B., et al.: Leitlinie körperliche Aktivität zur Sekundärprävention und Therapie kardiovaskulärer Erkrankungen (2009)
Borg, G.: Anstrengungsempfinden und körperliche Aktivität. Deutsches Ärzteblatt 101(15), 1016–1021 (2004)
Broens, T.H.F., et al.: Determinants of successful telemedicine implementations: a literature study. J. Telemedicine Telecare 13(6), 303–309 (2007)
op den Akker, et al.: Development and evaluation of a sensor-based system for remote monitoring and treatment of chronic diseases—the continuous care & coaching platform. In: Proceedings of the 6th International Symposium on eHealth Services and Technologies, EHST 2012, 3–4 July 2012, Geneva, Switzerland. pp. 19–27 (2012)
Huis in’t Veld R.M.H.A., et al.: A scenario guideline for designing new teletreatments: a multidisciplinary approach. J. Telemedicine Telecare 16(6), 302–307 (2010)
Bangor, A., Kortum, P.T., Miller, J.T.: Determining what individual SUS scores mean: Adding an adjective rating scale. J. Usability Stud. 4(3), 114–123 (2009)
Acknowledgments
HealthNavigator is a research project funded by the INTERREG IV A Programme D/NL.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Heuten, W. et al. (2017). Coaching of Body Awareness Through an App-Guide: The HealthNavigator. In: Nadin, M. (eds) Anticipation and Medicine. Springer, Cham. https://doi.org/10.1007/978-3-319-45142-8_11
Download citation
DOI: https://doi.org/10.1007/978-3-319-45142-8_11
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-45140-4
Online ISBN: 978-3-319-45142-8
eBook Packages: EngineeringEngineering (R0)