Abstract
The oral mucosa is normally semitranslucent, allowing the color of underlying tissues to show through to a variable degree. Lesions may appear white secondary to increased thickness of the epithelium or decreased subepithelial vascularity, however, the etiology of white lesions is quite varied. This chapter reviews commonly seen benign white lesions of the oral cavity, with attention to differential diagnosis and treatment recommendations.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Hypertrophy
- Hyperplasia
- Keratin
- Acanthosis
- Hyperkeratosis
- Leukoedema
- Linea alba
- Lichen planus
- Morsicatio
- Leukoplakia
- Hairy tongue
- Filiform papillae
- Candidiasis
- Oral hairy leukoplakia
- Nicotinic stomatitis
- Smoker’s palate
- Tobacco pouch keratosis
- White sponge nevus
- Exfoliative cheilitis
- Angular cheilitis
Introduction
The oral mucosa is normally semitranslucent, allowing the color of underlying tissues such as fat, blood vessels, or melanin pigment to show through to a variable degree. This is affected by the thickness of the overlying tissue as well as the amount of surface keratin, concentration of submucosal fat or other substance, and density of the tissue capillary bed. For this reason, the thin nonkeratinized mucosa lining the vestibule and floor of mouth normally appears darker red than the thicker pale pink keratinized gingiva. Likewise, the vermilion zone of the lip appears red secondary to an abundant subepithelial capillary blood supply.
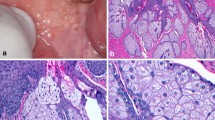
Inflammatory conditions frequently result in increased redness (erythema) due to thinning of the mucosa and/or increased underlying vascularity. Lesions most commonly appear white secondary to increased thickness of the epithelium, or to a lesser extent, decreased vascularity (Fig. 4.1). Thickening of the epithelium can be caused by epithelial hypertrophy or hyperplasia, edema, and increased production of surface keratin (hyperkeratosis). Thickening specifically in the spinous, or prickle, layer of the epithelium is referred to as acanthosis . Collapsed bullae or ulcerative lesions covered with a surface layer of fibrin may also appear white. Mechanical friction or other irritants to the mucosal lining can stimulate keratin production as a protective response. Some white lesions can be identified and treated on clinical grounds alone, whereas others require additional testing and/or biopsy for definitive diagnosis.
Appearance of the ventrolateral tongue in a patient following radiation therapy. The right side (a), which was in the field of radiation, appears pale white with obliteration of vasculature. On the left side (b), which was not radiated, normal appearing vessels are easily visualized. Also note small petechia secondary to bite trauma
Leukoedema
This is a common entity that presents as a generalized opacification or gray-white to milky opalescence of the buccal mucosa bilaterally (Fig. 4.2). It may appear filmy or wrinkled and cannot be rubbed off. The color becomes less evident or disappears entirely when the mucosa is stretched. It is usually noted as an incidental finding on exam and is asymptomatic; biopsy is not indicated. The etiology is not clearly established, however, there may be a hereditary component. This condition is more frequently seen in patients of African-American descent. Histologically, the tissue exhibits intracellular edema in the spinous cell layer of the epithelium. This is a benign condition, and no treatment is required.

Leukoedema
Linea Alba
Literally meaning “white line,” this is a focal hyperkeratosis resulting from chronic frictional trauma of the tissues rubbing against the adjacent teeth. It is most commonly seen as a horizontal white streak along the buccal mucosa at the level of the occlusal plane bilaterally and conforms to the configuration of the teeth in that area (Fig. 4.3). Frictional hyperkeratosis can also be seen focally in other commonly traumatized areas such as edentulous alveolar ridge spaces (Fig. 4.4), lips (Fig. 4.5), and lateral aspect of the tongue. This may be confused with lichen planus, which is a white lesion commonly occurring on the buccal mucosa (see Chap. 5).

Linea Alba
Cheek Biting
Hyperkeratosis from frictional trauma may be quite pronounced in cases of chronic cheek or lip biting or chewing (morsicatio buccarum, morsicatio labiorum). Lesions can appear ragged or frayed, with areas of ulceration or redness (Figs. 4.6, 4.7, and 4.8). Chronic chewing lesions of the tongue (morsicatio linguarum) can resemble oral hairy leukoplakia. Patients may or may not be aware of the habit and lesions are almost universally asymptomatic. Other than educating the patient as to the underlying cause, no treatment is necessary. There are no long-term consequences of this benign condition.

Cheek Biting
Hairy Tongue
Hairy tongue , or lingua villosa, is an entirely benign condition that can have a striking presentation. Elongation of the filiform papillae occurs secondary to decreased desquamation of the keratin layer causing a white coating on the tongue dorsum, usually posteriorly (Fig. 4.9). The surface coating can become quite matted and hair-like, with gagging or sensation of irritation in some patients if the papillae become extremely long. Oral burning may be noted in cases of superimposed candidiasis (see Chap. 7). Trapping of chromogenic organisms and debris and staining from coffee or tobacco can cause a range of color variations from black to green (Fig. 4.10). The etiology is unclear, but has been linked to the use of antibiotics and antimicrobial mouthrinses. It is also seen with dehydration, xerostomia (Fig. 4.11), poor nutrition, and a soft or minimally abrasive diet. Treatment is generally not necessary, and elimination of any contributing factors typically results in complete resolution. If lesions persist and are bothersome to the patient, gentle brushing or scraping of the tongue is recommended.

Hairy Tongue
Oral Hairy Leukoplakia
This is a benign, well-demarcated, generally asymptomatic white lesion of the ventrolateral tongue seen in HIV infected or immunosuppressed individuals. It can appear flat or raised, is often thick and corrugated, and frequently exhibits vertical ridge-like striations (Figs. 4.12 and 4.13). The lesions cannot be rubbed off, distinguishing the condition from pseuodomembranous candidiasis (see Chap. 7). The etiology is associated with Epstein-Barr virus infection and does not exhibit any malignant potential.

Oral Hairy Leukoplakia
Nicotinic Stomatitis
Direct irritation of the palatal mucosa from hot tobacco smoke can lead to inflammatory changes which are initia lly erythematous, then become white secondary to progressive epithelial hyperplasia and hyperkeratosis. The palate exhibits a cracked or wrinkled appearance, with punctate red dots representing inflammation and squamous metaplasia of minor salivary gland duct orifices (Figs. 4.14 and 4.15). This is commonly referred to as “smoker’s palate”. Any mucosa covered by a denture will be spared if the prosthesis is typically worn while smoking. The clinical appearance is usually diagnostic and biopsy is not necessary unless there are associated areas of ulceration or focal erythroplakia (see Chap. 9). This lesion is reversible with smoking cessation. Although this is not considered a precancerous condition, its presence directly correlates with the intensity of smoking and is usually a marker of heavy tobacco use. Observation is therefore recommended in conjunction with careful screening of the entire oral cavity.
Other white lesions related to tobacco are discussed in Chap. 9, including leukoplakia and tobacco pouch keratosis.

Nicotinic Stomatitis
White Sponge Nevus
This is an exceedingly rare lesion, inherited as an autosomal dominant trait, which usually presents in childhood or adolescence without gender predilection. Genetic analysis has pinpointed the defect to genes encoding mucosal keratin (keratin 4 and 13). It appears as a thick corrugated or folded white plaque with a spongy texture affecting the buccal mucosa bilaterally and is generally asymptomatic. The clinical appearance and family history are so distinctive that biopsy is not necessary. It can appear less frequently in other areas of the oral cavity as well as the esophagus, genitalia, and rectum, in which case biopsy may be indicated. This is a benign condition and no treatment is required.

White Sponge Nevus
Chemical Burn
A number of chemicals an d medications can be extremely caustic to the oral mucosa if they come in direct contact. Inappropriate topical use of certain medications by the patient, such as aspirin tablets or powder held against the tissue, can result in significant trauma, causing coagulation necrosis and sloughing of the epithelium. Iatrogenic injuries can also be caused by agents such as sodium hypochlorite (a disinfectant used for root canal irrigation), formocresol, silver nitrate, and acid etching solutions used during dental treatment. The initial lesion is usually white and leathery or wrinkled in appearance and generally very painful. If contact with the caustic substance was brief, which is usually the case, healing without scar or other complications should occur within 10–14 days and palliative treatment with topical agents can be used. If more severe injury occurs, with surface desquamation and presence of deeper tissue necrosis, then treatment with antibiotics and debridement may be required. Over the counter alcohol-containing mouthrinses and other topical dentrifices may cause superficial chemical burns, including hydrogen peroxide in concentrations greater than 3 % (Fig. 4.16). These are almost always painless and can be “peeled” away revealing normal appearing underlying mucosa.

Chemical Burn
Exfoliative Cheilitis
This is an unusual chronic conditi on of the lips characterized by crusting and peeling of the superficial epithelium, often associated with discomfort or burning. In most cases the entire upper and lower lips are involved, and there may be associated erythema and swelling (Fig. 4.17). The cause is believed to be related to repetitive lip irritation, such as chronic lip licking or picking, as well as other factitious or maladaptive behaviors. There may be an association with stress or depression in some patients. There is rarely an infectious component, but secondary infection with candida should be considered if features consistent with angular cheilitis (see Chap. 7) are present.

Exfoliative Cheilitis
Sources
Almazrooa SA, Woo SB, et al. Characterization and management of exfoliative cheilitis: a single-center experience. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013;116:e485–9.
Chi AC, Lambert PR, Pan Y, et al. Is alveolar ridge keratosis a true leukoplakia?: a clinicopathologic comparison of 2,153 lesions. J Am Dent Assoc. 2007;138:641–51.
Komatsu TL, Rivero ERC, et al. Epstein-Barr virus in oral hairy leukoplakia scrapes: identification by PCR. Braz Oral Res. 2005;19:317–21.
Martelli H, Pereira SM, Rocha TM, et al. White sponge nevus: report of a three-generation family. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:43–7.
Natarajan E, Woo SB. Benign alveolar ridge keratosis (oral lichen simplex chronicus): a distinct clinicopathologic entity. J Am Acad Dermatol. 2008;58:151–7.
Taybos G. Oral changes associated with tobacco use. Am J Med Sci. 2003;326:179–82.
Woo SB, Lin D. Morsicatio mucosae oris: a chronic oral frictional keratosis, not a leukoplakia. J Oral Maxillofac Surg. 2009;67:140–6.
Author information
Authors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Bruch, J.M., Treister, N.S. (2017). White Lesions. In: Clinical Oral Medicine and Pathology. Springer, Cham. https://doi.org/10.1007/978-3-319-29767-5_4
Download citation
DOI: https://doi.org/10.1007/978-3-319-29767-5_4
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-29765-1
Online ISBN: 978-3-319-29767-5
eBook Packages: MedicineMedicine (R0)