Abstract
The use of continuous EEG (cEEG) monitoring has grown significantly over the last 15 years. Monitoring for nonconvulsive seizures (NCS) and nonconvulsive status epilepticus (NCSE) is currently driving most cEEG utilization, but other uses are recognized and are becoming common indications. As with other areas in health care, the growth of EEG and information technology (IT) is increasing the capabilities of this century-old technology. As cEEG monitoring evolves, there is a small but growing base of evidence on how to use it. With time, that evidence base will become larger and provide better guidance on the most efficient and effective way to monitor patients. At this time though, institutions must rely on consensus statements, expert opinion, and their own resources to determine how cEEG will be deployed in their practice. Many institutions develop their own guideline such as the truncated example seen in Table 5.1 from Duke University Hospital. It is critical that any such service line has some form of guideline or service agreement to direct the use of this important resource.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Traumatic Brain Injury
- Target Temperature Management
- Seizure Detection
- Nonconvulsive Status Epilepticus
- Refractory Intracranial Hypertension
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
The use of continuous EEG (cEEG) monitoring has grown significantly over the last 15 years. Monitoring for nonconvulsive seizures (NCS) and nonconvulsive status epilepticus (NCSE) is currently driving most cEEG utilization, but other uses are recognized and are becoming common indications. As with other areas in health care, the growth of EEG and information technology (IT) is increasing the capabilities of this century-old technology. As cEEG monitoring evolves, there is a small but growing base of evidence on how to use it. With time, that evidence base will become larger and provide better guidance on the most efficient and effective way to monitor patients. At this time though, institutions must rely on consensus statements, expert opinion, and their own resources to determine how cEEG will be deployed in their practice. Many institutions develop their own guideline such as the truncated example seen in Table 1 from Duke University Hospital. It is critical that any such service line has some form of guideline or service agreement to direct the use of this important resource.
Criteria for Starting Continuous EEG Monitoring
The most common reason for initiating a cEEG study in the intensive care unit (ICU) is for the detection of subclinical or NCS. CEEG is the only type of monitor capable of detecting these types of seizures and, therefore, uniquely suited to this job. The most important population to monitor are those patients who are encephalopathic and were known or strongly suspected to have experienced generalized convulsive status epilepticus (GCSE). The time to recovery of a normal level of consciousness varies greatly, but if the patient does not appear to show improvement within 30 min, cEEG monitoring will almost certainly be needed. Multiple studies in adults and children have shown high rates of NCS (43–57 %) and NCSE (13 %) after clinical seizure activity has stopped with or without the use of abortive medications [1, 2]. In clinical practice, these patients should take precedence over others that will require cEEG monitoring. If cEEG resources are limited and monitoring cannot be initiated promptly, it may be necessary to transfer the patient to an institution with these capabilities. If cEEG is not available, an emergency 30 min EEG may be helpful, but it is likely to not meet the needs of the patient. The American Clinical Neurophysiology Society (ACNS) and Neurocritical Care Society recommend initiating the study as soon as possible and within 60 min, if possible [1, 3]. CEEG monitoring will be required for multiple days or longer if NCS or NCSE is detected after GCSE. Though the technique for monitoring and review does not change, the purpose of cEEG is now directed at terminating seizure activity and ensuring that it does not recur.
Refractory (RSE) and super refractory status epilepticus (SRSE) require IV anesthetic agents such as midazolam, propofol, and pentobarbital. Once RSE or SRSE has been diagnosed and IV anesthetics started, cEEG monitoring is required not only to monitor for the termination of seizure activity but also to titrate to the desired depth of anesthesia whether it is seizure, burst, or total EEG suppression. During the withdrawal of IV anesthetics, cEEG monitoring is needed to ensure that NCSs do not reemerge. In SRSE, the rate of seizure reoccurrence is unfortunately high (greater than 50 %), and close monitoring is necessary to confirm that treatment has been effective [4]. If monitoring is anticipated to last for many days, different tools could be used if they are available. Computed tomography (CT) and magnetic resonance imaging (MRI) compatible electrodes, like disposable plastic, subdermal needle, and wire electrodes, may be used in place of non-disposable gold-plated electrodes if neuroimaging is needed. Quantitative EEG (qEEG) software can be used to facilitate review of long periods of data particularly if a reproducible seizure pattern is found.
CEEG for the detection of seizure activity should not be limited to those with GCSE. In the setting of supratentorial brain injury, many encephalopathic patients are at risk for NCSs. Though clinical seizure activity noted prior to the onset of encephalopathy increases the risk, the rates of detecting subclinical seizure activity in this population remain relatively high. The patients most likely to experience NCS include those with prior epilepsy, intracranial hemorrhage (ICH), moderate-severe traumatic brain injury (TBI), central nervous system (CNS) infections, hypoxic-ischemic-related injury, and brain tumors and those who have undergone a recent neurosurgical procedure [1]. If there is suspicion for NCS, early application of cEEG is critical to identify and treat seizures as they become refractory to abortive agents without prompt recognition and treatment. Though little outcome data is available, it is likely that detection and treatment of seizures may reduce any secondary brain injury that may occur as a result of the NCS [5]. As with patients after GCSE, routine EEG will be inadequate. Therefore, patients with known brain injury and an unexplained encephalopathy should be considered “high risk” and undergo cEEG monitoring as soon as possible.
Though high rates of NCS and NCSE are well recognized in those with brain injury and encephalopathy, acutely ill medical and surgical patients with altered mental status may also be at high risk for seizures. Many acute illnesses, especially sepsis, with single or multi-organ failure and encephalopathy are associated with NCS and NCSE. Similarly, patients who are found to have epileptiform patterns, such as lateralized or generalized periodic discharges, on routine EEG are also at high risk for seizures. Therefore, in these cases cEEG should be strongly considered if resources are available [1, 6].
CEEG has proven critical in the ICU for spell characterization. Similar to studies performed outside the ICU, characterizing paroxysmal events is a common use for cEEG. Stereotyped motor movements presumed to represent seizure are a frequent request for a routine EEG. However, cEEG with audio and video has the advantage of detecting multiple events over several hours and is crucial for determining the etiology of these events. Many such movements are seen that resemble seizure activity but are not epileptic in nature, including clonus, tremors, and intermittent posturing from herniation. This is a common and expected use for cEEG monitoring. When monitoring for spell characterization, capturing several events is encouraged to properly define their etiology and determine their clinical significance. However, once the desired events have been captured, monitoring may no longer be needed.
Routine EEG has been used for several decades as a prognostication tool, particularly after cardiac arrest, but cEEG is becoming useful for this purpose as well. Though there is no evidence as of yet to suggest that cEEG would necessarily be more helpful than a routine study, compelling information has been gained from experience with cEEG monitoring. In most patient populations studied, a lack of EEG reactivity in the absence of significant sedation is consistently associated with a poor prognosis [1, 6]. EEG reactivity has been defined as a change in background frequency and/or amplitude when an external stimulus is applied [6, 7]. EEG reactivity is best determined using a standardized stimulation protocol, but a combination of auditory and tactile stimulation is probably all that is needed in most circumstances. The association between poor prognosis and a lack of reactivity is best documented in comatose post-cardiac arrest patients, but it is present in those with TBI, SAH, and sepsis as well. Though less well studied, a wide range of other prognostic findings can be found during cEEG monitoring. In cardiac arrest, burst suppression patterns are associated with a poor outcome, whereas a continuous reactive record is associated with a good outcome. In sepsis, the appearance of lateralized periodic discharges (LPD) and seizures may be associated with a poor outcome, but this association is less robust [1, 6, 8].
CEEG is also commonly used to measure the depth of anesthesia in circumstances outside of RSE. Refractory intracranial hypertension may require titration of anesthetics to burst suppression. Reducing EEG activity to that of burst suppression correlates well with maximal reduction in cerebral metabolic oxygen (CMRO2) demand, thereby decreasing cerebral blood volume. The anesthetics can be titrated to a desired intracranial pressure (ICP), but monitoring the depth of anesthesia is important for avoiding dose-dependent side effects. Treatment to total EEG suppression does not correlate with improved ICP control but risks over treatment. In many institutions, pentobarbital remains the agent of choice for controlling refractory intracranial hypertension. As serum levels do not correlate well with either effectiveness or toxicity, cEEG is required to titrate the effective dose of pentobarbital. Avoidance of electrocerebral inactivity may reduce the possibility of causing cardiac suppression and other harmful side effects including a gastrointestinal ileus and hypothermia. Though there may be alternatives to cEEG monitoring such as Bispectral index, familiarity with these modalities in the ICU is limited, and the available data to promote its use is sparse [9]. QEEG processing may assist in rapid review but requires the same equipment and resources as standard cEEG monitoring.
Throughout its development, cEEG has functioned chiefly as a seizure detector and secondarily as a neuromonitor. It provides information on a patient’s level of sedation and can reveal global or focal insults when imaging is unavailable and the clinical exam is unhelpful. A more recent and novel use for cEEG is the detection of cerebral ischemia [10]. Developments in quantitative trending tools now allow EEG to be a sensitive, real-time detector of cerebral ischemia and other forms of secondary brain injury. Though currently feasible with the aid of qEEG tools, the evidence base for cEEG in this role is limited. CEEG can provide data on the development or worsening of slowing or suppression suggestive of ischemia. However, given that slowing and suppression are not specific for ischemia, EEG should be used in combination with other data including imaging, transcranial ultrasound, brain parenchymal oxygen monitors, or cerebral microdialysis. This function of cEEG monitoring is also the most difficult to perform effectively and should only be used when an EEG laboratory is able to support it. Very frequent or real-time review is needed to relay information in a time frame that will allow intervention. Other options include training bedside providers to interpret qEEG trends. As this is a developing role, this should not be considered a routine use for cEEG in most institutions [1].
Duration of Continuous EEG Monitoring
The duration of cEEG monitoring is determined by the indication and goals of performing the study. CEEG started for spell characterization, in many instances, can be a short recording as long as the events of interest are satisfactorily captured. On the other hand, cEEG for ischemia monitoring will need to continue for a few days during the time when the patient is at highest risk for neurologic deterioration such as vasospasm in SAH. For determining prognosis in the setting of hypoxic-ischemic injury, there is no clear duration for EEG monitoring. Many institutions will perform cEEG during therapeutic hypothermia or targeted temperature management both to detect NCS as well as to assist in prognostication. This monitoring will often last for 3 or 4 days. If the study is restricted to assisting in prognostication, cEEG may not be necessary. If adequate samples of both baseline and post-stimulation EEG can be captured, intermittent routine EEGs are a reasonable alternative.
When monitoring for NCS, the most common use of cEEG, the proper length of an EEG study is less clear. For patients with RSE on continuous IV anesthetics, monitoring will typically be required until they are off of the infusion for at least 24 h. If the patient has been on IV anesthetics for several days or has SRSE, the duration of monitoring will often need to be a few days after anesthetic agents have been stopped. Due to either active metabolites (i.e., midazolam) or the volume of distribution (i.e., propofol), the effects of the drugs may be seen long after the infusion is stopped. This is a principle called context sensitive half time. In this circumstance, the patient effectively remains on the anesthetic until those effects have dissipated. The duration of this period is unpredictable and depends on many factors including age, renal and hepatic function, and temperature. In cases of RSE and SRSE, monitoring will need to continue until it is deemed safe to stop monitoring by the treating provider.
For both adults and children undergoing monitoring for NCS without known GCSE, the minimum duration of cEEG monitoring should be at least 24 h and perhaps 48 h in the pediatric population [1, 11]. It is likely that a single 30 min or 60 min study will not accurately identify a patient who is experiencing intermittent NCS. Increasing the duration of monitoring will almost certainly increase the likelihood of detecting seizures and epileptiform discharges if they are present. However, it has been difficult to determine how long the cEEG monitoring must be. Most studies have found 80–85 % seizure detection in the first 24 h and a yield of over 90 % when monitoring is extended to 48 h [2, 12]. Most of this data comes from a diverse neurocritical care population with a variety of different pathologies such as TBI, SAH, stroke, and CNS infections. No one population has been studied in large enough numbers to make a disease-specific monitoring duration recommendation. However, recent studies are beginning to provide some guidance on the duration of cEEG monitoring. For example, the first 30 min epoch of EEG data can provide a great deal of information and may predict which patients are likely to have seizures and those that will not. A recent study found that the majority of seizures detected in a neuro-ICU population are found within the first 30 min [12]. When seizures are not seen during this time, the background of the EEG can be predictive of seizures as well. With the possible exception of patients with known epilepsy, those with epileptiform findings in the first 30 min may be more likely to develop NCS than those without [12–15]. Similarly, the patient is much less likely to have NCSs if the first 2–4 h of EEG data shows only diffuse slowing without evidence of epileptiform discharges [12–14]. In a recent study of a large neuro-ICU population, the temporal dynamics of seizure risk were examined and showed a precipitous drop in seizure occurrence based on early EEG features [12]. When no epileptiform features are found within just 15 min, the likelihood of detecting a seizure falls below 10 %. With epileptiform features, the likelihood of detecting seizures drops below 10 % at 7 h.
Though the growing body of literature has been helpful to determine the adequate length of a cEEG study, many questions still remain. How long should EEG monitoring be when a patient’s brain injury is in evolution or the susceptibility to further insult remains high for several days. Examples of this include vasospasm in SAH or worsening ICP in TBI or ICH. In these circumstances, there is susceptibility to further brain injury for several days and the likelihood of subsequent seizures could be high as well. Therefore, it may be wise to monitor a particularly tenuous patient for a longer period of time even if seizures are not seen early in the monitoring period.
Conclusions
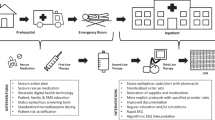
Although clinical research data on seizure detection and prediction is helpful to determine the duration of monitoring, cEEG resources are a critical element in determining who will be monitored and for how long. Maintaining a cEEG service line is expensive and labor intensive. An EEG laboratory capable of maintaining cEEG services requires a large amount of capital expense for EEG acquisition and review equipment as well as robust network and IT services. IT infrastructure is critical both for recording a study as well as review, as remote viewing of cEEG is typically necessary. Without it, an interpreting provider will need to be present in the hospital or be easily able to come to the hospital to ensure timely review and communicate the findings. An equally, if not more important, element to maintaining an effective cEEG service is technologist staffing. Adequately trained and registered technologists are the lynchpin of an effective service line, and their availability will frequently determine how many patients can be monitored and how quickly a study can be performed. Most EEG laboratories capable of high volume cEEG monitoring require 24 h staffing either with in-house or on-call technologists. As many of these elements are not universally available, a hospital-specific service agreement or guideline that emphasizes appropriate triage of studies is critical. CEEG requires a great deal of resources. Therefore, judicious ordering and appropriate triage are always necessary.
References
Herman ST, Abend NS, Bleck TP, Chapman KE, Drislane FW, Emerson RG, Gerard EE, Hahn CD, Husain AM, Kaplan PW, LaRoche SM, Nuwer MR, Quiqq M, Riviello JJ, Schmitt SE, Simmons LA, Tuschida TN, Hirsch LJ. Consensus statement on continuous EEG in critically ill adults and children, part 1: indications. J Clin Neurophysiol. 2015;32(2):87–95.
Claassen J, Mayer SA, Kowalski RG. Detection of electrographic seizures with continuous EEG monitoring in critically ill patients. Neurology. 2004;62:1743–8.
NCS status guidelines
Mayer SA, Claassen J, Lokin J, Mendelsohn F, Dennis LJ, Fitzsimmons B-F. Refractory status epilepticus: frequency, risk factors, and impact on outcome. Arch Neurol. 2002;59:205–10.
Vespa PM, McArthur DL, Xu Y, Eliseo M, Etchepare M, Dinov I, Alger J, Glenn TP, Hovda D. Nonconvulsive seizures after traumatic brain injury are associated with hippocampal atrophy. Neurology. 2010;75(9):792–8.
Gilmore E, Gaspard N, Choi HA, Cohen E, Burkart KM, Chong DH, Claassen J, Hirsch LJ. Acute brain failure in severe sepsis: a prospective study in the medical intensive care unit utilizing continuous EEG monitoring. Intensive Care Med. 2015;41:686–94.
Hermans MC, Westover MB, van Putten MJ, Hirsch LJ, Gaspard N. Quantification of EEG reactivity in comatose patients. Clin Neurophysiol. 2016;127(1):571–80.
Classen J, Taccone FS, Horn P, Holtkamp M, Stocchetti N, Oddo M. Recommendations on the use of EEG monitoring in critically ill patients: consensus statement from the neurointensive care section of the ESICM. Intensive Care Med. 2013;39:1337–51.
Prins SA, de Hoog M, Blok JH, Tibboel D, Visser GH. Continuous noninvasive monitoring of barbiturate coma in critically ill children using the Bispectral index monitor. Crit Care. 2007;11(5):R108.
Claassen J, Foreman B. Quantitative EEG for the detection of brain ischemia. Crit Care. 2012;16(2):216.
Gutierrez-Colina A, Topjian AA, Dlugos DJ, Abend NS. Electroencephalogram monitoring in critically Ill children: indications and strategies. Pediatr Neurol. 2012;46:158–61.
Westover MB, Mouhsin MS, Bianchi MT, Moura L, O’Rourke D, Rosenthal ES, Chu CJ, Donovan S, Hoch DB, Kilbride RD, Cole AJ, Cash SS. The probability of seizure during EEG monitoring in critically ill adults. Clin Neurophysiol. 2015;126:463–71.
Swisher CB, Shah D, Sinha SR, Husain AM. Baseline EEG pattern on continuous ICU EEG monitoring and incidence of seizures. J Clin Neurophysiol. 2015;32(2):147–51.
Shafi MM, Brandon Westover M, Cole AJ, Kilbride RD, Hoch DB, Cash SS. Absence of early epileptiform abnormalities predicts lack of seizures on continuous EEG. Neurology. 2012;79(17):1796–801.
Khan OI, Azevedo CJ, Hartshorn AL, Montanye JT, Gonzalez JC, Natola MA, Surgenor SD, Morse RP, Nordgren RE, Bujarski KA, Holmes GL, Jobst BC, Scott RC, Thadani VM. A comparison of continuous video-EEG monitoring and 30-minute EEG in an ICU. Epileptic Disord. 2014;16(4):439–48.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Dombrowski, K.E. (2017). Criteria for Continuous EEG Monitoring. In: Husain, A., Sinha, S. (eds) Continuous EEG Monitoring. Springer, Cham. https://doi.org/10.1007/978-3-319-31230-9_5
Download citation
DOI: https://doi.org/10.1007/978-3-319-31230-9_5
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-31228-6
Online ISBN: 978-3-319-31230-9
eBook Packages: MedicineMedicine (R0)