Abstract
The objective of this chapter is to describe the development, validation, and practical application of the first noninvasive, embryo viability assessment tool that has been designed to meet clinical test criteria and proven to add critical information to the decision-making practices of clinical embryologists. In describing this novel test, we review the criteria for development and validation of a clinical test, assess the scientific underpinning of prediction using time-lapse imaging, and introduce new advances in automation enabled by state-of-the-art computer vision software.
Note: The Eeva™ Test is CE mark approved in Europe and is cleared by the US FDA to provide adjunctive information on early human embryos during IVF cycles.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others

Keywords
FormalPara Learning Objectives-
Limitations of traditional embryo assessment methods based on embryo morphology
-
Emerging noninvasive technologies for embryo assessment
-
Validation steps needed to introduce new tools and technologies into the IVF laboratories
-
Automated time-lapse analysis in the Eeva Test
-
Clinical outcome studies using the Eeva Test
1 Introduction
In in vitro fertilization (IVF) practice, technologies or tests that can help assess the viability and developmental competence of embryos may not only improve IVF success rates; they may also enable broader adoption of single embryo transfer (SET), which would in turn reduce multiple gestation pregnancies and lower associated maternal/fetal risks [1]. Currently, standard embryo assessment methods depend on morphological evaluation by microscope at a few static points in time (e.g., Day 1, Day 2, Day 3, and Day 5 post-insemination) [2, 3]. Morphological evaluation and selection, however, have lacked underlying biological understanding and sufficient predictability for implantation due to the inherent subjectivity of morphological grading [4,5,6] and the weak correlation between morphology and embryonic health [7,8,9]. Without predictive and objective tools that can supplement morphology, clinical embryologists are routinely forced to make their best guess of which embryo(s) to transfer among morphologically similar embryos.
New research in embryo assessment promises to provide additional information to help discriminate among morphologically similar embryos and improve the likelihood of selecting the single embryo that will successfully develop, implant, and result in a live birth. However, before new tools and technologies can be introduced into the IVF laboratory, several validation steps should be taken to ensure their safety, accuracy, and efficacy. These steps, which follow the initial discovery and development phases, may include biological validation, clinical validation, performance characterization, and comparison to standard of care [10]. Increasingly, clinical practitioners and patients also expect successful validation to result in approval from a regulatory body [11]. In this case, the regulatory body would require the intended use of the new tool or technology to be clearly stated and validated.
The objective of this chapter is to describe the development, validation, and practical application of the first noninvasive embryo viability assessment tool that has been designed to meet clinical test criteria and proven to add critical information to the decision-making practices of clinical embryologists. In describing this novel test, we review the criteria for development and validation of a clinical test, assess the scientific underpinning of prediction using time-lapse imaging, and introduce new advances in automation enabled by state-of-the-art computer vision software.
2 Clinical Testing
The goal of clinical testing is to help clinicians improve assessment or treatment decisions by determining a disease risk probability (in the case of a screening test) or diagnosing a disease (in the case of a diagnostic test) [12]. Typically, a clinical test is developed against a reference standard test that is more invasive, more risky, or prohibitively expensive. A clinical test may also be developed as a first-pass surrogate for a more invasive procedure (e.g., venous ultrasonography serves as a surrogate marker of vein thrombosis and reduces the need for a highly invasive venography procedure [13]; cell-free fetal DNA analysis of maternal blood can detect fetal genetic anomalies without requiring invasive amniocentesis or chorionic villus sampling procedures [14]).
In clinical embryology, several noninvasive candidate technologies have been proposed as surrogates for invasive embryo assessment and predictors of embryo developmental potential, including culture media assessment [15,16,17], cumulus cell assessment [18, 19], and time-lapse imaging [20,21,22]. Parallel advances in assay and embryo biopsy techniques have resulted in increased use of preimplantation genetic testing (PGT) together with blastocyst culture for assessing not only the genetic and chromosomal status of an embryo but also its overall implantation potential [23, 24]. While embryo biopsy is invasive to the embryo and typically relevant for IVF patients indicating a need for PGT, noninvasive technologies have the potential to be more economical and more broadly applicable. However, most noninvasive technologies are in early development stages; as such, they have not been prospectively validated in independent clinical trials and lack the basic prerequisites for successful clinical translation.
Three major requirements are needed in order to successfully implement a novel embryo assessment technology or test into the IVF laboratory. First, a predictive biomarker based on scientific evidence and validated in clinical studies must be associated with a confirmable and desirable outcome. Second, the detection of the predictive biomarker must be accurate, reliable, and practical to use by clinicians. Finally, the combined test (predictive biomarker + detection method) must be characterized for performance and shown to provide actionable information that improves the standard of care. In addition to these major requirements, scientists have increasingly demanded that new technologies be brought to patients via an evidence-based approach that includes basic research, which provides scientific understanding and clinical confidence in the test [10, 11, 22]. In a recent review, Palmer et al. noted that in reproductive medicine, it is common for only the first milestone—report of a novel biomarker correlation—to be achieved; whereas, successful culmination of all milestones ideally results in content for regulatory submission documents and eventual regulatory approval [11]. In support of this approach, new standards for reporting diagnostic accuracy (STARD) are being required of authors seeking to publish new test results [25].
3 The Eeva Test
The Eeva™ Test was designed with clinical test criteria in mind and combines both a highly robust predictive marker of embryo development and a novel detection assay to rapidly obtain quantitative measurements of the biomarker in a clinical setting. Below we detail the use of Eeva in the IVF laboratory workflow and its underlying science and technology. We further describe clinical results from multiple prospective, multicenter studies that compare the use of Eeva results combined with morphology (adjunctive grading method) against morphology alone (traditional morphology grading method).
4 The Eeva Test Deployed in Standard Incubators or Benchtop Incubators
The original Eeva Test consisted of (1) a multi-well dish that provides individual culture for embryos with the same media drop, (2) an imaging system that collects data inside a standard incubator, and (3) intelligent software that automatically analyzes and measures cell division timings (◘ Fig. 42.1).
Recently, other incubator formats have been developed and adapted for use with the Eeva™ Test. Benchtop incubators are now being fitted with cameras, lighting sources, and time-lapse imaging software so that benchtop incubator users may also leverage Eeva’s unique automation capabilities. Importantly, these new time-lapse benchtop incubators utilize both brightfield and darkfield imaging. Utilizing both brightfield and darkfield modalities together provides more information about embryos than brightfield alone and may lead to further discovery of novel features correlated to embryos’ development potential.
5 Predictive Information Enabled by Time-Lapse
The first major requirement of a clinical test is identifying a predictive biomarker with correlation to a measureable, clinical outcome. Recently, increasing availability and usage of time-lapse imaging systems —both homemade and commercial variations—have enabled researchers to identify potential image biomarkers during human embryo culture in a safe and noninvasive manner. Time-lapse systems currently vary in a number of ways, harboring variations in format/footprint (e.g., some are enclosed in stand-alone box formats [26, 27], while others integrate seamlessly with conventional incubators [28,29,30,31]), embryo culture environment (e.g., some require individual culture of embryos [27], while others enable group culture [28,29,30,31]), and mode of illumination (e.g., most offer brightfield imaging, while others offer darkfield or multimodal imaging). Importantly, all systems inherently have optical alignment, focusing, image capture, and image storage capabilities and utilize low-power illumination that exposes embryos to overall less light than conventional microscopy [27, 29, 31]. As a result of these advances, the clinical embryology field has been able to study the function and consequences of dynamics occurring during human embryo development and explore application to clinical practice.
Time-lapse imaging in clinical embryology has a relatively long history that can be broken down into two phases: an observational phase and a predictive phase. Beginning in 1997, time-lapse imaging was focused on observing new aspects of embryo development, such as polar body extrusion, fertilization, pronuclear formation and abuttal, cytoplasmic flares, and embryo hatching [26, 32,33,34]. Since 2010, time-lapse imaging has shifted focus to identifying predictive parameters that can help assess developmental outcomes of the embryo, such as blastocyst development, implantation, and most recently ploidy [27, 29, 30]. Numerous publications since 2010 have reported statistically significant correlations between time durations of cell stages and embryo outcomes. These studies, together with studies that have demonstrated safety of time-lapse and continuous monitoring of human embryos, are reviewed in detail elsewhere [20,21,22]. Overall, the increasing intensity of interest in time-lapse imaging suggests that noninvasive biomarker discovery is feasible, ongoing, and promising for use in the clinic.
Time-lapse biomarkers have great potential as predictive clinical tests, but the reproducibility of their predictive ability is critical to validating clinical utility. An analysis of the studies that defined a precise time window for embryo development prediction showed that the major predictors are biomarkers observed in early embryo development, before the 5-cell stage. In particular, the time from 2- to 3-cell (P2) and the time from 3- to 4-cell (P3) stage were reported in six out of seven of the studies that investigated which embryos are most likely to become a blastocyst or implant or be euploid [27, 29, 35,36,37] (◘ Fig. 42.2) and several following reports [35, 38]. These P2 and P3 timings were consistent embryo viability predictors even when stimulation protocols [39], fertilization methods [40], culture media [41, 42], and culture environments [43] were varied. In addition to clinical reproducibility, mechanistic studies have also demonstrated that embryos with abnormal P2 and P3 timings exhibit distinct gene expression profiles [29], aneuploidy probabilities at the embryo level [30], aneuploidy at the single blastomere level [44], and micronuclei patterns [30], compared to embryos with normal P2 and P3 timings. This collection of evidence supports the conclusion that P2 and P3 are reliable across independent datasets, and, moreover, are grounded in basic scientific understanding. Development of the Eeva Test, therefore, was based on (1) incorporation of P2 and P3 into a simple classification tree and prediction algorithm and (2) development of intelligent image analysis software that could reliably measure P2 and P3 in a busy clinical laboratory.
Overview of published time-lapse biomarkers that are predictive of clinical outcomes. Landmark events captured by time-lapse imaging are mapped to the progression of preimplantation embryo development. Time-lapse biomarkers that have been used for prediction in at least three publications—and are implemented in the Eeva Test—are colored dark red, while others are colored light blue. Average values for embryo outcomes within the optimally predictive windows are labeled above colored bars. (Adapted with permission from Chen et al. [22])
6 Automation Enabled by Intelligent Software
The second major requirement of a clinical test is that it is technically reliable, accurate, and practical for daily laboratory use. Although time-lapse biomarkers may provide great clinical value, extraction of these markers requires manual assessment of hundreds of images per embryo, which would be prohibitively time-consuming and laborious for routine use. In order for predictive time-lapse biomarkers to be clinically realized, novel detection methods are required to automatically extract and quantify image data in a high-throughput fashion.
Computer vision software that can analyze embryo videos in real time is now transforming the time-lapse imaging field and allowing predictive biomarkers to be rapidly quantified in the clinical laboratory. Image analysis software is widespread in many areas of clinical laboratory medicine, such as oncology and pathology. In reproductive medicine, software tools for quantitative and rapid image analysis of sperm quality [45] and for screening cervical cytology samples [46, 47] are also available. Applied to clinical embryology, image analysis software is particularly challenging due to several unique features of the developing human embryo. Blastomeres of the human embryo may divide in multiple dimensions (e.g., in and out of plane) and may include confounding events (e.g., fragmentation, reverse cleavage, abnormal cleavage). In addition, for each patient, multiple embryos developing at variable rates must be surveyed.
In their 2010 report demonstrating the first use of three cell cycle parameters to predict embryo development, Wong et al. also established the first proof of concept of cell tracking software used to measure the cell cycle parameters in human embryos [29]. The Wong et al. approach utilized computer vision techniques to simulate images and compare the simulations to observed image data for 14 cryopreserved embryos. In their study, darkfield imaging was employed as it provided strong contrast of blastomere membranes for model estimations. The development of the Eeva Test introduced a data-driven probabilistic framework that uses approximate inference to quantify P2 and P3 and validated the Eeva Test’s predictive performance for approximately 1000 fresh human embryos [31]. Eeva software predictions were shown to have good (>90%) agreement with manual predictions made by human observers [31]. Separate from this technological advance, other groups have performed research to help automate the morphological analysis of static embryo images to the blastocyst stage [48, 49] and the detection of cytoplasmic waves generated post-fertilization [50]. Since the objective in designing the Eeva Test was to provide embryologists with quantitative information about embryo development, the test focused on the clinically and scientifically validated predictive markers P2 and P3 and integrated automated software to quantify these validated parameters.
7 Clinical Outcomes for Using the Eeva Test
The final and often most elusive requirement for a novel clinical embryology test is that it is characterized for performance and shown to improve the standard of care. When performing a retrospective study, it is relatively straightforward to extract one or more promising biomarkers from a sampling of time-lapse videos. However, it is challenging and significantly less common to demonstrate comparable performance of the biomarker on an independent set of prospectively collected test data from multiple centers. It is rarer still that new potential selection methods are compared to traditional embryo selection methods based on morphology. Here, we describe how the Eeva Test provides validated and actionable information that may improve current embryo selection based on morphology.
7.1 The Eeva Test Is Independently Validated in Diverse Clinical Embryology Laboratories
Following the development of the integrated Eeva Test, we conducted a prospective, five-center clinical study that was designed to assess its performance on a diverse and independent clinical dataset and to evaluate the effectiveness and utility of using the test as an adjunct to traditional morphological assessment (► ClinicalTrials.gov #NCT01369446) [31]. Specifically, we sought to test the Eeva Test’s ability to assist embryologists in selecting embryos that have the greatest potential to develop into usable blastocysts (i.e., blastocysts suitable for transfer or freezing) as well as the Eeva Test’s impact on embryologists’ embryo selection decisions. The ability to predict blastocyst formation by Day 3 has clinical value as it could potentially improve IVF success rates while avoiding the potential risks associated with extended culture for blastocyst transfer [51,52,53,54,55,56].
Our initial results demonstrating the predictive power of time-lapse biomarkers P2 and P3 for identifying embryos with high developmental competence were consistent with Wong et al. and other successive studies [29]. Using refined cutoffs of P2 9.33–11.45 h and P3 0–1.73 h, the Eeva Test automatically differentiated a usable blastocyst from an arrested embryo with significantly improved diagnostic specificity (85%) compared to traditional morphology (57%, p < 0.0001) [31]. Specificity, or the ability to correctly predict which embryos will arrest, is highly relevant to embryo selection since traditional morphology is most limited in selecting among “good morphology” embryos. Furthermore, development and validation of the Eeva Test were performed on clinical data collected from five IVF clinics undergoing their own standard procedures for stimulation, egg retrieval, embryo culture, and insemination, suggesting broad applicability of the Eeva Test in diverse clinical embryology laboratories.
7.2 The Eeva Test Improves Embryo Selection and Reduces Embryologist Variability
Since clinical embryologists are faced daily with the challenge of selecting from among several comparable embryos those which are the top candidates for transfer, it was important to assess the impact of the Eeva Test on embryologists’ embryo assessment decisions. Our prospective study design evaluated the embryo assessment of three experienced clinical embryologists for 755 embryos. Two methods of embryo assessment were compared: in the first arm, embryologists made predictions about embryo development using Day 3 morphology only (traditional grading method); in the second arm, the same embryologists made predictions about embryo development using Day 3 morphology plus Eeva Test results (adjunctive grading method) (◘ Fig. 42.3a).
Adjunctive use of D3 morphology plus Eeva Test results significantly improves the specificity of D3 embryo selection. a Design for an embryo selection cohort study comparing the use of D3 morphology vs. D3 morphology plus Eeva Test results. b–d D3 embryo selection by individual embryologists (1, 2, and 3) using morphology only versus morphology plus Eeva Test for b all embryos (n = 755); c “good morphology” embryos (n = 235), defined using criteria of 6–10 cells, <10% fragmentation, and perfect symmetry; and d “good morphology” embryos (n = 178), defined using more stringent criteria of 7–8 cells, <10% fragmentation, and perfect symmetry. Note that embryologists 1 and 2 were very conservative in their morphological assessments and expected that almost all D3 “good morphology” embryos would become usable blastocysts. Error bars represent upper 95% confidence interval. **p < 0.01, #p < 0.0001. (Adapted with permission from Conaghan et al. [31])
When Eeva Test was used adjunctively with Day 3 morphology, each embryologist’s likelihood of selecting embryos that would develop to blastocysts was significantly improved compared to traditional morphological methods alone (◘ Fig. 42.3b). This improvement was even more pronounced among a subset of n = 235 embryos that were preselected as having “good” morphology (6–10 cells, <10% fragmentation, perfect symmetry) (◘ Fig. 42.3c) and a subset of n = 178 embryos where “good” morphology was more stringently defined (7–8 cells, <10% fragmentation, perfect symmetry) (◘ Fig. 42.3d). As expected, each case demonstrated remarkably high inter-individual variability when morphology alone was used for embryo assessment. When the Eeva Test was used together with morphology, the embryologists’ performances were more consistent, as the standard deviation among embryologists was reduced [31].
In a separate study, we used the Eeva Test to assess differences in embryo scoring among a diverse set of embryologists, postulating that better, more consistent embryo scoring would positively impact any embryologist’s ability to choose the embryo with the highest developmental potential [57]. This study was performed by looking at five different embryologists from unique practices around the United States, including three senior embryologists with at least 10 years of clinical experience and two junior embryologists with less than 3 years of experience from practices that performed between 300 and 1000 fresh IVF cycles per annum. To assess embryologists’ performance, odds ratio (OR) and other diagnostic measures were calculated by comparing prediction results to true blastocyst outcomes.
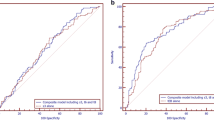
When Eeva Test results were used adjunctively with morphology, the odds of an embryo forming a blastocyst was 3.51-fold (95% CI = 2.62–4.69) higher in the group predicted to develop into blastocysts than in other embryos. In contrast, the OR using morphology alone was 2.69 (95% CI = 2.06–3.50). This improvement in OR was also assessed in the subset of morphologically good and fair embryos. By morphology alone, the OR for this subset dropped to 1.68, slightly better than random prediction (p < 0.0001). Adding Eeva Test results improved OR to 2.57, a 53% increase over traditional morphology and significantly better than random prediction (p < 0.0001, ◘ Fig.42.4a). In addition to OR, Eeva Test results also helped improve the positive predictive value (PPV) over morphology alone (54% vs. 43%, p = 0.02) while maintaining the same level of negative predictive value (NPV, 68% vs. 68%, ◘ Fig. 42.4b).
Adjunctive use of Day 3 morphology plus Eeva Test results significantly improves Day 3 embryo selection and consistency among embryologists. a OR for predicting blastocyst formation using Morphology Only (left) and Morphology followed by Eeva Test (right). ORs and 95% confidence intervals were calculated for all embryos (represented in gray) and for the subset of embryos graded as good/fair (represented in blue). b Mean PPV and mean NPV across all embryologists predicting blastocyst formation using Morphology Only and Morphology followed by Eeva Test, among good/fair embryos. *p = 0.02, ns (not significant; error bars represent upper 95% confidence intervals). c Consistent improvement in ORs for individual embryologists who predicted blastocyst formation using Morphology Only and Morphology followed by Eeva Test, among good/fair embryos. (Reproduced with permission from Diamond et al. [57])
These results indicate that the Eeva Test aids embryologists of diverse backgrounds by distinguishing among similar-looking embryos that are evaluated first by morphological criteria. Using Eeva Test results as an adjunct to morphology, every individual embryologist’s prediction performance was improved (◘ Fig. 42.4c). Using the Eeva Test adjunctively to morphology, the variability in performance across all five embryologists was reduced from a range of 1.06 (OR = 1.14–2.20) to a range of 0.45 (OR = 2.33–2.78, ◘ Fig. 42.4c). Notably, the embryologist with the greatest improvement in OR was one of the senior embryologists with more than 10 years of training in morphology grading. Since intra- and inter-operator variability in morphological grading has been shown to negatively impact IVF success rates [4, 6], adjunctive use of the Eeva Test may improve the standardization, reproducibility, and ultimate success of Day 3 embryo selection.
7.3 Eeva Test Results Correlate to Implantation and Pregnancy
While the first critical steps in developing the Eeva Test as a predictive and automated clinical assay have been achieved, further work is needed to confirm the impact of Eeva Test results on implantation and pregnancy outcomes . Toward this goal, we performed the first analysis examining whether the time-lapse markers used by the Eeva Test correlate with implantation and pregnancy outcomes. We focused our analysis on embryos that were transferred at the blastocyst stage using standard morphological selection criteria (without Eeva Test results). Of 141 embryos transferred at the blastocyst stage, those embryos denoted by the Eeva Test as having a high probability to develop (Eeva High indicating P2, 9.33–11.45 h, and P3, 0–1.73 h) had a statistically higher chance of implantation than those embryos denoted by the Eeva Test as having a low probability to develop (Eeva Low indicated by P2 or P3 out of specific timing windows) (49% vs. 21%, p < 0.001) (◘ Fig. 42.5). Similarly, for these 77 blastocyst transfer patients, those with at least one Eeva High embryo transferred were more likely to achieve clinical pregnancy (60% vs. 40%, p = 0.09) and ongoing pregnancy (56% vs. 37%, p = 0.11) than those with only Eeva Low embryos transferred. These results add further evidence to recent retrospective reports showing correlation between P2, P3, and implantation [27] and pregnancy outcomes [58].
Time-lapse markers used by the Eeva Test are correlated with positive implantation and pregnancy outcomes. A retrospective analysis of implantation and pregnancy rates was performed for two populations of patients with Eeva imaging and blastocyst transfer based on morphology only. The two patient populations included those with at least one Eeva High transferred (i.e., one Eeva High embryo could be transferred with another Eeva High or Eeva Low embryo) and those with only Eeva Low transferred (i.e., one or more Eeva Low embryos were transferred). The Eeva High vs. Low denominations are based on whether time-lapse markers P2 and P3 are within defined time windows (P2, 9.33–11.45 h, and P3, 0–1.73 h). (Adapted with permission from Chen et al. [22])
The Eeva Test’s fully automated algorithm was further examined in a blinded, multicenter study published in 2014 [59]. This study took place in six different IVF centers, each recruiting and treating patients using their own protocols, laboratory equipment, and consumables. A total of 331 transferred embryos with known implantation from 205 patients enrolled at 6 IVF clinics were analyzed. We found that Eeva High embryos had a significantly higher probability of successful implantation (37%, 41/111) than Eeva Low embryos (23%, 50/220, p = 0.003, ◘ Fig. 42.6a). Eeva Test results were also correlated with clinical pregnancy rates. Patients were divided into two groups: patients with at least one Eeva High embryo transferred and those with no Eeva High embryo transferred. Patients’ clinical characteristics for the two groups were compared, including egg age, number of eggs retrieved, number of 2PNs on Day 1 and number of embryos transferred. There was no statistically significant difference found for any of the clinical characteristics assessed. However, patients with at least one Eeva High embryo transferred had significantly higher clinical pregnancy rates than those with no Eeva High embryos transferred (51% vs. 39%, p = 0.04). Additional analysis of embryo implantation revealed a statistically significant difference between the two groups of patients (34% vs. 25%, p = 0.03). In a three-category version of the Eeva Test results (High/Medium/Low), Eeva High embryos had the highest likelihood of implantation (37%), followed by Eeva Medium (35%) and Eeva Low (15%); and the difference in implantation rates between Eeva High vs. Eeva Low embryos and Eeva Medium vs. Eeva Low embryos was statistically significant (p < 0.0001, p = 0.0004, respectively, ◘ Fig. 42.6b). Furthermore, although the IVF centers each followed their own standard procedures for embryo culture and selection, Eeva Test results correlated to embryo implantation consistently across the different IVF centers (◘ Fig. 42.6c).
The Eeva Test results are correlated with implantation. a Implantation rates for Eeva two-category High versus Low scored embryos. The difference in implantation rates between Eeva High and Eeva Low embryos is statistically significant: P = 0.003. b Implantation rates for Eeva three-category High, Medium, and Low scored embryos. Implantation rates between High versus Low and Medium versus Low were significantly different (P < 0.0001 and P = 0.0004, respectively). c Implantation rates for embryos with Eeva High, Medium, and Low scores from three clinical sites with at least 50 embryos of known implantation data per site. For all three sites, the difference in implantation rates between Eeva High and Low embryos is statistically significant (chi-squared test): P = 0.02 (site A); P = 0.02 (site B); P = 0.002 (site C). Error bars represent 95% upper confidence limit. (Reproduced with permission from VerMilyea et al. [59])
Consistent with our study results, a growing body of published, independent studies have reported that Eeva Test results correlate to implantation and/or pregnancy regardless of patient population or IVF practice patterns. Kirkegaard and colleagues performed a retrospective multicenter analysis of 1519 transferred embryos from 7 clinics located in 3 countries and found that embryos manually analyzed and classified as High had a statistically significantly higher implantation rate (30% relative increase) than embryos that were manually classified as Low [60]. Kieslinger and colleagues showed that in good prognosis patients (<41 years old, <3 previous attempts, and ≥ 5 2PNs) with mostly SET, transferring Eeva High and Medium embryos resulted in a significantly higher ongoing pregnancy rate of 36.8% (89/242) compared to 18.4% (7/ 38) for Eeva Low embryos (p = 0.02) [61]. Aparicio-Ruiz and colleagues conducted a multicenter retrospective study of 626 IVF cycles using donor oocytes with the following findings: (1) Eeva Test results were correlated with embryo implantation in not only cleavage-stage embryo transfer but also blastocyst transfer (implantation rates for cleavage stage transfer: Eeva High 38.2%, Medium 31.7%, and Low 26.1%; implantation rates for blastocyst transfer: Eeva High 66.7%, Medium 50%, Low 31%); (2) Patients where no Eeva High embryos were transferred had an ongoing pregnancy rate of 46.7%, while patients where at least one Eeva High embryo was transferred experienced a significantly increased ongoing pregnancy rate of 67% [62]. In comparison, no significant difference was observed for ongoing pregnancy rates in patients with or without morphology grade A embryos transferred (60.2% vs. 59.3%). This broad collection of publications by independent investigators provides strong evidence that the Eeva Test differentiates embryos with higher implantation potential, and may therefore complement traditional morphology to aid in embryo assessment.
7.4 The Eeva Test Improves Clinical Outcomes
The gold standard for evaluating the effectiveness of time-lapse-based embryo assessment is a well-designed randomized controlled trial (RCT). To ensure that an RCT is adequately powered, pilot studies are needed to estimate the sample size for RCT. Adamson and colleagues assessed the impact of using the Eeva Test in adjunct with traditional morphology by conducting a prospective concurrent cohort-controlled pilot study [63]. A total of 319 patients were assessed, 98 in the test group (the Eeva Test was used in embryo selection) and 221 in the control group (traditional morphology alone was used for embryo selection). All patients met the same inclusion/exclusion criteria including <41 years of age at the start of the IVF cycle, planned day 3 transfer, fewer than three failed IVF cycles, at least four zygotes (2PN on Day 1), and no PGT. Implantation rate and clinical pregnancy rate were significantly higher in the test group in which the Eeva Test was used compared to the control group (implantation rate, 30% vs. 19%, p = 0.003; clinical pregnancy rate 46% vs. 32%, p = 0.02, ◘ Fig. 42.7a, b). In a sub-analysis of the test group, the authors found that patients receiving at least one Eeva High embryo had significantly higher implantation rates than patients receiving only Eeva Low embryos (36.8% vs. 20.6%, ◘ Fig. 42.7c). Eeva High embryos compared with Low embryos also had significantly higher implantation rates (44.7% vs. 20.5%, ◘ Fig. 42.7d). Among morphologically good or top embryos, Eeva High embryos were also more likely to implant than Eeva Low embryos (◘ Fig. 42.7e–f). These results demonstrated the clinical impact of the Eeva Test in patients receiving Day 3 embryo transfers, adding further evidence that the Eeva Test results add valuable information beyond traditional morphology.
Using Eeva results together with morphology improves implantation and pregnancy rates for Day 3 embryo transfer. a Implantation rates in embryos selected using morphology plus Eeva results (Test) versus using morphology alone (Control). b Clinical pregnancy rates in patients whose embryos were selected using morphology plus Eeva results (Test) versus using morphology alone (Control). c Implantation rates for patients who had at least one Eeva High embryo transferred versus those who had only Low embryos transferred. d–f Known implantation rates for Eeva High versus Low embryos in all transferred embryos d, all good-quality embryos e, and top-quality embryos f. (Reproduced with permission from Adamson et al. [63])
8 Conclusion and Future Work
The Eeva Test is the first time-lapse-based clinical test for embryologists that has been cleared by the US Food and Drug Administration to aid in embryo selection. The Eeva Test has been validated in a series of prospective, multicenter studies and shown to add value to embryologists’ morphological evaluations by improving embryo assessment and reducing variability among embryologists. It combines both robust, predictive markers of embryo development along with a novel automated detection assay to rapidly obtain quantitative measurements of early embryo development markers that have been proven to be of value in determining the best embryo in a cohort of multiple embryos. The Eeva Test meets several important prerequisites for implementation in clinical practice: it is scientifically and clinically validated, it considers a practical intended use model, and it has demonstrated clinical utility compared to the standard of care.
As the Eeva Test continues to be developed in the lab, new markers of embryo viability and/or implantation potential can be unearthed. Additionally, as more labs routinely grow embryos to the blastocyst stage, significantly more frames of videos may be assessed to learn more about embryo development. Invasive tests of embryo chromosomal abnormality, for instance, PGT, continue to be applied to more embryos around the world, which supplies further outcome data to aid in ongoing time-lapse research. Ongoing time-lapse research will assess how noninvasive time-lapse imaging may be used in conjunction with invasive tests such as PGT to further improve embryo assessment. We envision that future versions of the Eeva Test will incorporate complementary morphological features and timings, blastocyst stage milestones, and other prospectively validated parameters. We further expect that automated analysis of these more complex morphological and timing features will require increasingly sophisticated approaches and likely a combination of illumination techniques. The introduction of any automated algorithm will be accompanied with the full spectrum of clinical validation steps described here to ensure safety and efficacy for clinical use.
References
van Montfoort AP, Dumoulin JC, Land JA, et al. Elective single embryo transfer (eSET) policy in the first three IVF/ICSI treatment cycles. Hum Reprod. 2005;20:433–6. https://doi.org/10.1093/humrep/deh619. deh619 [pii].
Alpha E. The Istanbul consensus workshop on embryo assessment: proceedings of an expert meeting. Hum Reprod. 2011;26:1270–83. https://doi.org/10.1093/humrep/der037. der037 [pii].
Racowsky C, Vernon M, Mayer J, et al. Standardization of grading embryo morphology. Fertil Steril. 2010;94:1152–3. https://doi.org/10.1016/j.fertnstert.2010.05.042.
Baxter Bendus AE, Mayer JF, Shipley SK, Catherino WH. Interobserver and intraobserver variation in day 3 embryo grading. Fertil Steril. 2006;86:1608–15. https://doi.org/10.1016/j.fertnstert.2006.05.037. S0015-0282(06)03047-0 [pii].
Montag M, Liebenthron J, Koster M. Which morphological scoring system is relevant in human embryo development? Placenta. 2011; https://doi.org/10.1016/j.placenta.2011.07.009. S0143-4004(11)00266-9 [pii].
Paternot G, Devroe J, Debrock S, et al. Intra- and inter-observer analysis in the morphological assessment of early-stage embryos. Reprod Biol Endocrinol. 2009;7:105. https://doi.org/10.1186/1477-7827-7-105.
Munné S, Tomkin G, Cohen J. Selection of embryos by morphology is less effective than by a combination of aneuploidy testing and morphology observations. Fertil Steril. 2009;91:943–5. https://doi.org/10.1016/j.fertnstert.2007.06.082.
Kroener L, Ambartsumyan G, Briton-Jones C, et al. The effect of timing of embryonic progression on chromosomal abnormality. Fertil Steril. 2012;98:876–80. https://doi.org/10.1016/j.fertnstert.2012.06.014.
Alfarawati S, Fragouli E, Colls P, et al. The relationship between blastocyst morphology, chromosomal abnormality, and embryo gender. Fertil Steril. 2011;95:520–4. https://doi.org/10.1016/j.fertnstert.2010.04.003. S0015-0282(10)00600-X [pii].
Harper J, Cristina Magli M, Lundin K, et al. When and how should new technology be introduced into the IVF laboratory? Hum Reprod. 2012;27:303–13. https://doi.org/10.1093/humrep/der414.
Palmer SS, Barnhart KT. Biomarkers in reproductive medicine: the promise, and can it be fulfilled? Fertil Steril. 2012;13:2431–4.
Feero WG, Guttmacher AE, Bodurtha J, Strauss JF. Genomics and perinatal care. N Engl J Med. 2012;366:64–73. https://doi.org/10.1056/NEJMra1105043.
Kucher N. Deep-vein thrombosis of the upper extremities. N Engl J Med. 2011;364:861–9. https://doi.org/10.1056/NEJMcp1008740.
Simpson JL. Cell-free fetal DNA and maternal serum analytes for monitoring embryonic and fetal status. Fertil Steril. 2013;99:1124–34. https://doi.org/10.1016/j.fertnstert.2013.02.012.
Hardarson T, Ahlstrom A, Rogberg L, et al. Non-invasive metabolomic profiling of day 2 and 5 embryo culture medium: a prospective randomized trial. Hum Reprod. 2012;27:89–96. https://doi.org/10.1093/humrep/der373.
Vergouw CG, Kieslinger DC, Kostelijk EH, et al. Day 3 embryo selection by metabolomic profiling of culture medium with near-infrared spectroscopy as an adjunct to morphology: a randomized controlled trial. Hum Reprod. 2012;27:2304. https://doi.org/10.1093/humrep/des175.
Seli E, Robert C, Sirard MA. OMICS in assisted reproduction: possibilities and pitfalls. Mol Hum Reprod. 2010;16:513–30. https://doi.org/10.1093/molehr/gaq041.
Huang Z, Wells D. The human oocyte and cumulus cells relationship: new insights from the cumulus cell transcriptome. Mol Hum Reprod. 2010;16:715–25.
Wathlet S, Adriaenssens T, Segers I, et al. New candidate genes to predict pregnancy outcome in single embryo transfer cycles when using cumulus cell gene expression. Fertil Steril. 2012;98:432. https://doi.org/10.1016/j.fertnstert.2012.05.007.
Kirkegaard K, Agerholm IE, Ingerslev HJ. Time-lapse monitoring as a tool for clinical embryo assessment. Hum Reprod. 2012;27:1277–85. https://doi.org/10.1093/humrep/des079. des079 [pii].
Wong CC, Chen AA, Behr B, Shen S. Time-lapse microscopy and image analysis in basic and clinical embryo development research. Reprod Biomed Online. 2012;26:120. https://doi.org/10.1016/j.rbmo.2012.11.003.
Chen AA, Tan L, Suraj V, et al. Biomarkers identified with time-lapse imaging: discovery, validation, and practical application. Fertil Steril. 2013;99:1035–43. https://doi.org/10.1016/j.fertnstert.2013.01.143.
Yang Z, Liu J, Collins GS, et al. Selection of single blastocysts for fresh transfer via standard morphology assessment alone and with array CGH for good prognosis IVF patients: results from a randomized pilot study. Mol Cytogenet. 2012;5:24. https://doi.org/10.1186/1755-8166-5-24.
Forman EJ, Upham KM, Cheng M, et al. Comprehensive chromosome screening alters traditional morphology-based embryo selection: a prospective study of 100 consecutive cycles of planned fresh euploid blastocyst transfer. Fertil Steril. 2013;100:718–24. https://doi.org/10.1016/j.fertnstert.2013.04.043.
Ochodo EA, Bossuyt PM. Reporting the accuracy of diagnostic tests: the STARD initiative 10 years on. Clin Chem. 2013;59:917–9. https://doi.org/10.1373/clinchem.2013.206516.
Mio Y, Maeda K. Time-lapse cinematography of dynamic changes occurring during in vitro development of human embryos. Am J Obs Gynecol. 2008;199:660 e1–5. https://doi.org/10.1016/j.ajog.2008.07.023. S0002-9378(08)00805-3 [pii].
Meseguer M, Herrero J, Tejera A, et al. The use of morphokinetics as a predictor of embryo implantation. Hum Reprod. 2011;26:2658–71. https://doi.org/10.1093/humrep/der256. der256 [pii].
Vajta G, Peura TT, Holm P, et al. New method for culture of zona-included or zona-free embryos: the well of the well (WOW) system. Mol Reprod Dev. 2000;55:256–64. https://doi.org/10.1002/(SICI)1098-2795(200003)55:3<256::AID-MRD3>3.0.CO;2-7. [pii] 10.1002/(SICI)1098-2795(200003)55:3<256::AID-MRD3>3.0.CO;2-7.
Wong CC, Loewke KE, Bossert NL, et al. Non-invasive imaging of human embryos before embryonic genome activation predicts development to the blastocyst stage. Nat Biotechnol. 2010;28:1115–21. https://doi.org/10.1038/nbt.1686. nbt.1686 [pii].
Chavez SL, Loewke KE, Han J, et al. Dynamic blastomere behaviour reflects human embryo ploidy by the four-cell stage. Nat Commun. 2012;3:1251. https://doi.org/10.1038/ncomms2249.
Conaghan J, Chen AA, Willman SP, et al. Improving embryo selection using a computer-automated time-lapse image analysis test plus day 3 morphology: results from a prospective multicenter trial. Fertil Steril. 2013;100:412–9.e5. https://doi.org/10.1016/j.fertnstert.2013.04.021.
Martini E, Flaherty SP, Swann NJ, et al. Analysis of unfertilized oocytes subjected to intracytoplasmic sperm injection using two rounds of fluorescence in-situ hybridization and probes to five chromosomes. Hum Reprod. 1997;12:2011–8.
Hardarson T, Lofman C, Coull G, et al. Internalization of cellular fragments in a human embryo: time-lapse recordings. Reprod Biomed Online. 2002;5:36–8.
Pribenszky C, Matyas S, Kovacs P, et al. Pregnancy achieved by transfer of a single blastocyst selected by time-lapse monitoring. Reprod Biomed Online. 2010;21:533–6. https://doi.org/10.1016/j.rbmo.2010.04.015. S1472-6483(10)00227-0 [pii].
Cruz M, Garrido N, Herrero J, et al. Timing of cell division in human cleavage-stage embryos is linked with blastocyst formation and quality. Reprod Biomed Online. 2012;25:371–81. https://doi.org/10.1016/j.rbmo.2012.06.017.
Hlinka D, Kalatova B, Uhrinova I, et al. Time-lapse cleavage rating predicts human embryo viability. Physiol Res. 2012;61:513–25.
Rubio I, Kuhlmann R, Agerholm I, et al. Limited implantation success of direct-cleaved human zygotes: a time-lapse study. Fertil Steril. 2012;98:1458–63.
Hashimoto S, Kato N, Saeki K, Morimoto Y. Selection of high-potential embryos by culture in poly(dimethylsiloxane) microwells and time-lapse imaging. Fertil Steril. 2012;97:332–7. https://doi.org/10.1016/j.fertnstert.2011.11.042. S0015-0282(11)02818-4 [pii].
Munoz M, Cruz M, Humaidan P, et al. Dose of recombinant FSH and oestradiol concentration on day of HCG affect embryo development kinetics. Reprod Biomed Online. 2012;25:382–9.
Dal Canto M, Coticchio G, Mignini Renzini M, et al. Cleavage kinetics analysis of human embryos predicts development to blastocyst and implantation. Reprod Biomed Online. 2012;25:474–80.
Ciray HN, Aksoy T, Goktas C, et al. Time-lapse evaluation of human embryo development in single versus sequential culture media-a sibling oocyte study. J Assist Reprod Genet. 2012;29:891. https://doi.org/10.1007/s10815-012-9818-7.
Basile N, Morbeck D, Garcia-Velasco J, et al. Type of culture media does not affect embryo kinetics: a time-lapse analysis of sibling oocytes. Hum Reprod. 2013;28:634–41. https://doi.org/10.1093/humrep/des462.
Ingerslev H, Hindkjaer J, Kirkegaard K. Effect of oxygen concentration on human embryo development evaluated by time-lapse monitoring. Hum Reprod. 2013;99:738–27. (suppl:ii22–ii24).
Vera-Rodriguez M, Chavez SL, Rubio C, et al. Prediction model for aneuploidy in early human embryo development revealed by single-cell analysis. Nat Commun. 2015;6:7601. https://doi.org/10.1038/ncomms8601.
Krause W, Viethen G. Quality assessment of computer-assisted semen analysis (CASA) in the andrology laboratory. Andrologia. 1999;31:125–9.
Dziura B, Quinn S, Richard K. Performance of an imaging system vs. manual screening in the detection of squamous intraepithelial lesions of the uterine cervix. Acta Cytol. 2006;50:309–11.
Lozano R. Comparison of computer-assisted and manual screening of cervical cytology. Gynecol Oncol. 2007;104:134–8. https://doi.org/10.1016/j.ygyno.2006.07.025.
Filho ES, Noble JA, Wells D. A review on automatic analysis of human embryo microscope images. Open Biomed Eng J. 2010;4:170–7. https://doi.org/10.2174/1874120701004010170.
Filho ES, Noble JA, Poli M, et al. A method for semi-automatic grading of human blastocyst microscope images. Hum Reprod. 2012;27:2641. https://doi.org/10.1093/humrep/des219.
Swann K, Windsor S, Campbell K, et al. Phospholipase C-zeta-induced Ca2+ oscillations cause coincident cytoplasmic movements in human oocytes that failed to fertilize after intracytoplasmic sperm injection. Fertil Steril. 2012;97:742–7. https://doi.org/10.1016/j.fertnstert.2011.12.013. S0015-0282(11)02865-2 [pii].
Papanikolaou EG, D’Haeseleer E, Verheyen G, et al. Live birth rate is significantly higher after blastocyst transfer than after cleavage-stage embryo transfer when at least four embryos are available on day 3 of embryo culture. A randomized prospective study. Hum Reprod. 2005;20:3198–203. https://doi.org/10.1093/humrep/dei217. dei217 [pii].
Papanikolaou EG, Camus M, Kolibianakis EM, et al. In vitro fertilization with single blastocyst-stage versus single cleavage-stage embryos. N Engl J Med. 2006;354:1139–46. https://doi.org/10.1056/NEJMoa053524. 354/11/1139 [pii].
Blake DA, Farquhar CM, Johnson N, Proctor M. Cleavage stage versus blastocyst stage embryo transfer in assisted conception. Cochrane Database Syst Rev. 2007:CD002118. https://doi.org/10.1002/14651858.CD002118.pub3.
Kallen B, Finnstrom O, Lindam A, et al. Blastocyst versus cleavage stage transfer in in vitro fertilization: differences in neonatal outcome? Fertil Steril. 2010;94:1680–3. https://doi.org/10.1016/j.fertnstert.2009.12.027. S0015-0282(09)04213-7 [pii].
Kalra SK, Ratcliffe SJ, Barnhart KT, Coutifaris C. Extended embryo culture and an increased risk of preterm delivery. Obstet Gynecol. 2012;120:69–75. https://doi.org/10.1097/AOG.0b013e31825b88fc.
Diamond MP, Willman S, Chenette P, Cedars MI. The clinical need for a method of identification of embryos destined to become a blastocyst in assisted reproductive technology cycles. J Assist Reprod Genet. 2012;29:391–6. https://doi.org/10.1007/s10815-012-9732-z.
Diamond MP, Suraj V, Behnke EJ, et al. Using the Eeva test™ adjunctively to traditional day 3 morphology is informative for consistent embryo assessment within a panel of embryologists with diverse experience. J Assist Reprod Genet. 2015;32:61–8. https://doi.org/10.1007/s10815-014-0366-1.
Meseguer M, Rubio I, Cruz M, et al. Embryo incubation and selection in a time-lapse monitoring system improves pregnancy outcome compared with a standard incubator: a retrospective cohort study. Fertil Steril. 2012;98:1481–1489.e10.
VerMilyea MD, Tan L, Anthony JT, et al. Computer-automated time-lapse analysis results correlate with embryo implantation and clinical pregnancy: a blinded, multi-Centre study. Reprod Biomed Online. 2014;29:729–36. https://doi.org/10.1016/j.rbmo.2014.09.005.
Kirkegaard K, Campbell A, Agerholm I, et al. Limitations of a time-lapse blastocyst prediction model: a large multicentre outcome analysis. Reprod Biomed Online. 2014;29:156–8. https://doi.org/10.1016/j.rbmo.2014.04.011.
Kieslinger DC, De Gheselle S, Lambalk CB, et al. Embryo selection using time-lapse analysis (early embryo viability assessment) in conjunction with standard morphology: a prospective two-center pilot study. Hum Reprod. 2016;31:2450–7. https://doi.org/10.1093/humrep/dew207.
Aparicio-Ruiz B, Basile N, Pérez Albalá S, et al. Automatic time-lapse instrument is superior to single-point morphology observation for selecting viable embryos: retrospective study in oocyte donation. Fertil Steril. 2016;106:1379–1385.e10. https://doi.org/10.1016/j.fertnstert.2016.07.1117.
Adamson GD, Abusief ME, Palao L, et al. Improved implantation rates of day 3 embryo transfers with the use of an automated time-lapse–enabled test to aid in embryo selection. Fertil Steril. 2016;105:369–375.e6. https://doi.org/10.1016/j.fertnstert.2015.10.030.
Acknowledgments
We gratefully acknowledge the physicians, embryologists, and patients who participated in the development and validation studies of the Eeva Test. We also thank the clinical trial experts, biology scientists, and computer vision engineers, for their technical contributions and insightful discussions.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Review Questions
Review Questions
-
1.
What are the limitations of traditional embryo assessment methods based on embryo morphology?
-
2.
What are the emerging noninvasive technologies for embryo assessment?
-
3.
What is the information provided by time-lapse imaging?
-
4.
What are the validation steps needed before new technologies are introduced?
-
5.
What types of evidence support the use of the Eeva Test?
-
6.
What are some of the future directions for time-lapse-based embryo assessment tool?
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Tan, L., Chen, A.A., Shen, S. (2019). Predicting Embryo Developmental Potential and Viability Using Automated Time-Lapse Analysis (Eeva™ Test). In: Nagy, Z., Varghese, A., Agarwal, A. (eds) In Vitro Fertilization. Springer, Cham. https://doi.org/10.1007/978-3-319-43011-9_42
Download citation
DOI: https://doi.org/10.1007/978-3-319-43011-9_42
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-43010-2
Online ISBN: 978-3-319-43011-9
eBook Packages: MedicineMedicine (R0)