Abstract
Functional ischemic mitral regurgitation is most commonly repaired by mitral annuloplasty. Important surgical principles must be followed when repairing ischaemic mitral valves by annuloplasty to ensure a durable long term repair. When these principles are followed, a durable, long term repair is achievable. Recent randomized controlled trials have given insights into the groups of patients who would benefit most from concomitant mitral annuloplasty and coronary artery bypass graft surgery. Risk factors for recurrent mitral regurgitation following mitral annuloplasty have been identified; these patients may require additional adjunctive repair procedures or a mitral valve replacement.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Functional ischemic mitral regurgitation
- Mitral annuloplasty
- Mitral valve repair
- Coronary artery bypass graft surgery
- Functional capacity
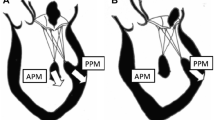
Principles of Treatment
The aim of mitral valve repair for mitral regurgitation is to restore the surface of coaptation of the two mitral valve leaflets, thereby, making the valve competent. In functional ischaemic mitral regurgitation, the mitral valve leaflets are normal in structure. The normal mitral valve leaflets are pulled apart, either as a result of a dilated mitral annulus or left ventricle, or due to tethering consequent upon poor contraction of the left ventricle in the region where the papillary muscles attach [1–3]. The surface of coaptation can be restored by reducing the size of the mitral annulus, especially in the septolateral dimension. This can be achieved by implanting a ring onto the mitral annulus (mitral annuloplasty) (Fig. 7.1). The annuloplasty ring is sized by measurement of the inter-trigonal distance at the anterior mitral annulus and also the height of the anterior mitral valve leaflet (Fig. 7.2). Typically, the ring is downsized, i.e., a ring two sizes smaller than that measured is used [5, 6]. Such downsizing reduces the septolateral dilatation of the mitral annulus and, hence, increases leaflet coaptation. Newer rings have been designed specifically for functional ischaemic mitral regurgitation, which reduce the septolateral dimension, particularly in the medial part of the posterior annulus and do not require downsizing [7]. A complete rigid or semi-rigid ring is generally recommended in functional ischaemic mitral regurgitation as a higher incidence of recurrent mitral regurgitation has been reported with the use of flexible rings or bands [5, 6].
Mitral annuloplasty. The size and shape of the annuloplasty ring restores normal mitral annular size and geometry resulting in improved mitral leaflet coaptation and competence (Adapted from Chan et al. [4]. With permission from Elsevier)
Sizing the annuloplasty ring. The annuloplasty ring is sized by measurement of the distance between the fibrous trigones and the size of the anterior mitral valve leaflet (Adapted from Chan et al. [4]. With permission from Elsevier)
Good long-term results following undersized mitral annuloplasty for functional ischaemic mitral regurgitation have been associated with: (i) complete coronary artery revascularisation, (ii) use of a complete rigid or semi-rigid ring, (iii) achieving a surface of mitral leaflet coaptation of 8 mm or greater, and (iii) leaving minimal residual mitral regurgitation [5, 8]. Braun et al., for example, reported that at 5 years following mitral annuloplasty combined with CABG in patients with functional ischaemic mitral regurgitation, mean mitral regurgitation grade improved from 3.1 ± 0.6 to 0.8 ± 0.7 (p < 0.001) [5, 9]. 84 % had less than moderate mitral regurgitation, 14.6 % had moderate mitral regurgitation, and 1.4 % had moderate-severe mitral regurgitation at 5 years. The mitral leaflet coaptation length was maintained at 8 mm.
However, significant recurrence of mitral regurgitation has been reported in several studies following mitral annuloplasty [10–16]. This has been associated with the following factors:
-
(i)
Flexible rings or bands [6, 11, 13–17]. The mitral annulus is dilated both at the anterior annulus and the posterior annulus in functional ischaemic mitral regurgitation with the greatest increase being in the septolateral diameter [1, 3, 18, 19]. The use of a complete rigid or semi-rigid ring, rather than a flexible ring or band, may, therefore, be important to restore mitral annular size and geometry. Moreover, continued left ventricular remodelling has been associated with recurrent mitral regurgitation and the use of a complete rigid or semi-rigid ring may be important to overcome this [12, 20].
-
(ii)
Failure to undersize [11–15]. The use of an undersized ring has been recommended to decrease the septolateral dilatation present in functional ischaemic mitral regurgitation and, hence, increase the surface of mitral leaflet coaptation. Studies which have reported good results in functional ischaemic mitral regurgitation have generally used this approach [5, 8].
-
(iii)
Failure to achieve an adequate surface of mitral leaflet coaptation. It has been reported that a mitral leaflet coaptation length of at least 8 mm is important to ensure long-term durability of the repair [8, 9].
-
(iv)
Incomplete coronary artery revascularisation. The primary cause of functional ischaemic mitral regurgitation is left ventricular dysfunction and dilatation secondary to myocardial ischemia or infarction. Complete coronary artery revascularisation, particularly of viable ischaemic left ventricular segments is, therefore, important to restore left ventricular contractility [21]. Progression of mitral regurgitation has been reported following incomplete coronary artery revascularisation [22].
-
(v)
Leaving greater than trace mitral regurgitation [13, 23]. The presence of greater than trace mitral regurgitation at the end of the operation may mean greater severity of the mitral regurgitation during physical activity and, hence, continued left ventricular volume overload and impairment of left ventricular reverse remodelling [24, 25].
-
(vi)
Excessive dilatation of the left ventricle. Greater recurrence of mitral regurgitation has been reported with significantly dilated left ventricles (e.g., left ventricular end systolic diameter greater than 51 mm or left ventricular end diastolic diameter greater than 65 mm) [5, 9, 26]. In such patients, it has been suggested that undersized mitral annuloplasty should be combined with additional surgical procedures on the left ventricle such as left ventricular restoration surgery [27], left ventricular infarct plication [28] or external left ventricular constraining devices such as the Coapsys [29].
-
(vii)
Excessive leaflet tethering. There are some reports that excessive leaflet tethering is a risk factor for the development of significant recurrent mitral regurgitation (tethering distance greater than 1.1 cm, tethering area greater than 1.6 cm2) [30, 31]. Such cases may benefit from additional surgical adjuncts to mitral annuloplasty such as papillary muscle relocation [32], papillary muscle sling [33], and secondary chordal cutting [34]. These techniques are discussed in separate chapters. Long-term results of these techniques are currently awaited.
Surgical Operative Technique
Intra-operative trans-oesophageal echocardiographic assessment of the mitral valve is essential to confirm the findings of the pre-operative transthoracic echocardiography. This is usually performed after the induction of general anaesthesia and before the commencement of cardiopulmonary bypass. It is important to ensure that there is no associated structural valve lesions as other etiologies of mitral regurgitation can co-exist with functional ischaemic mitral regurgitation.
As in all mitral valve surgery, optimal setup is very important in ischaemic mitral valve surgery to maximise exposure and visualisation of the mitral valve. This is particularly so in functional ischaemic mitral regurgitation as the left atrium is typically not very enlarged, unlike in degenerative or rheumatic mitral regurgitation. To maximize exposure of the mitral valve, the pericardium should be lifted up on the right side and left free on the left side. This has the effect of rotating the heart upwards and towards the left, bringing the mitral valve into view when the left atrium is opened. A Cosgrove mitral retractor is used. Further visualisation of the mitral valve is enabled by incising the pericardium on top of the superior vena cava (SVC) and perpendicular to it; this allows retraction of the heart upwards when the retractors are placed [35].
The aorta, SVC and IVC are cannulated. An antegrade cardioplegia and a retrograde cardioplegia cannula are inserted. Tapes may be passed around the SVC and IVC. Cardiopulmonary bypass is commenced. A cross clamp is applied. Cardioplegia is delivered antegradely to start with and then every 20 min retrogradely while suction is applied to the aortic root. The venous cannulation lines are placed over on the left side supported by the mitral retractor.
The mitral valve can be approached either through a left atriotomy or a right atriotomy via a trans-septal approach. With a left atriotomy approach, the fat within Sondergaard’s grove is dissected with diathermy so as to approach the left atrium more medially and nearer to the mitral valve. Alternatively, an incision is made midway between the inter-atrial septum and the origin of the right superior pulmonary vein, and extended inferiorly along the left atrium towards the left inferior pulmonary vein, ending a few mm inferior to it. The incision is then extended superiorly a few mm beyond the end of the right superior pulmonary vein onto the roof of the left atrium. One or two small mitral retractors are then inserted and lifted up together and towards the left side, opening up the left atrium and exposing the mitral valve. To improve visualisation of the mitral valve further, the incision can be extended superiorly and medially, underneath the SVC and onto the roof of the left atrium [35].
A systematic analysis of the mitral valve is performed. The mitral valve is first inspected. Note is made of any excessive leaflet tissue, leaflet perforations, ruptured chordae or ruptured papillary muscles. The lesion is then determined using a pair of nerve hooks. A reference point, such as P1 or the commissures, is chosen. Each part of the mitral valve leaflet is lifted up in turn and compared to the reference point to determine if there is leaflet prolapse or restriction. Leaflet restriction in functional ischaemic mitral regurgitation is typically difficult to assess in the arrested flaccid heart and is often not apparent. It is important to ensure that there are no associated lesions as these would need to be addressed.
In the absence of any other lesions, an undersized mitral annuloplasty is performed. The mitral annulus is first sized by pulling on the marginal chordae supporting the anterior leaflet with two nerve hooks or a right angled clamp. The ring sizer is then placed over the unfurled anterior leaflet and a sizer is chosen which matches the surface area of the anterior leaflet. If the leaflet restriction is asymmetric and mainly in the P3 area as identified by echocardiography, the Carpentier-McCarthy-Adams IMR ETlogix Annuloplasty Ring (Edwards LifeSciences) is a suitable ring. A ring of the same size as the sizer is used as this ring is already downsized in the P2-P3 area. However, if the leaflet restriction is more symmetrical, as in a more global dilatation of the LV, a symmetrical complete rigid or semi-rigid ring, such as the Carpentier-Edwards Physio or Classic Rings (Edwards LifeSciences), or equivalent, are used, downsized by 2 sizes. For example, if the annulus is sized as 30 mm, a 26 mm ring is used. Under-sizing of the annuloplasty ring compensates for the loss of mitral annular function in functional ischaemic mitral regurgitation as discussed in Chap. 2 and increases the coaptation surface area between the anterior and posterior leaflets.
Interrupted non-pledgeted 2/0 ethibond horizontal mattress sutures are placed around the mitral annulus. Unlike in degenerative and rheumatic mitral regurgitation where under-sizing of the annuloplasty ring is not used, the use of an undersized annuloplasty ring in functional ischaemic mitral regurgitation results in increased tension in the annuloplasty ring and care must therefore be taken to ensure that adequate sutures are placed around the mitral annulus, and which are of sufficient length and depth, to avoid ring dehiscence. The sutures can be overlapped if necessary to provide added strength. If the IMR ring is used, this is broader in the P3 region to permit a double row of sutures to be placed. However, care must be taken when using this ring to ensure that the annuloplasty suture positioned at the middle of the P2 scallop is placed in the middle of this ring posteriorly so as not to distort the mitral annulus.
The competency of the mitral valve is tested by injecting water or saline through the valve into the left ventricle. The mitral valve should be able to hold a reasonable pressure of water with no more than trace mitral regurgitation. The final test of the repair is performed using transoesophageal echocardiography when the patient is off cardiopulmonary bypass with a systolic blood pressure above 100 mmHg. There should be no more than trace mitral regurgitation. The left atrium is closed by a single continuous layer of 4/0 polypropylene starting at either end of the incision.
Results of Treatment
Hospital Mortality
The hospital mortality of patients with functional ischaemic mitral regurgitation undergoing mitral annuloplasty combined with CABG in recent series varies from 1.5 to 21 % and may be related to differences in the baseline characteristics of the patients [5, 7, 8, 10, 11, 13, 15, 16, 20, 23, 36–41]. In one study which reported an operative mortality of 21 %, 93 % of patients either had a myocardial infarction within 2 weeks or had unstable angina requiring intravenous heparin and nitrates [10]. Higher operative mortality is also reported for patients with a poor left ventricular ejection fraction (less than 30–40 %) [23, 36–38, 40]. The hospital mortality in the 3 most recent randomised controlled trials of functional ischemic mitral regurgitation was less than 3 % [41–43].
Left Ventricular Reverse Remodelling
Observational studies have long reported significant left ventricular reverse remodelling, improvement in cardiac function and NYHA functional class following concomitant CABG plus mitral valve annuloplasty in functional ischaemic mitral regurgitation. However, most of these studies did not have a control group of patients who only had CABG and so it was not possible to determine how much of these improvements could be attributed to the mitral valve repair and how much was a result of successful coronary artery revascularisation. These findings have now been confirmed in several randomised controlled trials which have recently reported (Table 7.1) [41–43].
Mean regression of left ventricular volumes and dimensions by up to 28 % have been reported 1–2 years following CABG combined with mitral annuloplasty, provided a durable mitral valve repair is achieved [8, 36, 41, 42]. The reduction in left ventricular volumes appears to be dependent on the success of eliminating the mitral regurgitation. In the Randomised Ischemic Mitral Evaluation (RIME) Trial, left ventricular end systolic volumes decreased by 28 % at 1 year following CABG plus mitral annuloplasty compared to a reduction in 6 % in those undergoing isolated CABG [41]. Of note, the freedom from moderate or more mitral regurgitation at 1 year following CABG plus mitral annuloplasty in this study was 96 % compared to 50 % in those undergoing isolated CABG. Greater reductions in left ventricular dimensions following combined CABG plus mitral valve annuloplasty compared to isolated CABG were also reported in an Italian randomised controlled trial [44]. In the Cardiothoracic Surgical Network (CTSN) moderate ischemic mitral regurgitation trial, left ventricular volumes decreased by 16 % at 1 year following CABG plus mitral annuloplasty compared to 17 % in those undergoing isolated CABG. The freedom from moderate or more mitral regurgitation following combined CABG plus mitral annuloplasty in this trial was 89 % compared to 70 % in those undergoing isolated CABG [42]. In the CTSN severe ischemic mitral regurgitation trial, left ventricular volumes decreased by only 11 % at 1 year following CABG plus mitral annuloplasty. However, the freedom from moderate or more mitral regurgitation in this trial was only 67 % [43]. Of note, in patients who had no recurrent mitral regurgitation at 1 year in this study, left ventricular volumes decreased by 22 %, a result similar to that reported in the RIME Trial [41, 43]. Similar results at 2 years were recently reported by the CTSN severe ischemic mitral regurgitation trial. Left ventricular volumes decreased by 15 % 2 years after CABG plus mitral valve repair; the freedom from moderate or more mitral regurgitation was only 41 %. However, in those with no recurrent mitral regurgitation, left ventricular volumes decreased by 31 % at 2 years, as compared to an increase of 2 % in those with recurrent mitral regurgitation [45]. A consistent finding in these randomised studies is that significant left ventricular reverse remodelling can be expected if a successful and durable mitral valve repair is achieved at the time of CABG (Table 7.1). However, left ventricular reverse remodelling will not occur if recurrent or persistent mitral regurgitation is present.
The extent of left ventricular reverse remodelling is also dependent on the baseline size of the left ventricle. Bax et al., for example, reported that left ventricular end systolic diameters decreased from 51 ± 10 mm to 43 ± 12 mm (p < 0.001) 2 years after CABG combined with mitral annuloplasty [8]. Regression of left ventricular size was greater in those in whom the left ventricle was less dilated pre-operatively. Braun et al. reported that a left ventricular end systolic diameter less than 51 mm and a left ventricular end diastolic diameter less than 65 mm were predictive of increased reverse remodelling [5].
Improvement in cardiac function by up to 10 % has also been reported following successful mitral annuloplasty combined with CABG. Bonacchi et al. reported an improvement in cardiac index from 2.2 ± 0.4 l/min/m2 to 2.5 ± 0.3 l/min/m2 (p = 0.001) following mitral annuloplasty combined with CABG [40].
Functional Status
An improvement in functional status can be expected if a successful and durable mitral valve repair has been achieved at the time of CABG. In the RIME Trial, peak oxygen consumption, an objective marker of functional capacity, improved by 22 % in the CABG plus mitral annuloplasty group compared to a 5 % improvement in the isolated CABG group [41]. The median NYHA class was class I in the combined CABG plus mitral annuloplasty group compared to class II in the isolated CABG group (p = 0.03). Similar results were reported from a randomised trial from Italy where patients who had combined CABG plus mitral annuloplasty had a better NYHA functional class at 3 years [44]. A significant improvement in NYHA class following combined CABG plus mitral annuloplasty was also reported in the CTSN moderate ischemic mitral regurgitation trial although in this trial, a similar improvement was also reported in the isolated CABG group [42]. Similarly, the CTSN severe ischemic mitral regurgitation trial reported significant improvement in NYHA class and quality of life scores 2 years following either mitral valve repair or mitral valve replacement, with the greatest improvement reported in those who did not have recurrent mitral regurgitation [45].
A recent randomised controlled trial from a single Italian centre of 102 patients with moderate functional ischaemic mitral regurgitation who were randomised to either CABG only or concomitant CABG plus mitral annuloplasty reported no difference in survival between the two groups at 3 years (88.8 % ± 3.2 % versus 93.7 % ± 3.1 %) although patients who had concomitant CABG plus mitral valve annuloplasty had a better NYHA functional class (1.6 ± 0.6 versus 0.6 ± 0.8, p < 0.001) and better left ventricular reverse remodelling (LVESD 42 ± 8 mm versus 37 ± 5 mm, p < 0.01) [44].
These findings have also been reported in earlier observational studies with several studies reporting that the majority of patients in NYHA class III and IV pre-operatively were in NYHA class I and II at 1–5 years [8, 16, 20, 36]. Bax et al., for example, reported that NYHA class improved from 3.4 ± 0.8 to 1.3 ± 0.4 (p < 0.01) 2 years after CABG plus mitral annuloplasty with all patients in NYHA class I or II [8].
Survival
In observational studies, the actuarial survival for patients with functional ischaemic mitral regurgitation undergoing mitral annuloplasty combined with CABG is 75–86 % and 60–88 % at 2 years and 5 years respectively. This may be related to the baseline characteristics of the patients and the successful treatment of the mitral regurgitation [5, 8, 16, 20, 37, 40]. The recent CTSN severe ischaemic mitral regurgitation trial reported a 2-year survival of 81 % in the mitral valve repair group and 76.8 % in the mitral valve replacement group [45]. 1-year survival in patients with moderate functional ischaemic mitral regurgitation receiving combined CABG plus mitral valve annuloplasty was 95 % in the RIME Trial and 93 % in the CTSN moderate ischaemic mitral regurgitation trial; 3 year survival was 94 % in an Italian randomised controlled trial [44]. Following isolated CABG in patients with moderate functional ischemic mitral regurgitation, 1-year survival was 94 % in the RIME Trial and 93 % in the CTSN moderate ischaemic mitral regurgitation trial; 3-year survival was 89 % in an Italian randomised trial [41, 42, 44]. It must be emphasised that none of the randomised trials are adequately powered to detect differences in survival in the different randomised groups.
Despite the worse survival of patients with functional ischaemic mitral regurgitation undergoing isolated CABG, it is unclear if performing mitral annuloplasty in addition to CABG improves survival. Observational studies in fact suggest that although mitral valve annuloplasty combined with CABG may reduce the severity of functional ischaemic mitral regurgitation, survival may not actually be improved [46, 47]. Mihaljevic, et al., for example, reported a propensity matched study of 390 patients with severe functional ischaemic mitral regurgitation, 100 of whom underwent CABG only and 290 underwent concomitant CABG plus mitral valve annuloplasty [47]. At a mean follow-up of 5 years, no difference was observed between the two groups in survival (75 % versus 74 %) or NYHA functional class (25 % in NYHA class III/IV versus 23 %). Patients who had concomitant CABG plus mitral valve annuloplasty had lesser degrees of mitral regurgitation at 1 year compared to those who had CABG only (12 % 3–4 + MR versus 48 %, p < 0.001). Complete echocardiographic data was, however, not available at late follow-up but the authors estimate up to 20 % of those who had concomitant CABG plus mitral annuloplasty may have developed significant mitral regurgitation compared to about 50 % in those who underwent CABG only. A meta-analysis of nine non-randomized observational studies involving 2479 patients with severe functional ischaemic mitral regurgitation who underwent either CABG alone or concomitant CABG plus mitral valve annuloplasty reported no difference in late survival between the groups although patients who underwent concomitant CABG plus mitral valve annuloplasty had less residual mitral regurgitation [46].
Durability of Mitral Valve Annuloplasty
The long term durability of mitral valve annuloplasty for functional ischaemic mitral regurgitation has long been a concern with several observational studies reporting a high rate of significant recurrent mitral regurgitation. Mihaljevic, for example, estimates a recurrence rate of up to 20 % at 5 years [47]. A criticism of this study, however, is that there was no standard downsizing of the annuloplasty, and only in 22 % of cases was a rigid complete annuloplasty ring used; a partial flexible band was used in 71 % of cases and suture plication was used in 7 %.
As discussed earlier, several important principles are necessary to help ensure the long term durability of mitral annuloplasty for functional ischaemic mitral regurgitation. These include the use of a complete rigid or semi-rigid annuloplasty ring and not a flexible ring or band, undersizing the annuloplasty ring, achieving an adequate surface of mitral leaflet coaptation of at least 8 mm between the anterior and posterior leaflets, complete coronary artery revascularisation, and ensuring no more than trace mitral regurgitation at the end of the operation [5, 8, 12, 20]. Following these principles, Braun and Dion reported a mean mitral regurgitant grade of 0.8 ± 0.7 at 4 years with 85 % of patients having less than 2+ mitral regurgitation [9]. However, 16 % of survivors had moderate or more mitral regurgitation. Gelsomino et al. reported that 5 years after mitral annuloplasty and CABG, 28 % of patients had moderate mitral regurgitation, 31 % had moderate-severe mitral regurgitation, and 13 % had severe mitral regurgitation [48]. The recurrence of mitral regurgitation developed in most patients after 3 years. Of note, in this study, a complete annuloplasty ring was used, a rigid Classic ring in 52.9 % and a semi-rigid Physio ring in 47.1 %, and there was standard down-sizing of the annuloplasty ring by two sizes. Predictors of recurrent mitral regurgitation in this study was a dilated ventricle (left ventricular end-systolic volume greater than 45 ml), a more spherical left ventricle (sphericity index greater than 0.7), and poorer left ventricular function (left ventricular wall motion score index greater than 1.5). A criticism of this study was that the mean number of coronary artery bypass grafts performed was only 2.2 and it is possible that the patients were under revascularised allowing continued adverse left ventricular remodelling and left ventricular dilatation.
The concern over the long-term durability of mitral annuloplasty for functional ischaemic mitral regurgitation has added to the controversy over the optimal treatment for this condition, particularly if the mitral regurgitation is only of moderate severity. Proponents for concomitant mitral annuloplasty and CABG argue that uncorrected moderate mitral regurgitation will progress and worsen, and will have a significant impact on the ability of the left ventricle to recover and reverse remodel. However, opponents of this strategy argue that if significant numbers of patients are going to develop recurrent moderate or more mitral regurgitation even with mitral annuloplasty, the benefits of this strategy is questionable and needs to be balanced against the slightly increased operative risk of adding mitral annuloplasty to CABG [49].
Which Patient Should Have This Procedure
When deciding on which patient would benefit from combined CABG plus mitral annuloplasty, as compared to isolated CABG only, or mitral annuloplasty plus adjunctive subvalvular repair techniques, or a mitral valve replacement, several factors have to be taken into consideration. These include the severity of the mitral regurgitation, the degree of mitral leaflet tethering, the extent of left ventricular viability, and the size of the left ventricle.
Patients with mild-to-moderate ischemic mitral regurgitation, particularly if the left ventricle is fully viable, do very well with isolated CABG and do not need a concomitant mitral annuloplasty. This has been demonstrated in the CTSN moderate ischemic mitral regurgitation trial where 70 % of patients improved their mitral regurgitation severity with just isolated CABG [42]. When compared to those who had concomitant CABG plus mitral annuloplasty, no differences in left ventricular reverse remodelling were observed. Although left ventricular viability was not assessed in this trial, it is likely that most of the patients had fully viable myocardium as seen by the improvement in mitral regurgitation severity and left ventricular volumes with CABG alone. If large areas of non-viable myocardium are present, concomitant mitral annuloplasty should be considered.
If the mitral regurgitation is more severe with an effective regurgitation orifice area (ERO) between 20 and 40 mm2, and particularly if there are significant segments of non-viable myocardium, a mitral annuloplasty should be performed in addition to CABG. This has been demonstrated in the RIME Trial which recruited patients with moderate-severe functional ischaemic mitral regurgitation, 75 % of whom had non-viable scarred myocardium. Although the RIME Trial was set up as a trial to assess the best treatment for moderate functional ischaemic mitral regurgitation, a change in the threshold of severity for functional ischemic mitral regurgitation in the guidelines, meant that patients recruited into the RIME Trial can be considered as having moderate-severe functional ischaemic mitral regurgitation according to current guidelines [50]. These patients do much better with a concomitant CABG plus mitral annuloplasty compared to CABG alone, with improvements in functional capacity, symptoms and left ventricular reverse remodelling [41]. Mitral annuloplasty in these patients also have a very good result with a 96 % freedom from moderate or more mitral regurgitation at 1 year. Longer follow-up is obviously needed to ensure that the benefits reported are sustained in the longer term.
In the group of patients with even more severe ischemic mitral regurgitation (ERO greater than 40 mm2), and particularly if the left ventricle is also very dilated (left ventricular end diastolic diameter greater than 65 mm) with severe leaflet tethering (tethering distance greater than 10 mm), mitral annuloplasty does not appear to give very satisfactory results [9, 45]. This has been demonstrated in the CTSN severe ischemic mitral regurgitation trial where the freedom from moderate or more mitral regurgitation at 2 years was only 41 % [45]. In these patients, additional adjunctive procedures on the subvalvular apparatus should be considered if mitral annuloplasty is to be used, or alternatively, a mitral valve replacement should be considered.
References
Kaji S, Nasu M, Yamamuro A, Tanabe K. Annular geometry in patients with chronic ischemic mitral regurgitation. Three dimensional magnetic resonance imaging study. Circulation. 2005;112:I-409–14.
Yu H-Y, Su M-Y, Liao T-Y, Peng H-H. Functional mitral regurgitation in chronic ischemic coronary artery disease: analysis of geometric alterations of mitral apparatus with magnetic resonance imaging. J Thorac Cardiovasc Surg. 2004;128:543–51.
Ahmad RM, Gillinov M, McCarthy PM, Blackstone EH. Annular geometry and motion in human ischemic mitral regurgitation: novel assessment with three-dimensional echocardiography and computer reconstruction. Ann Thorac Surg. 2004;78:2063–8.
Chan KMJ, Amirak E, Zakkar M, Flather M, Pepper JR, Punjabi PP. Ischemic mitral regurgitation: in search of the best treatment for a common condition. Prog Cardiovasc Dis. 2009;51:460–71.
Braun J, Bax JJ, Versteegh MIM, Voigt PG. Pre-operative left ventricular dimensions predict reverse remodelling following restrictive mitral annuloplasty in ischemic mitral regurgitation. Eur J Cardiothorac Surg. 2005;27:847–53.
Spoor MT, Geltz A, Bolling SF. Flexible versus nonflexible mitral valve rings for congestive heart failure: differential durability of repair. Circulation. 2006;114(1 Suppl):I67–71.
Daimon M, Fukuda S, Adams D, McCarthy PM. Mitral valve repair with Carpentier-McCarthy-Adams IMR ETlogix annuloplasty ring for ischemic mitral regurgitation: early echocardiographic results from a multi-center study. Circulation. 2006;114:I588.
Bax J, Braun J, Somer S, Klautz R, Holman E. Restrictive annuloplasty and coronary revascularization in ischemic mitral regurgitation results in reverse left ventricular remodelling. Circulation. 2004;110:II-103–8.
Braun J, van de Veire NR, Klautz RJM, Versteegh MIM, Holman ER, Westenberg JM, Boersma E, van der Wall EE, Bax JJ, Dion RAE. Restrictive mitral annuloplasty cures ischemic mitral regurgitation and heart failure. Ann Thorac Surg. 2008;85:430–7.
Harris KM, Sundt TM, Aeppli D, Sharma T. Can late survival of patients with moderate ischemic mitral regurgitation be impacted by intervention on the valve? Ann Thorac Surg. 2002;74:1468–75.
Tahta SA, Oury JH, Maxwell JM, Hiro SP, Duran CMG. Outcome after mitral valve repair for functional ischemic mitral regurgitation. J Heart Valve Dis. 2002;11:11.
Hung J, Papakostas L, Tahta SA, Hardy BG. Mechanism of recurrent ischemic mitral regurgitation after annuloplasty. Continued LV remodelling as a moving target. Circulation. 2004;110:II-85–90.
Bhudia SK, McCarthy PM, Smedira NG, Lam B-K, Rajeswaran J, Blackstone EH. Edge-to-edge (Alfieri) mitral repair: results in diverse clinical settings. Ann Thorac Surg. 2004;77:1598–606.
McGee EC, Gillinov AM, Blackstone EH, Rajeswaran J, Cohen G. Recurrent mitral regurgitation after annuloplasty for functional ischemic mitral regurgitation. J Thorac Cardiovasc Surg. 2004;128:916–24.
Al-Radi OO, Austin PC, Tu JV, David TE, Yau TM. Mitral repair versus replacement for ischemic mitral regurgitation. Ann Thorac Surg. 2005;79:1260–7.
Calafiore AM, Di Mauro M, Gallina S, Giammarco GD. Mitral valve surgery for chronic ischemic mitral regurgitation. Ann Thorac Surg. 2004;77:1989–97.
Czer LSC, Maurer G, Bolger AF, De Robertis M, Chaux A, Matloff JM. Revascularization alone or combined with suture annuloplasty for ischemic mitral regurgitation: evaluation by color doppler echocardiography. Tex Heart Inst J. 1996;23:270–8.
Hueb AC, Jatene FB, Moreira LFP, Pomerantzeff PM. Ventricular remodelling and mitral valve modifications in dilated cardiomyopathy: new insights from anatomic study. J Thorac Cardiovasc Surg. 2002;124.
Timek TA, Lai DT, Tibayan F, Liang D. Ischemia in three left ventricular regions: insights into the pathogenesis of acute ischemic mitral regurgitaiton. J Thorac Cardiovasc Surg. 2003;125:559–69.
Kang DH, Kim M-J, Kang S-J, Song J-M. Mitral valve repair versus revascularization alone in the treatment of ischemic mitral regurgitation. Circulation. 2006;114:I499.
Bax JJ, Visser FC, Poldermans D, Elhendy A. Time course of functional recovery of stunned and hibernating segments after surgical revascularisation. Circulation. 2001;104:I-314–8.
Campwala SZ, Bansal RC, Wang N, Razzouk A, Pai RG. Mitral regurgitation progression following isolated coronary artery bypass surgery: frequency, risk factors, and potential prevention strategies. Eur J Cardiothorac Surg. 2006;29:348.
Hausmann H, Siniawski H, Hertzer R. Mitral valve reconstruction and replacement for ischemic mitral insufficiency: seven years follow up. J Heart Valve Dis. 1999;8:536–42.
Giga V, Ostojic M, Vujisic-Tesic B, Djordjevic-Dikic A. Exercise-induced changes in mitral regurgitation in patients with prior myocardial infarction and left ventricular dysfunction: relation to mitral deformation and left ventricular function and shape. Eur Heart J. 2005;26:1860–5.
Lancellotti P, Lebrun F, Pierard LA. Determinants of exercise-induced changes in mitral regurgitation in patients with coronary artery disease and left ventricular dysfunction. J Am Coll Cardiol. 2003;42:1921–8.
Ueno T, Sakata R, Iguro Y, Yamamoto H, Ueno M, Ueno T, Matsumoto K. Pre-operative advanced left ventricular remodelling predisposes to recurrence of ischemic mitral regurgitation with less remodelling. J Heart Valve Dis. 2008;17:36–41.
Menicanti L, Donato MD, Castelvecchio S, Santambrogio C. Functional ischemic mitral regurgitation in anterior ventricular remodelling: results of surgical ventricular restoration with and without mitral repair. Heart Fail Rev. 2005;9:317–27.
Ramadan R, Al-Attar N, Mohammadi S. Left ventricular infarct plication restores mitral function in chronic ischemic mitral regurgitation. J Thorac Cardiovasc Surg. 2005;129:440–2.
Mishra YK, Mittal S, Jaguri P, Trehan N. Coapsys mitral annuloplasty for chronic functional ischemic mitral regurgitation: 1-year results. Ann Thorac Surg. 2006;81:42.
Kongsaerepong V. Echocardiographic predictors of successful versus unsuccessful mitral valve repair in ischemic mitral regurgitation. Am J Cardiol. 2006;98:504.
Gelsomino S, Lorusso R, Caciolli S, Capecchi I, Rostagno C, Chioccioli M, De Cicco G, Bille G, Stefano P, Gensini GF. Insights on left ventricular and valvular mechanisms of recurrent ischemic mitral regurgitation after restrictive annuloplasty and coronary artery bypass grafting. J Thorac Cardiovasc Surg. 2008;136:507–18.
Kron IL, Green GR, Cope JT. Surgical relocation of the posterior papillary muscle in chronic ischemic mitral regurgitation. Ann Thorac Surg. 2002;74:600–1.
Hvass U, Tapia M, Baron F, Pouzet B. Papillary muscle sling: a new functional approach to mitral repair in patients with ischemic left ventricular dysfunction and functional mitral regurgitation. Ann Thorac Surg. 2003;75:809–11.
Messas E, Pouzet B, Touchot B, et al. Efficacy of chordal cutting to relieve chronic persistent ischemic mitral regurgitation. Circulation. 2003;108:111–5.
Punjabi PP, Chan KMJ. Mitral valve surgery. In: Punjabi PP, editor. Essentials of operative cardiac surgery. Cham: Springer International Publishing; 2015.
Vaskelyte J, Stoskute N, Ereminiene E, Zaliunas R, Benetis R. The impact of unrepaired versus repaired mitral regurgitation on functional status of patients with ischemic cardiomyopathy at one year after coronary artery bypass grafting. J Heart Valve Dis. 2006;15:747.
Serri K, Bouchard D, Demers P, Coutu M, Pellerin M. Is a good perioperative echocardiographic result predictive of durability in ischemic mitral valve repair? [see comment]. J Thorac Cardiovasc Surg. 2006;131:565.
Filsoufi F, Aklog L, Byrne JG, Cohn LH, Adams DH. Current results of combined coronary artery bypass grafting and mitral annuloplasty in patients with moderate ischemic mitral regurgitation. J Heart Valve Dis. 2004;13:747–53.
Gillinov AM, Wierup PN, Blackstone EH, Bishay ES. Is repair preferable to replacement for ischemic mitral regurgitation? J Thorac Cardiovasc Surg. 2001;122:1125–41.
Bonacchi M, Prifti E, Maiani M, Frati G. Mitral valve surgery simultaneous to coronary revascularization in patients with end-stage ischemic cardiomyopathy. Heart Vessels. 2006;21:20–7.
Chan KMJ, Punjabi PP, Flather M, Wage RR, Symmonds K, Roussin I, Rahman-Haley S, Pennell DJ, Kilner PJ, Dreyfus GD, Pepper JR, Investigators R. Coronary artery bypass surgery with or without mitral valve annuloplasty in moderate functional ischemic mitral regurgitation: final results of the randomized ischemic mitral evaluation (RIME) trial. Circulation. 2012;126:2502–10.
Smith PK, Puskas JD, Ascheim DD, Voisine P, Gelijns AC, Moskowitz AJ, Hung JW, Parides MK, Ailawadi G, Perrault LP, Acker MA, Arenziano M, Thourani V, Gammie JS, Miller MA, Page P, Overbey JR, Dagenais F, Rose EA, Moquete EG, Jeffries N, Gardner TJ, O’Gara PT, Alexander JH, Michler RE. Surgical treatment of moderate ischemic mitral regurgitation. New Engl J Med. 2014;371:2178–88.
Acker MA, Parides MK, Perrault LP, Moskowitz AJ, Gelijns AC, Voisine P, Smith PK, Hung J, Blackstone EH, Puskas JD, Argenziano M, Gammie JS, Mack M, Ascheim DD, Bagiella E, Moquete EG, Ferguson TB, Horvath KA, Geller NL, Miller MA, Woo YJ, D’Alessandro DA, Ailawadi G, Dagenais F, Gardner TJ, O’Gara PT, Michler RE, Kron IL, CTSN. Mitral valve repair versus replacement for severe ischemic mitral regurgitation. New Engl J Med. 2014;370:23–32.
Fattouch K, Guccione F, Sampognaro R, Panzarella G, Corrado E, Navarra E, Calvaruso D, Ruvolo G. Efficacy of adding mitral valve annuloplasty to coronary artery bypass grafting in patients with moderate ischemic mitral valve regurgitation: a randomized trial. J Thorac Cardiovasc Surg. 2009;138:278–85.
Goldstein D, Moskowitz AJ, Gelijns AC, Ailawadi G, Parides MK, Perrault LP, Voisine P, Dagenais F, Gillinov AM, Thourani V, Argenziano M, Gammie JS, Mack M, Demers P, Atluri P, Rose EA, O’Sullivan K, Williams DL, Bagiella E, Michler RE, Weisel RD, Miller MA, Geller NL, Taddei-Peters WC, Smith PK, Moquete EG, Overbey JR, Kron IL, O’Gara PT, Acker MA, CTSN. Two year outcomes of surgical treatment of severe ischemic mitral regurgitation. New Engl J Med. 2016;374(20):1932–41.
Benedetto U, Melina G, Roscitano A, Fiorani B, Capuano F, Sclafani G, Comito C, di Nucci GD, Sinatra R. Does combined mitral valve surgery improve survival when compared to revascularisation alone in patients with ischemic mitral regurgitation? A meta-analysis on 2479 patients. J Cardiovasc Med. 2009;10:109–14.
Mihaljevic T, Lam B-K, Razzouk A, Takagaki M, Lauer MS, Gillinov AM, Blackstone EH, Lytle BW. Impact of mitral valve annuloplasty combined with revascularization in patients with functional ischemic mitral regurgitation. J Am Coll Cardiol. 2007;49:2191–201.
Gelsomino S, Lorusso R, De Cicco G, Capecchi I, Rostagno C, Caciolli S, Romagnoli S, Broi UG, Stefano P, Gensini GF. Five year echocardiographic results of combined undersized mitral ring annuloplasty and coronary artery bypass grafting for chronic ischaemic mitral regurgitaiton. Eur Heart J. 2008;29:231–40.
Jones RH. Adding mitral valve annuloplasty to surgical revascularisation does not benefit patients with functional ischemic mitral regurgitation. J Am Coll Cardiol. 2007;49:2202–3.
Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin III JP, Guyton RA, O’Gara PT, Ruiz CE, Skubas NJ, Sorajja P, Sundt III TM, Thomas JD. 2014 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63:e57–185.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Chan, K.M.J., Pepper, J.R. (2017). Treatment of Functional Ischemic Mitral Regurgitation by Mitral Valve Repair and Coronary Artery Bypass Grafting. In: Chan, K. (eds) Functional Mitral and Tricuspid Regurgitation. Springer, Cham. https://doi.org/10.1007/978-3-319-43510-7_7
Download citation
DOI: https://doi.org/10.1007/978-3-319-43510-7_7
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-43508-4
Online ISBN: 978-3-319-43510-7
eBook Packages: MedicineMedicine (R0)