Abstract
Functional ischemic mitral regurgitation is primarily caused by myocardial ischaemia or infarction with secondary effects on the mitral valve apparatus and the left ventricle leading to mitral regurgitation and left ventricular dilatation and dysfunction. A range of treatment options are available to treat this condition and these must be tailored to each individual patient. It must be appreciated that functional ischaemic mitral regurgitation is a heterogeneous condition with a range of severity of the different pathologies.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
Functional ischemic mitral regurgitation has an adverse outcome with an increased probability of death and of heart failure, which is related to the severity of the mitral regurgitation [1–3]. The greater the severity of the mitral regurgitation, the higher the probability of death and of heart failure. The aim of any intervention in this condition is therefore twofold: to improve survival, and to improve symptoms and functional status. To achieve this, it is necessary to correct any myocardial ischemia which was responsible for causing this condition, and to correct the mitral regurgitation if it is significant. Addressing these two pathologies successfully would lead to left ventricular reverse remodeling, which should translate to an improvement in symptoms, functional status and survival. Several treatment options are available and successful treatment of this condition would necessitate a combination of these interventions so that each of the underlying pathologies is adequately addressed: (1) optimal medical treatment for coronary artery disease and heart failure, (2) coronary artery revascularization, (3) mitral valve repair or replacement, and (4) left ventricular restoration surgery.
Functional ischemic mitral regurgitation is a heterogeneous condition (Table 16.1). Patients present with varying severity of the mitral regurgitation: from mild, to moderate, to severe, to the very severe mitral regurgitation. There are varying degrees of mitral leaflet tethering, and of left ventricle viability, size and function. Each of these factors has a significant impact on the natural history of the condition, and on the response to coronary artery revascularization alone, concomitant mitral valve repair or replacement, and the need for additional interventions on the left ventricle. Treatment therefore needs to be tailored to each individual patient taking into consideration all of these factors. Furthermore, the American Heart Association (AHA) and the American College of Cardiology (ACC) has recently revised its grading of the severity of functional ischemic mitral regurgitation (Table 16.2) [4]. In addition to mitral valve hemodynamics, valve and left ventricular anatomy and geometry, as well as associated cardiac findings and symptoms are now taken into consideration in the grading of functional ischemic mitral regurgitation severity. These are all considerations which need to be taken into account when deciding on the best treatment for the patient with functional ischemic mitral regurgitation (Table 16.3).
Grade A Ischemic Mitral Regurgitation
Using the recent AHA/ACC guidelines classification, these patients are at risk of mitral regurgitation; they do not have significant mitral regurgitation and have only a small mitral regurgitant jet at most. The mitral valve leaflet geometry is relatively normal and the left ventricle is normal in size or only mildly dilated [4]. These patients do not require any intervention on the mitral valve. They need to be optimized on medical treatment for ischemic heart disease and coronary artery revascularization performed if appropriate. In observational studies, only 12 % of these patients had progression of their mitral regurgitation severity [5]. However, the long term survival of these patients remains worse compared to patients who do not have mitral regurgitation, although the mitral regurgitation in these cases may not be the cause of the worse prognosis, but may just be a marker of a more dilated left ventricle with poorer function [6].
Grade B Ischemic Mitral Regurgitation
These patients are referred to as having progressive mitral regurgitation in the AHA/ACC guidelines. The mitral regurgitation is mild-to-moderate in severity with an effective regurgitant orifice area (ERO) of less than 20 mm2, the mitral leaflet tethering is mild and the left ventricle is only mildly dilated with some systolic dysfunction [4]. In these patients, if the left ventricle myocardium is fully viable, left ventricular function is likely to recover with complete coronary artery revascularization in addition to optimal medical therapy, and the mitral regurgitation will likely reduce as a result, with reverse remodeling of the left ventricle. This was demonstrated in the Cardiothoracic Surgical Network (CTSN) Moderate Mitral Regurgitation randomized trial where 70 % of patients receiving isolated coronary artery bypass graft surgery (CABG) showed an improvement in their mitral regurgitation severity at 1 year, and there was similar reductions in left ventricular volumes regardless of whether the patients received isolated CABG or concomitant CABG plus mitral valve annuloplasty [7]. However, if significant non-viable myocardium is present, recovery of left ventricular function is less likely to occur, leaving the patient with persistent mitral regurgitation and absence of left ventricular reverse remodeling; in these patients, concomitant mitral annuloplasty should be considered at the time of CABG.
Grades C and D Ischemic Mitral Regurgitation
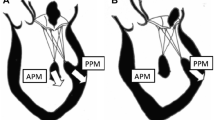
The AHA/ACC guidelines refer to this group of patients as having severe ischemic mitral regurgitation. They may be asymptomatic (Grade C) or symptomatic (Grade D) [4]. These patients have significant mitral regurgitation with an ERO greater than 20 mm2 and require an intervention on the mitral valve, as demonstrated in the Randomised Ischemic Mitral Evaluation (RIME) Trial, where patients randomized to concomitant CABG plus mitral annuloplasty had significantly better functional capacity, symptoms, and left ventricular reverse remodeling at 1 year compared to patients who received isolated CABG [8]. Provided the correct surgical principles are followed and there is no severe mitral leaflet tethering (tethering distance less than 10 mm), and the left ventricle is not overly dilated (left ventricular end diastolic diameter less than 65 mm), mitral annuloplasty in this group of patients is very successful and durable; the freedom from moderate or more mitral regurgitation at 1 year in the RIME Trial was 96 % [8, 9]. However, if significant mitral leaflet tethering is present (tethering distance greater than 10 mm), some additional subvalvular repair techniques may be necessary in addition to mitral annuloplasty to ensure a durable repair [10]. Alternatively, a mitral valve replacement may be the preferred operation. If the left ventricle is severely dilated (LVEDD greater than 65 mm), additional left ventricular restoration surgery may be necessary to improve the survival of the patient [9].
Very Severe Mitral Regurgitation
This refers to the group of patients with an ERO greater than 40 mm2. This group of patients are not distinguished from those with lesser severity of mitral regurgitation (ERO 20–40 mm2) in the recent AHA/ACC guidelines; both groups are considered as having severe ischemic mitral regurgitation [4]. However, the two groups behave very differently and so should be considered separately when deciding on the choice of surgical interventions. The CTSN Severe Ischemic Mitral Regurgitation Trial demonstrated that mitral annuloplasty in patients with an ERO greater than 40 mm [2] did not have a very good durability; the freedom from moderate or more mitral regurgitation at 2 years was only 64 %, and patients receiving a mitral annuloplasty had significantly more heart failure episodes compared to patients who received a mitral valve replacement [11]. Mitral valve replacement is therefore the preferred intervention in this group of patients, or alternatively, additional subvalvular repair procedures in addition to an annuloplasty are necessary if mitral valve repair is to be performed. On the other hand, patients with lesser severity of mitral regurgitation (ERO 20–40 mm2), but who are still considered as having severe ischemic mitral regurgitation according to current guidelines, do very well with a mitral annuloplasty at the time of CABG [4]. The RIME Trial demonstrated a 96 % freedom from moderate or more recurrent mitral regurgitation at 1 year following concomitant mitral annuloplasty plus CABG in this group of patients, with corresponding improvements in functional capacity, symptoms and left ventricular reverse remodeling compared to those receiving isolated CABG [8].
References
Aronson D, Goldsher N, Zukermann R, Kapeliovich M. Ischemic mitral regurgitation and risk of heart failure after myocardial infarction. Arch Intern Med. 2006;166:2362–8.
Lamas GA, Mitchell GF, Flaker GC, Smith SC, Gersh BJ. Clinical significance of mitral regurgitation after acute myocardial infarction. Circulation. 1997;96(3):827–33.
Grigioni F, Detaint D, Avierinos J-F, Scott C, Tajik J, Enriquez-Sarano M. Contribution of ischemic mitral regurgitation to congestive heart failure after myocardial infarction. J Am Coll Cardiol. 2005;45:260–7.
Nishimura RA, Otto CM, Bonow RO, et al. 2014 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63(22):e57–185.
Campwala SZ, Bansal RC, Wang N, Razzouk A, Pai RG. Mitral regurgitation progression following isolated coronary artery bypass surgery: frequency, risk factors, and potential prevention strategies. Eur J Cardiothorac Surg. 2006;29(3):348.
Grossi EA, Crooke GA, Di Giorgi PL, Schwartz CA. Impact of moderate functional mitral insufficiency in patients undergoing surgical revascularization. Circulation. 2006;114(1):I573.
Smith PK, Puskas JD, Ascheim DD, et al. Surgical treatment of moderate ischemic mitral regurgitation. N Engl J Med. 2014;371:2178–88.
Chan KMJ, Punjabi PP, Flather M, et al. Coronary artery bypass surgery with or without mitral valve annuloplasty in moderate functional ischemic mitral regurgitation: final results of the randomized ischemic mitral evaluation (RIME) trial. Circulation. 2012;126:2502–10.
Braun J, van de Veire NR, Klautz RJM, et al. Restrictive mitral annuloplasty cures ischemic mitral regurgitation and heart failure. Ann Thorac Surg. 2008;85:430–7.
Fattouch K, Murana G, Castrovinci S, et al. Mitral valve annuloplasty and papillary muscle relocation oriented by 3-dimensional tranesophagel echocardiography for severe functional mitral regurgitation. J Thorac Cardiovasc Surg. 2012;143:S38–42.
Goldstein D, Moskowitz AJ, Gelijns AC, et al. Two year outcomes of surgical treatment of severe ischemic mitral regurgitation. N Engl J Med. 2016;374(4):344–53.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Chan, K.M.J. (2017). Which Treatment is Best for Functional Ischemic Mitral Regurgitation?. In: Chan, K. (eds) Functional Mitral and Tricuspid Regurgitation. Springer, Cham. https://doi.org/10.1007/978-3-319-43510-7_16
Download citation
DOI: https://doi.org/10.1007/978-3-319-43510-7_16
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-43508-4
Online ISBN: 978-3-319-43510-7
eBook Packages: MedicineMedicine (R0)