Abstract
Several units across Europe have established transoral robotic programs to treat patients diagnosed with obstructive sleep apnoea. The experiences of four countries, the UK, Belgium, Spain and Germany, are reported. Drug-induced sleep endoscopy (DISE) is universally used to guide patient selection. Although the indication, technique and peri-operative management may differ between countries, the outcomes are broadly similar with a 65 % rate of success reported. There are no consensus European guidelines for the application of TORS in OSA. However, it appears to be a promising treatment option in carefully selected patients particularly when DISE identifies collapse at the tongue base and epiglottis.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Vicini et al. first performed TORS for OSAH in Italy in 2008, as a modification of open tongue base reduction and hyoid epiglottopexy [1]. Since this time, several other units across Europe have established similar TORS programs to treat this condition. The following section provides an overview of the experience of four such programs from the UK, Belgium, Spain and Germany.
2 The UK Experience
2.1 Background
In the UK, the first robotic program in ENT was established at St. Mary’s Hospital, Imperial College London, by Mr. Neil Tolley and Mr. Asit Arora in 2009. A subsequent collaboration with Mr. Bhik Kotecha at the Royal National Throat Nose and Ear Hospital, London, was established in 2010 to apply TORS for treating patients with OSA who have failed conventional treatment modalities. This team has performed approximately 40 cases to date, carefully selecting patients using drug-induced sedation endoscopy (DISE) to identify potential candidates for TORS. Patients are eligible for treatment within the public (National Healthcare Service) system. Clinical evaluation is conducted within the context of a national ethically approved prospective study.
To date, there are 44 hospitals in the UK with a da Vinci system. In the last 3 years, six other ENT departments have established a robotic program although only one of these, in Newcastle, is also using TORS for patients with sleep-disordered breathing. As is the case in other countries, notably Belgium, there is the potential for many more departments to start a TORS program for OSAS given the number of hospitals in the UK with a da Vinci system. Nevertheless, as evident in Spain, access to the da Vinci is often restricted by its use in other specialties, particularly urology.
2.2 Guidelines and Patient Selection
To date there are no formal UK guidelines available. TORS is generally reserved as a ‘final option’ when all other existing treatment options have failed. Criteria for offering TORS for OSAH within the context of NHS healthcare provision include patients with (1) moderate-to-severe OSA confirmed by sleep study (defined as an apnoea-hypopnoea index (AHI) ≥15 episodes/h); (2) failure or refusal of all other treatment modalities including CPAP, mandibular advancement device (MAD), and surgery; (3) BMI less than 35 kg/cm2 and (4) predominant BOT collapse with or without epiglottic collapse evaluated by DISE. All patients undergo robotic-assisted tongue base reduction (TBR) and those with concurrent epiglottic prolapse identified by DISE, also undergo wedge epiglottoplasty. The possibility of intensive care admission, nasogastric tube insertion and tracheostomy is routinely included as part of the standard consent process.
2.3 Technique
Nasotracheal intubation is performed to facilitate access to the tongue base and epiglottis . The operating room configuration described by O’Malley et al. is used [2]. Tongue base reduction is performed by thulium laser ablation (2013 nm, 15 W), commencing in the midline from the foramen caecum and circumvallate papillae to the vallecula. A 1 cm mucosal bridge between the base of the epiglottis and the tongue represents the posterior limit and is employed to minimise oedema at the epiglottic base. The lateral limits are 1 cm to either side of the midline to a depth of 2 cm. Any excess lingual tonsillar tissue is additionally ablated down to muscle. Regarding epiglottic resection, a wedge-shaped laser excision of the upper one-half of the epiglottis is performed. The plane of resection is above the pharyngo-epiglottic folds to minimise the chance of aspiration and to avoid bleeding from branches of the superior laryngeal artery.
2.4 Peri-operative Management
All patients receive perioperative and post-operative steroids (dexamethasone 2 mg three times daily for 5 days) to minimise swelling, nausea and pain. In addition, antibiotics are given (co-amoxiclav 625 mg three times daily for 5 days), analgesia (paracetamol 1 g four times daily, ibuprofen 400 mg three times daily, and codeine 30 mg as required) and benzydamine hydrochloride gargles (4–6 times daily for 2 weeks). Usually patients are discharged within 24 h after surgery having been commenced on a soft diet. Nasogastric tube insertion and tracheostomy have not been required in any of the patients to date.
2.5 Outcome
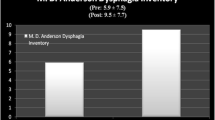
The preliminary results are encouraging and a 64 % cure rate has been achieved with a normal post-operative sleep study in 36 % of cases. No major complications have been witnessed. Minor bleeding which settled with conservative measures was a complication observed in one patient. The vast majority of patients start a soft diet immediately after surgery and swallow function returns to normal after 4 weeks. A sustained reduction in the mean Epworth Sleep Score and significant improvement in quality of life measures were evident 24 months following surgery [3].
2.6 Other Considerations
The TORS technique utilised in the UK can be but is usually not part of extensive multilevel surgery as reported in the literature by most other units. The laser ablation technique used for tongue base reduction may represent a less aggressive technique compared with resection. In accordance with others, TORS for BOT reduction can be safely performed without the need for tracheostomy or conversion to open surgery [4, 5]. A success rate of 64 % was achieved based on Sher criteria [6]. This is consistent with other studies that report success rates of 45–90 % with TORS [4, 7–10].
3 The Belgian Experience
3.1 Background
In Belgium over 30 hospitals currently use the da Vinci system for urological and gynecological procedures . Since the approval of TORS by the FDA in 2009, approximately ten ENT departments established a robotic program. Of these, four use TORS for sleep-disordered breathing: AZ Sint-Jan Hospital Bruges—Ostend, University Hospital Antwerp, AZ Sint-Lucas Hospital Ghent and University Hospital Namur. Considering the number of robotic systems in Belgium, there is a high potential for ENT departments to start a TORS programme for OSAS in the future.
3.2 Guidelines and Patient Selection
To date there are no Belgian guidelines available. On a European level, the European Respiratory Society (ERS) task force report concerning non-CPAP therapies for OSAS does not mention TORS [11]. TORS should be seen as another way of performing conventional procedures of the oropharynx . Therefore, guidelines of these conventional procedures should apply to robotic procedures, but possibly with better outcome.
The main indication for TORS in sleep-disordered breathing is OSAS. We consider TORS in an OSAS patient when CPAP is not tolerated or wanted by the patient, or when CPAP is not reimbursed (apnoea hypopnoea index (AHI) of less than 20 per hour). Occasionally, TORS is used in patients with isolated snoring. In such cases, these patients need to be strongly motivated.
Surgery is performed in centres where there is a specific multidisciplinary programme for OSAS and snoring. Patient evaluation is always performed in close collaboration with colleagues from respiratory medicine, maxillofacial surgery and neurology and consists of clinical examination, laryngoscopy and polysomnography.
When surgery is considered DISE is performed to select patients for the most appropriate surgical procedure. Tongue base collapse should be observed on DISE prior to consideration of TORS-assisted tongue base reduction. Belgian centres consider TORS as a better alternative to perform tongue base reduction than laser surgery.
If necessary, an additional simultaneous procedure to address the soft palate and lateral pharynx may be indicated and selected accordingly.
Mandibular advancement treatments (with osteotomies or a device) are recognised as a valuable alternative.
Finally, patients are informed about the additional cost of TORS. If this is a financial problem for the patient, trans-oral laser surgery (TLS) is an option, although we believe that this is a less optimal operative technique.
3.3 Technique
As with other surgical procedures, it is difficult to describe a uniform technique for different centres. Most hospitals use the da Vinci Si system, and some the MedRobotics-Flex-System . Some centres only do isolated robotic tongue base procedures whilst others combine this with conventional oropharyngeal surgery. Some always perform epiglottoplasty when reducing the tongue base whilst others only do so when circular collapse of the epiglottis is witnessed at DISE. As is the case in the UK and Spain, tracheostomy is not routinely performed in TORS. In our centre we use the 30° endoscope, the Maryland bipolar forceps and the unipolar cautery installed at the three robotic arms.
3.4 Other Considerations
Because of the strict selection criteria, TORS for sleep-disordered breathing is not a common procedure. Approximately 90 robotic sleep-disordered breathing procedures were performed in Belgium in the last 5 years. In this way we feel that it is important to perform TORS for head and neck cancer and chronic lingual tonsillar hypertrophy to improve expertise and to shorten the learning curve.
4 The Spanish Experience
4.1 Background
As in many other countries in Europe, treatment of oropharyngeal pathology has been performed using trans-oral laser microsurgery (TLM ) in recent years. Thus, the introduction of TORS to treat such cases has been delayed to some extent by this practice and the TLM expertise evident across the country.
In 2011, the first TORS case was performed in Pamplona, in 2011, after Dr. Peter Baptista had been trained in TORS. Although the da Vinci system is available throughout many hospitals in Spain, TORS as a treatment for OSA is only performed in a few selected centres. This includes two private hospitals (Clínica Universitaria de Navarra, Pamplona, and Hospital Sanitas La Zarzuela, Madrid) and a public hospital (Hospital Rey Juan Carlos, Móstoles, Madrid). Just recently, two more hospitals in Madrid have acquired a da Vinci robot and may start a TORS programme. Specifically, at Hospital Quiron (Madrid), Prof. Julio Acero, a maxillofacial surgeon, has been recently trained in TORS. In contrast, the public system of hospitals does not promote any TORS program, although there are several robots available.
4.2 Guidelines and Patient Selection
In Spain there are national guidelines for OSA diagnosis and treatment. However, this does not include tongue base surgery of any kind. Therefore, for every patient, the correct indication must be established through a complete physical exam and significant findings during DISE. The latter is in accordance with the DISE protocol established to diagnose and manage OSA patients. Thereafter, local OSA committees are key to help to find the right candidates. Potential candidates for TORS are similar to those in the UK, namely patients with OSA when the AHI is >25 and CPAP is not tolerated.
4.3 Technique
In contrast to UK practice, surgery is usually performed in a multilevel fashion, with pharyngoplasty and/or septoplasty also performed as indicated. The da Vinci Si system is currently used to perform tongue base reduction and epiglottoplasty and in keeping with other European centres, tracheostomy is not routinely performed [6, 8, 11–13].
In total, we have performed TORS in approximately 70 cases of OSA across three hospitals in Spain over the last 4 years. The team at Pamplona has performed 43 cases, 16 cases have been performed at Hospital Sanitas La Zarzuela and in Móstoles, in the public system, three TORS cases have been performed for OSA. It is noticeable that in the private hospital setting it is easier to establish and perform a programme of TORS for OSA compared to the public sector. This is because in the latter, use of the robot is more restricted in non-oncological cases.
4.4 Outcome
Different authors have reported success in most cases. Our results are similar, with AHI reductions by half in more than 80 % patients, when TORS has been correctly indicated and performed. Nevertheless, complications are an important issue [14]. Bleeding after the procedure has been a major problem in three cases (out of 70) with one patient requiring an emergency tracheostomy . Pain and severe dysphagia lasting as long as 3 weeks are common and patients should be appropriately consented [15].
4.5 Other Considerations
Establishing a TORS programme is associated with numerous challenges. Once the robot is available in any hospital in Spain, it usually ‘belongs’ to the urologic department, which is able to easily perform 50–75 cases per year. It is very important to discuss the need to use the robot for TORS with the local managers so that we are ‘allowed’ to use this equipment on a regular basis. When using the laser, usually it is to the contrary: this equipment traditionally ‘belongs’ to the ENT department.
Cost is also an important issue. Our health system does not cover the additional costs that TORS require. Once TORS has been proposed to a patient, it is the responsibility of their local ENT team to search for the necessary financial support to make surgery possible. This is difficult in the public setting and very demanding for the patient in the private sector.
Going forward, patient selection for TORS needs to be optimised. DISE is a mandatory tool in this regard [16]. MRI may also provide important additional information to determine how much tissue needs to be removed during TORS and to establish the exact location of lingual arteries and branches to avoid unnecessary damage and bleeding [16].
Furthermore, the TORS technique should also be improved. Maryland forceps were not designed for TORS and better grasping forceps are needed. Decreasing the optic size and increasing the flexibility of surgical instruments would also be beneficial.
5 The German Experience
5.1 Background
In general, trans-oral surgery has been practiced in Germany for many decades, mostly in the form of trans-oral laser surgery (TLS ). Consequently, TLS is established as a standard therapy for benign and malignant disease, as well as in OSAS surgery [18–21]. Therefore, as is the situation in Spain, TORS has had to ‘compete’ with TLS. Comparative studies have not been published, so the benefit of TORS over TLS is not proven. In our own experience, TLS has a broad spectrum of indications and regarding patient outcome TORS seems to be at least as good as TLM in selected patient groups.
Following FDA approval of TORS in 2009, ENT departments across the country began to adopt this technique. At the present time, nine centres (out of 38 university hospitals and an additional 120 ENT departments) have an established robotic programme. These are the University Hospital Heidelberg (2010); University Hospital Essen (2011); University Hospital Hamburg (2011); Prosper Hospital Recklinghausen (2011); University Hospital Erlangen (2012); University Hospital Marburg (2012); University Hospital Homburg (2012); St. Elizabeth Hospital Straubing (2012) and University Hospital Ulm (2013). Approximately 20 additional otolaryngology departments have the potential to start a TORS programme due to the fact that there is a da Vinci system available in their hospital.
5.2 Guidelines and Patient Selection
Regarding the use of TORS in OSAS surgery, TORS has not been included in German guidelines of operative therapy for OSAS or snoring thus far [22, 23].
5.3 Technique
In our opinion TORS simply represents another technique to perform an operation, so strategies like reduction of base of tongue or UVPP can be performed by TORS as well as by conventional operation techniques. Consequently, in Marburg, we performed ten operations with focus on surgical OSAS therapy using two robotic systems: the da Vinci and the MedRobotics-Flex-System .
5.4 Outcome
The advantage of TORS in comparison with TLS was the improvement of visualisation, especially in base of tongue due to the 30°-angled optic system. Other German centres report similar experiences in personal discussion.
5.5 Other Considerations
The delayed adoption of TORS is at least in part due to the differences in health-care structure in Germany compared to the USA. In Germany, the health system is based on diagnose-related-group-system (DRG) where insurance providers do not cover the additional costs which are about 800–1000€ per case [4–23].
Another factor related to poor adoption is the issue concerning the reprocessing of used instruments and the need for different cleaning techniques for robotic equipment. This has led to the establishment of a completely new set of procedures of reprocessing, i.e. cleaning, disinfection and sterilisation, which have to be altered and adapted to the German regulations of the Commission for Hospital Hygiene and Infection Prevention at the Robert Koch Institute (RKI), the Federal Institute for Drugs and Medical Devices (BfArM) and the DIN EN ISO 17664 [24].
6 Summary
TORS for OSA is only established in a few selected centres in the UK, Germany, Spain and Belgium. There are no consensus national guidelines for TORS and OSA and as a result TORS is only being used for sleep-disordered breathing in a fraction of centres. Careful patient selection on a case-by-case basis and in a multidisciplinary setting is important. In all the European centres reported, TORS represents a new treatment paradigm for OSA patients that do not tolerate CPAP. DISE is universally used to guide patient selection and the surgical technique is particularly useful to treat tongue base hypertrophy and epiglottic prolapse .
References
Vicini C, Dallan I, Canzi P, Frassineti S, La Pietra MG, Montevecchi F. Transoral robotic tonge base resection in obstructive sleep apnoea-hypopnoea syndrome: a preliminary report. ORL J Otorhinolaryngol Relat Spec. 2010;72(1):22–7.
O’Malley Jr BW, Weinstein GS, Snyder W, Hockstein NG. Transoral robotic surgery (TORS) for base of tongue neoplasms. Laryngoscope. 2006;116:1465–72.
Arora A, Tolley N, Kotecha B, et al. Functional outcomes after Transoral robotic surgery for obstructive sleep apnoea. Clin Otol. 2012;37(S1):97.
Friedman M, Hamilton C, Samuelson CG, Kelley K, Taylor D, Pearson-Chauhan K, Maley A, Taylor R, Venkatesan TK. Transoral robotic glossectomy for the treatment of obstructive sleep apnea-hypopnea syndrome. Otolaryngol Head Neck Surg. 2012;146:854–62.
Lin HS, Rowley JA, Badr MS, Folbe AJ, Yoo GH, Victor L, Mathoq RH, Chen W. Transoral robotic surgery for treatment of obstructive sleep apnea-hypopnea syndrome. Laryngoscope. 2013;123:1811–6.
Arora A, Chaidas K, Garas G, Amlani A, Darzi A, Kotecha B, Tolley NS. Outcome of TORS to tongue base and epiglottis in patients with OSA intolerant of conventional treatment. Sleep Breath. 2015 Dec 15 Ahead of print.
Lee JM, Weinstein GS, O’Malley Jr BW, Thaler ER. Transoral robotic-assisted lingual tonsillectomy and uvulopalatopharyngoplasty for obstructive sleep apnea. Ann Otol Rhinol Laryngol. 2012;121:636–9.
Vicini C, Montevecchi F, Campanini A, Dallan I, Hoff PT, Spector ME, Thaler E, Ahn J, Baptista P, Remacle M, Lawson G, Benazzo M, Canzi P. Clinical outcomes and complications associated with TORS for OSAHS: a benchmark for evaluating an emerging surgical technology in a targeted application for benign disease. ORL J Otorhinolaryngol Relat Spec. 2014;76:63–9.
Toh ST, Han HJ, Tay HN, Kiong KL. Transoral robotic surgery for obstructive sleep apnea in Asian patients: a Singapore sleep centre experience. JAMA Otolaryngol Head Neck Surg. 2014;140:624–9.
Randerath WJ, Verbraecken J, Andreas S, Bettega G, Boudewyns A, Hamans E, et al. ERS Task Force Report: non-CPAP therapies in obstructive sleep apnoea. Eur Respir J. 2011;37:1000–28.
Vicini C, Montevecchi F, Tenti G, et al. Transoral robotic surgery: tongue base reducction and supraglottoplasty for obstructive sleep apnea. Oper Tech Otolaryngol. 2012;23:45–7.
Vicini C, Dallan I, Canzi P, et al. Transoral robotic surgery of the tongue base in obstructive sleep Apnea-Hypopnea syndrome: anatomic considerations and clinical experience. Head Neck. 2012;34:15–22.
Vicini C, Montevecchi F, Pang K, et al. Combined transoral robotic tongue base surgery and palate surgery in obstructive sleep apnea-hypopnea syndrome: expansion sphincter pharyngoplasty versus uvulopalatopharyngoplasty. Head Neck. 2014;36:77–83.
Hoff PT, D'Agostino MA, Thaler ER. Transoral robotic surgery in benign diseases including obstructive sleep apnea: safety and feasibility. Laryngoscope. 2015;125:1249–53.
Eesa M, Montevecchi F, Hendawy E, et al. Swallowing outcome after TORS for sleep apnea: short- and long-term evaluation. Eur Arch Otorhinolaryngol. 2015;272:1537–41.
Lin HS, Rowley JA, Folbe AJ, et al. Transoral robotic surgery for treatment of obstructive sleep apnea: factors predicting surgical response. Laryngoscope. 2015;125:1013–20.
Chiffer RC, Schwab RJ, Keenan BT, et al. Volumetric MRI analysis pre and post transoral robotic surgery for obstructive sleep apnea (OSA-TORS). Laryngoscope. 2015;125:1988–95.
Werner JA. Transoral laser microsurgery in carcinomas of the oral cavity, pharynx, and larynx. Cancer Control. 2002;9(5):379–86.
Rudert HH. Endoscopic resections of glottic and supraglottic carcinomas with the CO2 laser. Eur Arch Otorhinolaryngol. 1995;252(3):146–8.
Steiner W. Transoral laser microsurgery for squamous cell carcinoma of the base of the tongue. Arch Otolaryngol Head Neck Surg. 2003;129(1):36–43.
Ambrosch P. Carbon dioxide laser microsurgery for early supraglottic carcinoma. Ann Otol Rhinol Laryngol. 1998;107(8):680–8.
Verse T. Guideline: treatment of obstructive sleep apnea in adults. HNO. 2009;57(11):1136–56.
Stuck BA. Diagnosis and treatment of snoring in adults-S2k Guideline of the German Society of Otorhinolaryngology, Head and Neck Surgery. Sleep Breath. 2015;19(1):135–48.
Mandapathil M. Establishing a transoral robotic surgery program in an academic hospital in Germany. Acta Otolaryngol. 2014;134:661–5.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Arora, A., Kotecha, B., Vauterin, T., Plaza, G., Güldner, C., Werner, J.A. (2016). The European Experience. In: Vicini, C., Hoff, P., Montevecchi, F. (eds) TransOral Robotic Surgery for Obstructive Sleep Apnea. Springer, Cham. https://doi.org/10.1007/978-3-319-34040-1_22
Download citation
DOI: https://doi.org/10.1007/978-3-319-34040-1_22
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-34038-8
Online ISBN: 978-3-319-34040-1
eBook Packages: MedicineMedicine (R0)