Abstract
Several sources of information suggest that humans evolved on a diet with an equal ratio of omega-6 (ω-6) to omega-3 (ω-3) fatty acids, whereas in today’s Western diet, this ratio is ~10:1 to 20–25:1. From an evolutionary perspective, Western diets are thus deficient in ω-3 fatty acids. This is problematic as while ω-3 and ω-6 fatty acids are important components of practically all cell membranes, they are not interconvertible in the human body. Moreover, a balanced ratio of ω-6 to ω-3 fatty acids is required for homeostasis and normal development. Excessive amounts of ω-6 polyunsaturated fatty acids (PUFAs) and a very high ω-6/ω-3 ratio, as is found in today’s Western diets, promote the pathogenesis of many diseases including cardiovascular disease, cancer, and inflammatory and autoimmune diseases. On the contrary, increased levels of ω-3 PUFA (a lower ω-6/ω-3 ratio) exert suppressive effects. We thus recommend that ω-3 and ω-6 fatty acids should be distinguished on food labels because they both are metabolically and functionally distinct and have opposing physiological effects. We further argue that a lower ratio of ω-6/ω-3 fatty acids is desirable as it is likely to reduce the risk of many of the chronic diseases of high prevalence in Western societies, as well as in the developing countries.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Omega-6/omega-3 fatty acid ratio
- Physiological aspects
- Opposing metabolic effects
- Genetic variation
- Cardiovascular disease and cancer
Modern agriculture, in particular agribusiness and its emphasis on production, changed animal feeds from grass to seeds and favoured the production of vegetable oils rich in ω-6 fatty acids. This has led to a pro-inflammatory diet characterized by an increased consumption of both linoleic acid (ω-6) and arachidonic acid (ω-6) and a decreased consumption of alpha-linoleic acid and its metabolites (ω-3). In the last 100–150 years, the absolute and relative change of ω-6 and ω-3 fatty acids in the food supply of Western societies led the Western diet to reach a ratio of 20:1 ω-6/ω-3. This ratio is at odds with human evolutionary history, during which a balance (1:1) existed between ω-6 and ω-3 fatty acids as ω-3 fatty acids were found in all foods consumed: meat, eggs, fish, wild plants, nuts, and berries. While a balance between the ω-6 and ω-3 fatty acids is consistent with human evolution and normal human development, a number of studies suggest that an imbalance lead to an increase in the risk of cardiovascular and other chronic diseases, particularly in those genetically predisposed. Therefore, we recommend that food labels distinguish between ω-6 and ω-3 fatty acids. In addition, in order to balance the consumption of ω-6 and ω-3 fatty acids, we advocate a decrease in the intake of vegetable oils high in ω-6 (corn oil, sunflower oil, safflower oil, cottonseed oil, and soybean oil) and an increase in the intake of oils both high in ω-3 fatty acids (flaxseed, perilla, chia, rapeseed, and walnuts) and low in ω-6 fatty acids (olive oil, macadamia nut oil, and hazelnut oil). Finally, we suggest people should eat more fish and less meat.
1 Introduction
There are two classes of essential fatty acids (EFA), omega-6 (ω-6) and omega-3 (ω-3). The distinction between ω-6 and ω-3 fatty acids is based on the location of the first double bond, counting from the methyl end of the fatty acid molecule (Fig. 9.1). ω-6 and ω-3 fatty acids are essential because humans, like all mammals, cannot synthesize them and must obtain them from the diet. ω-6 fatty acids are represented by linoleic acid (LA) (18:2w6) and ω-3 fatty acids by alpha-linolenic acid (ALA) (18:3w3). LA is plentiful in nature and is found in the seeds of most plants except for coconut, cocoa, and palm. ALA, on the other hand, is found in the chloroplasts of green leafy vegetables, and in the seeds of flax, rape, chia, perilla, and walnuts. Both essential fatty acids are metabolized to longer-chain fatty acids of 20 and 22 carbon atoms. LA is metabolized to arachidonic acid (AA) (20:4w6), while ALA is metabolized to eicosapentaenoic acid (EPA) (20:5w3) and docosahexaenoic acid (DHA) (22:6w3). This is achieved by increasing the chain length and the degree of unsaturation by adding extra double bonds to the carboxyl end of the fatty acid molecule [1] (Fig. 9.2). AA is found predominantly in the phospholipids of grain-fed animals, dairy, and eggs. EPA and DHA are found in the oils of fish, particularly fatty fish.
Structural formulas for ω-3 (a-linoleic = ALA), ω-6 (linoleic = LA), and ω-9 (oleic) fatty acids. The first number (before the colon) gives the number of carbon atoms in the molecule, and the second gives the number of double bonds. ω-3, ω-6, and ω-9 indicate the position of the first double bond in a given fatty acid molecule [1]
Desaturation and elongation of ω-3 and ω-6 fatty acids by the enzymes fatty acid desaturases FADS2 (D6) and FADS1 (D5) [10]
In mammals, including humans, the cerebral cortex, retina, testis, and sperm are particularly rich in DHA. DHA is one of the most abundant components of the brain’s structural lipids. DHA, like EPA, can be derived only from direct ingestion or by synthesis from dietary EPA or ALA: Humans and other mammals, except for certain carnivores such as lions, can convert LA to AA and ALA to EPA and DHA, although it is slow [2, 3]. There is competition between ω-6 and ω-3 fatty acids for the desaturation enzymes. Both fatty acid desaturase 1 (D-5) and fatty acid desaturase 2 (D-6) prefer ωALA to ωLA [2, 4, 5]. However, a high LA intake, such as that characterizing Western diets, interferes with the desaturation and elongation of ALA [3–6]. Similarly, trans-fatty acids interfere with the desaturation and elongation of both LA and ALA.
In addition, fatty acid desaturase 2 is the limiting enzyme and there is some evidence that it decreases with age [2]. Premature infants [7], hypertensive individuals [8], and some diabetics [9] are limited in their ability to make EPA and DHA from ALA. These findings are important and need to be considered when making dietary recommendations.
Mammalian cells cannot convert ω-6 to ω-3 fatty acids because they lack the converting enzyme, ω-3 desaturase. Ω-6 and ω-3 fatty acids are not interconvertible, are metabolically and functionally distinct, and often have important opposing physiological effects; therefore, their balance in the diet is important. When humans ingest fish or fish oil, the EPA and DHA from the diet partially replace the ω-6 fatty acids, especially AA, in the membranes of probably all cells, but especially in the membranes of platelets, erythrocytes, neutrophils, monocytes, and liver cells (reviewed in Refs. [10, 11]). AA and EPA are two alternative parent compounds for eicosanoid production (Fig. 9.3). Because of the increased amounts of ω-6 ω in the Western diet, the eicosanoid metabolic products from AA, specifically prostaglandins, thromboxanes, leukotrienes, hydroxy fatty acids, and lipoxins, are formed in larger quantities than those derived from ω-3 fatty acids, specifically EPA (Fig. 9.3) [10]. The eicosanoids from AA are biologically active in very small quantities and, if they are formed in large amounts, they contribute to the formation of thrombus and atheromas; to allergic and inflammatory disorders, particularly in susceptible people; and to proliferation of cells [12] (Table 9.1). Thus, a diet rich in ω-6 fatty acids shifts the physiological state to one that is proinflammatory, prothrombotic, and proaggregatory, with increases in blood viscosity, vasospasm, and vasoconstriction.
Oxidative metabolism of arachidonic acid (AA) and eicosapentaenoic acid by the cyclooxygenase and 5-lipoxygenase pathways. 5-HPETE denotes the 5-hydroperoxyeicosatetranoic acid, and 5-HPEPE denotes the 5-hydroxyeicosapentaenoic acid [10]
1.1 The Importance of the ω-6/ω-3 Fatty Acid Ratio: And Evolutionary Aspects
A balance existed between ω-6 and ω-3 fatty acids during the long evolutionary history of the genus Homo [13]. During evolution, ω-3 fatty acids were found in all foods consumed: particularly meat, fish, wild plants, nuts, and berries [13–29]. Recent studies by Cordain et al. [30] on the composition of the meat of wild animals confirm the original observations of Crawford [15] and Sinclair et al. [31]. However, rapid dietary changes over short periods of time as have occurred over the past 100–150 years is a totally new phenomenon in human evolution (Fig. 9.4). A balance between the ω-6 and ω-3 fatty acids is a physiological state that is less inflammatory in terms of gene expression [32], prostaglandin and leukotriene metabolism, and interleukin-1 (IL-1) production [10]. The current recommendation to substitute vegetable oils (ω-6) for saturated fats leads to increases in IL-1, prostaglandins, and thromboxanes of the 2 series from LA that are prothrombotic and leukotrienes of the 3 series that are proinflammatory. It is not consistent with human evolution and may lead to maladaptation in those genetically predisposed (Table 9.1; Figs. 9.2 and 9.3).
Hypothetical scheme of fat, fatty acid (ω6, ω3, trans, and total) intake (as percent of calories from fat), and intake of vitamins E and C (mg/d). Data were extrapolated from cross-sectional analyses of contemporary hunter-gatherer populations and from longitudinal observations and their putative changes during the preceding 100 years [10]
Prior to the agricultural revolution, humans ate a wide variety of wild plants, whereas today about 17 % of plant species provide 90 % of the world’s food supply, with the greatest percentage contributed by cereal grains [33]. Agribusiness and modern agriculture contributed to the decrease in ω-3 fatty acids in animal carcasses. Wild animals and birds who feed on wild plants are very lean, with a carcass fat content of only 3.9 % [34], and contain about five times more polyunsaturated fatty acids (PUFAs) per gram than those found in domestic livestock [15, 16]. Most importantly, 4 % of the fat of wild animals contains EPA. Domestic beef contains very small or undetectable amounts of ALA because cattle are fed grains rich in ω-6 fatty acids and poor in ω-3 fatty acids [17], whereas deer that forage on ferns and mosses contain more ω-3 fatty acids in their meat.
Although diets differed in the various geographic areas [35], a number of investigators including Crawford [15], Cordain et al. [30], Eaton et al. [36], and Kupiers et al. [37] have shown that during the Paleolithic period, the diets of humans included equal amounts of ω-6 and ω-3 fatty acids from both plants (LA + ALA) and from the fat of animals in the wild and fish (AA + EPA + DHA). Recent studies by Kuipers et al. [37] estimated macronutrient and fatty acid intakes from an East African Paleolithic diet in order to reconstruct multiple Paleolithic diets and thus estimated the ranges of nutrient intakes on which humans evolved. They found (range of medians in energy %) intakes of moderate-to-high protein (25–29), moderate-to-high fat (30–39), and moderate carbohydrates (39–40). Just as others have concluded previously, Kuipers et al. [37] stated “compared with Western diets, Paleolithic diets contained consistently high-protein and long-chain PUFA and lower LA.” Guil-Guerrero et al. [38] determined the fat composition of frozen mammoths (from 41,000 to 34,000 years BP), Bisons from Early Holocene (8200–9300 years BP) and horses from Middle Holocene (4600–4400 years BP), often consumed by Paleolithic/Neolithic hunters-gatherers, and concluded. It “contained suitable amounts of ω-3 and ω-6 fatty acids, possibly in quantities sufficient to meet today’s dietary requirements for good health.” The elucidation of sources of ω-3 fatty acids available for the humans who lived in the Paleolithic and Neolithic is highly relevant to ascertain the availability of nutrients at that time and to draw conclusions about healthy dietary habits for present-day humans. As in previous studies, the amount of ALA was higher than LA in the fat of the frozen specimens [39, 40] (Tables 9.2 and 9.3).
Modern agriculture, by changing animal feeds as a result of its emphasis on production, has decreased the ω-3 fatty acid content in many foods: green leafy vegetables, animal meats, eggs, and even fish [18–21]. Foods from edible wild plants contain a good balance of ω-6 and ω-3 fatty acids. Purslane, a wild plant, in comparison with spinach, red leaf lettuce, buttercrunch lettuce, and mustard greens, has eight times more ALA than the cultivated plants [25]. Modern aquaculture produces fish that contain less ω-3 fatty acids than do fish grown naturally in the ocean, rivers, and lakes [20]. The fatty acid composition of egg yolk from free-ranging chicken has an ω-6:ω-3 ratio of 1.3, whereas the US Department of Agriculture (USDA) egg has a ratio of 19.9 [21]. By enriching the chicken feed with fishmeal or flaxseed, the ratio of ω-6:ω-3 decreased to 6.6 and 1.6, respectively.
1.2 Genetic Adaptation of Fatty Acid Metabolism
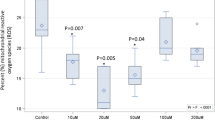
There are important genetic variables in fatty acid biosynthesis involving fatty acid desaturase 1 (FADS1) and fatty acid desaturase 2 (FADS2), which encode rate-limiting enzymes for fatty acid metabolism (Fig. 9.2). Ameur et al. [41] performed genome-wide genotyping (n = 5, 652 individuals) of the FADS region in five European population cohorts and analyzed available genomic data from human populations, archaic hominins, and more distant primates. Their results show that present-day humans have two common FADS haplotypes A and D that differ dramatically in their ability to generate LC-PUFAs. The most common haplotype, denoted haplotype D, was associated with high lipid levels (P = 1 × 10−65), whereas the less common haplotype (haplotype A) was associated with low levels (P = 1 × 10−52). The haplotype D associated with the enhanced ability to produce AA and DHA from their precursors LA and ALA, respectively, is specific to humans and has appeared after the split of the common ancestor of humans and Neanderthals. This haplotype shows evidence of a positive selection in African populations in which it is presently almost fixed and it is less frequent outside of Africa. Haplotype D provides a more efficient synthesis of LC-PUFAs, and in today’s high LA ω-6 dietary intake from vegetable oils, it leads to increased synthesis of AA from LA. Thus, it represents a risk factor for coronary heart disease (CHD), cancer, obesity, diabetes, and the metabolic syndrome, thus adding further to health disparities in populations of African origin living in the West, in addition to lower socioeconomic status.
As estimated from the human genome diversity panel (HGDP-CEPH) [42], the geographic distributions of haplotypes A and D differ dramatically among continents. In African populations, HGDP populations haplotype A is essentially absent (has a frequency of 1 %), whereas in Europe, West, South and East Asia, and Oceania, it occurs at a frequency of 25–50 %. Among the 126 Native Americans included in HGDP, haplotype A occurs at a frequency of 97 %. Among individuals of African ancestry, 49 % carry mixed FADS haplotypes with a higher resemblance to haplotype D than to haplotype A, consistent with a decay of haplotype D by recombination in African populations.
It has been proposed that a shift in diet, characterized by access to food sources that are rich in essential LC-PUFAs, was initiated about 2 million years ago [43]. This change in the availability of LC-PUFAs might have been important for maintaining the proportionally large hominoid brain relative to body size. Humans use a very large portion of dietary fats, predominantly AA and DHA to feed the brain [43]. Consequently, human’s ability to more efficiently synthesize LC-PUFAs from their precursors might have played an important role in their ability to survive in periods where AA and DHA rich diets were not available. Therefore, haplotype D is likely to have been advantageous to humans living in environments with limited access to these fatty acids, and this could explain the positive selection for haplotype D in African populations. However, as the present Western diet is high in LA due to the elevated intake of vegetable oils high in ω-6 fatty acids, the advantage of having faster biosynthesis of LC-PUFAs for carriers of haplotype D has turned into a disadvantage: High intake of LA leads to an increased production of AA and thereby increases the synthesis of AA-derived pro-inflammatory eicosanoids, which are associated with the increased risk of atherosclerotic vascular disease [44].
1.3 Research Findings
1.3.1 The Diet of Crete and Its Relation to Cardiovascular Disease and Cancer
Over the past 15 years, a number of animal experiments, epidemiological investigations, and double-blind controlled clinical trials have confirmed the hypotriglyceridemic, anti-inflammatory, and antithrombotic aspects of ω-3 fatty acids [45–50] as well as the essentiality of ω-3 fatty acids, particularly DHA, for the development of retina and brain in the premature infant. It therefore became important to investigate the ω-3 fatty acid composition of diets that have been shown to be associated with a decreased rate of cardiovascular disease and cancer. Such an opportunity then arose with the diet of Crete [51].
The population of Crete was one of the populations participating in the Seven Countries Study [52]. The others were the populations of the former Yugoslavia, Italy, the Netherlands (Zutphen), Finland, USA, and Japan. The results of the Seven Countries Study are interesting because they show that the population of Crete had the lowest rate of cardiovascular disease and cancer, followed by the population of Japan. The investigators concluded that the reason must be the high olive oil intake and the low saturated fat intake of the “Mediterranean diet.” The fact that Crete had a high-fat diet, 37 % of energy from fat, and Japan had a low-fat diet, 11 % of energy from fat, was not very much discussed nor were any other fatty acids considered, despite the fact that the people of Crete ate 10 times more fish than the US population. Furthermore, the people of Crete ate plenty of vegetables, fruits, nuts, and legumes, all rich sources of folate, calcium, vitamins, and minerals. In addition, since the meat came from animals that grazed, rather than being grain-fed, it contained ω-3 PUFAs as did their milk and milk products, such as cheese. The population of Crete ate snails about three times per week throughout the year. Renaud has shown that the snails of Crete and Greece contain more ω-3 fatty acids and less ω-6 fatty acids than the snails of France (personal communication). Figs are the most popular fruit eaten throughout the year. Both fresh and dried figs contain equal amounts of LA + ALA and are rich in vitamins and minerals, especially calcium.
The traditional Greek diet, including the diet of Crete, includes wild plants. Wild plants are rich sources of ω-3 fatty acids and antioxidants [19, 22, 25]. A commonly eaten plant is purslane. Purslane is rich in ALA (400 mg/100 g) as well as in vitamin E (12 mg/100 g) [25]. In Crete and Greece, purslane is eaten fresh in salads, soups, and omelets, or cooked with poultry, and during the winter months, the dried purslane is used in soups, vegetable pies, and as a tea for sore throats and earaches. It is highly recommended for pregnant and lactating women and for patients with diabetes. The purslane study was just the beginning in our involvement in a series of studies that investigated the ω-3 fatty acids in the Greek diet under conditions similar to those prior to 1960 [19, 21, 22, 25]. In the Greek countryside, chickens wander in the farm, eat grass, purslane, insects, worms, and dried figs, all good sources [19, 21, 22, 25] of ω-3 fatty acids. As mentioned earlier, their eggs have a ratio of ω-6/ω-3 fatty acids of 1.3, whereas the USDA egg has a ratio of 19.4.
Similarly, Greek cheeses contain ω-3 fatty acids, whereas American cheeses do not. Noodles made with milk and eggs in Greece also contain ω-3 fatty acids. A pattern thus began to unfold. The diet of Greece, including Crete prior to 1960, contained ω-3 fatty acids in every meal—breakfast, lunch, dinner, and snacks. Figs stuffed with walnuts are a favorite snack. Both figs and walnuts contain ω-3 fatty acids. Contrast this snack with a chocolate chip cookie, which contains trans-fatty acids and ω-6 fatty acids from the partially hydrogenated oils used in preparation [28]. While these studies were carried out between 1984 and 1986, further analyses of blood specimens from the Seven Countries Study [52] were published in 1993 by Sandker et al. [53], indicating that the serum cholesteryl esters of the population in Crete had threefold the amount of ALA as compared to the population of Zutphen in the Netherlands. Similar data indicated that the Japanese population also had higher concentrations of ω-3 fatty acids than that of the Netherlands. Here was the missing link. It was the higher concentrations of ω-3 fatty acids and the lower concentration of ω-6 fatty acids leading to a balanced ω-6/ω-3 that added protection for cardiovascular disease. This is in addition to the olive oil, wine, fruits, and vegetables of the diet of Crete, which is superior to other Mediterranean diets due to a balanced ω-6 and ω-3 fatty acid intake and high antioxidants (Table 9.3). Participants from the two countries (Crete and Japan) with the lowest CHD in the Seven Countries Study had a higher intake of fish and ALA. The Japanese obtained ALA from perilla oil and soybean oil and the population of Crete from purslane, other wild plants, walnuts, and figs. Additional studies showed that the population of Crete not only had higher serum cholesteryl ester levels of ALA but also lower LA (18:2w-6) [53].
Renaud had been working with ALA and shown that it decreases platelet aggregation [54]. Everything seems now to fall into place in terms of defining the characteristics of the diet of the population of Crete. Their diet was very similar to the Paleolithic diets in composition. It was low in saturated fat, balanced in the essential fatty acids (ω-6 and ω-3) [40] (Table 9.3), very low in trans-fatty acids, and high in vitamins E and C. This diet formed the basis of the diet used by Renaud and de Lorgeril in their now famous Lyon Study [51, 54–56]. The Lyon study is a prospective randomized single-blinded secondary prevention trial that compared the effects of a modified Crete diet enriched with ALA to those of a Step I American Heart Association Diet. A total of 605 patients were divided into two groups, 302 in the experimental group were fed the modified diet of Crete, including 2 g of ALA per day, and 303 in the control group followed the Step I American Heart Association diet. Two months after randomization, plasma levels of vitamins C and E (P < 0.5) and ω-3 fatty acids (P < 0.001) were higher in experimental subjects while those of ω-6 fatty acids were lower (P < 0.001). The ratio of ω-6/ω-3 fatty acids was 4/1. After a mean follow-up of 27 months, there were 16 cardiac deaths in the control group and three in the experimental group, and 17 non-fatal myocardial infarctions in the control group and five in the experimental group. The combined risk ratio for these two main end points was 0.27 (95 % CI 0.12–0.59, P = 0.001) after adjustment for prognostic variables. Overall, mortality was 20 in the control group, eight in the experimental group, and an adjusted risk ratio of 0.30 (95 % CI 0.11–0.82, P = 0.02).
This study showed a decrease in death rate by 70 % in the experimental group and clearly showed that a modified Crete diet low in butter and meats, such as deli products but high in fish and fruits and vegetables, and enriched with ALA, is more efficient than that of the American Heart Association or similar prudent diets in the secondary prevention of coronary events and death. The same subjects were followed for 5 years. At 4 years of follow-up, de Lorgeril et al. [57] reported that the reduction of risk in the experimental subjects compared with control subjects was 56 % for total deaths, and 61 % for cancers, indicating that a modified diet of Crete is associated with lower risk for CHD and cancer.
The diet of Crete or the traditional diet of Greece resembles hunter-gatherers’ diets in terms of antioxidants, saturated fat, and monounsaturated fat and in the ω-6/ω-3 ratio. The Lyon Heart Study and subsequently the Singh et al. study [58] support the importance of having a diet consistent with human evolution. Western diets today deviate from Paleolithic diets and are associated with high rates of cardiovascular disease, diabetes, obesity, and cancer. In as much as the health of the individual and the population in general is the result of the interaction between the genetic profile and the environment, nutrition is one of the most important environmental factors [59].
1.3.2 Other Beneficial Effects of ω-3 Fatty Acids
In addition to the studies of CHD and Cancer, a number of clinical intervention studies have shown that the high ω-6/ω-3 ratio in Western diets has increased the risk of many of the chronic “diseases of civilization” as a result of a “mismatch” between our genes and the environment. Clinical intervention studies in patients with asthma [60], osteoporosis [61, 62], mental health and major depression [63], bipolar disorder [64, 65], and mood [66] have shown improvements upon treatment with EPA + DHA. A number of studies show that LA increases low-density lipoprotein oxidation and the severity of coronary atherosclerosis and inhibits EPA incorporation from dietary fish oil supplements in human subjects, whereas decreasing LA in the diet while maintaining constant ALA increases EPA in plasma phospholipids in healthy men. A lower ω-6/ω-3 ratio as part of a Mediterranean diet decreases vascular endothelial growth factor. As the ω-6/ω-3 ratio decreases, so does the platelet aggregation. The higher the ratio of ω-6/ω-3 fatty acids in platelet phospholipids, the higher the death rate from cardiovascular disease. A high plasma ω-6/ω-3 ratio increases inflammatory markers, thus increasing the risk of chronic diseases. EPA and DHA attenuate the rate of shortening of telomere length suggesting a decrease in the rate of the aging process [67], whereas LA intake is associated with shorter telomere length [68].
1.4 Implications for Policy and Practice
Studies on the evolutionary aspects of diet suggest that during evolution, ω-3 fatty acids were present in practically all foods that humans ate and in equal or higher amounts than the ω-6 fatty acids. Western diets are characterized by high ω-6 and low ω-3 fatty acid intake, whereas during most of the human evolutionary history, there was a balance between ω-6 and ω-3 fatty acids. Today, human beings live in a nutritional environment that differs from that for which their genetic constitution was selected. The balance of ω-6/ω-3 fatty acids is an important determinant in maintaining homeostasis, normal development, and mental health throughout the life cycle. Excessive amounts of ω-6 PUFA and a very high ω-6/ω-3 ratio, as is found in today’s western diets, promote the pathogenesis of many diseases, including cardiovascular disease, cancer, and inflammatory and autoimmune diseases, and interfere with normal brain development.
Diets must be balanced regarding ω-6 and ω-3 fatty acids to be consistent with the evolutionary understanding of the human diet. This balance can best be accomplished by decreasing the intake of oils rich in ω-6 fatty acids (corn oil, sunflower, safflower, cottonseed, and soybean) and increasing the intake of oils rich in ω-3s (canola, flaxseed, perilla, and chia) and olive oil which is particularly low in ω-6 fatty acids and high in monounsaturated fatty acids.
The ratio of ω-6 and ω-3 fatty acids in the brain is between 1:1 and 2:1, which is in agreement with the data from the evolutionary aspects of diet, genetics, and the studies with the fat-1 transgenic animal model [69, 70]. Therefore, a ratio of 1:1 to 2:1 ω-6 to ω-3 fatty acids should be the target ratio for health [10, 71]. Because chronic diseases are multigenic and multifactorial, it is quite possible that the therapeutic dose of the ω-3 fatty acids will vary between individuals: It will depend on the degree of severity of diseases, which in turn results from the genetic predispositions, and notably the endogenous metabolism of LA and ALA.
In the Lyon Heart Study, a ratio of 4:1 LA:ALA decreased total mortality by 70 % in patients with one episode of myocardial infarction. Whether an ω-6/ω-3 ratio of 3:1 to 4:1 could prevent the pathogenesis of many diseases induced by today’s Western diets, a target of 1:1 to 2:1 appears to be consistent with studies on evolutionary aspects of diet, neurodevelopment, and genetics. The ω-6/ω-3 fatty acid ratio in red cell membrane phospholipids could be used as a biomarker for dietary intake and endogenous metabolism, thus providing a more accurate nutritional status for dietary recommendations.
It is essential that food labels distinguish between ω-3 and ω-6 fatty acids instead of the current label that distinguishes only saturated fatty acids (SFAs), monounsaturated fatty acids (MONOs), and polyunsaturated fatty acids (PUFAs). Regulatory agencies should follow the scientific advances in forming dietary regulations and recommendations.
Clinical intervention studies should include complete fatty acid information of the background diet as well as fatty acid levels in red cell membrane phospholipids. Discrepancies in the results of clinical studies are often due to inadequate data on fatty acid levels before, during, and at the completion of the studies.
References
Simopoulos AP (1991) Ω-3 fatty acids in health and disease and in growth and development. Am J Clin Nutr 54:438–463
de Gomez Dumm INT (1975) Brenner RR. Oxidative desaturation of alphalinolenic, linoleic, and stearic acids by human liver microsomes. Lipids 10:315–317
Emken EA, Adlof RO, Rakoff H, Rohwedder WK (1989) Metabolism of deuterium-labeled linolenic, linoleic, oleic, stearic and palmitic acid in human subjects. In: Baillie TA, Jones JR (eds) Synthesis and application of isotopically labeled compounds 1988. Elsevier Science Publishers, Amsterdam, pp 713–716
Hague TA, Christoffersen BO (1984) Effect of dietary fats on arachidonic acid and eicosapentaenoic acid biosynthesis and conversion to C22 fatty acids in isolated liver cells. Biochim Biophys Acta 796:205–217
Hague TA, Christoffersen BO (1986) Evidence for peroxisomal retroconversion of adrenic acid (22:4n6) and docosahexaenoic acid (22:6n3) in isolated liver cells. Biochim Biophys Acta 875:165–173
Indu M, Ghafoorunissa (1992) n-3 fatty acids in Indian diets—comparison of the effects of precursor (alpha-linolenic acid) vs product (long chain n-3 polyunsaturated fatty acids). Nutr Res 12:569–582
Carlson SE, Rhodes PG, Ferguson MG (1986) Docosahexaenoic acid status of preterm infants at birth and following feeding with human milk or formula. Am J Clin Nutr 44:798–804
Singer P, Jaeger W, Voigt S, Theil H (1984) Defective desaturation and elongation of n-6 and n-3 fatty acids in hypertensive patients. Prostaglandins Leukot Med 15:159–165
Honigmann G, Schimke E, Beitz J, Mest HJ, Schliack V (1982) Influence of a diet rich in linolenic acid on lipids, thrombocyte aggregation and prostaglandins in type I (insulin-dependent) diabetes. Diabetologia 23:175 (abstract)
Simopoulos AP (2008) The importance of the omega-6/omega-3 fatty acid ratio in cardiovascular disease and other chronic diseases. Exp Biol Med (Maywood). 233(6):674–688
Simopoulos AP (1999) Essential fatty acids in health and chronic disease. Am J Clin Nutr 70(suppl):560S–569S
Simopoulos AP (2011) The importance of the Ω-6/Ω-3 Balance in health and disease: evolutionary aspects of diet. In: Simopoulos AP (ed) Healthy agriculture, healthy nutrition, healthy people, vol 102. World Rev Nutr Diet. Karger, Basel, pp 10–21
Eaton SB, Konner M (1985) Paleolithic nutrition. A consideration of its nature and current implications. New Engl J Med 312:283–289
Simopoulos AP (1998) Overview of evolutionary aspects of w3 fatty acids in the diet. In: Simopoulos AP (ed) The return of w-3 fatty acids into the food supply. I. Land-based animal food products and their health effects. World Rev Nutr Diet. Karger, Basel, pp 1–11
Crawford MA (1968) Fatty acid ratios in free-living and domestic animals. Lancet 1:1329–1333
Wo CKW, Draper HH (1975) Vitamin E status of Alaskan Eskimos. Am J Clin Nutr 28:808–813
Crawford MA, Gale MM, Woodford MH (1969) Linoleic acid and linoleic acid elongation products in muscle tissue of Syncerus caffer and other ruminant species. Biochem J 115:25–27
Raper NR, Cronin FJ, Exler J (1992) Ω-3 fatty acid content of the US food supply. J Am College Nutr 11:304
Simopoulos AP, Salem N Jr (1986) Purslane: a terrestrial source of ω-3 fatty acids. N Engl J Med 315:833
van Vliet T, Katan MB (1990) Lower ratio of n-3 to n-6 fatty acids in cultured than in wild fish. Am J Clin Nutr 51:l–2
Simopoulos AP, Salem N Jr (1992) Egg yolk as a source of long-chain polyunsaturated fatty acids in infant feeding. Am J Clin Nutr 55:411–414
Simopoulos AP, Norman HA, Gillapsy JE et al (1992) Common purslane: a source of ω-3 fatty acids and antioxidants. J Am College Nutr 11:374–382
Simopoulos AP (1989) Nutrition and fitness. JAMA 261:2862–2863
Simopoulos AP, Salem N Jr (1989) n-3 Fatty acid in eggs from range-fed Greek chickens. N Engl J Med 321:1412
Simopoulos AP, Norman HA, Gillapsy JE (1995) Purlsane in human nutrition and its potential for world agriculture. World Rev Nutr Diet 77:7–74
Simopoulos AP (1995) Trans-fatty acids. In: Spiller GA (ed) Handbook of lipids in human nutrition. CRC Press, Florida, pp 91–99
Dupont J, White PJ, Feldman EB (1991) Saturated and hydrogenated fats in food in relation to health. J Am College Nutr 10:577–592
Litin L, Sacks F (1993) Trans-fatty acid content of common foods. N Engl Med 329:1969–1970
Guil JL, Torija ME, Gimenez JJ et al (1996) Identification of fatty acids in edible wild plants by gas chromatography. J Chromatog A 719:229–235
Cordain L, Martin C, Florant G, Watkins BA (1998) The fatty acid composition of muscle, brain, marrow and adipose tissue in elk: evolutionary implications for human dietary lipid requirements. World Rev Nutr Diet 83:225–226
Sinclair AJ, Slattery WJ, O’Dea K (1982) The analysis of polyunsaturated fatty acids in meat by capillary gas-liquid chromatography. J Food Sci Agri 33:771–776
Simopoulos AP (1996) The role of fatty acids in gene expression: health implications. Ann Nutr Metab 40:303–311
Simopoulos AP (ed) (1995) Plants in human nutrition. World Rev Nutr Diet 77
Ledger HP (1968) Body composition as a basis for a comparative study of some East African animals. Symp Zool Soc London 21:289–310
Elton S (2008) Environments, adaptation, and evolutionary medicine: should we be eating a stone age diet? In: Elton S, O’Higgins P (eds) Medicine and evolution: current applications, future prospects. CRC Press, Boca Raton, pp 9–34
Eaton SB, Konner M, Shostak M (1988) Stone agers in the fast lane: chronic degenerative diseases in evolutionary perspective. Am J Med 84:739–749
Kuipers RS et al (2010) Estimated macronutrient and fatty acid intakes from an East African Paleolithic diet. Br J Nutr 104(11):1666–1687
Guil-Guerrero JL et al (2014) The fat from frozen mammals reveals sources of essential fatty acids suitable for Palaeolithic and Neolithic humans. PLoS ONE 9(1):e84480
Eaton SB, Eaton SB 3rd, Sinclair AJ, Cordain L, Mann NJ (1998) Dietary intake of long-chain polyunsaturated fatty acids during the Paleolithic. In: Simopoulos AP (ed) The return of w-3 fatty acids into the food supply. I. Land-based animal food products and their health effects, vol 83. World Rev Nutr Diet. Karger, Basel, pp 12–23
Simopoulos AP (2003) Importance of the ratio of ω-6/ω-3 essential fatty acids: evolutionary aspects. World Rev Nutr Diet 92:1–22
Ameur A et al (2012) Genetic adaptation of fatty-acid metabolism: a human-specific haplotype increasing the biosynthesis of long-chain Ω-3 and Ω-6 fatty acids. Am J Hum Genet 90:809–820
Li JZ, Absher DM, Tang H, Southwick AM, Casto AM, Ramachandran S, Cann HM, Barsh GS, Feldman M, Cavalli-Sforza LL, Myers RM (2008) Worldwide human relationships inferred from genome-wide patterns of variation. Science 319:1100–1104
Leonard WR, Snodgrass JJ, Robertson ML (2010) Evolutionary perspectives on fat ingestion and metabolism in humans. In: Montmighteur JP, Le Coutre J (eds) Fat detection: taste, texture, and post ingestive effects. CRC Press, Boca Raton, FL
Martinelli N, Consoli L, Olivieri O (2009) A ‘desaturase hypothesis’ for atherosclerosis: Janus-faced enzymes in ω-6 and ω-3 polyunsaturated fatty acid metabolism. J Nutrigenet Nutrigenomics 2:129–139
Simopoulos AP, Kifer RE, Martin RR (eds) (1986) Health effects of polyunsaturated fatty acids in seafoods, proceedings from the conference. Academic Press, Orlando
Galli C, Simopoulos AP (eds) (1989) Dietary w3 and w6 fatty acids: biological effeots and nutritional essentiality. Plenum Publishing Corporation, New York
Simopoulos AP, Kifer RR, Martin RE, Barlow SM (eds) Health effects of w3 polyunsaturated fatty acids in seafoods. World Rev Nutr Diet 66
Galli C, Simopoulos AP, Tremoli E (eds) Effects of fatty acids and lipids in health and disease. World Rev Nutr Diet 76
Galli C, Simopoulos AP, Tremoli E (eds) Fatty acids and lipids: biological aspects. World Rev Nutr Diet 75
Salem N Jr, Simopoulos AP, Galli C, Lagarde M, Knapp H (eds) Proceedings of the 2nd congress of ISSFAL on fatty acids and lipids from cell biology to human disease. Lipids 31(Supplement):S-l–S-326
Simopoulos AP, Robinson J (1998) The Ω plan. The medically proven diet that gives you the essential nutrients you need. Macmillan, New York
Keys A (1970) Coronary heart disease in seven countries. Circulation 41(suppl):l–211
Sandker GW, Kromhout D, Aravanis C et al (1993) Serum lipids in elderly men in Crete and The Netherlands. Eur J Clin Nutr 47:201–208
Renaud S, Godsey F, Dumont F et al (1986) Influence of long-term diet modification on platelet function and composition in Moselle farmers. Am J Clin Nutr 43:136–150
De Lorgeril M, Renaud S, Mamelle N et al (1994) Mediterranean alpha-linolenic acid rich-diet in the secondary prevention of coronary heart disease. Lancet 343:1454–1459
Renaud S, de Lorgetil M, Delaye J et al (1995) Cretan Mediterranean diet for prevention of coronary heart disease. Am J Clin Nutr 6l(suppl):1360S–1367S
de Lorgeril M, Salen P, Martin J-L et al (1998) Mediterranean dietary pattern in a randomized trial. Prolonged survival and possible reduced cancer rate. Arch Intern Med 158:1181–1187
Singh RB, Niaz MA, Sharma JP et al (1997) Randomized, double-blind, placebo-controlled trial of fish oil and mustard oil in patients with suspected acute myocardial infarction: the Indian experiment of infarct survival 4. Cardivasc Drugs Ther 11:485–491
Simopoulos AP, Herbert V, Jacobson B (1995) The healing diet: how to reduce your risks and live a longer and healthier life if you have a family history of cancer, heart disease, hypertension, diabetes, alcoholism, obesity, food allergies. Macmillan Publishers, New York
Broughton KS, Johnson CS, Pace BK, Liebman M, Kleppinger KM (1997) Reduced asthma symptoms with n-3 fatty acid ingestion are related to 5-series leukotriene production. Am J Clin Nutr 65:1011–1017
Weiss LA, Barret-Connor E, von Muhlen D (2005) Ratio of n-6 to n-3 fatty acids and bone mineral density in older adults: the Rancho Bernardo Study. Am J Clin Nutr 81:934–938
Hogstrom M, Nordstrom P, Nordstrom A (2007) n-3 fatty acids are positively associated with peak bone mineral density and bone accrual in healthy men: the NO2 study. Am J Clin Nutr 85:803–807
Maes M, Smith R, Christophe A, Cosyns P, Desnyder R, Meltzer H (1996) Fatty acid composition in major depression: decreased ω3 fractions in cholesteryl esters and increased C20:4 ω6/C20:5 ω3 ratio in cholesteryl esters and phospholipids. J Affect Disord 38:35–46
Locke CA, Stoll AL (2001) Ω-3 fatty acids in major depression. World Rev Nutr Diet 89(173–185):118
Stoll AL, Severus WE, Freeman MP, Rueter S, Zboyan HA, Diamond E, Cress KK, Marangell LB (1999) Ω3 fatty acids in bipolar disorder: a preliminary double-blind, placebo-controlled trial. Arch Gen Psychiatry 56:407–412
Fontani G et al (2005) Cognitive and physiological effects of Ω-3 polyunsaturated fatty acid supplementation in healthy subjects. Eur J Clin Invest 35(11):691–699
Kiecolt-Glaser JK, Epel ES, Belury MA, Andridge R, Lin J, Glaser R, Malarkey WB, Hwang BS, Blackburn E (2013) Ω-3 fatty acids, oxidative stress, and leukocyte telomere length: a randomized controlled trial. Brain Behav Immun 28:16–24
Cassidy A, De Vivo I, Liu Y, Han J, Prescott J, Hunter DJ, Rimm EB (2010) Associations between diet, lifestyle factors, and telomere length in women. Am J Clin Nutr 91(5):1273–1280
Kang JX, Liu A (2013) The role of the tissue ω-6/ω-3 fatty acid ratio in regulating tumor angiogenesis. Cancer Metastasis Rev 32(1–2):201–210
Kang JX (2011) The ω-6/ω-3 fatty acid ratio in chronic diseases: animal models and molecular aspects. World Rev Nutr Diet 102:22–29
Simopoulos AP (2010) Genetic variants in the metabolism of omega-6 and omega-3 fatty acids: their role in the determination of nutritional requirements and chronic disease risk. Exp Biol Med 235:785–795
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Glossary
- Essential fatty acids (EFA)
-
Fatty acids that human and other animals must ingest because the body requires them for good health but cannot synthesize them
- Polyunsaturated fatty acids (PUFAs)
-
Fatty acids that contain more than one double bond in their backbone
- Linoleic acid (LA)
-
An EFA ω-6 fatty acid found in corn, sunflower, cottonseed, safflower, soybean, and other vegetable oils
- Alpha-linolenic acid (ALA)
-
An EFA ω-3 fatty acid found in nuts, rapeseed, flaxseed, perilla, canola, and chia oils
- Arachidonic acid (AA)
-
A PUFA ω-6 fatty acid
- Eicosapentaenoic acid (EPA)
-
A PUFA ω-3 fatty acid
- Docosahexaeboic acid (DHA)
-
A PUFA ω-3 fatty acid that is a primary structural component of the human brain, cerebral cortex, skin, sperm, testicles, and retina
- Fatty acid desaturase 1 (FADS1)
-
An enzyme that in humans is encoded by the FADS1 gene
- Fatty acid desaturase 2 (FADS2)
-
An enzyme that in humans is encoded by the FADS2 gene
- Haplotype
-
The group of genes that a progeny inherits from one parent
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Simopoulos, A.P. (2016). Evolutionary Aspects of the Dietary Omega-6/Omega-3 Fatty Acid Ratio: Medical Implications. In: Alvergne, A., Jenkinson, C., Faurie, C. (eds) Evolutionary Thinking in Medicine. Advances in the Evolutionary Analysis of Human Behaviour. Springer, Cham. https://doi.org/10.1007/978-3-319-29716-3_9
Download citation
DOI: https://doi.org/10.1007/978-3-319-29716-3_9
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-29714-9
Online ISBN: 978-3-319-29716-3
eBook Packages: MedicineMedicine (R0)