Abstract
Francisella tularensis is a facultative intracellular bacterium causing tularemia, a zoonotic disease. Francisella replicates in the macrophage cytosol and eventually triggers cytosolic immune responses. In murine macrophages, Francisella novicida and Francisella tularensis live vaccine strain lyse in the host cytosol and activate the cytosolic DNA receptor Aim2. Here, we review the mechanisms leading or contributing to Aim2 inflammasome activation, including the role of TLRs and of IFN signaling and the implication of the guanylate-binding proteins 2 and 5 in triggering cytosolic bacteriolysis. Furthermore, we present how this cytosolic Gram-negative bacterium escapes recognition by caspase-11 but can trigger a non-canonical caspase-8 inflammasome. In addition, we highlight the differences in inflammasome activation in murine and human cells with pyrin, NLRP3, and AIM2 involved in sensing Francisella in human phagocytes. From a bacterial prospective, we describe the hiding strategy of Francisella to escape recognition by innate sensors and to resist to bacteriolysis in the host cytosol. Finally, we discuss the inability of the inflammasome sensors to detect F. tularensis subspecies tularensis strains, making them highly pathogenic stealth microbes.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
1.1 The Francisella Genus
Francisella is the only genus within the Francisellaceae family (McLendon et al. 2006). These gamma-proteobacteria from the Thiotrichales order are small and pleiomorphic Gram-negative bacteria. The Francisella genus is divided into several species including Francisella tularensis and Francisella novicida (Table 1). Francisella tularensis is the most pathogenic species for humans. Yet, the virulence of F. tularensis strains is highly dependent on the subspecies they belong to. F. tularensis subspecies tularensis (also named type A strains) and its representative strain SCHU S4 are highly infectious and highly virulent with a lethal dose estimated to be lower than 10 bacteria for humans. F. tularensis subspecies holarctica (type B strains, hereinafter referred to as F. holarctica), although responsible for numerous infections of immunocompetent humans, is slightly less pathogenic. The live vaccine strain (LVS) is a strain derived from a virulent F. holarctica strain through sequential, in vitro passages. Although not licensed for vaccination, F. holarctica LVS is commonly used to study Francisella virulence factors and host immune responses. F. novicida is a species closely related to F. tularensis with greater than 97 % nucleotide identities between the two species (Larsson et al. 2009). F. novicida strains have been isolated from a few human patients, most of them with immune deficits or underlying medical conditions (Kingry and Petersen 2014). Due to its high virulence in mouse models of tularemia and an intracellular life cycle very similar to the one of virulent F. tularensis strains, F. novicida strain U112 is used to study tularemia.
In this review, we will present the modalities of the inflammasome activation upon F. novicida infections and we will discuss the similarities and differences observed between F. novicida, F. holarctica LVS, and the highly virulent F. tularensis type A strains.
1.2 Francisella tularensis, the Agent of Tularemia
Tularemia is a zoonotic disease with no transmission from human to human. Several forms of tularemia are observed depending on F. tularensis route of entry into the human host. Tularemia is associated with flu-like symptoms with high fever and lymphadenopathies. The most common form is the ulceroglandular tularemia following entry of the bacterium through the skin either through the bite of an infected arthropod or after direct contact with an infected animal (Sjostedt 2007). Ulceroglandular tularemia is characterized by a necrotic ulcer at the site of infection and a swollen draining lymph node. Consumption of contaminated food or freshwater leads to oropharyngeal tularemia (Gurcan 2014) with the rapid development of cervical lymphadenopathy. Finally, the most life-threatening disease is respiratory tularemia, which is triggered upon inhalation of F. tularensis. The severity of this infection coupled to high infectivity of F. tularensis has led the Center for Diseases Control to classify F. tularensis as a bioterrorism class A agent.
1.3 Intracellular Life Cycle
F. tularensis is a facultative intracellular pathogen found in vivo mostly in phagocytic cells including macrophages, neutrophils, dendritic cells, and monocytes (Hall et al. 2008). In contrast to other intracellular bacteria such as Salmonella or Shigella, F. tularensis is unable to direct its entry into non-phagocytic cells. F. tularensis thus relies on host phagocytic receptors to invade host cells. F. tularensis uptake by macrophages proceeds through an atypical phagocytosis termed “looping phagocytosis.” Bacterial opsonization and several host receptors are involved in facilitating F. tularensis entry (Clemens et al. 2005; Clemens and Horwitz 2007). The engagement of a specific entry receptor modulates the subsequent pro-inflammatory response including IL-1β release (Dai et al. 2013).
Following uptake, F. tularensis rapidly lyses the phagosome (Golovliov et al. 2003; Clemens et al. 2004; Checroun et al. 2006) to reach the host cytosol. Escape into the host cytosol is dependent on an atypical type VI secretion system (T6SS) encoded in the Francisella Pathogenicity Island (FPI) (Nano et al. 2004; Barker et al. 2009; Broms et al. 2010). While the T6SS is thought to secrete lytic effectors into the host cytosol, the mechanisms underlying vacuolar escape remain to be identified (Broms et al. 2010). Upon reaching the host cytosol, F. tularensis replicates rapidly thanks to a metabolic adaptation allowing bacterial growth in this cellular compartment (Barel and Charbit 2013). Due to the cytosolic localization of Francisella strains, these bacteria are used as a model to study the cytosolic innate immune responses including the inflammasome complex. The vacuolar mutants deleted of the FPI locus, of key FPI genes, or mutated in the master regulator gene mglA (Baron and Nano 1998) are often used in comparison with wild-type strains to discriminate the immune responses elicited in the vacuole/phagosome from the cytosol-specific responses.
2 Overview of the Innate Immune Responses to Francisella Infection
The inflammasome is highly connected with other innate immune pathways (Henry et al. 2007; Cole et al. 2008; Jones and Weiss 2011; Man et al. 2015; Meunier et al. 2015). We will thus briefly review the roles of the Toll-like receptors (TLRs) and of the pathways leading to type I IFN secretion during Francisella infection.
2.1 TLRs and NF-κB Activation
Bacteria from the Francisellaceae family are Gram-negative bacteria harboring lipopolysaccharide (LPS) on the external leaflet of their outer membrane. It was noted early on that, in contrast to the typical Enterobacteriaceae LPS, Francisella LPS does not have any endotoxin properties and is unable to induce IL-1 in human monocytes (Sandstrom et al. 1992). Indeed, Francisella LPS is not recognized by TLR4 (Hajjar et al. 2006). This lack of recognition is due to three peculiar features of Francisella lipid A. First, while most Gram-negative bacteria have hexa-acylated LPS, Francisella lipid A is tetra-acylated. Second, the four fatty acyl chains are made of a chain of 16–18 carbons in length as opposed to 12–14 for Escherichia coli lipid A (Gunn and Ernst 2007; Kanistanon et al. 2008). Third, the carbon in position 4′ of the glucosamine is lacking the typical phosphate group observed in most Gram-negative lipid A (Wang et al. 2007).
TLR2 is thus the main pattern recognition receptor (PRR) responsible for transcription factor NF-κB activation during Francisella infection (Katz et al. 2006; Li et al. 2006). TLR2 activation occurs through the recognition of bacterial lipoproteins (Thakran et al. 2008) and is observed both at the plasma membrane and in the phagosome before Francisella escapes into the host cytosol (Cole et al. 2010).
2.2 Signaling Pathways Leading to Type I IFN Production
In addition to the pro-inflammatory response triggered at the plasma membrane or in the phagosome, escape of Francisella into the host cytosol triggers the “cytosolic innate immune responses.” Henry et al. studied these responses by comparing the transcriptional responses of bone marrow-derived macrophages (BMDMs) infected with either the cytosolic wild-type F. novicida strain (U112) or a vacuolar mutant (ΔFPI). They demonstrated that macrophages detecting Francisella specifically in the cytosol secrete type I interferon (IFN-α and IFN-β) (Henry et al. 2007). Cole et al. confirmed this finding using F. holarctica LVS (Cole et al. 2008). In agreement with the cytosolic localization required to trigger IFN-β secretion, the type I IFN response upon F. novicida infection is independent of TLR2 and of the TLR adaptors MyD88 and TRIF (Henry et al. 2007; Jones and Weiss 2011). Type I IFN induction during Francisella infection is dependent on STING (Jones et al. 2010; Jin et al. 2011) and could be recapitulated by transfecting into the host cytosol of a proteinase K-resistant, DNase1-sensitive factor contained in a Francisella extract (Jones et al. 2010). The cytosolic DNA sensor cyclic GMP-AMP synthase (cGAS) is required for type I IFN production in response to F. novicida infection (Storek et al. 2015; Man et al. 2015). In addition to cGAS, Storek et al. demonstrated that in infected BMDMs, the DNA sensor Ifi204 (the murine homologue of human IFI16) is required to induce IFN-β production. The respective roles of the cGAS and Ifi204 remain unknown (Storek et al. 2015). Altogether, the results demonstrate that detection of F. novicida DNA in the host cytosol by the synergistic action of two DNA sensors triggers type I IFN secretion. Downstream of the DNA sensors, STING contributes to activate the transcription factors IRF1 and 3 (Henry et al. 2007; Jin et al. 2011; Man et al. 2015) to induce IFN-β and expression of numerous interferon-stimulated genes (ISGs) (Fig. 1).
The pathway leading to type I IFN secretion upon F. holarctica LVS infection might be slightly different. Indeed, type I IFN secretion is neither observed in Sting −/− BMDMs (Jin et al. 2011) nor in Tlr2 −/− BMDMs (Cole et al. 2007). At the present time, it remains unclear whether TLR2 is directly involved in type I IFN response upon F. holarctica LVS infection, possibly through the MyD88-IRF1-IRF7 pathways elicited in the endosomal compartment (Dietrich et al. 2010) or whether TLR2 is required upstream of the release of LVS DNA into the host cytosol to elicit the cGAS/Ifi204-STING pathway.
3 Francisella Activates the Aim2 Inflammasome in Murine Phagocytes
Most of the published work on the modalities of inflammasome activation during Francisella infection has been performed in murine macrophages using F. novicida or F. holarctica LVS. First, we will describe activation of the inflammasome in mice and in murine phagocytes upon F. novicida and F. holarctica LVS infections (Fig. 1). In a second time, we will highlight the similarities and differences between human and murine cells and between F. novicida, F. holarctica LVS, and the highly pathogenic F. tularensis subsp. tularensis strains.
3.1 Aim2 Inflammasome and the IFN Requirement
3.1.1 In Vitro and In Vivo Role of the Inflammasome
The role of the inflammasome was demonstrated early on by Monack and colleagues (Mariathasan et al. 2005). In 2005, Mariathasan et al. described a cell death response that was dependent on both ASC and caspase-1 as well as on the cytosolic localization of F. novicida in BMDMs. This cell death is associated with caspase-1 processing, IL-1β, and IL-18 release. As expected, TNF-α release (which levels are regulated by NF-κB) is independent of both ASC and caspase-1. The in vitro results were validated in a mouse model of tularemia. Mariathasan et al. demonstrated that ASC and caspase-1 are required for the survival of the mice to F. novicida infection while Nlrc4 (known at the time as IPAF) is not. Indeed, when 1.5 × 105 F. novicida colony-forming units (CFU) were injected subcutaneously, 100 % of Asc −/− and Casp1 −/− mice died within 3–5 days. In contrast, with the same inoculum, 25 % of the wild-type mice survived the infection (Mariathasan et al. 2005). Cells expressing active caspase-1 are detected in the liver, in the spleen of LVS-infected mice (Wickstrum et al. 2009), and in the lung of F. novicida-infected mice (Mares et al. 2008). In agreement with the key role of the inflammasome pathway in these organs, F. novicida burden at 2 days post-inoculation is 100- to 1000-fold higher in the spleen, liver, and lung of inflammasome-deficient mice than in the corresponding organs of wild-type mice (Mariathasan et al. 2005).
Caspase-1-dependent cytokines orchestrate the innate immune response against Francisella. Indeed, IL-18 is key to induce IFN-γ production by NK cells in F. novicida-infected mice (Pierini et al. 2013; del Barrio et al. 2015). Interestingly, the survival of Il-18 −/− mice to LVS infection can be rescued by IFN-γ administration. In contrast, Il-1r1 −/− mice remained highly susceptible to LVS infection even upon IFN-γ administration (del Barrio et al. 2015). Re and colleagues identified that IL-1β is required early during infection to produce anti-LPS IgM (del Barrio et al. 2015). Anti LVS-IglM was observed in the serum of infected wild-type mice 7 days post-infection but were greatly reduced in Asc −/− and Il-1b −/− mice. B1a B cells are responsible for this specific IgM response, and their numbers were reduced in the spleen of infected Il-1b KO mice. This IglM response was demonstrated to be protective likely through opsonization and increased phagocytosis (del Barrio et al. 2015). Finally, caspase-1 inhibition reduces IL-23p19 level (an IL-1β-regulated cytokine controlling IL-17 levels) in LVS-infected macrophages (Skyberg et al. 2013).
Using IL-1β- and IL-18-neutralizing antibodies injections in wild-type mice, Monack and colleagues demonstrated that mature IL-1β and IL-18 are required to fight Francisella infection. However, the susceptibility of caspase-1-deficient mice is due only in part to the lack of these two active cytokines. These results were confirmed by comparing mice doubly deficient for IL-1β and IL-18 (Il-1β/Il-18 DKO) to wild-type and Casp1 −/− mice. Il-1β/Il-18 DKO mice display an intermediate phenotype in terms of bacterial burden in the spleen, liver, and lung between wild-type and Casp1 −/− mice (Henry and Monack 2007). These results led the authors to conclude that the cell death defect in caspase-1-deficient mice was also participating in the strong susceptibility of caspase-1-deficient mice (Mariathasan et al. 2005; Henry and Monack 2007). Similarly to what have been reported for Salmonella typhimurium, Legionella pneumophila, and Burkholderia thailandensis (Miao et al. 2010), pyroptosis is thus a potent innate immune mechanism against Francisella by removing its replicative niche and contributing to the clearance of this pathogen.
Of note, a Fas-mediated apoptotic pathway has been described for macrophages infected with F. novicida (Rajaram et al. 2009) but this pathway was characterized in RAW 264.7 cells, which are deficient for the inflammasome adaptor ASC (Pelegrin et al. 2008). While both apoptotic and pyroptotic pathways may occur during LVS or F. tularensis infections, in primary macrophages infected with F. novicida, the cell death is clearly inflammasome dependent.
3.1.2 Type I IFN Signaling Is Required for Francisella-mediated Inflammasome Activation
This inflammasome response in infected BMDMs was rapidly characterized as Nlrp3 independent (known at the time as cryopyrin) (Mariathasan et al. 2006). The first clue on the potential receptor-sensing Francisella in the cytosol came in 2007 with the demonstration that macrophages deficient in the type I IFN receptor (IFNAR1) were specifically deficient for inflammasome activation in response to Francisella infection (Henry et al. 2007). While the induction of pro-IL-1β protein is similar in wild-type and in Ifnar1 −/− macrophages, secretion of mature IL-1β, IL-18, and caspase-1 processing and cell death are fully deficient in the latter cells. The same phenotype is also observed in Irf3 −/− macrophages, which are deficient for IFN-β production during F. novicida infection. However, addition of rIFN-β to Irf3 −/− macrophages restores inflammasome activation in these cells (Henry et al. 2007). These results were strengthened by the study of cGAS- and STING-deficient BMDMs, which are deficient both for type I IFN induction and inflammasome activation in response to F. novicida infection (Jones et al. 2010; Storek et al. 2015). Altogether, these studies indicate that type I IFN production and signaling are required to trigger inflammasome activation in response to F. novicida infection. In 2007, this finding led Henry et al. (2007) to suggest that the inflammasome receptor-sensing Francisella in the cytosol could be a member of the interferon-stimulated genes (ISGs) family, which includes proteins with pyrin domain.
3.1.3 Aim2 Is the Inflammasome Receptor Detecting Francisella in the Host Cytosol
Absent in melanoma 2 (AIM2) was identified in 2009 as an inflammasome receptor-sensing cytoplasmic DNA (Roberts et al. 2009; Burckstummer et al. 2009; Fernandes-Alnemri et al. 2009; Hornung et al. 2009). Aim2 is an ISG coding a protein with a N-terminal pyrin domain and a C-terminal HIN domain. Through its HIN domain, AIM2, a cytosolic protein, binds double-stranded (ds)DNA. dsDNA is recognized by AIM2 in a sequence-independent manner as the HIN domain binds the dsDNA sugar-phosphate backbone (Jin et al. 2012). A DNA strand of at least 80 bp in length is required upon transfection to trigger IL-1β release. dsDNA in the cytosol may thus act as a scaffold to oligomerize AIM2. The resulting complex in turn recruits ASC oligomers through homotypic interactions of AIM2 and ASC pyrin domains leading to the formation of the active inflammasome complex (Jin et al. 2012).
The role of Aim2 as the Francisella inflammasome receptor was demonstrated independently in 2010 by three groups (the Fitzgerald, Alnemri, and Monack teams) who had generated Aim2 −/− mice (Fernandes-Alnemri et al. 2010; Rathinam et al. 2010; Jones et al. 2010). Among several Aim2-activating pathogens, Fitzgerald and colleagues demonstrated that Aim2 −/− macrophages were deficient for caspase-1 processing and IL-1β release in response to LVS infection (Rathinam et al. 2010). The Alnemri and Monack groups used F. novicida to demonstrate that, even at high multiplicity of infection, Aim2 was required for ASC oligomerization, caspase-1 processing, pro-IL-1β processing, IL-1β release, and macrophage death (Fernandes-Alnemri et al. 2010; Jones et al. 2010). The requirement for Aim2 is highly specific since neither Nlrp3 −/− nor Mefv −/− BMDMs (the latter being deficient in the pyrin receptor) display any deficiency in response to F. novicida infection (Fernandes-Alnemri et al. 2010). In agreement, with the cytosolic localization of AIM2 and with previous studies (Mariathasan et al. 2005; Gavrilin et al. 2006), the vacuole-restricted mutant (ΔFPI) is unable to trigger Aim2 activation. The direct recognition of Francisella DNA by Aim2 was demonstrated by immunofluorescence. Macrophages were infected with F. Novicida pre-labeled with Hoechst, a DNA intercalating dye. Following infection, Aim2 specks or clusters were observed co-localizing with Hoechst-labeled material in close proximity to bacteria. In addition, Aim2 specks co-localize with ASC specks likely corresponding to the mature inflammasome complex. Importantly, Aim2 specks are also observed in ASC-deficient macrophages further demonstrating the role of Aim2 as a receptor upstream of ASC (Fernandes-Alnemri et al. 2010; Jones et al. 2010). Of note, Aim2 is also required in bone marrow-derived dendritic cells (BMDC) to trigger inflammasome activation in response to F. novicida infection (Belhocine and Monack 2012).
Aim2 is also critical for the immune response in vivo in a mouse model of tularemia. As previously reported for Casp1 −/− and Asc −/−, Aim2 −/− mice are highly susceptible to F. novicida infection with 100 % of the mice dying in 5 days as opposed to 30 % of wild-type mice (Fernandes-Alnemri et al. 2010). The fast death is associated with a 100- to 1000-fold increase in the bacterial burden in the spleen, the lung, and the liver and a much lower concentration of IL-18 in the serum of Aim2 −/− mice compared to wild-type mice (Fernandes-Alnemri et al. 2010; Jones et al. 2010). The Aim2 inflammasome is thus a key receptor for the innate immune defense against Francisella.
The discovery of Aim2 as the receptor-sensing Francisella in the host cytosol gave an opportunity to question the role of type I IFN signaling in Aim2 induction and Aim2 inflammasome activation. While Aim2 expression was strongly induced upon Francisella infection in a STING- and type I IFN receptor-dependent manner in experiments performed by Jones and colleagues, Aim2 was not induced during similar experiments performed by Fernandes-Alnemri et al. Interestingly, while several groups confirmed a role for the type I IFN pathway [IRF3/IRF7 (Rathinam et al. 2010); IRF3, IFNAR1 (Fernandes-Alnemri et al. 2010); STING, IFNAR1(Jones et al. 2010)] in potentiating the Aim2 inflammasome, the type I IFN pathway is not required for Aim2 activation following transfection with synthetic DNA (p(dA:dT)) or following transfection with F. novicida genomic DNA (Fernandes-Alnemri et al. 2010; Rathinam et al. 2010; Meunier et al. 2015). This result indicates that the basal level of Aim2 is sufficient to detect cytosolic DNA and suggests that type I IFN and ISGs are required specifically during Francisella infection upstream of the Aim2 inflammasome.
3.2 Gbp-mediated Bacteriolysis Is Required to Trigger Aim2 Inflammasome Activation
One of the key questions regarding the activation of the cGAS/Ifi204 DNA sensor or of the Aim2 inflammasome during F. novicida infection is the source of cytosolic DNA. Indeed, bacterial DNA is normally enclosed within the bacterium and not accessible to cytosolic DNA sensors. During immunostaining experiments, Jones and colleagues had observed that Aim2 specks were localized in proximity to irregular-shaped bacterial remnants (Jones et al. 2010) suggesting that bacteriolysis may be a prerequisite for the release of genomic bacterial DNA into the host cytosol. This observation coupled to the lack of requirement for type I IFN signaling to activate the Aim2 inflammasome in response to synthetic DNA led Meunier et al. (2015) to hypothesize that type I IFN signaling may be involved in the bacteriolysis mechanism. As type I IFN signaling induces hundreds of ISGs in F. novicida-infected macrophages (Henry et al. 2007), they performed a RNA interference screening on 483 ISGs in F. novicida-infected BMDMs. They identified that the knockdown of the genes encoding two guanylate-binding proteins (Gbps): Gbp2 and Gbp5 strongly reduced Aim2 inflammasome activation upon F. novicida infection (Meunier et al. 2015). At the meantime, Kanneganti and colleagues demonstrated that in addition to IFNAR1, IFNAR2, Stat1, and IRF9, the IFN-inducible transcription factor IRF1 was required for F. novicida-mediated Aim2 inflammasome activation (Man et al. 2015). IRF1 regulates IFN-β induction during F. novicida infection. However, Man et al. demonstrated that the addition of IFN-β in Irf1 −/− BMDM does not rescue Aim2 inflammasome activation during F. novicida infection. This result suggested that IRF1 action is required downstream of the IFNAR receptor to induce one of several specific ISGs. Using a gene expression profiling approach, Man and colleagues identified Gbps as a family of protein strongly up-regulated by IRF1 and IFNAR1 in F. novicida-infected macrophages. A subsequent siRNA screen on the Gbp family confirmed Gbp2 and Gbp5 as two specific Gbps required for Aim2 inflammasome activation in response to F. novicida infection (Man et al. 2015).
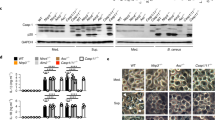
Gbps are interferon-inducible, dynamin-like GTPases involved in cell-autonomous immunity. They may act as scaffolding proteins to target antimicrobial proteins such as the NADPH oxidase, autophagic proteins, and the IFN-γ-inducible GTPase p47 to membrane-bound intracellular pathogens (Meunier and Broz 2016). In addition, Gbp5 directly binds NLRP3 and may promote NLRP3 inflammasome assembly in response to pathogenic bacteria and to ATP and Nigericin (Shenoy et al. 2012) although the latter observation is controversial (Meunier et al. 2014). In addition, Gbps contribute to caspase-11 activation following infection with Salmonella typhimurium (Meunier et al. 2014) and Legionella pneumophila (Pilla et al. 2014). The mechanisms controlling the enhanced activation of this non-canonical inflammasome are still unclear with three mechanisms proposed. (1) Gbps could favor the disruption of pathogen-containing vacuole, thus enhancing the release of the bacteria into the host cytosol (Meunier et al. 2014). (2) Gbps could act downstream of the release of the bacteria into the host cytosol (Pilla et al. 2014) by targeting cytosolic bacteria and triggering the shedding of LPS into the cytosol. (3) Gbps could directly act onto the non-canonical caspase-11 complex to promote its multimerization (Finethy et al. 2015). Eleven Gbp genes (and two Gbp pseudogenes) are present in two clusters on mouse chromosomes 3 and 5. Several of the chromosome 3-encoded Gbps control bacterial (Kim et al. 2011) and parasitic replication (Yamamoto et al. 2012; Degrandi et al. 2013). Using BMDMs from Gbp5 −/− and Gbp2 −/− mice and from mice deficient for the cluster of Gbps (Gbp1, Gbp2, Gbp3, Gbp5, and Gbp7) present on the chromosome 3 (Gbp chr3), Meunier et al. and Man et al. confirmed that Gbps and particularly Gbp2 and Gbp5 are required for Aim2 inflammasome activation during F. novicida infection. Indeed, Gbp chr3 macrophages secrete lower levels of IL-1β and IL-18 than wild-type macrophages during the infection. Similarly, Gbp chr3 macrophages are largely resistant to Francisella-induced pyroptosis. Since Gbps are known to target pathogen-containing phagosomes/vacuoles and destabilize the integrity of these compartments (Yamamoto et al. 2012; Meunier et al. 2014), Meunier et al. and Man et al. hypothesized that Gbps might attack Francisella-containing phagosomes leading to the release of bacteria into the host cytosol. Yet, there was no difference in the F. novicida escape rate between wild-type and Gbp chr3-deficient macrophages. This result indicates that Gbps act after Francisella escape into the host cytosol strengthening a role of Gbps in triggering cytosolic bacteriolysis.
By confocal microscopy, both Gbp2 and Gbp5 were observed surrounding the bacteria. Interestingly, using GFP-expressing bacteria, Man et al. noticed that bacteria decorated with Gbp5 tend to lose their GFP expression suggesting a loss of viability. Accordingly, a greater number of cytosolic bacteria are permeable to propidium iodide in wild-type macrophages compared to Gbp chr3-deficient macrophages indicating a Gbps-dependent loss of bacterial membrane integrity (Meunier et al. 2015). In addition, Francisella replication is impaired in wild-type macrophages compared to Gbpchr3-deficient and Irf1 −/− BMDMs as shown by CFU assay and by quantification of bacterial loads in single cells using confocal microscopy or high-resolution microscopy in flow. How Gbps trigger bacteriolysis following recruitment onto/on close proximity to cytosolic Francisella is still unclear. Bosio and colleagues have shown that the anti-oxidant N-acetyl cysteine and the mitochondrial-specific reactive oxygen species (ROS) scavenger, mitoTEMPO inhibit F. novicida-mediated inflammasome activation (Crane et al. 2014). ROS can target bacterial lipids and outer membrane proteins (Fang 2004). Mitochondrial ROS may thus participate in the killing of F. novicida inside the host cytosol leading to the release of DNA and Aim2 activation. Yet, the precise role of mitochondrial ROS and their connection with Gbps remain to be deciphered.
The roles of IRF1 and Gbps in inflammasome activation were validated in vivo in a mouse model of tularemia (Man et al. 2015; Meunier et al. 2015). Indeed, after F. novicida intradermal inoculation, both Irf1 −/− and Gbp chr3-deficient mice showed reduced IL-18 concentration in the serum. Furthermore, Irf1 −/−, Gbp2 −/−, and Gbp chr3-deficient mice had a higher bacterial burden in the liver and the spleen than wild-type mice. Finally, in a survival experiment, all Irf1 −/−, Gbp2 −/−, and Gbp chr3-deficient mice died within 4 days of infection, while most wild-type mice survived until the end of the experiment (day 8–10).
Importantly, while Gbps expression is induced by type I IFN, Gbps are also strongly induced by IFN-γ in a manner requiring the transcription factors Stat1 and IRF1 (Briken et al. 1995). In vitro, BMDMs do not produce IFN-γ and the IFN signaling is only due to autocrine and paracrine type I IFN signaling following engagement of the cytosolic DNA sensors. However, in vivo, IFN-γ produced early on by NK cells, T cells, and several different phagocyte populations (Bokhari et al. 2008; De Pascalis et al. 2008; Pierini et al. 2013) is likely to control Gbps induction. Indeed, while IFN-γ signaling is critical in vivo to fight Francisella infection (Anthony et al. 1989; Elkins et al. 1996), type I IFN signaling is deleterious in vivo during infections with several intracellular bacteria including Francisella (Auerbuch et al. 2004; Stanley et al. 2007; Henry et al. 2010).
3.3 TLR2 Controls pro-IL-1β Level and the Kinetics of AIM2 Inflammasome Activation
As previously mentioned, TLR2 is the main TLR responsible for NF-κB activation during Francisella infection (Katz et al. 2006). As such, induction of pro-IL-1β is fully abolished in F. holarctica LVS-infected Tlr2 −/− BMDMs and BMDCs (Li et al. 2006; Cole et al. 2007; Dotson et al. 2013). Upon F. holarctica LVS infection, IFN-β induction is also fully dependent on TLR2 (Cole et al. 2007). During F. novicida infection, TLR2 controls pro-IL-1β level but does not play a significant role in IFN-β induction (Jones and Weiss 2011). In addition, during F. novicida infection, TLR2 signaling modulates inflammasome activation kinetics. Indeed, wild-type macrophages display more ASC specks, secrete more mature caspase-1 and IL-18, and die faster than Tlr2 −/− macrophages (Jones and Weiss 2011). Importantly, the requirement for TLR2 signaling is also observed in vivo since (i) immunostaining with an antibody against active caspase-1 p20 subunit reveals more caspase-1 specks in the spleen of infected wild-type mice than in the spleen of Tlr2 −/− mice; (ii) TLR2-deficient mice present less IL-18 in their serum than wild-type mice do (Jones and Weiss 2011). While differences exist between LVS- and F. novicida-infected macrophages, these studies clearly demonstrate that TLR2 is required for full inflammasome activation during Francisella infection. Besides the role of TLR2 on IFN-β induction observed during LVS infection, the contributions of TLR2 to the induction of mitochondrial ROS (West et al. 2011), to Gbps-induced bacteriolysis, or to a possible priming of the Aim2 inflammasome remain to be evaluated.
4 Francisella and the Non-canonical Inflammasomes
4.1 Francisella LPS Escapes Caspase-11 Recognition
The presence of LPS inside the cytosol is detected by caspase-11 (Kayagaki et al. 2013; Hagar et al. 2013; Shi et al. 2014) leading to activation of this inflammatory caspase in a complex termed a non-canonical inflammasome (Kayagaki et al. 2013). The caspase-11 inflammasome is thus a molecular sentinel monitoring the cytosol for the presence of Gram-negative bacteria (Aachoui et al. 2013). As a Gram-negative bacterium replicating in the cytosol, Francisella was thus a likely pathogen to activate caspase-11. Although the expression of caspase-11, an IFN-inducible gene, is induced upon F. novicida infection (Akhter et al. 2012), F. novicida does not activate caspase-11 (Hagar et al. 2013). Miao and colleagues identified that F. novicida-mediated evasion from caspase-11 recognition is associated with its specific lipid A structure (Hagar et al. 2013). Indeed, as previously described, Francisella LPS is tetra-acylated while LPS from most Gram-negative bacteria are hexa-acylated (Okan and Kasper 2013). LpxF is a periplasmic phosphatase, which specifically removes the 4′ monophosphate group in the lipid A. Raetz and collaborators have observed that the presence of the 4′ monophosphate group in the lipid A of the lpxF mutant impairs the cleavage of the 3′ acyl chain. The lack of the LpxF enzyme thus results in the generation of a penta-acylated lipid A (Wang et al. 2007). Strikingly, while purified tetra-acylated LPS from F. novicida does not activate caspase-11, purified penta-acylated LPS from lpxF mutant does so (Hagar et al. 2013). This result highlights LpxF as a key enzyme to escape caspase-11 recognition. However, the lpxF mutant is also severely impaired for growth in axenic medium and for resistance to antimicrobial peptides indicating that this enzyme is also required for membrane integrity and the general fitness of the bacterium (Wang et al. 2007). Of note, LPS from the lpxF mutant does not activate TLR4 (Wang et al. 2007) while it does activate caspase-11 in the cytosol indicating that TLR4 and caspase-11 pathways have different structural requirements (Hagar et al. 2013).
4.2 ASC-dependent Caspase-1-independent Pathways
While the canonical inflammasome is defined by caspase-1 activation, Mariathasan et al. (2005) observed early on that, upon F. novicida infection, the kinetics of cell death differed between ASC- and caspase-1-deficient macrophages. This observation suggested the presence of an ASC-dependent caspase-1-independent cell death pathway. This non-canonical pathway was characterized by Pierini et al. (2012). They identified that while wild-type macrophages die rapidly by pyroptosis, caspase-1-deficient macrophages die 4–6 h later with features typical of apoptosis such as condensed nuclei and a ladder-like DNA pattern indicative of internucleosomal fragmentation. Importantly, neither Aim2-deficient nor ASC-deficient macrophages display any apoptotic nor necrotic features at the same time point. While in wild-type macrophages, the Aim2/ASC speck co-localizes with active caspase-1 (Jones et al. 2010), in caspase-1-deficient macrophages, the Aim2/ASC complex recruits and activates caspase-8 (Pierini et al. 2012). The Aim2/ASC-dependent, caspase-1-independent apoptosis is inhibited by caspase-8 or caspase-9 inhibitors or by ectopic expression of Bcl-2 or Bcl-XL, two anti-apoptotic proteins blocking the mitochondrial intrinsic pathway. Altogether, these data led to the conclusion that upon F. novicida infection, in the absence of caspase-1, Aim2/ASC complex recruits and activates caspase-8, which in turn activates the mitochondrial intrinsic pathway and caspase-9. The combined action of both caspase-8 and caspase-9 then triggers activation of the executioner caspase-3, leading to apoptosis of the infected macrophages (Pierini et al. 2012). Importantly, the ability of ASC platforms to activate caspase-8 is not restricted to Francisella infection or to Aim2 activation since Nlrp3, Aim2 and Nlrc4 complexes can recruit and activate caspase-8 to trigger apoptosis in response to a variety of stimuli (Sagulenko et al. 2013; Man et al. 2014). In addition to promoting apoptotic cell death, the ASC-dependent caspase-1-independent pathway also regulates the IL-18/IFN-γ cascade in a mouse model of tularemia (Pierini et al. 2013). While the level of IL-18 and IFN-γ in the serum of F. novicida-infected mice are much lower in caspase-1-deficient mice than in wild-type mice, the levels of the two cytokines are much higher in Casp1 −/− mice than in Asc −/− mice. Neutralization of IL-18 in infected Casp1 −/− mice reduces IFN-γ levels in the serum demonstrating that bioactive IL-18 can be generated in a caspase-1-independent manner. In vitro, caspase-8, expressed in the presence of Aim2, ASC, and pro-IL-18, triggers specifically the release of IL-18. Altogether, these results demonstrate that, as presented above for the apoptotic cell death, in vivo, in the absence of caspase-1, caspase-8 can be activated in the Aim2/ASC complex leading to pro-IL-18 processing, release of bioactive IL-18, and activation of NK cells to trigger IFN-γ production (Pierini et al. 2013). In a caspase-1-proficient context, the relevance of this caspase-8 pathway remains to be understood. Indeed, caspase-8 is inducing an apoptotic cell death outcompeted by the rapid pyroptosis and caspase-8 is triggering the IL-18/IFN-γ cascade in a manner less efficient than the canonical caspase-1-inflammasome. Such a fail-safe mechanism could be important in humans bearing defective caspase-1 variants (Luksch et al. 2012) or during infections with pathogens blocking specifically caspase-1 activity.
5 Inflammasome Activation in Human Cells
BMDMs have been the main cellular model to study inflammasome activation upon Francisella infection. Yet, there is clear evidence that the inflammasome complexes assembled in human phagocytes contain receptors that differ from the ones sensing Francisella in murine macrophages (Gavrilin et al. 2009; Atianand et al. 2011).
Inflammasome activation in human cells was first studied in monocytes (Fig. 2). Gavrilin et al. demonstrated that the cytosolic localization of F. novicida is required in human monocytes to trigger IL-1β release (Gavrilin et al. 2006). Indeed, various compounds blocking F. novicida escape into the cytosol abolish IL-1β secretion while pro-IL-1β level in the cell lysates is unaffected. Similarly, a mglA mutant, which remains in the vacuole, is unable to trigger IL-1β release in human monocytes (Gavrilin et al. 2006). Finally, while heat-killed Francisella readily induces pro-IL-1β expression, live bacteria are required to activate caspase-1 and IL-1β release in primary human dendritic cells (Li et al. 2006).
Inflammasome activation by Francisella in human cells (Fig. 2) is associated with three intracellular protein sensors, AIM2, NLRP3, and pyrin (encoded by the Mefv gene) (Gavrilin et al. 2009; Atianand et al. 2011). As described above, several groups have observed that murine Nlrp3 −/− and Mefv −/− BMDMs have a normal inflammasome response upon F. novicida infection indicating the key requirement for Aim2 in this experimental system (Mariathasan et al. 2006; Fernandes-Alnemri et al. 2010; Ulland et al. 2010; Atianand et al. 2011). Surprisingly, human macrophages rely on both NLRP3 and AIM2 to activate the inflammasome upon F. novicida infection (Atianand et al. 2011). Indeed, knockdown of either Nlrp3 or Aim2 reduced IL-1β release in PMA-differentiated THP-1 macrophages. A slightly higher IL-1β inhibition was observed upon combined knockdown of both Nlrp3 and Aim2 suggesting that the two PRRs are involved in sensing F. novicida in the human macrophage cytosol (Atianand et al. 2011). The role of NLRP3 was further confirmed in an inflammasome reconstitution system in 293T cells. In this system, NLRP3 but not NLRP12 co-localizes with ASC specks upon F. novicida infection and expression of NLRP3 strongly increases IL-1β release upon LVS or F. novicida infections. While this study by Harton and colleagues (Bedoya et al. 2007) clearly demonstrates the role of NLRP3 in human cells, the reasons explaining the species specificity of the NLRP3 response are unknown. The nucleotide-binding domain, leucine-rich repeat region of human NLRP3 differs from murine Nlrp3 in the distribution of potential serine/threonine phosphorylation sites, oxidant-sensitive cysteine residues, and lysines that may serve as ubiquitination sites to regulate NLRP3 activation (Atianand et al. 2011; Py et al. 2013). Furthermore, human NLRP3 may recognize a broader panel of ligands than its murine counterpart. Indeed, human NLRP3 senses multiple types of RNAs (bacterial mRNA, rRNA, tRNA; synthetic ssRNA) whereas murine Nlrp3 preferentially recognizes only bacterial mRNA (Sha et al. 2014). The exact nature of the PAMPs or of the danger signal leading to NLRP3 activation in human cells during Francisella infection is still elusive.
Pyrin is expressed in primary monocytes and in THP-1 monocytes but its expression is greatly reduced in primary macrophages cultured in the absence of M-CSF or in PMA-differentiated THP-1 cells. In primary human monocytes and in THP-1 monocytes, Mefv knockdown reduces IL-1β release upon F. novicida infection. Conversely, ectopic expression of pyrin in PMA-differentiated THP-1 cells increases IL-1β release upon F. novicida infection (Gavrilin et al. 2009). These results indicate that Pyrin is required in human monocytes to activate the inflammasome complex in response to F. novicida. Recently, pyrin was identified as a sensor of the modification of Rho GTPases activity. It is still unclear whether pyrin directly senses Rho GTPases activity or the consequences of Rho dysfunction on the actin cytoskeleton (Xu et al. 2014). Numerous bacteria target Rho GTPases and the actin cytoskeleton (Lemichez and Aktories 2013; Welch and Way 2013). Yet, in contrast to other cytosolic bacteria, F. tularensis does not use actin-based motility and has no Rho GTPases-targeting toxins. The molecular mechanisms governing pyrin activation during F. novicida infection of human monocytes thus remain mysterious. Inflammasome activation has not been investigated in murine monocytes. However, pyrin is expressed at functional level in murine macrophages (Xu et al. 2014) and Mefv −/− BMDMs, in contrast to Aim2 −/− macrophages, do not display any defect in inflammasome activation. The discrepancy observed between human and murine cells might be linked to the differences between the pyrin proteins in the two species. Murine pyrin lacks the C-terminal B30.2 domain, a domain known in certain immune proteins (e.g., butyrophilin 3A1, TRIM5α) to bind PAMPs (bacterial phospho-antigen, HIV-1 capsid, respectively) (Yang et al. 2012; Sandstrom et al. 2014). While the identity of the PAMP (cytosolic gDNA) and the inflammasome receptor (Aim2) is well established in murine macrophages, further work is needed in human cells to fully understand the nature of the detected PAMP/DAMP and the interaction of the different inflammasome receptors.
6 Lessons from the Bacterial Side: Study of Hypercytotoxic Mutants
Numerous F. novicida and F. holarctica LVS mutants with a hypercytotoxic phenotypes have been identified either through genetic screens (Jones 2010; Lai et al. 2010) or through phenotypic characterization of defined mutants of interest (Weiss et al. 2007; Platz et al. 2010; Ulland et al. 2010; Huang et al. 2010; Jayakar et al. 2011; Lindemann et al. 2011; Peng et al. 2011; Mahawar et al. 2012; Dotson et al. 2013; Doyle et al. 2014). As both F. novicida and F. holarctica LVS have the ability to replicate extensively in the macrophage cytosol before being detected by Aim2, the hypercytotoxic mutants were thought to be mutated in specific virulence factors inhibiting either the recognition by innate immune receptors or directly innate immune pathways. Deletion of the gene encoding an OmpA-like protein (FTL_0325/FTT_0831c) results in an F. holarctica LVS mutant hyperactivating the inflammasome pathway (Mahawar et al. 2012). Upon ectopic expression in HEK293T cells, FTL_0325/FTT_0831c inhibited NF-κB activation suggesting that the hyperinflammasome phenotype of the corresponding mutant is due to an inability of the mutant to specifically block this pathway (Mahawar et al. 2012). However, Norgard and colleagues identified that the OmpA-like protein FTL_0325 contributes to cell division, maintenance of cell shape, and structural integrity suggesting that the hyperinflammasome phenotype was more likely to result from enhanced bacteriolysis in the host cytosol (Robertson et al. 2014). TolC is an outer membrane protein involved in type I secretion pathway. The hypercytotoxic phenotype of the tolC mutant led Platz et al. to suggest that TolC was implicated in the secretion of a toxin inhibiting host cell death (Platz et al. 2010). While this hypothesis cannot be formerly excluded, TolC is well known in E. coli as a member of the Tol-Pal system required for membrane integrity (Lloubes et al. 2001) suggesting that this mutant might be more sensitive to bacteriolysis. Infection with a LVS mutant in ripA, a gene coding an inner membrane protein, leads to a stronger MAPK response and a faster inflammasome response than upon wild-type LVS infection (Huang et al. 2010). RipA was later on identified as a protein-modulating lipid A synthesis, suggesting that the ability of F. tularensis strains to resist to host antimicrobial factors and/or to remain undetected may be associated with membrane remodeling (Miller et al. 2014). This idea was strengthened by work from Weiss and colleagues, who identified that F. novicida used the CRISPR-cas9 endonuclease (FTN_0757) to down-regulate the expression level of a bacterial lipoprotein (FTN_1103) during infection. This down-regulation enhances envelope integrity, decreases TLR2 recognition, and reduces inflammasome activation (Jones et al. 2012; Sampson et al. 2014). In addition to the ripA mutant, several mutants in LPS/capsule biosynthesis genes are hypercytotoxic (Lai et al. 2010; Jayakar et al. 2011). ΔkdtA, ΔlpcC, ΔmanB, and ΔmanC mutants are hypercytotoxic and their LPS is lacking the O-antigen and has a defect in the lipid A core. The respective roles of the defect in the lipid A core and of the lack of O-antigen are unclear since wbtA mutants (which have a normal lipid A core but lack the O-antigen) have been reported as hypercytotoxic by Peng et al. (2011) but not hypercytotoxic by Lai et al. (2010). Conversely, a htrB mutant (deleted in a gene encoding a lipid A acylase) displays a LPS with a normal O-Antigen but is hypercytotoxic (Lai et al. 2010). Altogether, these data indicate that the lipid A structure is a key element to limit bacterial detection by the inflammasome pathway possibly through the maintenance of membrane integrity, resistance to cytosolic antimicrobial factors and spontaneous or host-induced bacteriolysis. MviN, a lipid II flippase, is an enzyme involved in peptidoglycan maturation. In contrast to mviN mutants in E. coli, an mviN mutant in LVS grows normally in axenic medium but presents an aberrant morphology suggesting it might be more susceptible to bacteriolysis than wild-type LVS (Ulland et al. 2010). While it is clear that envelope integrity and its regulation during infection are key factors to avoid recognition by TLR2 and the Aim2 inflammasome, most of the above-cited mutants have been shown by Peng et al. to display aberrant morphologies during growth in minimal medium and to lyse more in the host cell cytosol. This result suggests that under stressful conditions, numerous membrane proteins cooperate with peptidoglycan and LPS-biosynthetic proteins to ensure proper membrane integrity, a lack of PAMP exposure at the surface and a resistance to spontaneous and host-induced bacteriolysis inside the host cytosol (Peng et al. 2011). Altogether, the data from all these studies suggest that Francisella does not actively inhibit the inflammasome pathway but rather use a hiding strategy associated with tight envelope integrity and modification of the structure (e.g., LPS) or the level of expression of its surface exposed PAMP (e.g., TLR2-recognized bacterial lipoprotein). This stealth strategy is particularly striking for highly virulent F. tularensis subsp. tularensis strains.
7 Hypervirulent Strains Escape Inflammasome Detection
Considering the different Francisella species and the different F. tularensis subspecies, there is a good correlation between the ability of the various strains to escape recognition by the inflammasome and their ability to cause disease in humans (Table 1). As previously mentioned, F. novicida infection leads to a strong inflammasome activation although this activation occurs with a delay allowing significant replication in macrophages and in vivo (Mares et al. 2008). This delay in inflammasome activation is even stronger upon infection with F. holarctica LVS and is associated with a lower IL-1β release than upon F. novicida infection (Carlson et al. 2007; Ghonime et al. 2015). Finally, infection with F. tularensis type A strains elicits no or a very weak inflammasome activation (Wickstrum et al. 2009; Bauler et al. 2011; Crane et al. 2014; Ghonime et al. 2015).
While numerous groups have observed caspase-1 activation, IL-1β release, and pyroptosis in macrophages infected with LVS (Mariathasan et al. 2005; Gavrilin et al. 2006; Li et al. 2006; Wickstrum et al. 2009; Rathinam et al. 2010), apoptosis is also observed in F. holarctica LVS-infected macrophages with an involvement of the intrinsic pathway proceeding through caspase-9 and caspase-3 activation and PARP cleavage (Lai and Sjostedt 2003). This apoptotic pathway has been observed in the J774 macrophage cell line, which is deficient for F. novicida-mediated inflammasome cell death (TH unpublished observation) but also in BMDMs (Doyle et al. 2014). These observations suggest that F. holarctica LVS may be less detected by the inflammasome and that another cell-intrinsic mechanism may trigger mitochondrial apoptosis to synergize with pyroptosis to fully remove the bacterial replicative niche. The ability of F. holarctica LVS to dampen inflammasome activation correlates with a general ability of this strain to dampen pro-inflammatory signaling (Telepnev et al. 2003). Indeed, infection with F. holarctica LVS inhibits LPS-induced TNF-α and IL-1β release. This inhibition is dependent on FPI-encoded genes, and it is still unclear whether it is a direct consequence of phagosomal escape or whether a specific T6SS-effector modulates this pro-inflammatory response (Telepnev et al. 2003; Broms et al. 2010, 2011).
As mentioned above, infection with F. tularensis subs. tularensis strains, leads to almost no IL-1β (undetectable to less than 20 ng/ml depending on the studies) and no IL-18 (undetectable to less than 50 ng/ml depending on the studies) release (Wickstrum et al. 2009; Crane et al. 2014; Ghonime et al. 2015). Death of SCHU S4-infected macrophages occurs very late, suggesting that pyroptosis does not play a major role in restricting SCHU S4 replication. The low inflammasome response is not due to an inability of the NLRP3 inflammasome to be primed upon infection. Indeed, when the NLRP3 priming event was evaluated using ATP as a second signal, F. novicida, LVS, and F. tularensis strains had a similar NLRP3 priming activity (Ghonime et al. 2015). This result suggests that infection with SCHU S4 does not provide the signal 2 required for inflammasome activation. Bosio and co-workers (Crane et al. 2014) demonstrated that F. novicida is more sensitive to H2O2-mediated killing than SCHU S4. As previously mentioned, ROS are required for F. novicida-mediated inflammasome activation. The resistance of SCHU S4 to ROS could thus limit ROS-mediated bacteriolysis of SCHU S4 in the cytosol, DNA release, and AIM2 inflammasome activation (Crane et al. 2014). While this model is appealing, further evidence remains to be provided to understand the role of mitochondrial ROS and the inability of F. tularensis strain to be detected by the inflammasome. In addition to the resistance to ROS-mediated killing, the ability of F. tularensis SCHU S4 to escape recognition by the inflammasome pathway might be related to its LPS and capsule structure. Indeed, mutants lacking genes in a locus required for O-antigen and capsule biosynthesis are hypercytotoxic upon macrophage infection (Lindemann et al. 2011).
The ability of SCHU S4 strain to modulate IL-1β response is also dependent on its entry pathway in human macrophages. Indeed, the efficient uptake of SCHU S4 strain by human macrophages requires C3 opsonization and the presence of the CR3 receptor at the macrophage surface. Despite an increase entry into host cells, infection with C3-opsonized F. tularensis leads to a decreased IL-1β release compared to an infection with non-opsonized F. tularensis. This CR3-mediated immune suppression is not specific for the inflammasome pathway but may act through inhibition of TLR2 signaling highlighting the connections between these pathways (Dai et al. 2013).
In vivo, in a mouse model of tularemia with a type A strain, an immunostaining approach to detect active caspases revealed a predominant activation of caspase-3 suggesting that the absence of inflammasome activation is also true in vivo. Although the role of caspase-1 has not been deeply investigated, the formation of granuloma and the frequency of TUNEL+ cells were similar in the wild-type and Casp1 −/− mice infected with type A strain (Wickstrum et al. 2009). Only a few cells displayed active caspase-1 staining both in the liver and in the spleen. Interestingly, active Caspase-1 was restricted to the splenic marginal zones (Wickstrum et al. 2009), which contain macrophage subsets with great ability to phagocyte pathogens (Borges da Silva et al. 2015). Altogether, while the results suggest that the inflammasome does not play a major role to fight highly virulent F. tularensis subsp. tularensis strains, inflammasome activation may be important in dedicated macrophage subsets localized in strategic places in the lymphoid organs to orchestrate downstream immune responses.
8 Concluding Remarks
Inflammasome-deficient mice have demonstrated the key role of the inflammasome to fight F. novicida infection. The mechanisms leading to inflammasome activation are now well established with the action of the interferon-inducible proteins Gbp2 and Gbp5 required to lyse F. novicida and to release its genomic DNA into the host cytosol. Aim2 is then the key sensor to initiate inflammasome complex formation and trigger the ensuing inflammatory cascade. Interestingly, the ability of Francisella strains to activate the inflammasome pathway is inversely correlated with their pathogenicity toward human. In addition to having a non-toxic lipid A escaping recognition by both TLR4 and caspase-11, Francisella has evolved a tight membrane associated with resistance to bacteriolysis and down-regulation of potential PAMPs. This strategy allows F. novicida and F. holarctica LVS to replicate in the cytosol before being eventually detected by the inflammasome sensors. This furtiveness is even higher in the highly virulent F. tularensis subsp. tularensis strains since macrophages infected with these strains do not demonstrate any inflammasome activation markers.
One striking feature of F. novicida and F. holarctica LVS inflammasome in murine macrophages is their exclusive dependence on the Aim2 receptor. This is unique since several inflammasome sensors are involved in the detection of most other intracellular bacteria, including Listeria monocytogenes, which is detected by Nlrp3, Nlrc4, and Aim2 (Wu et al. 2010). This strict dependence is even more surprising considering that in human phagocytes, three different receptors (PYRIN, NLRP3, and AIM2) have been implicated in the detection of Francisella infection.
The inflammasome complex is highly interconnected with other immune pathways acting both upstream of Aim2 and downstream of caspase-1-dependent cytokines. Indeed, the TLR2 and the cGas/Ifi204-STING pathways potentiate or are required for Aim2 inflammasome activation in Francisella-infected cells. Surprisingly, for a cytosolic bacterium, the contribution of NOD1/2, the cytosolic sensors of peptidoglycan fragments, seems minimal. Downstream of caspase-1, there are clear evidences that IL-18 regulates IFN-γ level and that IL-1β regulates the IL-23/IL-17 cascade and a protective IgM response mediated by B1a B cells (del Barrio et al. 2015). IFN-γ (Anthony et al. 1989) and to a lesser extent IL-17 (Lin et al. 2009; Khader and Gopal 2010; Skyberg et al. 2013), are two very important cytokines to fight Francisella and other intracellular pathogens highlighting the key role of the inflammasome pathway in the orchestration of the immune response.
Of note, while this review focuses on mouse and human cells, F. noatunensis, a species responsible for the systemic granulomatous inflammatory disease, francisellosis in cod (Furevik et al. 2011) triggers IL-1β release in zebrafish leukocytes in a caspase-1-like dependent manner (Vojtech et al. 2012). The inflammasome pathway is thus likely to be very important in other Vertebrates species in response to other Francisella species.
Finally, while the understanding of the mechanisms controlling the inflammasome activation during Francisella infection has greatly progressed since the first report in 2005 (Mariathasan et al. 2005), there are still a number of questions to be solved, five of which are listed below.
First, while cytosolic DNA is detected early on during infection by cGAS and Ifi204, Aim2 activation by cytosolic DNA occurs much later during infection and requires the bacteriolytic action of Gbp2 and Gbp5. This observation suggests a hierarchy of sensing between the different DNA sensors, which is not understood.
Second, the mechanisms leading to the recruitment of Gbps onto cytosolic Francisella and to their bacteriolytic actions remain unknown. The presence of a CAAX-motif (prenylation motif) in the C-terminus of Gbp2 and Gbp5 suggests the involvement of an undefined membrane compartment. Furthermore, other interferon-inducible proteins might participate in Gbp2/5 action although such actors remain to be identified.
Third, the role of the autophagy pathway in counterbalancing inflammasome activation during Francisella remains to be assessed. Indeed, autophagy targets AIM2 inflammasome components during transfection of synthetic DNA (Shi et al. 2012). Furthermore, autophagy clears the cytosol from O-antigen mutants (Case et al. 2014) and from replication-deficient Francisella dying in the cytosol (Chong et al. 2012) possibly decreasing the source of cytosolic DNA to activate the Aim2 inflammasome.
Fourth, the specificity of the human inflammasomes remains to be understood. The activation of pyrin in monocytes remains mysterious in absence of any known modification of the actin cytoskeleton upon Francisella infections. Similarly, the danger signals or the PAMP leading to activation of the human NLRP3 receptor but not of the murine Nlrp3 remains to be identified.
Fifth, while in vivo experiments demonstrate that the inflammasome is an important mechanism to fight F. novicida and F. holarctica LVS infection, the repertoire of cells sustaining inflammasome activation in vivo during infection remains to be determined. Particularly, the role of the inflammasome pathway in neutrophils or in macrophages from the splenic marginal zones would be interesting to investigate to understand why despite efficient in vitro inflammasome activation, F. novicida kills wild-type mice at a very low infectious dose.
No doubt that the next decade will provide us with exiting findings regarding the activation of the inflammasome and how Francisella escapes this recognition to remain one of the most infectious pathogen.
References
Aachoui Y, Leaf IA, Hagar JA et al (2013) Caspase-11 protects against bacteria that escape the vacuole. Science 339:975–978. doi:10.1126/science.1230751
Akhter A, Caution K, Abu Khweek A et al (2012) Caspase-11 promotes the fusion of phagosomes harboring pathogenic bacteria with lysosomes by modulating actin polymerization. Immunity 37:35–47. doi:10.1016/j.immuni.2012.05.001
Anthony LS, Ghadirian E, Nestel FP, Kongshavn PA (1989) The requirement for gamma interferon in resistance of mice to experimental tularemia. Microb Pathog 7:421–428
Atianand MK, Duffy EB, Shah A et al (2011) Francisella tularensis reveals a disparity between human and mouse NLRP3 inflammasome activation. J Biol Chem 286:39033–39042. doi:10.1074/jbc.M111.244079
Auerbuch V, Brockstedt DG, Meyer-Morse N et al (2004) Mice lacking the type I interferon receptor are resistant to Listeria monocytogenes. J Exp Med 200:527–533
Barel M, Charbit A (2013) Francisella tularensis intracellular survival: to eat or to die. Microbes Infect Inst Pasteur. doi:10.1016/j.micinf.2013.09.009
Barker JR, Chong A, Wehrly TD et al (2009) The Francisella tularensis pathogenicity island encodes a secretion system that is required for phagosome escape and virulence. Mol Microbiol 74:1459–1470
Baron GS, Nano FE (1998) MglA and MglB are required for the intramacrophage growth of Francisella novicida. Mol Microbiol 29:247–259
Bauler TJ, Chase JC, Bosio CM (2011) IFN-beta mediates suppression of IL-12p40 in human dendritic cells following infection with virulent Francisella tularensis. J Immunol Baltim Md 1950 187:1845–1855. doi:10.4049/jimmunol.1100377
Bedoya F, Sandler LL, Harton JA (2007) Pyrin-only protein 2 modulates NF-kappaB and disrupts ASC:CLR interactions. J Immunol 178:3837–3845
Belhocine K, Monack DM (2012) Francisella infection triggers activation of the AIM2 inflammasome in murine dendritic cells. Cell Microbiol 14:71–80. doi:10.1111/j.1462-5822.2011.01700.x
Bokhari SM, Kim K-J, Pinson DM et al (2008) NK cells and gamma interferon coordinate the formation and function of hepatic granulomas in mice infected with the Francisella tularensis live vaccine strain. Infect Immun 76:1379–1389. doi:10.1128/IAI.00745-07
Borges da Silva H, Fonseca R, Pereira RM et al (2015) Splenic macrophage subsets and their function during blood-borne infections. Front Immunol 6:480. doi:10.3389/fimmu.2015.00480
Briken V, Ruffner H, Schultz U et al (1995) Interferon regulatory factor 1 is required for mouse Gbp gene activation by gamma interferon. Mol Cell Biol 15:975–982
Broms JE, Sjostedt A, Lavander M (2010) The role of the Francisella tularensis pathogenicity island in Type VI secretion, intracellular survival, and modulation of host cell signaling. Front Microbiol. doi:10.3389/fmicb.2010.00136
Broms JE, Lavander M, Meyer L, Sjostedt A (2011) IglG and IglI of the Francisella pathogenicity island are important virulence determinants of Francisella tularensis LVS. Infect Immun 79:3683–3696. doi:10.1128/IAI.01344-10
Burckstummer T, Baumann C, Bluml S et al (2009) An orthogonal proteomic-genomic screen identifies AIM2 as a cytoplasmic DNA sensor for the inflammasome. Nat Immunol 10:266–272
Carlson PEJ, Carroll JA, O’Dee DM, Nau GJ (2007) Modulation of virulence factors in Francisella tularensis determines human macrophage responses. Microb Pathog 42:204–214. doi:10.1016/j.micpath.2007.02.001
Case EDR, Chong A, Wehrly TD et al (2014) The Francisella O-antigen mediates survival in the macrophage cytosol via autophagy avoidance. Cell Microbiol 16:862–877. doi:10.1111/cmi.12246
Checroun C, Wehrly TD, Fischer ER et al (2006) Autophagy-mediated reentry of Francisella tularensis into the endocytic compartment after cytoplasmic replication. Proc Natl Acad Sci USA 103:14578–14583
Chong A, Wehrly TD, Child R et al (2012) Cytosolic clearance of replication-deficient mutants reveals Francisella tularensis interactions with the autophagic pathway. Autophagy 8:1342–1356. doi:10.4161/auto.20808
Clemens DL, Horwitz MA (2007) Uptake and intracellular fate of Francisella tularensis in human macrophages. Ann NY Acad Sci R 101196annals1409001 1105:160–186
Clemens DL, Lee BY, Horwitz MA (2004) Virulent and avirulent strains of Francisella tularensis prevent acidification and maturation of their phagosomes and escape into the cytoplasm in human macrophages. Infect Immun 72:3204–3217. doi:10.1128/IAI.72.6.3204-3217.2004
Clemens DL, Lee BY, Horwitz MA (2005) Francisella tularensis enters macrophages via a novel process involving pseudopod loops. Infect Immun 73:5892–5902. doi:10.1128/IAI.73.9.5892-5902.2005
Cole LE, Shirey KA, Barry E et al (2007) Toll-like receptor 2-mediated signaling requirements for Francisella tularensis live vaccine strain infection of murine macrophages. Infect Immun 75:4127–4137
Cole LE, Santiago A, Barry E et al (2008) Macrophage proinflammatory response to Francisella tularensis live vaccine strain requires coordination of multiple signaling pathways. J Immunol 180:6885–6891
Cole LE, Laird MHW, Seekatz A et al (2010) Phagosomal retention of Francisella tularensis results in TIRAP/Mal-independent TLR2 signaling. J Leukoc Biol 87:275–281. doi:10.1189/jlb.0909619
Crane DD, Bauler TJ, Wehrly TD, Bosio CM (2014) Mitochondrial ROS potentiates indirect activation of the AIM2 inflammasome. Front Microbiol 5:438. doi:10.3389/fmicb.2014.00438
Dai S, Rajaram MVS, Curry HM et al (2013) Fine tuning inflammation at the front door: macrophage complement receptor. PLoS Pathog 9:e1003114. doi:10.1371/journal.ppat.1003114
De Pascalis R, Taylor BC, Elkins KL (2008) Diverse myeloid and lymphoid cell subpopulations produce gamma interferon during early innate immune responses to Francisella tularensis live vaccine strain. Infect Immun 76:4311–4321
Degrandi D, Kravets E, Konermann C et al (2013) Murine guanylate binding protein 2 (mGBP2) controls Toxoplasma gondii replication. Proc Natl Acad Sci USA 110:294–299. doi:10.1073/pnas.1205635110
del Barrio L, Sahoo M, Lantier L et al (2015) Production of anti-LPS IgM by B1a B cells depends on IL-1beta and is protective against lung infection with Francisella tularensis LVS. PLoS Pathog 11:e1004706. doi:10.1371/journal.ppat.1004706
Dietrich N, Lienenklaus S, Weiss S, Gekara NO (2010) Murine toll-like receptor 2 activation induces type I interferon responses from endolysosomal compartments. PLoS ONE 5:e10250. doi:10.1371/journal.pone.0010250
Dotson RJ, Rabadi SM, Westcott EL et al (2013) Repression of inflammasome by Francisella tularensis during early stages of infection. J Biol Chem 288:23844–23857. doi:10.1074/jbc.M113.490086
Doyle CR, Pan J-A, Mena P et al (2014) TolC-dependent modulation of host cell death by the Francisella tularensis live vaccine strain. Infect Immun 82:2068–2078. doi:10.1128/IAI.00044-14
Elkins KL, Rhinehart-Jones TR, Culkin SJ et al (1996) Minimal requirements for murine resistance to infection with Francisella tularensis LVS. Infect Immun 64:3288–3293
Fang FC (2004) Antimicrobial reactive oxygen and nitrogen species: concepts and controversies. Nat Rev Microbiol 2:820–832. doi:10.1038/nrmicro1004
Fernandes-Alnemri T, Yu JW, Datta P et al (2009) AIM2 activates the inflammasome and cell death in response to cytoplasmic DNA. Nature 458:509–513
Fernandes-Alnemri T, Yu JW, Juliana C et al (2010) The AIM2 inflammasome is critical for innate immunity to Francisella tularensis. Nat Immunol 11:385–393. doi:10.1038/ni.1859
Finethy R, Jorgensen I, Haldar AK et al (2015) Guanylate binding proteins enable rapid activation of canonical and noncanonical inflammasomes in chlamydia-infected macrophages. Infect Immun 83:4740–4749. doi:10.1128/IAI.00856-15
Furevik A, Pettersen EF, Colquhoun D, Wergeland HI (2011) The intracellular lifestyle of Francisella noatunensis in Atlantic cod (Gadus morhua L.) leucocytes. Fish Shellfish Immunol 30:488–494. doi:10.1016/j.fsi.2010.11.019
Gavrilin MA, Bouakl IJ, Knatz NL et al (2006) Internalization and phagosome escape required for Francisella to induce human monocyte IL-1beta processing and release. Proc Natl Acad Sci USA 103:141–146
Gavrilin MA, Mitra S, Seshadri S et al (2009) Pyrin critical to macrophage IL-1beta response to Francisella challenge. J Immunol Baltim Md 1950 182:7982–7989. doi:10.4049/jimmunol.0803073
Ghonime MG, Mitra S, Eldomany RA et al (2015) Inflammasome priming is similar for Francisella species that differentially induce inflammasome activation. PLoS ONE 10:e0127278. doi:10.1371/journal.pone.0127278
Golovliov I, Baranov V, Krocova Z et al (2003) An attenuated strain of the facultative intracellular bacterium Francisella tularensis can escape the phagosome of monocytic cells. Infect Immun 71:5940–5950
Gunn J, Ernst R (2007) The structure and function of Francisella LPS
Gurcan S (2014) Epidemiology of tularemia. Balk Med J 31:3–10. doi:10.5152/balkanmedj.2014.13117
Hagar JA, Powell DA, Aachoui Y et al (2013) Cytoplasmic LPS activates caspase-11: implications in TLR4-independent endotoxic shock. Science 341:1250–1253. doi:10.1126/science.1240988
Hajjar AM, Harvey MD, Shaffer SA et al (2006) Lack of in vitro and in vivo recognition of Francisella tularensis subspecies lipopolysaccharide by toll-like receptors. Infect Immun 74:6730–6738
Hall JD, Woolard MD, Gunn BM et al (2008) Infected-host-cell repertoire and cellular response in the lung following inhalation of Francisella tularensis Schu S4, LVS, or U112. Infect Immun 76:5843–5852
Henry T, Monack DM (2007) Activation of the inflammasome upon Francisella tularensis infection: interplay of innate immune pathways and virulence factors. Cell Microbiol 9:2543–2551
Henry T, Brotcke A, Weiss DS et al (2007) Type I interferon signaling is required for activation of the inflammasome during Francisella infection. J Exp Med 204:987–994
Henry T, Kirimanjeswara GS, Ruby T et al (2010) Type I IFN signaling constrains IL-17A/F secretion by gammadelta T cells during bacterial infections. J Immunol 184:3755–3767. doi:10.4049/jimmunol.0902065
Hornung V, Ablasser A, Charrel-Dennis M et al (2009) AIM2 recognizes cytosolic dsDNA and forms a caspase-1-activating inflammasome with ASC. Nature 458:514–518
Huang MT-H, Mortensen BL, Taxman DJ et al (2010) Deletion of ripA alleviates suppression of the inflammasome and MAPK by Francisella tularensis. J Immunol Baltim Md 1950(185):5476–5485. doi:10.4049/jimmunol.1002154
Jayakar HR, Parvathareddy J, Fitzpatrick EA et al (2011) A galU mutant of Francisella tularensis is attenuated for virulence in a murine pulmonary model of tularemia. BMC Microbiol 11:1–16. doi:10.1186/1471-2180-11-179
Jin L, Hill KK, Filak H, et al (2011) MPYS is required for IFN response factor 3 activation and type I IFN production in the response of cultured phagocytes to bacterial second messengers cyclic-di-AMP and cyclic-di-GMP. J Immunol Baltim Md 1950 187:2595–2601. doi:10.4049/jimmunol.1100088
Jin T, Perry A, Jiang J et al (2012) Structures of the HIN domain: DNA complexes reveal ligand binding and activation mechanisms of the AIM2 inflammasome and IFI16 receptor. Immunity 36:561–571. doi:10.1016/j.immuni.2012.02.014
Jones J (2010) Molecular mechanisms of the innate immune response to Francisella tularensis. Stanford University
Jones CL, Weiss DS (2011) TLR2 signaling contributes to rapid inflammasome activation during F. novicida infection. PLoS ONE 6:e20609. doi:10.1371/journal.pone.0020609
Jones JW, Kayagaki N, Broz P et al (2010) Absent in melanoma 2 is required for innate immune recognition of Francisella tularensis. Proc Natl Acad Sci USA 107:9771–9776. doi:10.1073/pnas.1003738107
Jones CL, Sampson TR, Nakaya HI et al (2012) Repression of bacterial lipoprotein production by F. novicida facilitates evasion of innate immune recognition. Cell. doi:10.1111/j.1462-5822.2012.01816.x
Kanistanon D, Hajjar AM, Pelletier MR et al (2008) A Francisella mutant in lipid A carbohydrate modification elicits protective immunity. PLoS Pathog 4:e24. doi:10.1371/journal.ppat.0040024
Katz J, Zhang P, Martin M et al (2006) Toll-like receptor 2 is required for inflammatory responses to Francisella tularensis LVS. Infect Immun 74:2809–2816
Kayagaki N, Wong MT, Stowe IB et al (2013) Noncanonical inflammasome activation by intracellular LPS independent of TLR4. Science. doi:10.1126/science.1240248
Khader SA, Gopal R (2010) IL-17 in protective immunity to intracellular pathogens. Virulence 1:423–427. doi:10.4161/viru.1.5.12862
Kim BH, Shenoy AR, Kumar P et al (2011) A family of IFN-gamma-inducible 65-kD GTPases protects against bacterial infection. Science 332:717–721. doi:10.1126/science.1201711
Kingry LC, Petersen JM (2014) Comparative review of Francisella tularensis and Francisella novicida. Front Cell Infect Microbiol 4:35. doi:10.3389/fcimb.2014.00035
Lai XH, Sjostedt A (2003) Delineation of the molecular mechanisms of Francisella tularensis-induced apoptosis in murine macrophages. Infect Immun 71:4642–4646
Lai X-H, Shirley RL, Crosa L et al (2010) Mutations of Francisella novicida that alter the mechanism of its phagocytosis by murine macrophages. PLoS ONE 5:e11857. doi:10.1371/journal.pone.0011857
Larsson P, Elfsmark D, Svensson K et al (2009) Molecular evolutionary consequences of niche restriction in Francisella tularensis, a facultative intracellular pathogen. PLoS Pathog 5:e1000472. doi:10.1371/journal.ppat.1000472
Lemichez E, Aktories K (2013) Hijacking of Rho GTPases during bacterial infection. Exp Cell Res 319:2329–2336. doi:10.1016/j.yexcr.2013.04.021
Li H, Nookala S, Bina XR et al (2006) Innate immune response to Francisella tularensis is mediated by TLR2 and caspase-1 activation. J Leukoc Biol 80:766–773
Lin Y, Ritchea S, Logar A et al (2009) Interleukin-17 is required for T helper 1 cell immunity and host resistance to the intracellular pathogen Francisella tularensis. Immunity 31:799–810
Lindemann SR, Peng K, Long ME et al (2011) Francisella tularensis Schu S4 O-antigen and capsule biosynthesis gene mutants induce early cell death in human macrophages. Infect Immun 79:581–594. doi:10.1128/IAI.00863-10
Lloubes R, Cascales E, Walburger A et al (2001) The Tol-Pal proteins of the Escherichia coli cell envelope: an energized system required for outer membrane integrity? Res Microbiol 152:523–529
Luksch H, Romanowski MJ, Chara O et al (2012) Naturally occurring genetic variants of human caspase-1 differ considerably in structure and the ability to activate interleukin-1beta. Hum Mutat. doi:10.1002/humu.22169
Mahawar M, Atianand MK, Dotson RJ et al (2012) Identification of a novel Francisella tularensis factor required for intramacrophage survival and subversion of innate immune response. J Biol Chem 287:25216–25229. doi:10.1074/jbc.M112.367672
Man SM, Hopkins LJ, Nugent E et al (2014) Inflammasome activation causes dual recruitment of NLRC4 and NLRP3 to the same macromolecular complex. Proc Natl Acad Sci USA. doi:10.1073/pnas.1402911111
Man SM, Karki R, Malireddi RKS et al (2015) The transcription factor IRF1 and guanylate-binding proteins target activation of the AIM2 inflammasome by Francisella infection. Nat Immunol 16:467–475. doi:10.1038/ni.3118
Mares CA, Ojeda SS, Morris EG et al (2008) Initial delay in the immune response to Francisella tularensis is followed by hypercytokinemia characteristic of severe sepsis and correlating with upregulation and release of damage-associated molecular patterns. Infect Immun 76:3001–3010. doi:10.1128/IAI.00215-08
Mariathasan S, Weiss DS, Dixit VM, Monack DM (2005) Innate immunity against Francisella tularensis is dependent on the ASC/caspase-1 axis. J Exp Med 202:1043–1049
Mariathasan S, Weiss DS, Newton K et al (2006) Cryopyrin activates the inflammasome in response to toxins and ATP. Nature 440:228–232
McLendon MK, Apicella MA, Allen LA (2006) Francisella tularensis: taxonomy, genetics, and immunopathogenesis of a potential agent of biowarfare. Annu Rev Microbiol 60:167–185
Meunier E, Broz P (2016) Interferon-inducible GTPases in cell autonomous and innate immunity. Cell Microbiol 18:168–180. doi:10.1111/cmi.12546
Meunier E, Dick MS, Dreier RF et al (2014) Caspase-11 activation requires lysis of pathogen-containing vacuoles by IFN-induced GTPases. Nature 509:366–370. doi:10.1038/nature13157
Meunier E, Wallet P, Dreier RF et al (2015) Guanylate-binding proteins promote activation of the AIM2 inflammasome during infection with Francisella novicida. Nat Immunol 16:476–484. doi:10.1038/ni.3119
Miao EA, Leaf IA, Treuting PM et al (2010) Caspase-1-induced pyroptosis is an innate immune effector mechanism against intracellular bacteria. Nat Immunol 11:1136–1142. doi:10.1038/ni.1960
Miller CN, Steele SP, Brunton JC et al (2014) Extragenic suppressor mutations in DeltaripA disrupt stability and function of LpxA. BMC Microbiol 14:336. doi:10.1186/s12866-014-0336-x
Nano FE, Zhang N, Cowley SC et al (2004) A Francisella tularensis pathogenicity island required for intramacrophage growth. J Bacteriol 186:6430–6436
Okan NA, Kasper DL (2013) The atypical lipopolysaccharide of Francisella. Carbohydr Res 378:79–83. doi:10.1016/j.carres.2013.06.015
Pelegrin P, Barroso-Gutierrez C, Surprenant A (2008) P2X7 receptor differentially couples to distinct release pathways for IL-1beta in mouse macrophage. J Immunol 180:7147–7157
Peng K, Broz P, Jones J et al (2011) Elevated AIM2-mediated pyroptosis triggered by hypercytotoxic Francisella mutant strains is attributed to increased intracellular bacteriolysis. Cell Microbiol 13:1586–1600. doi:10.1111/j.1462-5822.2011.01643.x
Pierini R, Juruj C, Perret M et al (2012) AIM2/ASC triggers caspase-8-dependent apoptosis in Francisella-infected caspase-1-deficient macrophages. Cell Death Differ 19:1709–1721. doi:10.1038/cdd.2012.51
Pierini R, Perret M, Djebali S et al (2013) ASC controls IFN-gamma levels in an IL-18-Dependent Manner in Caspase-1-Deficient mice infected with Francisella novicida. J Immunol 191:3847–3857. doi:10.4049/jimmunol.1203326
Pilla DM, Hagar JA, Haldar AK et al (2014) Guanylate binding proteins promote caspase-11-dependent pyroptosis in response to cytoplasmic LPS. Proc Natl Acad Sci USA 111:6046–6051. doi:10.1073/pnas.1321700111
Platz GJ, Bublitz DC, Mena P et al (2010) A tolC mutant of Francisella tularensis is hypercytotoxic compared to the wild type and elicits increased proinflammatory responses from host cells. Infect Immun 78:1022–1031. doi:10.1128/IAI.00992-09
Py BF, Kim M-S, Vakifahmetoglu-Norberg H, Yuan J (2013) Deubiquitination of NLRP3 by BRCC3 critically regulates inflammasome activity. Mol Cell 49:331–338. doi:10.1016/j.molcel.2012.11.009
Rajaram MVS, Butchar JP, Parsa KVL et al (2009) Akt and SHIP modulate Francisella escape from the phagosome and induction of the Fas-mediated death pathway. PLoS ONE 4:e7919. doi:10.1371/journal.pone.0007919
Rathinam VA, Jiang Z, Waggoner SN et al (2010) The AIM2 inflammasome is essential for host defense against cytosolic bacteria and DNA viruses. Nat Immunol 11:395–402. doi:10.1038/ni.1864
Roberts TL, Idris A, Dunn JA et al (2009) HIN-200 proteins regulate caspase activation in response to foreign cytoplasmic DNA. Science 323:1057–1060
Robertson GT, Case EDR, Dobbs N et al (2014) FTT0831c/FTL_0325 contributes to Francisella tularensis cell division, maintenance of cell shape, and structural integrity. Infect Immun 82:2935–2948. doi:10.1128/IAI.00102-14
Sagulenko V, Thygesen SJ, Sester DP et al (2013) AIM2 and NLRP3 inflammasomes activate both apoptotic and pyroptotic death pathways via ASC. Cell Death Differ (Epub May 2013) 3:1–12. doi:10.1038/cdd.2013.37
Sampson TR, Napier BA, Schroeder MR et al (2014) A CRISPR-Cas system enhances envelope integrity mediating antibiotic resistance and inflammasome evasion. Proc Natl Acad Sci USA 111:11163–11168. doi:10.1073/pnas.1323025111
Sandstrom G, Sjostedt A, Johansson T et al (1992) Immunogenicity and toxicity of lipopolysaccharide from Francisella tularensis LVS. FEMS Microbiol Immunol 5:201–210
Sandstrom A, Peigne C-M, Leger A et al (2014) The intracellular B30.2 domain of butyrophilin 3A1 binds phosphoantigens to mediate activation of human Vgamma9Vdelta2 T cells. Immunity 40:490–500. doi:10.1016/j.immuni.2014.03.003
Sha W, Mitoma H, Hanabuchi S et al (2014) Human NLRP3 inflammasome senses multiple types of bacterial RNAs. Proc Natl Acad Sci USA 111:16059–16064. doi:10.1073/pnas.1412487111
Shenoy AR, Wellington DA, Kumar P et al (2012) GBP5 promotes NLRP3 inflammasome assembly and immunity in mammals. Science 336:481–485. doi:10.1126/science.1217141
Shi CS, Shenderov K, Huang NN et al (2012) Activation of autophagy by inflammatory signals limits IL-1beta production by targeting ubiquitinated inflammasomes for destruction. Nat Immunol 13:255–263. doi:10.1038/ni.2215
Shi J, Zhao Y, Wang Y et al (2014) Inflammatory caspases are innate immune receptors for intracellular LPS. Nature 514:187–192. doi:10.1038/nature13683
Sjostedt A (2007) Tularemia: history, epidemiology, pathogen physiology, and clinical manifestations
Skyberg JA, Rollins MF, Samuel JW et al (2013) Interleukin-17 protects against the Francisella tularensis live vaccine strain but not against a virulent F. tularensis type A strain. Infect Immun 81:3099–3105. doi:10.1128/IAI.00203-13
Stanley SA, Johndrow JE, Manzanillo P, Cox JS (2007) The Type I IFN response to infection with Mycobacterium tuberculosis requires ESX-1-mediated secretion and contributes to pathogenesis. J Immunol 178:3143–3152
Storek KM, Gertsvolf NA, Ohlson MB, Monack DM (2015) cGAS and Ifi204 cooperate to produce Type I IFNs in response to Francisella infection. J Immunol Baltim Md 1950 194:3236–3245. doi:10.4049/jimmunol.1402764
Telepnev M, Golovliov I, Grundstrom T et al (2003) Francisella tularensis inhibits Toll-like receptor-mediated activation of intracellular signalling and secretion of TNF-alpha and IL-1 from murine macrophages. Cell Microbiol 5:41–51
Thakran S, Li H, Lavine CL et al (2008) Identification of Francisella tularensis lipoproteins that stimulate the toll-like receptor (TLR) 2/TLR1 heterodimer. J Biol Chem 283:3751–3760. doi:10.1074/jbc.M706854200
Ulland TK, Buchan BW, Ketterer MR et al (2010) Cutting edge: mutation of Francisella tularensis mviN leads to increased macrophage absent in melanoma 2 inflammasome activation and a loss of virulence. J Immunol 185:2670–2674. doi:10.4049/jimmunol.1001610
Vojtech LN, Scharping N, Woodson JC, Hansen JD (2012) Roles of inflammatory caspases during processing of zebrafish interleukin-1beta in Francisella noatunensis infection. Infect Immun 80:2878–2885. doi:10.1128/IAI.00543-12
Wang X, Ribeiro AA, Guan Z et al (2007) Attenuated virulence of a Francisella mutant lacking the lipid A 4′-phosphatase. Proc Natl Acad Sci USA 104:4136–4141. doi:10.1073/pnas.0611606104
Weiss DS, Brotcke A, Henry T et al (2007) In vivo negative selection screen identifies genes required for Francisella virulence. Proc Natl Acad Sci USA 104:6037–6042
Welch MD, Way M (2013) Arp2/3-mediated actin-based motility: a tail of pathogen abuse. Cell Host Microbe 14:242–255. doi:10.1016/j.chom.2013.08.011
West AP, Brodsky IE, Rahner C et al (2011) TLR signalling augments macrophage bactericidal activity through mitochondrial ROS. Nature 472:476–480. doi:10.1038/nature09973
Wickstrum JR, Bokhari SM, Fischer JL et al (2009) Francisella tularensis induces extensive caspase-3 activation and apoptotic cell death in the tissues of infected mice. Infect Immun 77:4827–4836. doi:10.1128/IAI.00246-09
Wu J, Fernandes-Alnemri T, Alnemri ES (2010) Involvement of the AIM2, NLRC4, and NLRP3 inflammasomes in caspase-1 activation by Listeria monocytogenes. J Clin Immunol 30:693–702. doi:10.1007/s10875-010-9425-2
Xu H, Yang J, Gao W et al (2014) Innate immune sensing of bacterial modifications of Rho GTPases by the Pyrin inflammasome. Nature 513:237–241. doi:10.1038/nature13449
Yamamoto M, Okuyama M, Ma JS et al (2012) A cluster of interferon-gamma-inducible p65 GTPases plays a critical role in host defense against Toxoplasma gondii. Immunity 37:302–313. doi:10.1016/j.immuni.2012.06.009
Yang H, Ji X, Zhao G et al (2012) Structural insight into HIV-1 capsid recognition by rhesus TRIM5alpha. Proc Natl Acad Sci USA 109:18372–18377. doi:10.1073/pnas.1210903109
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Wallet, P., Lagrange, B., Henry, T. (2016). Francisella Inflammasomes: Integrated Responses to a Cytosolic Stealth Bacterium. In: Backert, S. (eds) Inflammasome Signaling and Bacterial Infections. Current Topics in Microbiology and Immunology, vol 397. Springer, Cham. https://doi.org/10.1007/978-3-319-41171-2_12
Download citation
DOI: https://doi.org/10.1007/978-3-319-41171-2_12
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-41170-5
Online ISBN: 978-3-319-41171-2
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)