Abstract
The management of acute type B aortic dissection (TBAD) has largely been dictated by whether or not the case is “complicated,” meaning symptomatic or extensive such that no intervention would lead to death. Historically, complicated acute TBAD has been managed with operative intervention and uncomplicated acute TBAD has been managed with medical treatment. Acute complicated TBAD left untreated has mortality rates as high as 50 % in the first month. While uncomplicated acute TBAD has good outcomes with medical management in the short-term, long-term outcomes are discouraging with mortality rates approaching 30–50 % at 5 years, largely due to aneurysmal degeneration of the false lumen. Both open and endovascular treatment strategies have a role in both complicated and uncomplicated acute TBAD and the role of endovascular intervention is ever-expanding as research shows favorable short-term outcomes and long-term aortic remodeling.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
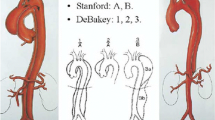
Aortic dissection is a relatively uncommon disease, with an incidence of 3.5–14 per 100,000 persons per year [1–4]. Acute TBAD accounts for 24–40 % of all aortic dissections and may be classified as complicated or uncomplicated. Complicated acute TBAD refers to the presence of rupture, malperfusion, continued pain, or hypertension with maximum medical management. While complicated acute TBAD accounts for a minority of cases, these cases require surgical repair. Uncomplicated acute TBAD has typically been managed medically with blood pressure control and anti-impulse therapy. With this approach, in-hospital mortality rates remain low, typically less than 10 %. However, long-term results remain disappointing due to aneurysmal expansion of the false lumen and late complications [5–7].
Current review of short- and long-term outcomes is showing the increasing role for early repair of both complicated and uncomplicated acute TBAD. In 1999, thoracic endovascular aortic repair (TEVAR) was introduced as an alternative surgical intervention for TBAD and proceeded to obtain FDA approval in 2005. Since the introduction of endovascular techniques for repair, an increasing number of surgical cases have been performed with a resultant decrease in short-term mortality [3, 4, 6]. Long-term results are limited since the recent paradigm shift towards early endovascular repair has only occurred in the last decade, however favorable outcomes with respect to aortic remodeling are promising in decreasing the occurrence of late aneurysmal degeneration [8–10].
Search Strategy
A literature search of English language publications from 2000 to present was performed to identify published data regarding acute type B aortic dissection management and intervention using the PICO outline (Table 1.1). The databases searched were PubMed, OVID Medline, and Cochrane Evidence Based Medicine. Terms searched included “acute aortic dissection,” “descending aortic dissection,” “type B aortic dissection,” AND (“complicated” OR “uncomplicated” OR “surgical treatment” OR “medical treatment”). Articles were excluded if they included type A aortic dissection. One Cochrane review, two randomized trials, one prospective registry review, two expert guidelines, and two review articles were included in our analysis. The data was classified using the GRADE system.
Results
Early Guidelines Summary
Contemporary management of acute type B aortic dissection has evolved over the last 15 years. In 2001 the European Society of Cardiology sought to review current diagnosis and management strategies regarding aortic dissection and provide recommendations and guidelines regarding optimal treatment [11]. This established the first set of society guidelines for aortic dissection. A task force of 11 members included one member appointed by the American College of Cardiology to include endorsement from that group as well. The group recommended strict heart rate and blood pressure control with beta-blockers and nitroprusside upon admission. Emergent operative repair was recommended in instances of hemodynamic instability. Other indications for operative repair in TBAD included persistent or recurrent chest pain, aortic expansion, periaortic hematoma, and mediastinal hematoma. Endovascular therapy was described as an evolving technique with goals of fenestration with or without stent placement for coverage of entry tears and relieving malperfusion due to the tears. However, the supporting evidence for endovascular intervention at this time was largely based on case reports and only awarded a GRADE “very low” quality of evidence. This paper served as the first formal guidelines supported by a society in the treatment of acute type B aortic dissections.
Prospective Registry- International Registry of Acute Aortic Dissection (IRAD)
Interest in better delineating the treatment and outcome of acute aortic dissection led to the need for a robust database, culminating in the creation of the International Registry of Acute Aortic Dissection (IRAD) in 1996. All patients with acute aortic dissection confirmed by imaging, visualization in the operating room, or at autopsy are included and data are enrolled prospectively and a questionnaire of 290 variables is used to collect data. Initially, patients were enrolled from 12 centers in 6 countries, and now this has expanded to 24 referral centers in 11 countries. Reports from the IRAD database are published periodically [5, 12, 13].
In 2008 Fattori et al. analyzed the impact of different treatment strategies on survival in patients in the IRAD database [12]. This review included 571 patients with acute type B aortic dissection who were enrolled in the database between 1996 and 2005. Of these patients, 390 were treated medically and 125 were treated surgically. The surgical treatment group included 59 patients who underwent open repair and 66 patients who were treated with an endovascular approach. All patients were initially treated with aggressive antihypertensive and anti-impulse therapy. The patients undergoing open intervention suffered either extension of dissection, recurrent or refractory pain, visceral ischemia, or limb ischemia. The reasons for endovascular treatment included recurrent or refractory pain, and limb or visceral ischemia. Endovascular techniques employed in this group included stent graft repair as well as endovascular balloon fenestration of the dissection flap. Mortality in the endovascular treatment group was 10.6 %, while mortality in the open surgical group was 33.9 % (P = .002). In-hospital complications, including stroke, spinal cord ischemia, myocardial infarction, acute renal failure, limb ischemia, and mesenteric ischemia were observed in 20.8 % of the patients undergoing endovascular intervention, and in 40.0 % of the patients undergoing open surgical repair (P = .04). Patients with uncomplicated acute TBAD were treated with medical therapy only and mortality in this group was similar to that of the complicated acute TBAD group treated with endovascular therapy. This report demonstrated the likely better short-term outcomes of endovascular repair versus open surgical repair of complicated acute TBAD with respect to mortality and in-hospital complications. However, long-term follow-up was lacking and no comparison directly between medical therapy and endovascular treatment was available.
As a follow-up to this analysis, Fattori et al. reviewed the IRAD database to compare medical therapy to thoracic endovascular aortic repair (TEVAR) therapy [13]. This review included 1129 patients enrolled between December 26, 1995 and January 20, 2012, 853 of whom were treated exclusively with medical therapy, and 276 of whom were treated with endovascular stent-graft placement in addition to medical therapy. Of note, patients undergoing endovascular treatment were more likely to present with signs of malperfusion, pre-operative renal failure, and pulse deficit. Additionally, endovascular therapy was more frequently used in European centers compared to North American sites. Despite these differences in the patient populations, in-hospital mortality was similar between the two groups with 10.9 % mortality in the endovascular group and 8.7 % in the medically treated group (P = .273). Complications in this acute phase, including renal failure, stroke, spinal cord ischemia, and extension of dissection, were more common in the TEVAR group (38.9 % vs. 17.8 %). At 1-year post-discharge, the mortality was 8.1 % in the patients treated with TEVAR and 9.8 % in the patients treated with medical therapy alone, though this was not statistically significant (P = .604). Kaplan-Meier estimates were modeled for 5-year follow-up and projected a lower mortality rate for those patients undergoing endovascular treatment versus medical therapy alone (15.5 % vs. 29.0 %, P = .018). While late intervention rates were projected to be more common after TEVAR (30.6 % vs. 19.7 %), this was not anticipated to be significant (P = .810). Additionally, projections demonstrated a smaller descending aortic diameter in the group treated with TEVAR as compared to the medical therapy group with median diameter of 4.2 cm for the TEVAR group and 4.6 cm for the medical therapy group (P = .034). The analysis from this review demonstrates similar long-term mortality between patients treated with TEVAR versus medical therapy alone as well as favorable long-term aortic remodeling in patients undergoing TEVAR.
Prospective Trials
While IRAD does provide “real-world” review of acute aortic dissection, it lacks the rigor of a randomized study to provide better comparison of outcomes between medical therapy alone versus medical therapy and operative intervention. The Investigation of Stent Grafts in Aortic Dissection (INSTEAD) Trial was the first randomized trial to compare TEVAR and medical therapy for subacute TBAD [14]. Nienaber et al. recruited 140 patients in stable clinical condition between November 2003 and November 2005 and randomized to elective stent-graft placement in addition to medical therapy or to medical therapy alone. Seventy-two patients were randomized to the TEVAR group and 68 were randomized to the medical treatment group, with no significant differences noted between the two study groups. Patients undergoing TEVAR had TALENT stent grafts placed (Medtronic, Inc, Santa Rosa, CA). At 2-year follow-up, overall survival was 88.9 % in the TEVAR group and 95.6 % in the medical therapy group (P = .145). Freedom from aorta-related mortality at 2 years was also not significantly different between the two groups, 94.4 % for the TEVAR group and 97.0 % for the medical treatment group (P = .435). Similarly, there was no difference in progression of aortic disease, 77.2 % for the TEVAR group and 72.5 % for the medical treatment group (P = .545). Of note, there was a significant trend towards decreased false-lumen diameter with concomitant increase in true-lumen diameter in the TEVAR group at the 3-month, 1-year, and 2-year follow-up. Additionally, complete false-lumen thrombosis at 2 years was achieved in 91.3 % of patients undergoing TEVAR and only 19.4 % of patients undergoing medical therapy (P < .001). The overall observed mortality rate was lower than expected, leading to the study being underpowered. However, this study did confirm that TEVAR leads to favorable aortic remodeling and false-lumen thrombosis, fostering the argument for the expanded role for operative intervention in subacute TBAD, even in uncomplicated cases traditionally managed with medical therapy alone.
Nienaber et al. followed INSTEAD with INSTEAD-XL, the 5-year follow-up of the randomized study [9]. While all-cause mortality was not significantly different at 2 years, there was a significant survival benefit seen with TEVAR between 2 and 5 years with 100 % of TEVAR patients surviving that time frame compared to 83.1 % of the medical treatment group (P = .0003). Similarly, there was a significant decrease in aorta-specific mortality between 2 and 5 years for the TEVAR group, with no patients from the TEVAR group experiencing aorta-specific mortality between 2 and 5 years. At 5 years, the overall aorta-specific mortality was 6.9 % for the TEVAR group and 19.3 % for the medical treatment group (P = .045). TEVAR also out-performed medical treatment between years 2 and 5 with respect to progression of disease and aorta-specific events, with 95.9 % of TEVAR patients free from these events compared to 71.9 % of medical treatment patients (P = .004). False lumen thrombosis and aortic remodeling was favorable in the TEVAR group with complete thoracic false lumen thrombosis in 90.6 % and morphologic remodeling in 79.2 % at 5 years. The medical treatment group was conversely associated with an increase in aortic diameter in 66.0 % and only demonstrated false lumen thrombosis in 22.0 % at 5 years. INSTEAD-XL demonstrated that while TEVAR was associated with excess early mortality largely due to peri-procedural risks, TEVAR was beneficial in treatment of subacute TBAD with respect to overall mortality, aorta-specific mortality, aortic remodeling, and false lumen thrombosis with a number needed to treat of 13.
While the INSTEAD-XL trial demonstrated long-term improvement in outcomes for patients with subacute uncomplicated TBAD, studies are undergoing to determine the impact of endovascular repair in complicated TBAD. The Study for the Treatment of complicated Type B Aortic Dissection using Endoluminal repair (STABLE) trial is a prospective, multicenter study to evaluate the use of proximal stent grafting with distal bare metal stents (Zenith Dissection Endovascular System; Cook Medical, Bloomington, IN) in the treatment of complicated TBAD. Lombardi et al. recently reported 2-year results with the system [8]. Eighty-six patients enrolled between December 2007 and February 2012 were reviewed, all of whom underwent treatment within 90 days of symptom onset. Inclusion criteria included impending rupture, resistant hypertension, persistent pain or symptoms, aortic growth greater than 5 mm in 3 months or transaortic diameter greater than 40 mm, and evidence of branch vessel obstruction or compromise. The 30-day mortality was 4.7 %. The freedom from all-cause mortality was 88.3 % at 1 year and 84.7 % at 2 years. The freedom from dissection-related mortality, based on the evaluation of a clinical events committee, was 90.6 % at 1 year and 89.3 % at 2 years. Subgroup analysis of patients with acute and non-acute dissections did not reveal any difference in overall mortality or dissection-related mortality. Overall complication rates were low, with paraplegia only occurring in one patient, renal failure in 9 patients, aortic rupture in 5 patients, stroke in 7 patients, and retrograde dissection in 7 patients during the 2 years studied, although the majority of complications were found among patients treated in the acute phase. Complete false lumen thrombosis was 43.5 % at 2 years (P < .001). The study also evaluated the changes in true-lumen, false-lumen, and transaortic diameters. At 2 years, the true lumen diameter increased significantly in the descending thoracic aorta and distal abdominal aorta. The false lumen diameter decreased significantly in these segments as well at 2 years. The authors concluded that the combined stent graft with distal bare metal stent in complicated TBAD leads to favorable mortality and morbidity rates as well as leading to favorable aortic remodeling at 2 years with respect to true lumen size, false lumen size and thrombosis, and transaortic size.
The first prospective randomized trial on acute type B aortic dissection, the Acute Dissection Stentgraft OR Best Medical Treatment (ADSORB) trial, recently published its preliminary findings [15]. Sixty-one patients were recruited from 17 European centers and randomized from December 2008 to December 2010. Thirty-one patients were randomized to best medical therapy (BMT) and 30 patients were randomized to BMT and TEVAR. The Gore TAG device (W. L. Gore & Associates, Inc. Flagstaff, AZ) was used for endovascular repair, which was performed within 48 h of randomization. The composite endpoint studied included incomplete or no false lumen thrombosis, aortic dilatation greater than 5 mm or maximum diameter of the descending thoracic aorta greater than 55 mm, and aortic rupture. No deaths occurred in either group at 30 days. At 1 year, the composite endpoint was met by 100 % of the patients in the BMT group and only 50 % in the TEVAR group (P < .001). No aortic rupture occurred in either study group. No false lumen thrombosis occurred in 97 % of the BMT group and only 43 % of the TEVAR group (P < .001). Of note, similar rates of aortic dilatation were noted between the two study groups with 37 % of the TEVAR group and 45 % of the BMT group experiencing aortic dilatation (P = .5). While the study was not powered for mortality, the authors concluded that the BMT only group results were inferior those seen the TEVAR group, supporting TEVAR for acute uncomplicated TBAD.
Guidelines Summary
Since results from IRAD, INSTEAD and INSTEAD-XL, STABLE, and ADSORB have been available, new reviews and society guidelines regarding treatment recommendations for aortic dissection have been established. Ulug et al. performed a Cochrane review of uncomplicated chronic subacute type B aortic dissection, largely based on INSTEAD results and while unable to make any specific practice recommendations, supported the idea that early endovascular interventions lead to favorable aortic remodeling and may likely be of long-term benefit [16]. Erbel et al. through the Task Force for the Diagnosis and Treatment of Aortic Diseases updated the European Society of Cardiology (ESC) guidelines first set in 2001 [17]. With respect to uncomplicated TBAD, the ESC recommends medical therapy with Class I, Level C support and consideration of TEVAR with Class IIa, Level B support. For complicated TBAD, TEVAR was recommended with Class I, Level C support. Open surgery for complicated TBAD may be considered based on Class IIb, Level C support. The recommendations of the ESC demonstrate the evolving practice patterns and outcomes for TBAD over the last 15 years since the introduction of endovascular thoracic aortic repair for dissection.
Fattori et al. recently provided an interdisciplinary expert consensus document on the management of TBAD [18]. They reviewed data from 63 studies published from 2006 to 2012 with a total of 1548 patients treated medically, 1706 patients treated with open surgery, and 3457 patients treated with TEVAR. The expert panel recommended medical treatment for uncomplicated acute TBAD as there was no good evidence demonstrating a benefit of TEVAR or open surgery over medical treatment. For patients with complicated acute TBAD, the group suggests that TEVAR should be considered as first-line treatment as a survival benefit has been demonstrated over open surgical treatment. Because of aneurysmal degeneration and rupture risk in patients treated medically, as well as the possibility of adverse aortic events after TEVAR, both groups of patients should be followed closely with serial imaging, particularly in the first few months. The group cautioned that the data available currently is lacking in robust randomized trials and there are gaps in reporting standards of the studies available for review.
Recommendations
The management and treatment of acute TBAD has evolved over the last 15 years. Multiple studies and reviews have been performed to evaluate the impact of medical treatment, endovascular repair, and open repair on acute TBAD, and more studies are underway. Randomized controlled studies are few and typically underpowered, leading to recommendations based on imperfect data, and therefore any recommendation must be reviewed with caution.
With respect to acute uncomplicated TBAD, optimum medical treatment is still the standard of care. Low quality evidence exists from the ADSORB trial that demonstrates favorable aortic remodeling and false lumen thrombosis with TEVAR in this group. If using uncomplicated chronic TBAD as a marker for those cases with acute uncomplicated TBAD that continue to be uncomplicated, the INSTEAD-XL trial demonstrates low to moderate quality evidence for the use of TEVAR in this patient population.
For patients with acute complicated TBAD, good evidence exists that TEVAR is superior to open surgical intervention and should be utilized as first-line intervention. Data from IRAD and STABLE have shown decreased mortality, increased false lumen thrombosis, and decreased aortic size with TEVAR in patients with acute complicated TBAD.
Personal View of the Data
Acute TBAD requires consideration of acute events and pathology such as rupture, malperfusion, and ongoing symptomatology as well as anticipation of long-term sequelae and risks such as aneurysmal degeneration, aortic-related death, and recurrent symptoms. All patients require timely and strict medical management with blood pressure control and anti-impulse treatment. While there are good data that demonstrate TEVAR is the intervention of choice in those patients with complicated TBAD, there is a paucity of rigorous randomized trials for uncomplicated TBAD. All of the attempted randomized controlled trials suffer from low enrollment and inability to reach sufficient power as contemporary medical treatment has decreased the overall mortality rate, requiring more patients to be enrolled to detect a difference.
The ADSORB trial provides an opportunity to address this shortcoming, though its first results are lacking and fail to definitively show a survival benefit and, in fact, showed no difference in aortic dilation between the two treatment groups. More time is needed for enrollment to reach adequate numbers, and long-term follow-up will be needed to see the true impact of the study. However, given the evidence from the INSTEAD-XL trial and large analyses, we hypothesize that TEVAR does have a role in the treatment of uncomplicated subacute TBAD, though the extent of that role is yet to be determined.
Currently, much of the research focus regarding endovascular intervention for TBAD is centered on false lumen thrombosis in the thoracic aorta as a marker for aortic remodeling and eventual mitigation of the risk of aneurysmal degeneration. However, we believe that this data is incomplete and does not address the more difficult issue of outcomes related to the abdominal aorta and the difficulty in managing residual disease that may affect the visceral vessels. To date, no study has seriously studied the long-term effects of TEVAR for TBAD on the abdominal aorta, which will be needed to fully appreciate the impact of these interventions.
Summary of Recommendations
-
For patients with acute uncomplicated TBAD, we recommend optimum medical therapy and close surveillance to follow progression of disease. (evidence quality moderate, strong recommendation)
-
For patients with acute complicated TBAD, we recommend TEVAR in addition to optimum medical therapy and close surveillance. (evidence quality moderate, strong recommendation)
-
TEVAR may be of benefit in subacute uncomplicated TBAD (evidence quality low, weak recommendation)
References
Howard DPJ, Banerjee A, Fairhead JF, Perkins J, Silver LE, Rothwell PM. Population-based study of incidence and outcome of acute aortic dissection and premorbid risk factor control. Circulation. 2013;127:2031–7.
Zahn R, Erbel R, Nienaber C, Neumann F, Nef H, Eggebrecht H, et al. Endovascular aortic repair of thoracic aortic disease: early and 1-year results from a German multicenter registry. J Endovasc Ther. 2013;20:265–72.
Parker J, Golledge J. Outcome of endovascular treatment of acute type B aortic dissection. Ann Thorac Surg. 2008;86:1707–12.
Golledge J, Eagle K. Acute aortic dissection. Lancet. 2008;372:55–66.
Tsai T, Trimarchi S, Nienaber C. Acute aortic dissection: perspectives from the International Registry of Acute Aortic Dissection (IRAD). Eur J Vasc Endovasc Surg. 2009;37:149–59.
Wilkinson D, Patel H, Williams D, Dasika N, Deeb G. Early open and endovascular thoracic aortic repair for complicated type B aortic dissection. Ann Thorac Surg. 2013;96:23–30.
Ehrlich M, Rousseau H, Heijmen R, Piquet P, Beregi J, Nienaber C, et al. Midterm results after endovascular treatment of acute, complicated type B aortic dissection: the talent thoracic registry. J Thorac Cardiovasc Surg. 2013;145:159–65.
Lombardi J, Cambria R, Nienaber C, Chiesa R, Mossop P, Haulon S, et al. Aortic remodeling after endovascular treatment of complicated type B aortic dissection with the use of a composite device design. J Vasc Surg. 2014;59:1544–54.
Nienaber C, Kische S, Rousseau H, Eggebrecht H, Rehders T, Kundt G, et al. Endovascular repair of type B aortic dissection: long-term results of the randomized investigation of stent grafts in aortic dissection trial. Circ Cardiovasc Interv. 2013;6:407–16.
Qin Y, Deng G, Li T, Wang W, Teng G. Treatment of acute type-B aortic dissection: thoracic endovascular aortic repair or medical management alone? J Am Coll Cardiol Intv. 2013;6:185–91.
Erbel R, Alfonso F, Boileau C, Dirsch O, Eber B, Haverich A, et al. Diagnosis and management of aortic dissection: recommendations of the Task Force on Aortic Dissection, European Society of Cardiology. Eur Heart J. 2001;22:1642–81.
Fattori R, Tsai T, Myrmel T, Evangelista A, Cooper J, Trimarchi S, et al. Complicated acute type B dissection: is surgery still the best option? J Am Coll Cardiol Intv. 2008;1:395–402.
Fattori R, Montgomery D, Lovato L, Kische S, Di Eusanio M, Ince H, et al. Survival after endovascular therapy in patients with type B aortic dissection: a report from the International Registry of Acute Aortic Dissection (IRAD). J Am Coll Cardiol Intv. 2013;6:876–82.
Nienaber C, Rousseau H, Eggebrecht H, Kische S, Fattori R, Rehders T, et al. Randomized comparison of strategies for type B aortic dissection: the investigation of stent grafts in aortic dissection (INSTEAD) trial. Circulation. 2009;120:2519–28.
Brunkwall J, Kasprzak P, Verhoeben E, Heijmen R, Taylor P, the ADSORB trialists, et al. Endovascular repair of acute uncomplicated aortic type B dissection promotes aortic remodeling: 1 year results of the ADSORB trial. Eur J Vasc Endovasc Surg. 2014;48:285–91.
Ulug P, McCaslin J, Stansby G, Powell J. Endovascular versus conventional medical treatment for uncomplicated chronic type B aortic dissection (review). Cochrane Db Syst Rev. 2012;(11):1–23.
Erbel R, Aboyans V, Boileau C, Bossone E, Di Bartolomeo R, Eggebrecht H, et al. 2014 ESC guidelines on the diagnosis and treatment of aortic diseases. Eur Heart J. 2014;35(41):2873–926.
Fattori R, Cao P, De Rango P, Czerny M, Evangelista A, Nienaber C, et al. Interdisciplinary expert consensus document of management of type B aortic dissection. J Am Coll Cardiol. 2013;61:1661–78.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Awad, N., Lombardi, J. (2017). In Patients with Acute Type B Aortic Dissection, Do Current Operative Therapies Reduce Complications Compared to Medical Management?. In: Skelly, C., Milner, R. (eds) Difficult Decisions in Vascular Surgery. Difficult Decisions in Surgery: An Evidence-Based Approach. Springer, Cham. https://doi.org/10.1007/978-3-319-33293-2_1
Download citation
DOI: https://doi.org/10.1007/978-3-319-33293-2_1
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-33291-8
Online ISBN: 978-3-319-33293-2
eBook Packages: MedicineMedicine (R0)