Abstract
Probably benign (BI-RADS 3) lesions on MRI are an empirically assigned category that lack specific criteria that could be used for an objective diagnosis. In this chapter, we describe the probably benign BI-RADS 3 category on MRI and report frequency and malignancy rates. The rate of malignancy in BI-RADS 3 lesions on MRI is below 2 % in the majority of studies. It is lowest in foci (0.9 %) and highest in non-mass enhancements (4 %). Malignant BI-RADS 3 lesions diagnosed by immediate MR-directed ultrasound or a single MRI follow-up in 6–12 months (in case a lesion is not visible by MR-directed ultrasound or MR-directed ultrasound was not performed) support the recommendation of these two management approaches. Finally, in accordance with published data we discuss imaging criteria for those breast lesions that might or might not be appropriately be assigned BI-RADS 3 on MRI.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Probably benign
- BI-RADS 3
- Breast MRI
- Breast cancer
- Magnetic resonance imaging
- Breast Imaging Reporting and Data System
- Breast
- Breast lesion
- Breast disease
1 Introduction
The Breast Imaging and Reporting Data System (BI-RADS) of the American College of Radiology provides a lexicon of criteria for the description and categorization of breast lesions on mammography, ultrasound, and magnetic resonance imaging (MRI) [1].
The traditional definition of breast lesions categorized as BI-RADS 3 (probably benign) comes from mammography: these lesions are supposed to harbor a <2 % risk of malignancy. Consequently, immediate biopsy is not recommended and these lesions should undergo short-interval follow-up after 6 months, followed by additional examinations to establish long-term (2 years or more) lesion stability [2]. This approach ensures that the low proportion of lesions that might progress to cancer can be diagnosed early enough (short-interval follow-up) while the prognosis remains unaffected. Following the establishment of the BI-RADS 3 category on mammography, a reduction of unnecessary biopsies and decrease in health care costs has been achieved [2].
The BI-RADS 3 category on MRI has been adapted from the mammography BI-RADS 3 category [1]. However, several differences have to be considered. First, in contrast to the well-established criteria of BI-RADS 3 lesions on mammography and ultrasound, similar (imaging) criteria have not been established for MRI findings. Categorizing findings on breast MRI as probably benign (BI-RADS 3) has been modified primarily from the categorization of mammographic lesions (morphology, distribution, and symmetry). Nevertheless, the evaluation of breast MRI also includes additional information such as water content from (T2 signal), extracellular microstructure (Diffusion Weighted Imaging-DWI) and dynamic contrast-enhanced (DCE) analysis.
Second, short-interval follow-up MRI is not equivalent to short-interval follow-up mammography. Costs and interpretation times of MRI usually exceed those of mammography. Short-interval follow-up MRI is considered probably useful, but there are no established recommendations [1].
Third, the population undergoing MRI (e.g. for screening due to higher breast cancer risk, or staging due to known breast cancer) is different from that undergoing screening or diagnostic mammography [3]. Evaluation of a patient’s breast cancer risk and history, including planned and ongoing therapeutic interventions, is highly important when categorizing BI-RADS 3 lesions on MRI.
In this chapter, we describe the probably benign BI-RADS 3 category on MRI and report its frequency and malignancy rate (Table 14.1) [4–20]. We also review the published data and discuss management strategies and imaging criteria for those breast lesion types that might appropriately be classified as BI-RADS 3 on MRI.
2 Literature Data and Evidence-Based Recommendations
As outlined in the previous section, the probably benign category (BI-RADS 3) in breast MRI is based on subjective decision without standardized and established imaging criteria. Most published studies that evaluated the frequency of a BI-RADS 3 assessment (recommendation for short-interval follow-up) on MRI report a rate between 6 and 12 % (Table 14.1). The range of different frequency rates can be partly explained by the study populations. Indications for MRI in these studies showed a wide range from high-risk screening, to problem solving and breast cancer staging. In 17 studies published between 2000 and 2016 and comprising 2608 lesions, 51 cancers were finally diagnosed (Table 14.1). Only 24 of these 51 (47 %) lesions were diagnosed by MRI follow-up. Eight (16 %) lesions were immediately upgraded after MRI-directed ultrasound examinations were performed [16, 19, 20]. Other malignancies were either detected as incidental findings after prophylactic mastectomy, interval cancers by palpation or mammography after 24 months. Finally, information regarding time to and method of diagnosis was missing in a number of cases. Considering a time frame of 24 months as adequate to differentiate new interval cancers from real lesion progression (change in follow-up), only the 24 malignant findings identified by MRI follow-up constitute the basis for doing MRI follow-up examinations. These correspond to a 0.9 % rate of false negative BI-RADS 3 lesions on MRI. It seems to be evident from these numbers, that MRI follow-up over 24 months in 6 months intervals may not be justified considering the low likelihood of malignancy, examination costs and patient compliance. Considering these data, we can recommend the following management of MRI BI-RADS 3 lesions:
First, immediate MR-directed ultrasound (also known as second look ultrasound or targeted ultrasound) of the MRI-detected lesion. Despite the fact that MR-directed ultrasound is not yet standard of care to check BI-RADS 3 findings, this approach is justified by the substantial number of second look ultrasound upgrades of MRI BI-RADS 3 lesions reported in the literature [16, 19, 20]. The value of MR-directed ultrasound is corroborated by a recent meta-analysis reporting a substantial pooled detection rate of MRI detected malignant findings of 79 % (95 % CI 71–87 %) [21]. The same publication reports a pooled detection rate of benign findings of 52 % (95 % CI 44–60 %), suggesting that a substantial rate of benign MRI BI-RADS 3 lesions may be identified and followed up by ultrasound [21].
Second, a single MRI follow-up in 6–12 months should be performed in case the BI-RADS 3 lesion is not visible on MRI-directed ultrasound. As the majority of breast cancer screening programs apply 2 year screening intervals, the additional value of a 2 year MRI follow-up does not seem to be justified considering the low likelihood of malignancy after the aforementioned workup.
These considerations do not take into account the possibility of a misclassification of BI-RADS 3 lesions that demonstrate the criteria for malignancy. Although data on this topic is sparse, such misclassification has been described in up to 80 % of false negative MRI BI-RADS 3 lesions that should have been called BI-RADS 4 [20].
BI-RADS 3 lesions that undergo follow-up MRI should be histopathologically verified if they show any change in size or morphology. If, however, the lesion demonstrates stability as compared to prior MRI examinations, a decrease in size, or shows a resolution at any point during follow-up, the lesion should be considered benign.
In the following sections, we will discuss imaging features for those breast lesion types that might appropriately be assigned BI-RADS 3 on MRI.
2.1 Diagnostic Criteria in BI-RADS 3 Lesions
In short, there is no definite set of features that define BI-RADS 3 lesions. While the literature reports on malignancy rates in different types (e.g. mass, non-mass, foci) of BI-RADS 3 lesions, no definite data on diagnostic criteria defining the BI-RADS 3 category are given. BI-RADS 3 category should be assigned to lesions presenting benign appearing imaging features in case the radiologist feels the need for further confirmation. Presence of suspicious morphologic features that are unlikely associated with a benign diagnosis should always be called BI-RADS 4 and not BI-RADS 3. Specific features will be discussed in the respective lesion type sections.
Care should be taken in transferring conventional mammography and ultrasound criteria directly to breast MRI. For instance, a newly diagnosed lesion showing only benign features does not necessarily need to be followed-up. This holds true especially for mass lesions with circumscribed margins and persistent or plateau enhancement curves. These findings are generally benign, especially when additional T2w and DWI features are considered (Fig. 14.1).
Incidental lesion (dashed circle) on breast MRI of a 47-year-old woman performed for other reasons. Slow initial (a) and persistent late (b) enhancement, coded green on a parametric enhancement map (c). The lesion has a hyperintense and circumscribed T2w correlate (d) and shows high signal on the DWI image (e) and on the apparent diffusion coefficient (ADC) map (f). The quantitative ADC value was measured as 1.8 × 10−3 mm2/s. This finding fulfills all the criteria for a benign lesion and should rather be called BI-RADS 2 (benign finding) than BI-RADS 3 (probably benign finding). MR-directed ultrasound should be attempted in order to have documented the lesion for subsequent conventional screening rounds
Fibroadenomata, the most common benign lesions in the breast, usually show a circumscribed T2w correlate and high diffusivity on Apparent Diffusion Coefficient (ADC) maps [22]. The latter constitutes the juvenile myxoid or fluid-rich fibroadenoma type. These lesions can even show wash-out curve types, but the combination of high ADC and circumscribed margins excludes the only malignant lesion with high ADC values: invasive mucinous cancer. Fibroadenomata do mature, leading to a loss of water content and an increased hypovascularized stroma component over time. This loss of water may even cause low ADC values that are due to the low T2- signal rather than a real diffusion restriction. Although Schrading et al. have coined the term of fibroadenoma-like appearing cancers in high-risk patients [23], others have not confirmed this finding, and the authors’ conclusions are likely due to the reading method applied at that time (alternator views on printed films, visual assessment of signal intensity time curves). In our own clinical experience, we have never encountered a cancer lacking all three MRI hallmarks of malignancy: non-circumscribed or spiculated margins, plateau or wash-out curve types and restricted diffusivity. Moreover, basic consideration of tumor biology implies that dangerous, fast growing tumors may appear with circumscribed margins but their fast growth requires strong and typical hypervascularization and restricted diffusivity due to high cellularity. Again, the combination of circumscribed margins with low and persistent contrast medium uptake excludes any malignant diagnosis: invasive cancer is either not circumscribed or, if circumscribed, presents a highly proliferative lesion that will always show strong contrast uptake followed by wash-out or plateau curves.
The MRI BI-RADS lexicon is characterized by the lack of a clinical decision rule—a precise description of which diagnostic criteria constitute a specific diagnosis, e.g. BI-RADS 3. Although there are several classification systems in breast MRI, such as the Göttingen score [24] or the Jena Tree [25, 26], these systems do not provide rules to differentiate between benign and probably benign lesions. However, they assign levels of suspicion to specific feature combinations, allowing the user to assess whether a lesion is benign or whether the lesion is still benign but may need further follow-up. Still, the decision to differentiate between benign and probably benign lesions is largely a decision based on the clinical background, including patient age, individual breast cancer risk and prior imaging findings. That said, we can conclude the following: first, a lesion that is already known and does not show any imaging progression over time should generally not be assigned as BI-RADS 3 on MRI. Second, a newly diagnosed lesion should not be called BI-RADS 3 if unambiguous benign imaging features are present. This does also hold true for the high-risk screening situation. Here, many authors and colleagues prefer immediate biopsy of newly diagnosed lesions. However, considering the variety of MR imaging protocols and their sensitivity for contrast media, new or stronger enhancing lesions may show such characteristics either due to protocol differences or the cyclical physiologic enhancement in premenopausal women.
The clinical indication for the breast MRI should also be considered in evaluation of BIRADS 3 lesions. If a patient is referred to MRI, e.g., due to an asymmetric density in mammography without remarkable findings on ultrasound, the pretest probability for breast cancer is very low and the indication for the examination questionable. If an incidental lesion, that is a lesion not corresponding to the mammographic asymmetry, shows only benign characteristics, the likelihood of malignancy is negligible, and the lesion should be termed benign and not probably benign. The high sensitivity of MRI implies that many lesions detected by MRI may have been already present but were not seen on conventional imaging.
However, lesions identified on MRI’s performed for preoperative staging in breast cancer should be considered differently than those found on MRI’s performed for other indications. Here, breast MRI may identify additional lesions, a substantial number of them malignant [27]. DCIS components, in particular, may cause subtle enhancements of non-mass character, lacking the typical features of malignancy [22]. In this setting, a BI-RADS 3 category should be restricted to findings that show benign features only. It is our clinical practice to perform biopsy on all enhancing lesions in cancer patients when typical feature combinations of benign lesions (such as fibroadenoma) are lacking, if that particular lesion would potentially change patient management. Our interdisciplinary communication in these cases has led to a very low number of BI-RADS 3 findings in preoperative cancer staging MRIs, as definite diagnoses are warranted in this setting. A BI-RADS 3 categorization is of little use in the setting of newly diagnosed cancer both in ipsilateral and contralateral breast. Short-interval follow-up for patients who will undergo breast cancer treatment is of little clinical use. If a lesion resolves during short-interval follow-up on a breast cancer patient receiving therapy (e.g. chemotherapy, hormonal therapy), it will remain unclear whether this lesion represented successfully treated breast cancer or suppressed benign proliferative activity.
2.2 BI-RADS 3 Masses on MRI
The literature reports 10 out of 564 masses classified as BI-RADS 3 with a final diagnosis of malignancy (1.8 %) [5, 11–13, 16–19]. These studies did not perform dedicated comparisons of feature combinations in benign and malignant lesions, thus, an evidence based recommendation on which specific criteria in masses should lead to a BI-RADS 3 categorization cannot be given. As discussed above, a mass lesion presenting with benign imaging criteria should not be called BI-RADS 3 but rather BI-RADS 2. A mass is a three-dimensional lesion that occupies a space within the breast. A mass should be evaluated by its shape, its margins and its internal characteristics (T1-weighted and T2-weighted characteristics and kinetic behavior, ADC if available). Further evaluations for a mass seen on MRI include a comparison to other breast imaging methods, previous MRIs, clinical history and breast cancer risk. Prior investigations have shown that masses with irregular shapes and those with irregular or spiculated borders have the highest likelihood of malignancy [15, 28–30]. This has also been supported by a study that revealed that the single most predictive imaging feature for malignancy was the margin [31]. Therefore, masses with irregular shape or irregular margins should not be assessed as probably benign. The arguably most important diagnostic criteria in mass lesions are margins, enhancement curve type, T2-weighted correlate and ADC values. Circumscribed margins, slow and persistent enhancement and high ADC values practically exclude cancer in mass lesions. Low ADC values and wash-out curves may be seen in benign fibroadenoma lesions; however, these findings do not present simultaneously in an individual fibroadenoma. A juvenile fibroadenoma is usually highly vascularized and demonstrates a high water content, thus presenting with wash-out and high ADC values whereas a fibroadenoma in an elderly woman presents with slow and persistent enhancement and mixed high, intermediate or even low ADC values. Non-circumscribed margins and rim enhancement are atypical in benign mass lesions and should not be assessed as BI-RADS 3 but rather categorized BI-RADS 4 [22, 24–26, 28, 29, 31]. An example of a BI-RADS 3 mass lesion is given in Fig. 14.2.
Example of a BI-RADS 3 mass lesion in a 43-year-old woman. Initial examination appears on the left side (denoted by 1), final follow-up examination after 24 months on the right side (denoted by 2). The lesion initially [1] presented with non-circumscribed margins, and was rather homogeneous with slow initial (a) and persistent delayed (b) enhancement. A non-circumscribed dark T2w correlate (c) disturbs the benign impression, while the ADC map (d) showed high ADC values of 1.6 × 10−3 mm2/s. Due to the ambiguous, but predominantly benign findings, a BI-RADS 3 rating was assigned. Follow-up examination [2] gave a stable impression; however, lesion contrast was higher due to a modernized protocol, revealing heterogeneous internal enhancement. The lowest ADC value inside the lesion was 1.4 × 10−3 mm2/s, and the lesion was subsequently downgraded to BI-RADS 2. Due to cosmetic reasons, the patient underwent plastic surgery of both breasts and the lesion was removed after wire localization. Histopathology revealed a fibroadenoma with regressive changes
2.3 BI-RADS 3 Foci on MRI
Foci classified BI-RADS 3 have the lowest probability of malignancy in all BI-RADS 3 lesions. The literature lists 5 malignant foci out of 518 BI-RADS 3 foci (0.9 %) [11, 12, 16, 17, 19]. Similar to reports on BI-RADS 3 masses, no dedicated feature combinations that should lead to a BI-RADS 3 categorization in foci can be extracted from the literature. A focus (foci) is an enhancing area of less than 5 mm in diameter and is not space-occupying like a mass. Although, foci are traditionally considered to be too small to allow evaluation of margins or internal enhancement, the possibility of applying morphologic and dynamic features in foci for diagnostic purposes has been demonstrated [32].
Foci have been described as comprising up to 48 % of MRI BI-RADS 3 lesions [11, 17]. On the other hand, the likelihood for malignancy in foci is rather low as they are regularly part of normal background parenchymal enhancement. In a histologically verified series, suspicious foci detected on MRI had a 3 % (1/37) frequency of malignancy [33]. One study evaluating foci on follow-up reported that a single BI-RADS 3 focus (1.5 %, 1/67) with 4 mm (on baseline examination) increased to 7 mm on follow-up MRI and biopsy revealed a DCIS [17]. Similarly, another study identified a single focus (0.6 %, 1/168) with wash-out kinetics increasing in size on follow-up MRI. Again MRI-guided biopsy revealed a DCIS [11].
A high malignancy rate of 21 % (14/68) was seen in a series of suspicious small masses (<5 mm) [34]. All lesions remained undetected by MRI-directed ultrasound, appeared to be suspicious (BI-RADS 4 equivalent) and thus underwent MR-guided biopsy. A final diagnosis of malignancy was associated with recently diagnosed breast cancer and in this case, malignant foci were usually found in the same quadrant [34].
Data suggest that the absence of a high T2 signal and increased size are the most predictive features for malignancy [32, 35]. Importantly, foci presenting with persistent enhancement kinetics are usually benign and might be safely classified as BI-RADS 2 [11, 32, 36]. Finally, the distribution of foci is essential: multiple diffuse bilateral foci should not be considered probably benign but rather benign (BI-RADS 2), as they represent a variation of normal background parenchymal enhancement [1]. Such findings are regularly seen in perimenopausal women. A focus with wash-out harbors a significant risk of malignancy and should thus be categorized BI-RADS 4 instead of BI-RADS 3 [32, 34]. An example of a BI-RADS 3 focus is given in Fig. 14.3.
BI-RADS 3 focus in a 41-year-old patient. On the baseline scan (left hand, 1), the focus demonstrated an intermediate initial (a) enhancement followed by washout (b). T2w (c) showed a hyperintense correlate with circumscribed margins. The follow-up examination after 12 months (right hand, 2) did not show any change in morphology and kinetics. Note the modernized dynamic enhanced protocol, allowing a better depiction of lesion characteristics
2.4 BI-RADS 3 Non Mass Enhancement on MRI
As opposed to mass lesions, non-mass enhancement (NME) or non-mass lesions are not space-occupying. NME categorized BI-RADS 3 have the highest probability of malignancy in all BI-RADS 3 lesions. The literature reports on 19 out of 467 BI-RADS 3 NME that were finally malignant (4 %) [5, 11–13, 16–19]. Again, no dedicated feature combinations that should lead to a BI-RADS 3 categorization in NME can be extracted from the literature. NME lesions are evaluated by their distribution, enhancement pattern and enhancement kinetics. Diagnostic BI-RADS criteria in non-mass lesions are limited [28, 29]. However, studies have demonstrated that linear and segmental NME have been most predictive for malignancy [15, 37].
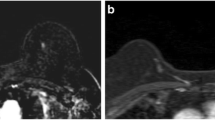
Data on BI-RADS 3 NME on MRI are limited. One study reported that BI-RADS 3 may be assigned if the NME is either focal or regional in distribution and homogeneous enhancement and benign enhancment kinetics (persistent type I or plateau type II curves) [18]. Regional, multiple regions, and diffuse distribution patterns have demonstrated the lowest frequency of malignancy [15]. Another study revealed that eight (8.4 %, 8/95) BI-RADS 3 NME were malignant. All of these NME were heterogeneous or clumped or showed wash-out kinetics [19]. Thus, BI-RADS 3 NME on MRI may be appropriately assigned for focal/regional homogeneous or slightly heterogeneous NME that does not show any suspicious features on baseline MRI (Fig. 14.4). Especially the presence of clumped and segmental or linear enhancement in non-mass lesions should be a reason to categorize these lesions as BI-RADS 4 [19, 22, 37].
Example of a BI-RADS 3 non-mass lesion (dashed circle): a 44-year-old woman who presented with an incidental regional heterogeneous non-mass enhancement with intermediate initial enhancement (a 1 ) and a persistent signal increase in the delayed phase (b 1 ). Non-specific dark T2w correlate with small cysts (c 1); ADC map correlate resembles normal breast parenchyma (d1). Follow-up examination after 6 months (right side, 2) reveals no residual enhancement
2.5 Variations of Background Parenchymal Enhancement
The MRI BI-RADS lexicon term “background parenchymal enhancement” (BPE) is a generalized term for all physiologic enhancements in the breast [1]. Such enhancements comprise regional as well as focal enhancements if they are bilateral and symmetric. In clinical practice, symmetry is not perfect: breasts show slight differences in size, as well as the amount of fibroglandular tissue, cysts, and BPE. Asymmetric focal or patchy BPE often correspond to an ipsilaterally increased amount of cysts and should thus easily be identified. In addition to individual side differences, asymmetric background enhancement can be caused by prior invasive procedures (vacuum-assisted biopsy, open surgery), inflammations and post-radiotherapeutic changes. Radiotherapy has a varying effect immediately after radiation dose delivery but does finally lead to a complete loss of any BPE on the treated side, possibly aggravating a BPE consisting of multiple foci on the contralateral side. If the BPE is clearly asymmetric, and not associated with features of malignancy or pathological findings on conventional imaging, this finding may be called BI-RADS 3 and MRI follow-up may appropriately be initiated.
3 Summary/Conclusion
Probably benign (BI-RADS 3) lesions on MRI are an empirically assigned category that lack specific criteria that could be used for an objective diagnosis. That said, rates of BI-RADS 3 ratings will shift towards BI-RADS 2 with reader experience. The rate of malignancy in BI-RADS 3 lesions is below 2 % in the majority of studies. Malignant BI-RADS 3 lesions may be diagnosed by immediate MR-directed ultrasound or a single MRI follow-up in six to 12 months (if a lesion is not visible by MR-directed ultrasound or MR-directed ultrasound was not performed), supporting the recommendation of these two management approaches.
References
American College of Radiology. Breast imaging reporting and data system (BI-RADS). 5th ed. Reston: American College of Radiology; 2013.
Sickles EA. Probably benign breast lesions: when should follow-up be recommended and what is the optimal follow-up protocol? Radiology. 1999;213(1):11–4.
American College of Radiology. American College of Radiology. ACR practice guideline for the performance of contrast-enhanced Magnetic Resonance Imaging (MRI) of the breast. [Internet]. [cited 2016 Feb 1]. http://www.acr.org/~/media/2A0EB28EB59041E2825179AFB72EF624.pdf.
Kuhl CK, Schmutzler RK, Leutner CC, Kempe A, Wardelmann E, Hocke A, et al. Breast MR imaging screening in 192 women proved or suspected to be carriers of a breast cancer susceptibility gene: preliminary results. Radiology. 2000;215(1):267–79.
Liberman L, Morris EA, Benton CL, Abramson AF, Dershaw DD. Probably benign lesions at breast magnetic resonance imaging: preliminary experience in high-risk women. Cancer. 2003;98(2):377–88.
Hartman A-R, Daniel BL, Kurian AW, Mills MA, Nowels KW, Dirbas FM, et al. Breast magnetic resonance image screening and ductal lavage in women at high genetic risk for breast carcinoma. Cancer. 2004;100(3):479–89.
Kriege M, Brekelmans CTM, Boetes C, Besnard PE, Zonderland HM, Obdeijn IM, et al. Efficacy of MRI and mammography for breast-cancer screening in women with a familial or genetic predisposition. N Engl J Med. 2004;351(5):427–37.
Sadowski EA, Kelcz F. Frequency of malignancy in lesions classified as probably benign after dynamic contrast-enhanced breast MRI examination. J Magn Reson Imaging JMRI. 2005;21(5):556–64.
Kuhl CK, Schrading S, Leutner CC, Morakkabati-Spitz N, Wardelmann E, Fimmers R, et al. Mammography, breast ultrasound, and magnetic resonance imaging for surveillance of women at high familial risk for breast cancer. J Clin Oncol Off J Am Soc Clin Oncol. 2005;23(33):8469–76.
Eby PR, Demartini WB, Peacock S, Rosen EL, Lauro B, Lehman CD. Cancer yield of probably benign breast MR examinations. J Magn Reson Imaging JMRI. 2007;26(4):950–5.
Eby PR, DeMartini WB, Gutierrez RL, Saini MH, Peacock S, Lehman CD. Characteristics of probably benign breast MRI lesions. AJR Am J Roentgenol. 2009;193(3):861–7.
Weinstein SP, Hanna LG, Gatsonis C, Schnall MD, Rosen MA, Lehman CD. Frequency of malignancy seen in probably benign lesions at contrast-enhanced breast MR imaging: findings from ACRIN 6667. Radiology. 2010;255(3):731–7.
Hauth E, Umutlu L, Kümmel S, Kimmig R, Forsting M. Follow-up of probably benign lesions (BI-RADS 3 category) in breast MR imaging. Breast J. 2010;16(3):297–304.
Marshall AL, Domchek SM, Weinstein SP. Follow-up frequency and compliance in women with probably benign findings on breast magnetic resonance imaging. Acad Radiol. 2012;19(4):406–11.
Mahoney MC, Gatsonis C, Hanna L, DeMartini WB, Lehman C. Positive predictive value of BI-RADS MR imaging. Radiology. 2012;264(1):51–8.
Lourenco AP, Chung MTM, Mainiero MB. Probably benign breast MRI lesions: frequency, lesion type, and rate of malignancy. J Magn Reson Imaging JMRI. 2014;39(4):789–94.
Bahrs SD, Baur A, Hattermann V, Hahn M, Vogel U, Claussen CD, et al. BI-RADS® 3 lesions at contrast-enhanced breast MRI: is an initial short-interval follow-up necessary? Acta Radiol Stockh Swed. 1987. 2014;55(3):260–5.
Spick C, Szolar DHM, Baltzer PA, Tillich M, Reittner P, Preidler KW, et al. Rate of malignancy in MRI-detected probably benign (BI-RADS 3) lesions. AJR Am J Roentgenol. 2014;202(3):684–9.
Grimm LJ, Anderson AL, Baker JA, Johnson KS, Walsh R, Yoon SC, et al. Frequency of malignancy and imaging characteristics of probably benign lesions seen at breast MRI. AJR Am J Roentgenol. 2015;205(2):442–7.
Guillaume R, Taieb S, Ceugnart L, Deken-Delannoy V, Faye N. BIRADS 3 MRI lesions: was the initial score appropriate and what is the value of the blooming sign as an additional parameter to better characterize these lesions? Eur J Radiol. 2016;85(2):337–45.
Spick C, Baltzer PAT. Diagnostic utility of second-look US for breast lesions identified at MR imaging: systematic review and meta-analysis. Radiology. 2014;273(2):401–9.
Kaiser WA. Signs in MR-Mammography [Internet]. Berlin, Heidelberg: Springer Berlin Heidelberg; 2008. [cited 2015 Mar 17]. http://www.springer.com/us/book/9783540732921.
Schrading S, Kuhl CK. Mammographic, US, and MR imaging phenotypes of familial breast cancer. Radiology. 2008;246(1):58–70.
Baum F, Fischer U, Vosshenrich R, Grabbe E. Classification of hypervascularized lesions in CE MR imaging of the breast. Eur Radiol. 2002;12(5):1087–92.
Marino MA, Clauser P, Woitek R, Wengert GJ, Kapetas P, Bernathova M, et al. A simple scoring system for breast MRI interpretation: does it compensate for reader experience?. Eur Radiol. 2016;26(8):2529–37.
Baltzer PAT, Dietzel M, Kaiser WA. A simple and robust classification tree for differentiation between benign and malignant lesions in MR-mammography. Eur Radiol. 2013;23(8):2051–60.
Houssami N, Ciatto S, Macaskill P, Lord SJ, Warren RM, Dixon JM, et al. Accuracy and surgical impact of magnetic resonance imaging in breast cancer staging: systematic review and meta-analysis in detection of multifocal and multicentric cancer. J Clin Oncol Off J Am Soc Clin Oncol. 2008;26(19):3248–58.
Baltzer PAT, Benndorf M, Dietzel M, Gajda M, Runnebaum IB, Kaiser WA. False-positive findings at contrast-enhanced breast MRI: a BI-RADS descriptor study. AJR Am J Roentgenol. 2010 Jun;194(6):1658–63.
Gutierrez RL, DeMartini WB, Eby PR, Kurland BF, Peacock S, Lehman CD. BI-RADS lesion characteristics predict likelihood of malignancy in breast MRI for masses but not for nonmasslike enhancement. AJR Am J Roentgenol. 2009;193(4):994–1000.
Lehman CD, Gatsonis C, Kuhl CK, Hendrick RE, Pisano ED, Hanna L, et al. MRI evaluation of the contralateral breast in women with recently diagnosed breast cancer. N Engl J Med. 2007;356(13):1295–303.
Schnall MD, Blume J, Bluemke DA, DeAngelis GA, DeBruhl N, Harms S, et al. Diagnostic architectural and dynamic features at breast MR imaging: multicenter study. Radiology. 2006;238(1):42–53.
Dietzel M, Baltzer PA, Vag T, Gröschel T, Gajda M, Camara O, et al. Differential diagnosis of breast lesions 5 mm or less: is there a role for magnetic resonance imaging? J Comput Assist Tomogr. 2010;34(3):456–64.
Liberman L, Mason G, Morris EA, Dershaw DD. Does size matter? Positive predictive value of MRI-detected breast lesions as a function of lesion size. AJR Am J Roentgenol. 2006;186(2):426–30.
Raza S, Sekar M, Ong EMW, Birdwell RL. Small masses on breast MR: is biopsy necessary? Acad Radiol. 2012;19:412–9.
Ha R, Sung J, Lee C, Comstock C, Wynn R, Morris E. Characteristics and outcome of enhancing foci followed on breast MRI with management implications. Clin Radiol. 2014;69(7):715–20.
Spick C, Szolar DHM, Tillich M, Reittner P, Preidler KW, Baltzer PA. Benign (BI-RADS 2) lesions in breast MRI. Clin Radiol. 2015;70:395–9.
Liberman L, Morris EA, Dershaw DD, Abramson AF, Tan LK. Ductal enhancement on MR imaging of the breast. AJR Am J Roentgenol. 2003 Aug;181(2):519–25.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Baltzer, P.A., Spick, C. (2017). BI-RADS 3 Lesions on MRI. In: Heller, S., Moy, L. (eds) Breast Oncology: Techniques, Indications, and Interpretation. Springer, Cham. https://doi.org/10.1007/978-3-319-42563-4_14
Download citation
DOI: https://doi.org/10.1007/978-3-319-42563-4_14
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-42561-0
Online ISBN: 978-3-319-42563-4
eBook Packages: MedicineMedicine (R0)