Abstract
The prevalence of dementia, representing a category of age-associated disorders, is continuously increasing in our aging society. Currently, more than 9 Mio patients are supposed to be affected by this devastating condition in Europe (http://www.alzheimer-europe.org/), not including a presumably high number of patients who have not yet been diagnosed or patients in early stages of disease. Approximately 20 % of persons in an age greater than 80 years are suffering from clinically manifest dementia [1, 2]. With regard to the rising life expectancy, this poses a massive burden not only on patients and their relatives but also on the healthcare/socioeconomic systems. These facts appear even more alarming in the light of the very limited therapeutic options which are currently available for most forms of dementia.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
The prevalence of dementia, representing a category of age-associated disorders, is continuously increasing in our aging society. Currently, more than 9 Mio patients are supposed to be affected by this devastating condition in Europe (http://www.alzheimer-europe.org/), not including a presumably high number of patients who have not yet been diagnosed or patients in early stages of disease. Approximately 20 % of persons in an age greater than 80 years are suffering from clinically manifest dementia [1, 2]. With regard to the rising life expectancy, this poses a massive burden not only on patients and their relatives but also on the healthcare/socioeconomic systems. These facts appear even more alarming in the light of the very limited therapeutic options which are currently available for most forms of dementia.
In short, dementia itself is defined as an impairment of cognitive abilities sufficient to affect the activities of daily living, which is developing gradually and is not associated with a loss of consciousness [3]. Different causal pathologies can underlie the clinical manifestation of a dementia, the most frequent being Alzheimer’s disease which holds responsible for approximately 60 % of all cases, followed by vascular dementia, dementia with Lewy body disease, and the frontotemporal lobar degenerative disorders [4, 5]. A common factor contributing to the development of neurodegenerative forms of dementia appears to be the pathological aggregation of proteins in the brain. For Alzheimer’s disease, this includes the deposition of ß-amyloid protein aggregates in the form of extracellular plaques and of tau protein aggregates in the form of intraneuronal neurofibrillary tangles [6]. According to current disease concepts, these aggregates contribute to neuronal dysfunction and later neuronal loss [7]. Modern therapy approaches are directed toward the removal/prevention of these protein aggregation pathologies. However, so far these studies have not resulted in very promising results. As for factors possibly contributing to this limited success, it has been discussed that attempts to treat have been initiated too late in the course of disease, i.e., when irreversible neuronal damage has already occurred. Furthermore, it has been demonstrated that a relevant proportion of patients included in these trials may have been clinically misdiagnosed [8].
These insights underline the need for a reliable and early diagnosis of ongoing neurodegeneration. However, clinical diagnosis of dementia is hampered in many respects. First, it is well accepted that the causal neuropathologies leading to dementia are usually starting to develop years to decades ahead of the symptomatic onset of disease. Consequently, today preclinical and pre-dementia mild clinical stages (the so-called mild cognitive impairment or MCI) are discussed, particularly with regard to Alzheimer’s disease [9]. From this perspective, dementia can be considered a late stage of disease and early diagnosis on the basis of the assessment of clinical symptoms is limited per definition. In the same context, biomarker-supported diagnosis of Alzheimer’s disease is recently recommended, all the more if early diagnosis of ongoing neurodegeneration is required [10–13]. Also, differential diagnosis of different forms of dementia is difficult, because different causal pathologies can result in similar cognitive deficits. Finally, clinical symptomatology of dementia may not be an optimal parameter for follow-up and therapy monitoring, because of a limited association between neuropathology and extent of symptoms as well as fluctuation of the latter. Consequently, the role of imaging biomarkers in the diagnosis of pathologies underlying the development of dementia may be of growing importance. In this context, nuclear medicine offers particularly promising methods for imaging molecular pathologies and neuronal dysfunction.
[18F]FDG-PET
It is well known that glucose represents the source of energy for the brain and that cerebral neuronal activity is tightly coupled to the uptake and metabolism of glucose, probably mediated by the glial cells [14]. Consequently, regional cerebral uptake of [18F]FDG as a tracer for measuring glucose metabolism reflects neuronal function or dysfunction. It has been demonstrated by numerous studies – including studies with in vivo versus postmortem histopathological cross evaluation – that typical patterns of hypometabolism can be observed in manifest neurodegenerative forms of dementia [15]. In Alzheimer’s disease, a characteristic pattern of hypometabolism in the temporoparietal, posterior cingulate, and later also frontal cortex can be observed [16]. The pattern of affected brain regions fits to the functional abnormalities which are usually involving memory, language functions, visual-spatial abilities, and later personality changes. The sensorimotor regions as well as the primary visual cortex and cerebellum are usually spared from metabolic changes, in correspondence with maintained motor and sensory functions in these patients. The topography of these hypometabolic changes is highly specific for Alzheimer’s disease, and it has been demonstrated that FDG-PET allows more accurate diagnosis as compared to neuropsychological assessment [17]. Importantly, hypometabolic abnormalities are not only observed in patients with manifest dementia of Alzheimer’s type but also in earlier stages of disease. A number of studies analyzed the value of FDG-PET in the early detection of Alzheimer’s disease in the stage of MCI. It has been demonstrated that mild hypometabolism in posterior cingulate cortical regions, often accompanied by subtle parietal and temporal hypometabolism, has a high predictive value with regard to later conversion to manifest dementia in these patients [16, 18]. On the other hand, patients with MCI symptoms but without signs of hypometabolism on FDG-PET have a very low risk of conversion to dementia of Alzheimer’s type. FDG-PET has also been demonstrated to have a very high value in the differential diagnosis between different forms of neurodegenerative disorders [19]. For non-Alzheimer forms of dementia, disease-specific patterns of hypometabolism have been described. Dementia with Lewy bodies has been shown to be associated with a pattern of temporoparietal hypometabolism similar to Alzheimer’s disease, however, extending clearly into the occipital cortex, involving primary visual cortical areas [20]. This goes hand in hand with the known visual hallucinations in these patients. FDG-PET has also been shown to have a high value for differentiation between Alzheimer’s-type dementia and the frontotemporal lobar degenerative disorders [21]. Also, for the different subtypes of frontotemporal lobar degeneration (FTLD), specific patterns of hypometabolism have been described [22–27], with the behavioral variant (bvFTD) showing stronger frontal and temporal polar abnormalities [28], the semantic variant of primary progressive aphasia (svPPA) displaying bilateral temporal hypometabolism [25, 29, 30], and the logopenic variant as well as the nonfluent variant (lvPPA, nfvPPA) both demonstrating clearly asymmetric unilateral (usually left-hemispheric) hypometabolism of the temporal and in part frontal and parietal cortex. In nfvPPA, involvement of left frontal cortical regions (often including Broca’s area) has been shown [31, 32], and in lvPPA hypometabolic regions have been observed within the left lateral temporal and parietal lobe as well as in the precuneus and posterior frontal lobe [33–36]. It has to be mentioned that the FDG pattern is reflecting the symptomatic appearance of these subtypes of neurodegeneration without allowing a clear distinction of the underlying neuropathology. FTLD has been demonstrated to comprise a number of different causal pathologies which can result in similar clinical phenotypes of disease [37, 39]. This includes tau-positive forms, TDP-43 aggregation-positive forms, and even atypical forms of Alzheimer’s disease. In particular the variant of logopenic aphasia has been demonstrated to frequently represent an atypical variant of Alzheimer’s disease [31]. However, other neuropathological changes such as TDP-43 may result in the clinical appearance of lvPPA accompanied by a similar hypometabolic pattern in FDG-PET [33]. In addition to the phenotype of logopenic aphasia, Alzheimer’s disease can appear in other atypical variants. This includes the so-called posterior cortical atrophy, which is characterized by predominantly visual-constructive deficits in the early phases of disease, often leading the patients to see an ophthalmologist [39]. In the FDG-PET scan these patients exhibit a distinct bilateral occipitoparietal hypometabolism [40, 41]. Another atypical form of Alzheimer’s disease is the frontal/executive subtype [42]. Patients may show symptoms more similar to the behavioral variant of frontotemporal dementia in early cases. In the FDG-PET scan, they show frontal cortical hypometabolism, but in contrast to bvFTD usually some involvement of temporoparietal cortices is to be expected. Using amyloid imaging (see below) doubts about the causal pathology in these atypical cases of Alzheimer’s disease can be cleared. Finally, FDG-PET represents a valuable tool to differentiate pseudodementia in patients with depression and cognitive symptoms (who will show a rather normal finding on the FDG-PET scan) versus patients suffering from early Alzheimer’s disease with depressive symptoms [43].
Amyloid Imaging
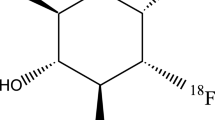
Since their first description by Alois Alzheimer himself, amyloid plaques represent one key hallmark for the diagnosis of Alzheimer’s disease. Until very recently, definite diagnosis of Alzheimer’s disease has only been possible by means of postmortem histopathological assessment of brain tissue. The advent of tracers for amyloid imaging now allows the detection of this core pathology in vivo. Consequently, for the first time, noninvasive in vivo proof of amyloid deposition in the brain and longitudinal observation of the onset and course of this pathology became possible. A great number of studies on in vivo imaging of amyloid deposits in the brain have been performed with the tracer [11C]PiB [44]. These studies form the basis of our current knowledge on the potential value of amyloid imaging in clinical practice. In addition, for a number of 18F-labeled tracers (with longer half-life), FDA approval has been achieved and they are now also commercially available. This includes [18F]florbetaben (NeuraCeqTM), [18F]florbetapir (AmyvidTM), and [18F]flutemetamol (VizamylTM) [45–47]. All tracers had to undergo extensive evaluation before approval, including in vivo versus postmortem evaluation of their properties [48–57].
For all tracers, typically intense tracer uptake is observed in the frontal, temporoparietal, and posterior cingulate cortex, the precuneus, and also the caudate nucleus. Sensorimotor and visual cortices are usually somewhat less affected and the cerebellum is spared of amyloid aggregates and, thus, can serve as a reference region [45, 47, 58, 59].
Regarding early diagnosis, several studies were now able to demonstrate that the proof of amyloid pathology in the brain in patients with MCI has a high sensitivity with regard to prediction of later conversion to manifest Alzheimer’s dementia [60–65]. The specificity varied depending on the selected follow-up periods. Importantly, studies consistently demonstrated that in approximately 25–30 % of elderly subjects (>60 years), significant amyloid pathology could be detected using amyloid imaging in the presence of normal cognitive function [58, 66–69]. A recent study demonstrated the rate of amyloid positivity appears to increase exponentially with age in otherwise healthy elderly subjects in dependence of the ApoE genotype, with homozygous carriers of the e4 allele showing the highest risk [69]. It is yet unclear if “amyloid positivity” translates inevitably into symptomatic Alzheimer’s disease in all of these subjects. Several studies indicate that amyloid-positive elderly subjects may in fact be suffering from preclinical Alzheimer’s disease by demonstrating abnormalities in other imaging tests, comparatively lower cognitive performance and steeper cognitive decline in these subjects as compared to amyloid-negative age-matched controls [70–72]. However, even in this case the information on the potential time to conversion in these subjects is still very limited. It appears possible that amyloid pathology may be detected in the brain 10–20 years ahead of clinical disease onset [63]. Consequently, according to recently published appropriate use criteria for amyloid imaging, it would not be recommended to offer an amyloid PET scan in otherwise healthy elderly subjects [73]. First, the interpretation of a positive amyloid scan in terms of prognosis would be difficult to judge. Second, at this time no therapeutic options would be on hand. Thus, the disclosure of the information of amyloid positivity to an otherwise healthy person would in fact be ethically problematic. On the other hand, in the context of clinical trials, it obviously stands to reason to include subjects with only mild or even no clinical symptoms into studies aiming for the removal or prevention of amyloid deposition in the brain. In fact, large clinical trials have been initiated following this concept [74]. Thus, in summary, there is a value of amyloid imaging with regard to early diagnosis/exclusion of Alzheimer pathology in patients with mild symptoms. However, in asymptomatic stages, amyloid imaging would currently be restricted to systematic clinical trials.
Regarding differential diagnosis, it has been demonstrated that the available amyloid tracers are specific with regard to amyloid pathology, i.e., they would not bind to other forms of protein aggregation such as tau or alpha-synuclein [52, 75–78]. However, it is also known that amyloid plaques do not only develop in Alzheimer’s disease but can also be found in up to 80 % of cases of dementia with Lewy bodies [79–81]. Thus, differential diagnosis between AD and DLB cannot be performed using amyloid imaging. For this diagnostic question, it has been demonstrated that dopamine transporter imaging can be applied which reveals normal findings in AD but reduced transporter density in patients with DLB [82]. Amyloid imaging may be of high value to differentiate between the amyloid-negative forms of frontotemporal lobar degeneration and Alzheimer’s disease [83]. As mentioned above, atypical clinical variants of Alzheimer’s disease may appear in symptomatic forms typically associated with frontotemporal lobar degeneration, e.g., in logopenic aphasia [31, 84, 85]. Inversely, frontotemporal lobar degenerative disorders may mimic Alzheimer’s disease as well. Consequently, according to the appropriate use criteria, it can be recommended to clinically employ amyloid imaging in cases of early-onset dementia and in cases with atypical appearance of suspected Alzheimer’s disease [73]. Amyloid imaging is currently not recommended in cases of clinically typical Alzheimer’s disease. This position can however be challenged with regard to recent insights from clinical trials, indicating that a high proportion (>30 %) of patients clinically diagnosed with Alzheimer’s disease by experts in fact do not show amyloid pathology in their amyloid scans [8]. Amyloid imaging may therefore be crucial for inclusion of patients into anti-amyloid therapy trials. Some studies have also employed amyloid imaging to monitor therapy response [86]. It may not be useful for disease follow-up, however, because it has been demonstrated that amyloid deposition shows a stagnation or plateau in the symptomatic stages of disease [87]. Regarding differential diagnosis with amyloid PET, it should be kept in mind that the probability of amyloid positivity increases with age not only in healthy subjects but also in patients suffering from clinical forms of neurodegeneration other than Alzheimer’s disease, as recently demonstrated [88]. Consequently, in elderly subjects, the possibility of amyloid deposition, which is not disease related, or the presence of dual pathology should be taken into account.
Tracers for Tau Imaging
In addition to now established tracers for amyloid imaging, recently introduced experimental tracers are promising to be suitable for imaging tau aggregates [89, 90]. The imaging of tau is considerably more complicated as compared to amyloid imaging, as tracers have to enter not only the brain across the blood-brain barrier but also enter the neurons because tau aggregates occur intracellularly.
For several tracers promising results in humans have already been published. This includes tracers developed at Tohoku University, Japan [91–94], and the tracer [18F]T807 ([18F]AV1451) now licensed by Avid Radiopharmaceuticals [95, 96]. The first studies with these tracers in humans demonstrate an uptake pattern which is different from amyloid deposition in the same patients with Alzheimer’s disease and consistent with the distribution of tau pathology, as known from neuropathology. In a first study, the binding behavior of T807 has also been evaluated on human brain tissue [97]. However, for all of these tracers, histopathological in vivo versus postmortem cross evaluation is still pending. A clinical value of tau imaging tracers with regard to early diagnosis of Alzheimer’s disease may be discussed [89, 90]. However, according to currently discussed concepts on the order of appearance of biomarkers of Alzheimer’s disease, it would be expected that amyloid pathology would be detectable ahead of tau pathology [98]. On the other hand, neuropathological studies suggest that cerebral tau aggregation correlates with the extent of cognitive decline (in contrast to amyloid plaque deposition). Correspondingly, the first tau imaging studies indicate that the uptake of tau correlates closely with the level of cognitive impairment [96]. Thus, tau imaging may represent a suitable biomarker for disease follow-up but rather not for very early detection of Alzheimer pathology in the asymptomatic stages. It may, however, be helpful to detect the onset of neurodegeneration in amyloid-positive subjects. Future studies will need to demonstrate an added value in this context, as compared to markers of neuronal dysfunction such as [18F]FDG. With regard to differential diagnosis, the application of tau imaging may be very complicated, because tau as a target is highly heterogeneous [99, 100]. There are two different haplotypes and 6 isoforms, tau can occur in phosphorylated/non-phosphorylated forms, and there are different structural variants of aggregation (straight filaments, helical filaments/tangles, coiled bodies, etc.). Depending on the disorder, aggregates can occur in neurons and in the glial cells [101]. Tau imaging may be helpful to differentiate between tau-positive and tau-negative forms of syndromes, e.g., tau-positive corticobasal syndrome versus synuclein-positive multiple system atrophies (MSA). However, tau pathology can be found in a number of different neurodegenerative disorders, summarized under the term “tauopathies” [102]. This includes Alzheimer’s disease, corticobasal syndrome, progressive supranuclear palsy, Pick’s disease, FTLD-MAPT (FTD/parkinsonism, chromosome 17 (FTDP-17)), and also brain trauma. Thus, differential diagnosis between these neurodegenerative disorders on the basis of tau positivity or negativity will not be possible. However, patterns of cerebral tau aggregation are different between the various tauopathies, thus potentially providing information beyond the bare presence of tau pathology. The fact that levels and anatomical distribution of tau aggregation pathology may be detected by tau imaging potentially also represents an added value over CSF tests (Fig. 1).
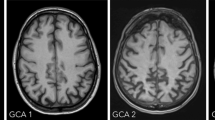
Exemplary presentation (surface projections, 3DSSP, Neurostat) of [18F]FDG-PET (glucose metabolism) and [11C]PiB-PET (amyloid imaging) in different forms of dementia. Images are displayed in left lateral (1st and 3rd column) and right lateral (2nd and 4th column) aspects of the brain (1st two columns, FDG-PET; 3rd and 4th column, PiB-PET). AD Alzheimer’s disease, lvPPA logopenic variant of primary progressive aphasia, svPPA semantic variant of primary progressive aphasia, bvFTD behavioral variant of frontotemporal dementia
Summary
Recent guidelines for diagnosis of Alzheimer’s disease recommend a three-step biomarker-supported categorization [10]. According to these guidelines, increased levels of amyloid pathology in the brain are coding for a low risk, presence of additional neuronal injury for an intermediate risk, and the additional proof of cognitive decline for a high risk of suffering from Alzheimer’s disease. Molecular imaging methods offer the unique opportunity to monitor these parameters in vivo, noninvasively. Amyloid imaging has entered the clinical arena and may allow to detect subjects at risk for Alzheimer’s disease in very early stages, to select patients for therapy trials, and (if negative) to exclude Alzheimer’s disease as a reason for cognitive decline. FDG-PET as the best established tracer for imaging neurodegeneration can be considered the Swiss Knife in dementia diagnosis. It allows reliable prediction in the stages of mild cognitive impairment and provides information on the pattern and extent of neuronal dysfunction in different forms of neurodegenerative disorders. Novel tau imaging procedures are still in an experimental stage but may allow to detect onset of neurodegeneration in amyloid-positive subjects, select patients for tau trials, and differentiate between tau-positive and tau-negative forms of neurodegeneration in the future.
References
Hebert LE, Weuve J, Scherr PA et al (2013) Alzheimer disease in the United States (2010–2050) estimated using the 2010 census. Neurology 80(19):1778–1783
Plassman BL, Langa KM, Fisher GG et al (2007) Prevalence of dementia in the United States: the aging, demographics, and memory study. Neuroepidemiology 29(1–2):125–132
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, V.A.P.P
Alafuzoff I (1992) The pathology of dementias: an overview. Acta Neurol Scand Suppl 139:8–15
Zaccai J, McCracken C, Brayne C (2005) A systematic review of prevalence and incidence studies of dementia with Lewy bodies. Age Ageing 34(6):561–566
Braak H, Braak E (1991) Neuropathological stageing of Alzheimer-related changes. Acta Neuropathol (Berl) 82(4):239–259
Selkoe DJ (2003) Folding proteins in fatal ways. Nature 426(6968):900–904
Salloway S, Sperling R, Fox NC et al (2014) Two phase 3 trials of bapineuzumab in mild-to-moderate Alzheimer’s disease. N Engl J Med 370(4):322–333
Petersen RC, Smith GE, Waring SC et al (1999) Mild cognitive impairment: clinical characterization and outcome. Arch Neurol 56(3):303–308
Dubois B, Feldman HH, Jacova C et al (2007) Research criteria for the diagnosis of Alzheimer’s disease: revising the NINCDS-ADRDA criteria. Lancet Neurol 6(8):734–746
Sperling RA, Aisen PS, Beckett LA et al (2011) Toward defining the preclinical stages of Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement 7(3):280–292
McKhann GM, Knopman DS, Chertkow H et al (2011) The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement 7(3):263–269
Albert MS, DeKosky ST, Dickson D et al (2011) The diagnosis of mild cognitive impairment due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement 7(3):270–279
Magistretti PJ, Pellerin L (1996) Cellular mechanisms of brain energy metabolism. Relevance to functional brain imaging and to neurodegenerative disorders. Ann N Y Acad Sci 777:380–387
Herholz K (2003) PET studies in dementia. Ann Nucl Med 17(2):79–89
Minoshima S, Giordani B, Berent S et al (1997) Metabolic reduction in the posterior cingulate cortex in very early Alzheimer’s disease. Ann Neurol 42(1):85–94
Silverman, D.H., G.W. Small, C.Y. Chang, et al (2001) Positron emission tomography in evaluation of dementia: Regional brain metabolism and long-term outcome. Jama, 286(17): p. 2120–7.
Drzezga A, Lautenschlager N, Siebner H et al (2003) Cerebral metabolic changes accompanying conversion of mild cognitive impairment into Alzheimer’s disease: a PET follow-up study. Eur J Nucl Med Mol Imaging 30(8):1104–1113
Panegyres PK, Rogers JM, McCarthy M et al (2009) Fluorodeoxyglucose-positron emission tomography in the differential diagnosis of early-onset dementia: a prospective, community-based study. BMC Neurol 9:41
Minoshima S, Foster NL, Sima AA et al (2001) Alzheimer’s disease versus dementia with Lewy bodies: cerebral metabolic distinction with autopsy confirmation. Ann Neurol 50(3):358–365
Foster NL, Heidebrink JL, Clark CM et al (2007) FDG-PET improves accuracy in distinguishing frontotemporal dementia and Alzheimer’s disease. Brain 130(Pt 10):2616–2635
Diehl J, Grimmer T, Drzezga A et al (2004) Cerebral metabolic patterns at early stages of frontotemporal dementia and semantic dementia. A PET study. Neurobiol Aging 25(8):1051–1056
Diehl-Schmid J, Grimmer T, Drzezga A et al (2006) Longitudinal changes of cerebral glucose metabolism in semantic dementia. Dement Geriatr Cogn Disord 22(4):346–351
Diehl-Schmid J, Grimmer T, Drzezga A et al (2007) Decline of cerebral glucose metabolism in frontotemporal dementia: a longitudinal 18F-FDG-PET-study. Neurobiol Aging 28:42–50
Drzezga A, Grimmer T, Henriksen G et al (2008) Imaging of amyloid plaques and cerebral glucose metabolism in semantic dementia and Alzheimer’s disease. Neuroimage 39(2):619–633
Nestor PJ, Graham NL, Fryer TD et al (2003) Progressive non-fluent aphasia is associated with hypometabolism centred on the left anterior insula. Brain 126(Pt 11):2406–2418
Nestor PJ, Fryer TD, Hodges JR (2006) Declarative memory impairments in Alzheimer’s disease and semantic dementia. Neuroimage 30(3):1010–1020
Schroeter ML, Laird AR, Chwiesko C et al (2014) Conceptualizing neuropsychiatric diseases with multimodal data-driven meta-analyses - The case of behavioral variant frontotemporal dementia. Cortex 57C:22–37
Edwards-Lee T, Miller BL, Benson DF et al (1997) The temporal variant of frontotemporal dementia. Brain 120(Pt 6):1027–1040
Jagust WJ, Reed BR, Seab JP et al (1989) Clinical-physiologic correlates of Alzheimer’s disease and frontal lobe dementia. Am J Physiol Imaging 4(3):89–96
Rabinovici GD, Jagust WJ, Furst AJ et al (2008) Abeta amyloid and glucose metabolism in three variants of primary progressive aphasia. Ann Neurol 64(4):388–401
Drzezga A, Grimmer T, Siebner H et al (2002) Prominent hypometabolism of the right temporoparietal and frontal cortex in two left-handed patients with primary progressive aphasia. J Neurol 249(9):1263–1267
Josephs KA, Duffy JR, Strand EA et al (2014) Progranulin-associated PiB-negative logopenic primary progressive aphasia. J Neurol 261(3):604–614
Gorno-Tempini ML, Dronkers NF, Rankin KP et al (2004) Cognition and anatomy in three variants of primary progressive aphasia. Ann Neurol 55(3):335–346
Madhavan A, Whitwell JL, Weigand SD et al (2013) FDG PET and MRI in logopenic primary progressive aphasia versus dementia of the Alzheimer’s type. PLoS One 8(4):e62471
Teichmann M, Kas A, Boutet C et al (2013) Deciphering logopenic primary progressive aphasia: a clinical, imaging and biomarker investigation. Brain 136(Pt 11):3474–3488
Mesulam M, Wieneke C, Rogalski E et al (2009) Quantitative template for subtyping primary progressive aphasia. Arch Neurol 66(12):1545–1551
Bonner MF, Ash S, Grossman M (2010) The new classification of primary progressive aphasia into semantic, logopenic, or nonfluent/agrammatic variants. Curr Neurol Neurosci Rep 10(6):484–490
Crutch SJ, Lehmann M, Schott JM et al (2012) Posterior cortical atrophy. Lancet Neurol 11(2):170–178
Nestor PJ, Caine D, Fryer TD et al (2003) The topography of metabolic deficits in posterior cortical atrophy (the visual variant of Alzheimer’s disease) with FDG-PET. J Neurol Neurosurg Psychiatry 74(11):1521–1529
Whitwell JL, Jack CR Jr, Kantarci K et al (2007) Imaging correlates of posterior cortical atrophy. Neurobiol Aging 28(7):1051–1061
Back-Madruga C, Boone KB, Briere J et al (2002) Functional ability in executive variant Alzheimer’s disease and typical Alzheimer’s disease. Clin Neuropsychol 16(3):331–340
Videbech P (2000) PET measurements of brain glucose metabolism and blood flow in major depressive disorder: a critical review. Acta Psychiatr Scand 101(1):11–20
Klunk WE, Engler H, Nordberg A et al (2004) Imaging brain amyloid in Alzheimer’s disease with Pittsburgh Compound-B. Ann Neurol 55(3):306–319
Barthel H, Gertz HJ, Dresel S et al (2011) Cerebral amyloid-beta PET with florbetaben (18F) in patients with Alzheimer’s disease and healthy controls: a multicentre phase 2 diagnostic study. Lancet Neurol 10(5):424–435
Vandenberghe R, Van Laere K, Ivanoiu A et al (2010) 18F-flutemetamol amyloid imaging in Alzheimer disease and mild cognitive impairment: a phase 2 trial. Ann Neurol 68(3):319–329
Fleisher AS, Chen K, Liu X et al (2011) Using positron emission tomography and florbetapir F18 to image cortical amyloid in patients with mild cognitive impairment or dementia due to Alzheimer disease. Arch Neurol 68(11):1404–1411
Bacskai BJ, Frosch MP, Freeman SH et al (2007) Molecular imaging with Pittsburgh Compound B confirmed at autopsy: a case report. Arch Neurol 64(3):431–434
Burack MA, Hartlein J, Flores HP et al (2010) In vivo amyloid imaging in autopsy-confirmed Parkinson disease with dementia. Neurology 74(1):77–84
Cairns NJ, Ikonomovic MD, Benzinger T et al (2009) Absence of Pittsburgh compound B detection of cerebral amyloid beta in a patient with clinical, cognitive, and cerebrospinal fluid markers of Alzheimer disease: a case report. Arch Neurol 66(12):1557–1562
Clark CM, Schneider JA, Bedell BJ et al (2011) Use of florbetapir-PET for imaging beta-amyloid pathology. JAMA 305(3):275–283
Ikonomovic MD, Klunk WE, Abrahamson EE et al (2008) Post-mortem correlates of in vivo PiB-PET amyloid imaging in a typical case of Alzheimer’s disease. Brain 131(Pt 6):1630–1645
Kadir A, Marutle A, Gonzalez D et al (2011) Positron emission tomography imaging and clinical progression in relation to molecular pathology in the first Pittsburgh Compound B positron emission tomography patient with Alzheimer’s disease. Brain 134(Pt 1):301–317
Leinonen V, Alafuzoff I, Aalto S et al (2008) Assessment of beta-amyloid in a frontal cortical brain biopsy specimen and by positron emission tomography with carbon 11-labeled Pittsburgh Compound B. Arch Neurol 65(10):1304–1309
Sojkova J, Driscoll I, Iacono D et al (2011) In vivo fibrillar beta-amyloid detected using [11C]PiB positron emission tomography and neuropathologic assessment in older adults. Arch Neurol 68(2):232–240
Villemagne VL, McLean CA, Reardon K et al (2009) 11C-PiB PET studies in typical sporadic Creutzfeldt-Jakob disease. J Neurol Neurosurg Psychiatry 80(9):998–1001
Wolk DA, Grachev ID, Buckley C et al (2011) Association between in vivo fluorine 18-labeled flutemetamol amyloid positron emission tomography imaging and in vivo cerebral cortical histopathology. Arch Neurol 68(11):1398–1403
Pike KE, Savage G, Villemagne VL et al (2007) Beta-amyloid imaging and memory in non-demented individuals: evidence for preclinical Alzheimer’s disease. Brain 130(Pt 11):2837–2844
Rowe CC, Ellis KA, Rimajova M et al (2010) Amyloid imaging results from the Australian Imaging, Biomarkers and Lifestyle (AIBL) study of aging. Neurobiol Aging 31(8):1275–1283
Forsberg A, Engler H, Almkvist O et al (2008) PET imaging of amyloid deposition in patients with mild cognitive impairment. Neurobiol Aging 29:1456–1465
Koivunen J, Scheinin N, Virta JR et al (2011) Amyloid PET imaging in patients with mild cognitive impairment: a 2-year follow-up study. Neurology 76(12):1085–1090
Okello A, Koivunen J, Edison P et al (2009) Conversion of amyloid positive and negative MCI to AD over 3 years: an 11C-PIB PET study. Neurology 73(10):754–760
Villemagne VL, Pike KE, Chetelat G et al (2011) Longitudinal assessment of Abeta and cognition in aging and Alzheimer disease. Ann Neurol 69(1):181–192
Zhang S, Han D, Tan X et al (2012) Diagnostic accuracy of 18 F-FDG and 11 C-PIB-PET for prediction of short-term conversion to Alzheimer’s disease in subjects with mild cognitive impairment. Int J Clin Pract 66(2):185–198
Nordberg A, Carter SF, Rinne J et al (2013) A European multicentre PET study of fibrillar amyloid in Alzheimer’s disease. Eur J Nucl Med Mol Imaging 40(1):104–114
Mintun MA, Larossa GN, Sheline YI et al (2006) [11C]PIB in a nondemented population: potential antecedent marker of Alzheimer disease. Neurology 67(3):446–452
Villemagne VL, Pike KE, Darby D et al (2008) Abeta deposits in older non-demented individuals with cognitive decline are indicative of preclinical Alzheimer’s disease. Neuropsychologia 46(6):1688–1697
Villemagne VL, Fodero-Tavoletti MT, Pike KE et al (2008) The ART of loss: Abeta imaging in the evaluation of Alzheimer’s disease and other dementias. Mol Neurobiol 38(1):1–15
Jansen WJ, Ossenkoppele R, Knol DL et al (2015) Prevalence of cerebral amyloid pathology in persons without dementia: a meta-analysis. JAMA 313(19):1924–1938
Hedden T, Van Dijk KR, Becker JA et al (2009) Disruption of functional connectivity in clinically normal older adults harboring amyloid burden. J Neurosci 29(40):12686–12694
Sperling RA, Laviolette PS, O’Keefe K et al (2009) Amyloid deposition is associated with impaired default network function in older persons without dementia. Neuron 63(2):178–188
Drzezga A, Becker JA, Van Dijk KR et al (2011) Neuronal dysfunction and disconnection of cortical hubs in non-demented subjects with elevated amyloid burden. Brain 134(Pt 6):1635–1646
Johnson KA, Minoshima S, Bohnen NI et al (2013) Appropriate use criteria for amyloid PET: a report of the Amyloid Imaging Task Force, the Society of Nuclear Medicine and Molecular Imaging, and the Alzheimer’s Association. J Nucl Med 54(3):476–490
Sperling RA, Rentz DM, Johnson KA et al (2014) The A4 study: stopping AD before symptoms begin? Sci Transl Med 6(228):228fs13
Fodero-Tavoletti MT, Brockschnieder D, Villemagne VL et al (2012) In vitro characterization of [(18)F]-florbetaben, an Abeta imaging radiotracer. Nucl Med Biol 39:1042–1048
Fodero-Tavoletti MT, Smith DP, McLean CA et al (2007) In vitro characterization of Pittsburgh compound-B binding to Lewy bodies. J Neurosci 27(39):10365–10371
Lockhart A, Lamb JR, Osredkar T et al (2007) PIB is a non-specific imaging marker of amyloid-beta (Abeta) peptide-related cerebral amyloidosis. Brain 130(Pt 10):2607–2615
Thompson PW, Ye L, Morgenstern JL et al (2009) Interaction of the amyloid imaging tracer FDDNP with hallmark Alzheimer’s disease pathologies. J Neurochem 109(2):623–630
Weisman D, Cho M, Taylor C et al (2007) In dementia with Lewy bodies, Braak stage determines phenotype, not Lewy body distribution. Neurology 69(4):356–359
Rowe CC, Ng S, Ackermann U et al (2007) Imaging beta-amyloid burden in aging and dementia. Neurology 68(20):1718–1725
Edison P, Rowe CC, Rinne JO et al (2008) Amyloid load in Parkinson’s disease dementia and Lewy body dementia measured with [11C]PIB positron emission tomography. J Neurol Neurosurg Psychiatry 79(12):1331–1338
McKeith I, O’Brien J, Walker Z et al (2007) Sensitivity and specificity of dopamine transporter imaging with 123I-FP-CIT SPECT in dementia with Lewy bodies: a phase III, multicentre study. Lancet Neurol 6(4):305–313
Rabinovici GD, Furst AJ, O’Neil JP et al (2007) 11C-PIB PET imaging in Alzheimer disease and frontotemporal lobar degeneration. Neurology 68(15):1205–1212
Formaglio M, Costes N, Seguin J et al (2011) In vivo demonstration of amyloid burden in posterior cortical atrophy: a case series with PET and CSF findings. J Neurol 258(10):1841–1851
de Souza LC, Corlier F, Habert MO et al (2011) Similar amyloid-beta burden in posterior cortical atrophy and Alzheimer’s disease. Brain 134(Pt 7):2036–2043
Rinne JO, Brooks DJ, Rossor MN et al (2010) 11C-PiB PET assessment of change in fibrillar amyloid-beta load in patients with Alzheimer’s disease treated with bapineuzumab: a phase 2, double-blind, placebo-controlled, ascending-dose study. Lancet Neurol 9(4):363–372
Engler H, Forsberg A, Almkvist O et al (2006) Two-year follow-up of amyloid deposition in patients with Alzheimer’s disease. Brain 129:2856–2866
Ossenkoppele R, Jansen WJ, Rabinovici GD et al (2015) Prevalence of amyloid PET positivity in dementia syndromes: a meta-analysis. JAMA 313(19):1939–1949
Villemagne VL, Okamura N (2014) In vivo tau imaging: obstacles and progress. Alzheimers Dement 10(3 Suppl):S254–S264
Okamura N, Furumoto S, Fodero-Tavoletti MT et al (2014) Non-invasive assessment of Alzheimer’s disease neurofibrillary pathology using 18F-THK5105 PET. Brain 137(Pt 6):1762–1771
Villemagne VL, Okamura N (2015) Tau imaging in the study of ageing, Alzheimer’s disease, and other neurodegenerative conditions. Curr Opin Neurobiol 36:43–51
Ishiki A, Okamura N, Furukawa K et al (2015) Longitudinal assessment of tau pathology in patients with Alzheimer’s disease using [18F]THK-5117 positron emission tomography. PLoS One 10(10):e0140311
Harada R, Okamura N, Furumoto S et al (2016) 18F-THK5351: a novel PET radiotracer for imaging neurofibrillary pathology in Alzheimer’s disease. J Nucl Med 57:208–214
Harada R, Okamura N, Furumoto S et al (2015) [(18)F]THK-5117 PET for assessing neurofibrillary pathology in Alzheimer’s disease. Eur J Nucl Med Mol Imaging 42(7):1052–1061
Chien DT, Bahri S, Szardenings AK et al (2013) Early clinical PET imaging results with the novel PHF-tau radioligand [F-18]-T807. J Alzheimers Dis 34(2):457–468
Johnson KA, Schultz A, Betensky RA et al (2016) Tau PET imaging in aging and early Alzheimer’s disease. Ann Neurol 79:110–119
Marquie M, Normandin MD, Vanderburg CR et al (2015) Validating novel tau positron emission tomography tracer [F-18]-AV-1451 (T807) on postmortem brain tissue. Ann Neurol 78(5):787–800
Jack CR Jr, Knopman DS, Jagust WJ et al (2010) Hypothetical model of dynamic biomarkers of the Alzheimer’s pathological cascade. Lancet Neurol 9(1):119–128
Majounie E, Cross W, Newsway V et al (2013) Variation in tau isoform expression in different brain regions and disease states. Neurobiol Aging 34(7):1922 e7–1922 e12
Houlden H, Baker M, Morris HR et al (2001) Corticobasal degeneration and progressive supranuclear palsy share a common tau haplotype. Neurology 56(12):1702–1706
Wang Y, Mandelkow E (2016) Tau in physiology and pathology. Nat Rev Neurosci 17:22–35
Lee VM, Goedert M, Trojanowski JQ (2001) Neurodegenerative tauopathies. Annu Rev Neurosci 24:1121–1159
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Drzezga, A. (2016). Nuclear Imaging of Dementia. In: Hodler, J., Kubik-Huch, R., von Schulthess, G. (eds) Diseases of the Brain, Head and Neck, Spine 2016-2019. Springer, Cham. https://doi.org/10.1007/978-3-319-30081-8_26
Download citation
DOI: https://doi.org/10.1007/978-3-319-30081-8_26
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-30080-1
Online ISBN: 978-3-319-30081-8
eBook Packages: MedicineMedicine (R0)