Abstract
Shoulder arthroplasty is an established successful treatment with increasing numbers of primary procedures being performed each year. There is also an increasing revision surgery burden linked to this and for a number of reasons. A comprehensive and logical approach, to the assessment of a patient for consideration of revision shoulder surgery, is provided. The evidence base for indications for revision surgery and expected outcomes has been comprehensively reviewed to aid surgical decision-making by the surgeon and patient.
Invaluable technical tips are presented, and described, to enable the revision surgeon to form an effective operative strategy to address those challenges commonly faced in the operating room. Specific issues related to the surgical exposure, including soft tissue releases and component removal, are covered in an accessible and reproducible format. Up-to-date evidence, from the literature, and the authors’ own experience in techniques for dealing with complex issues, such as bone loss from the proximal humerus and glenoid, are imparted. The increasing use of reverse geometry total shoulder replacement as a key tool in revision shoulder surgery is also highlighted.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Revision shoulder arthroplasty
- Revision total shoulder
- Anatomic shoulder replacement
- Reverse shoulder replacement
- Hemiarthroplasty
- Glenoid component
- Glenoid component failure
- Glenohumeral joint, loosening, radiolucent lines
- Humeral component
- Implant removal
- Humeral windows
- Soft tissue releases
- Bone grafting
- Bone loss, tumour prostheses
- Salvage shoulder surgery
- Instability
- Rotator cuff
- Infection
- Preoperative imaging
- CT scan
Introduction
Arthroplasty as a treatment for painful disabling conditions of the shoulder has undergone significant development since the first shoulder hemiarthroplasty (HA) performed by Neer in 1953 [1] for proximal humeral fracture. The two major advances in shoulder arthroplasty have been the introduction of the glenoid component for total shoulder arthroplasty (TSA) in 1974 [2] and the concept of semi-constrained reverse shoulder arthroplasty (RSA) popularised by Grammont [3]. With these advances in implant design, the indications for shoulder arthroplasty have increased dramatically, as has the need for revision surgery [4].
Management of the failed shoulder arthroplasty is challenging for the patient and surgeon. There may be many reasons why a primary shoulder arthroplasty has not produced the desired successful outcome. It is important that the shoulder surgeon has a thorough understanding of the concepts of revision shoulder arthroplasty to minimise pitfalls and optimise outcomes.
This chapter considers the evaluation of a failed shoulder arthroplasty, addresses the specific indications for revision shoulder arthroplasty, along with the surgical techniques for undertaking such procedures and the likely outcomes.
Evaluation
Prior to revision surgery, the patient must be fully evaluated with a detailed history, clinical examination and appropriate tests. Documenting previous shoulder surgery, perioperative events and implants used provides invaluable information for the revision arthroplasty surgeon. When assessing the patient who presents with a failed arthroplasty, the surgeon must make an assessment of a number of key factors:
-
Presence or absence of infection
-
Component positioning and stability of the joint
-
Loosening of either humeral or glenoid components
-
Wear of bearing surfaces – native or prosthetic
-
Integrity and function of the rotator cuff and deltoid
Patient Complaints
Pain is by far the most common reason for a patient to seek further treatment following shoulder arthroplasty. Pain may occur at rest, prevent activities of daily living and disturb sleep. Another common reason for revision is limited function. There are many patients with failed shoulder replacements that are willing to tolerate some pain and shoulder dysfunction rather than undergoing revision surgery. It is important to discuss expected goals of revision surgery with patients and balance them with the potential risks when considering further surgery.
Physical Examination
Clinical examination should focus on assessment of the soft tissue envelope of the shoulder, range of motion and integrity of the rotator cuff and anterior deltoid. Visual inspection should assess for signs of infection, previous scars and wasting of the deltoid and rotator cuff. Range of motion should be assessed, passively and actively, and the cuff strength determined. Loss of active motion in the presence of preserved passive motion may indicate deltoid failure, axillary nerve palsy or severe cuff deficiency. The subscapularis should be tested using the lift-off or belly-press tests; rotator cuff integrity is crucial if revision to an unconstrained implant is being considered.
Imaging Studies
Radiographic evaluation should include a true anteroposterior (AP) view, scapular Y view and an axillary view. These should be critically assessed for implant positioning, wear and evidence of loosening. The AP view may show proximal migration of the proximal humerus indicative of superior cuff failure. The axillary view may reveal evidence of humeral head subluxation and allows an initial assessment of the glenoid version and bone stock. A computed tomography (CT) scan is necessary to more accurately assess glenoid and humeral version, loosening of components and glenoid bone stock. A CT arthrogram can provide more information regarding the integrity of the surrounding soft tissues. In addition, the use of 3D reformats has been shown to be superior in aiding surgical decision-making in comparison to 2D scans [5]. Imaging of the rotator cuff may be considered where there is uncertainty from the clinical examination. Sperling et al. [6, 7] assessed the role of specialised MRI (magnetic resonance imaging) in painful shoulder arthroplasties undergoing revision surgery. MRI correctly predicted the presence of a cuff tear in 10 of 11 shoulders and the absence of a tear in 8 of 10. MRI also correctly predicted glenoid cartilage wear in eight of nine shoulders. The authors suggest that MRI might be a useful technique to determine the integrity of the rotator cuff and residual cartilage in the painful shoulder arthroplasty. Ultrasound (US) offers a dynamic non-invasive method to assess the rotator cuff without distortion from the metal implants; a few reports have shown it to be particularly useful in evaluating the integrity of the subscapularis after TSA [8].
Additional Tests
The possibility of infection should be considered in every revision shoulder arthroplasty, even in the absence of clinical symptoms and signs of infection, because indolent infection is prevalent. There are additional tests that may yield useful information in the workup of a failed shoulder arthroplasty; in particular blood investigations including white blood cell count, C-reactive protein and erythrocyte sedimentation rate can provide an indicator of any infective process.
If there is any concern regarding an underlying infection, then samples should be acquired for microbiological culture either by sterile joint aspiration or arthroscopic biopsy, although false positive rates are high [9]. All microbiology specimens should be subjected to extended cultures and enrichment medium regimes as advised by a microbiologist to ensure the successful identification of any low-virulence organisms, such as Propionibacterium acnes.
Indications for Revision
There are a number of reasons why patients may require revision shoulder arthroplasty. In a review of 47 studies with non-constrained shoulder implants that were implanted for degenerative or inflammatory conditions and had at least 2 years follow-up, complications occurred in 906 out of 4,010 shoulders (22.6 %) [10]. Surgical revision was needed in 11.2 % of cases, with at least one of the implant components being changed in 7.9 % of cases. Most complications were on the glenoid side: either bone wear in cases of hemiarthroplasty (20.6 %) or loosening in cases of total arthroplasty (14.3 %). The cause of failure is important for treatment strategies but also in predicting prognosis following revision surgery. Dines et al. [11] reviewed 78 shoulders that underwent revision shoulder arthroplasty; they found that those undergoing revision for osseous or component-related problems achieved better results than those performed for soft tissue deficiency.
Suboptimal Prosthesis Positioning
Neer first recognised that poor component positioning was a cause for failure and suboptimal outcome following shoulder arthroplasty [12]. Humeral malpositioning and alterations of the centre of rotation of the glenohumeral joint have been found to be the most common surgical errors in one of the largest series of failed shoulder arthroplasties [13]. The single most common technical error in failed shoulder arthroplasty is overly superior placement of the humeral component in relation to the greater tuberosity [13]. Anatomic reconstruction of the proximal humerus with regard to the glenohumeral centre of rotation and the relationship of the articular surface to the rotator cuff insertion have been shown to improve range of motion and shoulder function and provide indirect evidence of decreased glenoid loading and wear [14, 15]. In particular glenohumeral offset and the positioning of the humeral articular surface just superior to the greater tuberosity appear to be key in maintaining optimal shoulder function [16, 17]. There is a strong association between component malposition and postoperative superior humeral migration (Fig. 10.1), glenoid loosening and excessive glenoid wear [18–20].
Glenoid Failure
The single largest point of long-term failure in shoulder arthroplasty is due to failure of the glenoid, either due to erosion in hemiarthroplasty (HA) (Fig. 10.2) or excessive wear or loosening of glenoid component [17–20]. The prevalence of glenoid erosion has been estimated to approach 100 % [21] with symptomatic glenoid erosion being most common after HA performed for arthritic conditions as opposed to arthroplasty for proximal humeral fracture [13]. Resurfacing of the glenoid has demonstrated improvements in patient-reported outcome measures [22, 23]; however there is no long-term comparative data on these groups of patients. Failure of the glenoid component following TSA is considered to be the most common reason for revision of shoulder arthroplasty [18–20, 24].
The diagnosis of a loose glenoid component relies on identifying progressive radiological lucency surrounding the glenoid component in the presence of pain. Lucent lines associated with the glenoid component following TSA are commonly reported, especially with the progression of time [25]. Torchia et al. [1] reported results at 5–17 years postoperatively and showed that early development of lucencies around the glenoid component on radiographs correlated to the development of subsequent symptomatic glenoid loosening. This particular series demonstrated that at 12 years following surgery, 84 % of patients had radiographic evidence of peri-glenoid lucencies in the implant bone interface [26]. Nagels et al. [27] defined radiological loosening as the observation of a progressive lucency around the glenoid component of 2 mm or more, spanning the whole cement-bone interface or an apparent shift in the position of the component. Deutsch et al. [28] attempted to further classify the presence of radiological loosening by setting out the following four features: circumferential radiolucent line of at least 2 mm around the glenoid component, progression of radiolucent lines on serial radiographs, presence of cement fragmentation and gross component migration.
It is important to note that lucent lines around a glenoid component on plain radiographs do not necessarily imply glenoid loosening [29]. The rate of clinical failure and revision TSA due to a loose glenoid is lower than the rate of postoperative radiographic lucent lines and no definite causal relationship has been established.
The aetiology of glenoid loosening is multifactorial, including aseptic osteolysis, rotator cuff insufficiency and the so-called rocking horse phenomenon and infection. It is postulated that eccentric loading of the glenoid by the humeral head subjects the glenoid component to torque, ultimately generating tensile stress at either the bone-implant or bone-cement-implant interface, with the end result of loosening. The degree of eccentric loading has been found to be maximal in a superior-inferior direction, which presumably explains the rates of glenoid loosening observed in patients with non-functional rotator cuffs [25]. It has also been shown that glenoid components implanted in a central position demonstrate superior resistance to mechanical failure in comparison to those glenoid components implanted superiorly or inferiorly inclined or retroverted positions [30].
Humeral Failure
Component loosening is much less common on the humeral side compared to that of the glenoid [31]. In a large study of 1,584 shoulder arthroplasties, the revision rate, for any cause, of the humeral component was 8 % at 10 years [31]. Humeral loosening may be due to aseptic osteolysis but must raise the suspicion of infection. Risk factors for humeral revision include younger age, male gender, replacement due to posttraumatic arthritis and the use of a metal-backed glenoid component [31].
Instability
Shoulder subluxation or dislocation is a well-recognised complication of anatomic TSA; nearly 30 % of all complications associated with anatomic TSA relate to glenohumeral instability [6]. The overall rate of instability after TSA is 4.9 % of which 20 % of cases are posterior. Sanchez-Sotelo et al. [32] reported on 33 shoulders with anterior (Fig. 10.3) or posterior instability (Fig. 10.4). Based upon radiographic, clinical, and intraoperative findings, the authors attributed instability to abnormal soft tissue tension in 21 shoulders, component malpositioning in 1 shoulder and a combination of factors in 11 cases. Excessive posterior capsular laxity was implicated in 10 of the 14 shoulders with posterior instability, 1 of which also had excessive anterior capsular tightness.
The most common cause for anterior instability is attributed to rupture of the subscapularis. However, posterior instability is most likely multifactorial in nature including excessive humeral retroversion, glenoid retroversion and failure to balance the soft tissues. Moeckel et al. [8] reported on three cases of posterior instability and found that retroversion of the glenoid and humeral component in combination with a tight subscapularis were causative factors.
Rotator Cuff
In the context of unconstrained shoulder arthroplasty, rotator cuff deficiency can occur intraoperatively or postoperatively. Risk factors for intraoperative injury include excessive retroversion of the humeral saw cut, which may damage the supraspinatus and infraspinatus [30] and excessive humeral head resection. Chronic failure of the rotator cuff after HA or TSA manifests as pain, lack of function and superior migration of the humeral head. This radiographic finding has been reported in up to 46 % of TSA procedures [5]. Whilst the true incidence of revision for rotator cuff failure is not well documented, there are an increasing number of reports of revision to RSA for this problem [33].
Infection
Infection is a rare (1 %) but devastating complication following shoulder arthroplasty [18]. Risk factors for infection include diabetes, infection at a distant site, revision surgery, previous local radiotherapy, inflammatory arthropathies, immunosuppression, advanced age and malnutrition [18, 34]. Infection must be a consideration in the evaluation of any patient with postoperative shoulder pain, especially in the context of radiographic evidence of loosening [34]. A detailed discussion related to the infected shoulder arthroplasty is covered in a separate chapter.
Surgical Techniques and Considerations
Prior to commencing surgery, previous operative reports should be accessed to confirm the index surgical approach, operative findings and type of implant that was used. The surgeon should be familiar with the implant that is being revised and have available any necessary instruments to assist removal.
Surgical Exposure
The patient is set up in the beach-chair position following general anaesthesia and an inter-scalene nerve block. Perform an examination under anaesthesia to determine degree of flexion, abduction, and external and internal rotation. Restriction in motion can direct the surgeon to the releases required.
Previous incisions are incorporated if possible although there should be a low threshold for a new incision in the optimal position away from the axilla to minimise contamination. The deltopectoral approach is generally recommended for use during revision cases, given it is extensile, to provide access to almost the entire humeral shaft distally. This is particularly relevant in cases where removal of a well-fixed humeral component is necessary. An anteromedial approach to the shoulder with detachment of the anterior deltoid from its clavicular and anterior acromial origins has been described as a method of enhancing exposure for difficult cases [35]. The surgeon should be aware that the cephalic vein can often no longer be relied upon as a landmark in revision surgery and that the delta-pectoral interval may be difficult to find due to scarring. It is best to start the dissection proximally adjacent to the most medial aspect of the deltoid origin from the clavicle. The superior 1–2 cm of pectoralis major insertion should be released to facilitate exposure.
There will frequently be dense adhesions on the deep surface of deltoid and lateral border of the conjoint tendon. Both surgical planes will need to be carefully developed, affording significant care for the axillary and musculocutaneous nerves. First release the adhesions on the lateral aspect of the conjoint tendon by starting on the lateral aspect of the coracoid and working distally, and subsequently develop the planes on the anterior and superior aspects of subscapularis. Develop the subcoracoid space, and retract the conjoint tendon medially taking care not to injure the musculocutaneous nerve [36] and brachial plexus [37].
Next release the subacromial and subdeltoid spaces with a combination of sharp and blunt dissection. Flexion and internal rotation of the arm further exposes this tissue plane and allows proximal dissection up into the subacromial space. After the rotator cuff is identified, scar tissue is excised. To complete and confirm the subdeltoid release, use an index finger to sweep superiorly, posteriorly, laterally and finally anteriorly. At this point the deltoid should be fully separated and mobile from the rotator cuff and the underlying proximal humerus down to the level of the deltoid insertion; this will allow easy insertion of retractors to expose the subscapularis and rotator interval.
Protection of the axillary nerve is necessary throughout the procedure; it is found at the inferior border of the subscapularis in the subcoracoid space although identification may be difficult in cases of severe scarring. The “tug test” [38] can be useful to facilitate identification of the axillary nerve; this is performed by placing a finger from one hand on the nerve as it passes inferior to subscapularis and a finger from the other hand under the deltoid on the anterior branch of the nerve. The application of gentle pressure from one end will allow the transmission to be felt in the other end confirming the location of the nerve as well as demonstrating undersurface release of the deltoid. The long head of biceps should be examined and if diseased or scarred within the joint, then a tenotomy or tenodesis are performed.
After complete extra-articular mobilisation, the rotator interval is identified and opened. The coracoacromial ligament overhangs the rotator interval and therefore excision may improve exposure. The method of subscapularis release is determined by the degree of limitation of external rotation and the quality and thickness of the tendon. Typically, each centimetre increase of subscapularis length increases external rotation by approximately 20° [39]. The surgical options include a standard subscapularis tenotomy with capsular releases (for ER greater than 40°), subscapularis release directly from its bony insertion with subsequent medial reattachment (for ER between 20 and 40°) and a Z-lengthening of the tendon (for ER less than 20°).
The simplest and most familiar technique is a subscapularis tenotomy with circumferential release to increase tendon excursion and lateral advancement. A vertical incision is made by the use of a scalpel or electrocautery through the tendinous portion of the subscapularis 1 cm medial to its insertion on the lesser tuberosity to allow for direct tissue repair. Attention is paid to ligate or cauterise the anterior humeral circumflex artery as it crosses the inferior aspect of the tendon, and the arm should be placed in external rotation and adduction to further protect the axillary nerve. Simple traction sutures are then placed in the edge of the subscapularis tendon along the line of the tenotomy to facilitate mobilisation. Once the subscapularis has been divided, a circumferential release can be performed to maximise the muscle-tendon unit excursion. This release involves freeing its superior margin from the coracoid (coracohumeral ligament), the posterior surface from the anterior capsule and scapular neck, the inferior border from the axillary nerve and circumflex vessels and the anterior surface from the conjoined tendon [40].
The second option for the subscapularis is to dissect the tendon directly from its insertion on the lesser tuberosity with a more medial reattachment to effectively lengthen the muscle-tendon unit (subscapularis “peel”) The subscapularis and capsule are dissected off the humerus as a single unit after which a circumferential release is performed as described above. Once the intra-articular release is completed, the subscapularis tendon is reattached to the humerus via trans-osseous sutures or anchors.
Third, for tendons of sufficient quality and thickness, a subscapularis Z-plasty to lengthen the subscapularis is an option, although this is contraindicated if the tendon is thin and atrophic. Subscapularis Z-plasty was originally described for internal rotation contractures after surgery for recurrent anterior instability [41, 42]. A modification of this technique was described by Green and Norris [43] in the setting of shoulder arthroplasty for glenohumeral arthritis after anterior instability repair. Essentially the technique involves carefully dividing the anterior half of the subscapularis tendon at the margin of the lesser tuberosity, leaving the posterior half of the tendon attached. The anterior half of the tendon is then dissected medially to the level of the anterior glenoid, and the anterior capsule is divided at this level to create two tissue flaps. The lateral aspect of the anterior flap is sutured to the medial edge of the posterior flap to effectively lengthen the subscapularis. Nicholson et al. [44] have described a coronal Z-lengthening for internal rotation contractures in the setting of shoulder arthroplasty using the plane between the subscapularis and capsule which are then sutured to each other, creating an overlapping slide instead of an end to end repair. It is important to be aware that there are significant concerns regarding subscapularis Z-plasty, namely, that the repair is weak and that failure will lead to shoulder instability and that internal rotation strength is diminished. As a result of these issues, many authors have moved away from performing subscapularis Z-plasty.
The proximal humerus can now be dislocated anteriorly giving access to the humeral head; when doing so, care should be taken as to not use excessive external rotation force that can lead to an iatrogenic fracture or rotator cuff tear.
Humeral Component Revision
In most revision cases, the humeral component will need to be removed. Furthermore, in the majority of cases, the humeral stem is well fixed either with cement or bone on-growth. For this reason removal can be a challenging procedure that requires experience and appropriate instrumentation to minimise the risk of fracture and humeral bone defects. Occasionally the humeral stem can be retained if the implant is modular and only the glenoid requires revision. The most common reason is when revising a HA to a TSA or a TSA with a loose glenoid. There are also modern platform systems now available that allow conversion of an anatomic shoulder to a reverse without exchange of the humeral component.
In the first instance, scar tissue surrounding the neck of the prosthesis is removed. If the implant is modular, then the head is removed using a tuning fork. The proximal bone-implant or cement-implant interface is disrupted with the use of fine high-speed burrs and narrow osteotomes to facilitate implant removal (Fig. 10.5). Some implants have a connector for the stem with a slap-hammer adapter that will facilitate stem removal. If this is not the case, then a square-tipped impactor placed under the infero-medial aspect of the neck is struck with a mallet to try to extract the implant (Fig. 10.6). In the situation where this does not work, and the humeral component remains well fixed further distally, then an anterior longitudinal humeral osteotomy can be used to gain access to the remaining humeral implant in a safe and controlled manner [13]. Sperling and Cofield have also described the application of a number of different humeral cortical “windows” to facilitate the removal of a well-fixed humeral stem [31]. They describe anterior humeral windows (Fig. 10.7) and advocate the use of a proximal medial humeral window (Fig. 10.8) when revising a humeral component with only proximal coating and a smooth distal stem. In contrast for fully textured components, or those with a well-fixed cement mantle, they recommend an anterior cortical window, which can be subsequently bypassed by a longer humeral revision stem. Good rates of union were achieved through either suture or wire cerclage fixation of the windows and a stable construct achieved using a cemented revision stem [31]. Pre-drilling in the line of the proposed osteotomy is a useful technique to avoid unwanted distal fracture propagation, and cerclage wires can be positioned prior to revision stem insertion for osteotomy fixation. The use of distal humeral windows has also been described for gaining access to the stem tip and distal cement mantle [12]. Ultrasonic devices may aid cement removal, but we would advocate caution to the potential risk of thermal injury to the radial nerve. Efforts to remove all cement in its entirety are only necessary in the case of revision for infection; in the absence of infection, a cement-in-cement revision can be performed.
Anterior humeral window [31]
Medial humeral window [31]
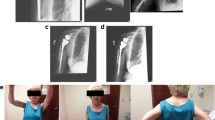
Larger proximal bony deficiencies pose an additional challenge to the revision surgeon. Reconstructive options include the use of an allograft-prosthetic composite, a modular revision component system or custom tumour-type prostheses. Chacon et al. [45] reported high rates of bone incorporation with the use of APC combined with a reverse implant. The use of newer modular proximal humeral prostheses is an attractive option as it allows the resection level to be determined at the time of surgery and intraoperative flexibility via extensive component modularity (Fig. 10.1).
Glenoid Component Revision
Addressing the glenoid component is also very challenging during revision shoulder arthroplasty. The mode of failure and glenoid bone stock should be assessed prior to surgery. Large glenoid bony deficiencies frequently compromise implant fixation in a revision setting and sometimes may preclude glenoid component placement altogether [29]. In the case of an isolated loose glenoid component in a patient who is too frail to undergo major revision surgery, arthroscopic extraction of the loose component has been described with good postoperative results in a small series of patients [46].
After the humeral side has been addressed, the glenoid is exposed for revision. In the case of a failed HA with minimal bone loss, the glenoid can be replaced in the standard fashion. For an all polyethylene glenoid that is well fixed, the component can be cut into equal segments with a sagittal saw (Fig. 10.9). This allows piecemeal removal (Fig. 10.10) whilst minimising damage to the underlying glenoid bone stock. The central peg or keel can then be extracted using a rongeur, and the remaining cement mantle can be removed using osteotomes or a high-speed burr. Removal of metal-backed components can be associated with increased glenoid bone loss, so this should be done cautiously in a manner that preserves as much glenoid bone as possible. After removal of the glenoid, gentle reaming of the glenoid surface is performed to remove any fibrous tissue and to expose healthy subchondral bone.
The glenoid should now be carefully inspected to assess the location and extent of bone loss and the feasibility of reimplantation. Defects have been classified as central, peripheral and combined, which in turn can be mild, moderate or severe (Fig. 10.11). Deficiencies are classified as mild if they involve less than a third of the glenoid rim or surface, moderate if they involve between one- and two-thirds and severe if they involve greater than two-thirds. Mild and moderate deficiencies may be suitable for single-stage reimplantation with or without bone grafting whilst severe defects may preclude reimplantation. Superior outcomes have been observed when bone grafting and glenoid implantation are compared to cases where bone grafting alone is performed [47]. Cheung et al. [48] performed revision in 68 shoulders for glenoid loosening. In 33 patients, new glenoid implantation was possible at the time of the revision procedure, and the remaining patients were revised to HA with glenoid bone grafting. Benefits of glenoid reimplantation were increased in forward elevation and greater patient satisfaction. The rate of revision-free survival at 5 years was not significantly different between the two groups. Overall, the results suggested that a new glenoid component should be implanted if structurally feasible.
Classification of glenoid bone defects [47]
Severe central or combined deficiencies may preclude a new component being implanted. In this situation, bone grafting using either cancellous or corticocancellous bone should be performed to restore glenoid bone stock and facilitate potential future glenoid revision. Selective second-stage glenoid component implantation is considered only in those patients who continue to report pain once the first-stage graft has fully consolidated [21, 47] Phipatanakul and Norris [21] reported on 24 patients undergoing revision TSA with removal of the glenoid component and bone grafting. Eighteen patients had adequate pain relief after the initial procedure, and four patients achieved good pain relief after a second-stage glenoid implantation for persistent pain. Graft subsidence was reported in 10 out of 20 cases (50 %) although it did not preclude placement of a new glenoid component during the second-stage revision. Overall, the investigators found bone grafting of the glenoid beneficial in terms of pain relief as well as enabling delayed glenoid implantation. However, range of motion did not improve significantly and graft subsidence rate was concerning.
The two available techniques for bone grafting of a glenoid defect are corticocancellous impaction grafting or the use of a structural cortical bone graft. The type of defect, and whether it is contained or un-contained, will determine the appropriateness of the use of these available techniques. Central contained glenoid defects are typically managed with cancellous bone graft, whilst peripheral and combined defects are addressed with a combination of cancellous and structural bone graft. In cases with an isolated central glenoid deficiency, Neyton et al. [49] have described a technique using a central bicortical graft with the cortical aspect of the graft positioned laterally, with further cancellous graft packed peripherally and medially behind the cortical graft. In cases with a peripheral deficiency, the same group describes the use of a bicortical graft secured with two cortical screws and then further cancellous graft being packed into the now “contained” residual defect. The biggest problem with impaction grafting alone is the risk of subsidence. Cancellous allograft either in morcellized or structural form has been associated with resorption and medialization of the humeral head [50]. When using structural grafts that are fixed with screws, placement should be planned to avoid interference with the glenoid component fixation. Although initial results were encouraging with the use of bulk allografts, longer-term follow-up has revealed evidence of graft resorption on radiographs [34].
Management of Instability
Anterior instability most commonly arises from failure of subscapularis, which is the main restraint to anterior glenohumeral translation. Mobilisation and repair of a ruptured subscapularis following shoulder arthroplasty patient is entirely dependent on the chronicity of the tendon failure. Early intervention implies easier mobilisation of the torn tendon from the anterior glenoid neck and possible direct repair. However, the subscapularis typically retracts quickly after rupture making adequate mobilisation and repair impossible. Pectoralis major transfer has been described to augment deficient anterior structures although results in the setting of TSA are associated with high failure rates [51]. More recently more predictable results have been achieved with conversion to reverse shoulder arthroplasty [52].
Surgical management of posterior instability after shoulder arthroplasty has traditionally involved improving component position and soft tissue balance including release of tight anterior structures and plication of the lax posterior capsule [53, 54]. When considering shoulder arthroplasty revision for posterior instability, the surgeon should have a thorough understanding of the factors that predispose to the problem to optimise the chance of a successful outcome. Few studies have reported on the results after revision for posterior instability after shoulder arthroplasty. Furthermore, due to the limited number of patients, these reports have combined anterior and posterior instability cases making the results more difficult to evaluate. Moeckel et al.[8] reported on 7 cases of anterior instability and 3 cases of posterior instability in a series of 236 total shoulder arthroplasties. Revision surgery restored stability in all seven of the anteriorly unstable shoulders, whereas of the three with posterior instability, only two were stable at follow-up. The final patient failed two revisions and eventually underwent component removal. In a multicentre study performed by Ahrens et al. [55] consisting of 29 patients with posterior instability, revision surgery was successful in only 53 % of cases. In the Mayo Clinic [32] series of revision procedures for instability, 8 of the 14 shoulders with posterior instability underwent posterior capsule plication. However, 7 of the 14 patients required additional revision surgery in an attempt to restore stability. The authors concluded that surgical treatment of instability after shoulder arthroplasty is associated with a moderately high failure rate. The results of these studies suggest that the surgical treatment of posterior instability after shoulder arthroplasty with unconstrained anatomic components is associated with a significant failure rate, particularly when soft tissue procedures alone are performed. On this basis, RSA has emerged as an attractive revision alternative.
Abdel et al. [52] published results on 33 unstable anatomic shoulder arthroplasties that were revised to a reverse design of which two patients had posterior instability. Outcomes evaluated included visual analogue scores (VAS) for pain, range of motion, shoulder stability and Neer rating. The mean age of the patients at the time of revision surgery was 71 years. They were followed for a mean of 42 months (range, 25–71 months) or until revision surgery (one patient) or death (two patients). The average time from the index arthroplasty to revision was 26 months. Pain scores improved significantly as did mean active forward elevation from 40 to 97°, whereas there was no difference in internal or external rotation. At last follow-up 31 shoulders (94 %) were stable, the remaining two patients experienced dislocations, one at 2.5 weeks postoperatively and the other at 3 months postoperatively. According to the Neer rating system, there were 13 excellent, 10 satisfactory and 10 unsatisfactory results. The authors concluded that revision to a reverse prosthesis reliably restores shoulder stability with improved pain and active elevation although the overall results are inferior to the outcome with RSA in cuff-tear arthropathy. Whilst there is currently no literature available directly comparing the results of revision for instability using anatomic versus reverse techniques, these studies suggest that revision to RSA more predictably restores shoulder stability with better clinical outcomes compared to revision using anatomic components. It should be remembered that this is a complex patient group and that complication and revision rates remain high.
Revision to Reverse Shoulder Arthroplasty
Rotator cuff dysfunction (involving either the anterior or superior cuff) is a common cause of failed anatomic shoulder arthroplasty. This is associated with significant pain and loss of function. Revision surgeries using anatomic prosthesis designs are often disappointing. For this reason reverse shoulder arthroplasty (RSA) has emerged as an attractive revision alternative in dealing with a failed HA or TSA with cuff deficiency with or without bone loss [56]. RSA provides increased stability due to greater constraint and conformity enhanced by the increased tension within the deltoid muscle, which generates greater compressive forces across the glenohumeral joint.
Once the glenoid component has been removed, the glenoid should be carefully inspected to assess the location and extent of bone loss. Glenoid bone defects must be addressed to obtain secure fixation of the reverse baseplate, and larger defects may require structural bone grafts or may even preclude implantation of a component. The guide pin is positioned in the appropriate location, and reaming is kept to a minimum to maintain subchondral bone and allow seating of the baseplate. The baseplate is now secured in place in a standard fashion with a combination of central and peripheral screws. The glenosphere is inserted using the largest available diameter to enhance stability and lessen the chance of dislocation. The humerus is brought into the wound, taking care not to get caught on the glenosphere in doing so, a trial liner is inserted on the trial humeral component and the shoulder reduced and the stability and tension assessed. The trials are now removed and the definitive implants inserted.
Walker et al. [57] performed a retrospective case series of 24 patients with failed TSA who were treated with conversion to RSA. Indications for conversion to RSA included failure of TSA from glenohumeral instability in 19, mechanical failure of the humeral or glenoid component in 10 and infection in 2. American Shoulder and Elbow Surgeons score improved from 38.5 preoperatively to 67.5. Fourteen patients rated their outcome as excellent, 3 as good, 3 as satisfactory and 2 as unsatisfactory. The overall complication rate was 22.7 %. The authors concluded that RSA is an effective treatment for failed TSA by decreasing pain and improving shoulder function although RSA in the revision setting is associated with a higher complication rate.
Patel et al. [15] considered the outcomes of 31 patients with a failed anatomic arthroplasty that were revised to a RSA; their results showed statistically significant improvement in all outcome measures. Improved function and pain relief were reliably achieved with 82.2 % or patients reporting a satisfactory, good or excellent outcome; the greatest improvement was noted in revision of failed TSA [15]. The authors concluded that RSA is a reliable salvage option for a challenging clinical problem. Kelly et al. [16] also found a significant improvement in function and pain when using RSA as a revision tool, although a complication rate of 50 % was observed in those requiring concomitant tri-cortical glenoid bone grafting; 80 % of these patients remained either satisfied or very satisfied with their outcome.
Melis et al. [58] specifically considered the outcome of RSA used to address aseptic glenoid loosening in 37 patients, 78 % requiring an associated structural bone graft in combination with glenosphere insertion. In three cases early glenoid component loosening was observed due to the use of baseplate with an insufficiently long central peg to provide adequate primary fixation to native glenoid bone. Two of these cases required revision to a “long-pegged” baseplate, going on to demonstrate successful radiological graft incorporation, and one was converted to a HA. Given the encouraging rates of graft incorporation that have been seen with RSA prostheses, some surgeons prefer to use RSA and bone grafting as a revision tool to address a glenoid bony deficiency even in the setting of an intact rotator cuff.
Conclusion
Revision shoulder arthroplasty is challenging for the patient and surgeon. Successful management of the failed shoulder arthroplasty starts with a thorough assessment of the patient, adequate imaging studies and exclusion of infection. The mode of failure must be clearly identified to direct the subsequent treatment strategy. Patients should be counselled carefully with regard to expected outcomes and potential complications. The surgeon should be clearly aware of the technical challenges presented by the exposure, removal of humeral and glenoid components and reimplantation. Soft tissue and bone deficiencies may preclude revision to a further anatomic implant, which has led to the expanding role of RSA in the revision setting.
References
Torchia ME, Cofield RH, Settergren CR. Total shoulder arthroplasty with the Neer prosthesis: long-term results. J Should Elb Surg. 1997;6:495–505.
Havelin L. The norwegian joint registry. Bulletin hospital of joint diseases (NY). 1999;58:139–47.
Chen A, Bain E, Horan M, Hawkins R. Determinants of patient satisfaction with outcome after shoulder arthroplasty. J Should Elb Surg. 2007;16:25–30.
Neer C, Kirby R. Revision of humeral head and total shoulder arthroplasties. Clin Orthop Relat Res. 1982;170:189–95.
Scalise JJ, Codsi M, Bryan J, Iannotti JP. The three-dimensional glenoid vault model can estimate normal glenoid version in osteoarthritis. J Should Elb Surg. 2008;17:487–91.
Chin PY, Sperling JW, Cofield RH, Schleck C. Complications of total shoulder arthroplasty: are they fewer or different? J Shoulder Elbow Surg. 2006;15(1):19–22.
Sperling JW, Potter HG, Craig EV, Flatow E, Warren RF. Magnetic resonance imaging of painful shoulder arthroplasty. J Shoulder Elbow Surg. 2002;11(4):315–21.
Moeckel BH, Altchek DW, Warren RF, Wickiewicz TL, Dines DM. Instability of the shoulder after arthroplasty. J Bone Joint Surg Am. 1993;75(4):492–7.
Updegrove GF, Armstrong AD, Kim HM. Preoperative and intraoperative infection workup in apparently aseptic revision shoulder arthroplasty. J Shoulder Elbow Surg. 2015;24(3):491–500.
Boileau P, Pennington SD, Alami G. Proximal humeral fractures in younger patients: fixation techniques and arthroplasty. J Shoulder Elbow Surg. 2011;20(2 Suppl):S47–60.
Dines JS, Fealy S, Strauss EJ, Allen A, Craig EV, Warren RF, et al. Outcomes analysis of revision total shoulder replacement. J Bone Joint Surg Am. 2006;88(7):1494–500.
Plausinis D, Kwon Y, Zuckerman J. Complications of humeral head replacement for proximal humeral fractures. Instr Course Lect. 2005;54:371–80.
Neer C. Replacement arthroplasty for gleno-humeral osteoarthritis. J Bone Joint Surg (Am). 1974;56:1–13.
Stechel A, Fuhrmann U, Irlenbusch L, Rott O, Irlenbusch U. Reversed shoulder arthroplasty in cuff tear arthritis, fracture sequelae and revision arthroplasty. Acta Orthop. 2010;81(3):367–72.
Patel D, Young B, Onyekwelu I, Zuckerman J, Kwon Y. Reverse total shoulder arthroplasty for failed shoulder arthroplasty. J Should Elb Surg. 2012;21:1478–83.
Kelly 2nd JD, Zhao J, Hobgood ER, Norris TR. Clinical results of revision shoulder arthroplasty using the reverse prosthesis. J Should Elbow Surg. 2012;21:1516–25.
Wirth M, Jr CR. Complications of shoulder arthroplasty. Clin Orthop Relat Res. 1994;307:47–69.
Jerosch J, Schneppenheim M. Management of infected shoulder replacement. Arch Orthop Trauma Surg. 2003;123:209–14.
Klatte TO, Junghans K, Al-Khateeb H, Rueger JM, Gehrke T, Kendoff D, et al. Single-stage revision for peri-prosthetic shoulder infection: outcomes and results. Bone Joint J. 2013;95-B:391–5.
Cabo J, Euba G, Saborido A, González-Panisello M, Domínguez MA, Agulló JL, et al. Clinical outcome and microbiological findings using antibiotic-loaded spacers in two-stage revision of prosthetic joint infections. J Infect. 2011;63:23–31.
Phipatanakul W, Norris T. Treatment of glenoid loosening and bone loss due to osteolysis with glenoid bone grafting. J Should Elb Surg. 2006;15:84.
Muh SJ, Streit J, Lenarz CJ, McCrum C, Warner JP, Shishani Y, et al. Resection arthroplasty for failed shoulder arthroplasty. J Should Elb Surg. 2013;22:247–52.
Phipatanakul WP, Bowen J, Jobe C. Removal of well fixed flanged humeral prostheses may require humeral expansion. J Should Elb Surg. 2009;18:724–7.
Cil A, Veillette C, Sanchez-Sotelo J, Sperling JW, Schleck CD, Cofield RH. Survivorship of the humeral component in shoulder arthroplasty. J Should Elb Surg. 2010;19:143–50.
Strauss E, Roche C, Flurin P-H, Wright T, Zuckman J. The glenoid in shoulder arthroplasty. J Should Elb Surg. 2009;18:819–33.
Owens CJ, Sperling J, Cofield R. Utility & complications of long-stem humeral components in revision shoulder arthroplasty. J Should Elb Surg. 2013;22:e7–12.
Nagels J, Valstar E, Stokdijk M, Rozing PM. Patterns of loosening of the glenoid component. J Bone Joint Surg (Br). 2002;84:83–7.
Deutsch A, Abboud J, Kelly J, Mody M, Norris T, Ramsey ML. Clinical results of revision shoulder arthroplasty for glenoid component loosening. J Should Elb Surg. 2007;16:706–16.
Namdari S, Goel D, Romanowski J, Glaser D, Warner JJP. Principles of glenoid component design and strategies for managing glenoid bone loss in revision shoulder arthroplasty in the absence of infection and rotator cuff tear. J Should Elb Surg. 2011;20:1016–24.
Hopkins A, Hansen U, Amis A, Emery R. The effects of glenoid component alignment variations on cement mantle stresses in total shoulder arthroplasty. J Should Elb Surg. 2004;13:668–75.
Sperling JW, Cofield RH. Humeral windows in revision shoulder arthroplasty. J Should Elb Surg. 2005;14(3):258–63.
Sanchez-Sotelo J, Sperling JW, Rowland CM, Cofield RH. Instability after shoulder arthroplasty: results of surgical treatment. J Bone Joint Surg Am. 2003;85-A(4):622–31.
Sperling J, Cofield R, Rowland C. Neer hemi-arthroplasty and Neer total shoulder arthroplasty in patients fifty years old or less. Long-term results. J Bone Joint Surg (Am). 1998;80:464–73.
RA FML, editor. Glenoid component failure treated with a bulk allograft for revision total surgery. Presented at American Shoulder & Elbow Surgeons 18th Annual Meeting, 24th–27th Oct 2001; Napa.
Foruria AM, Oh LS, Sperling JW, Cofield RH. Anteromedial approach for shoulder arthroplasty: current indications, complications, and results. J Shoulder Elbow Surg. 2010;19(5):734–8.
Flatow EL, Bigliani LU, April EW. An anatomic study of the musculocutaneous nerve and its relationship to the coracoid process. Clin Orthop Relat Res. 1989;244:166–71.
McFarland EG, Caicedo JC, Guitterez MI, Sherbondy PS, Kim TK. The anatomic relationship of the brachial plexus and axillary artery to the glenoid. Implications for anterior shoulder surgery. Am J Sports Med. 2001;29(6):729–33.
Flatow EL, Bigliani LU. Tips of the trade. Locating and protecting the axillary nerve in shoulder surgery: the tug test. Orthop Rev. 1992;21(4):503–5.
Cuomo F, Checroun A. Avoiding pitfalls and complications in total shoulder arthroplasty. Orthop Clin North Am. 1998;29(3):507–18.
Yung SW, Lazarus MD, Harryman 2nd DT. Practical guidelines to safe surgery about the subscapularis. J Should Elb Surg/Am Should Elb Surg [et al]. 1996;5(6):467–70.
Hawkins RJ, Angelo RL. Glenohumeral osteoarthrosis. A late complication of the Putti-Platt repair. J Bone Joint Surg Am. 1990;72(8):1193–7.
MacDonald PB, Hawkins RJ, Fowler PJ, Miniaci A. Release of the subscapularis for internal rotation contracture and pain after anterior repair for recurrent anterior dislocation of the shoulder. J Bone Joint Surg Am. 1992;74(5):734–7.
Green A, Norris TR. Shoulder arthroplasty for advanced glenohumeral arthritis after anterior instability repair. J Shoulder Elbow Surg. 2001;10(6):539–45.
Nicholson GP, Twigg S, Blatz B, Sturonas-Brown B, Wilson J. Subscapularis lengthening in shoulder arthroplasty. J Should Elb Surg/Am Should Elb Surg [et al]. 2010;19(3):427–33.
Chacon A, Virani N, Shannon R, Levy JC, Pupello D, Frankle M. Revision arthroplasty with use of a reverse shoulder prosthesis-allograft composite. J Bone Joint Surg Am. 2009;91(1):119–27.
O’Driscoll SW, Petrie RS, Torchia ME. Arthroscopic removal of the glenoid component for failed total shoulder arthroplasty. A report of five cases. J Bone Joint Surg Am. 2005;87(4):858–63.
Antuna S, Sperling J, Cofield R, Rowland C. Glenoid revision surgery after total shoulder arthroplasty. J Should Elb Surg. 2001;10(3):217–24.
Cheung EV, Sperling JW, Cofield RH. Revision shoulder arthroplasty for glenoid component loosening. J Shoulder Elbow Surg. 2008;17(3):371–5.
Neyton L, Walch G, Nove-Josserand L, Edwards TB. Glenoid cortico-cancellous bone grafting after glenoid component removal in the treatment of glenoid loosening. J Should Elb Surg. 2007;15:173–9.
Neyton L, Favard L, Mole D, Walch G. Aseptic glenoid loosening or failure in total shoulder arthroplasty: revision with glenoid reimplantation. J Should Elb Surg. 2012;3:342–349.
Elhassan B, Ozbaydar M, Massimini D, Diller D, Higgins L, Warner JJ. Transfer of pectoralis major for the treatment of irreparable tears of subscapularis: does it work? J Bone Joint Surg. 2008;90(8):1059–65.
Abdel MP, Hattrup SJ, Sperling JW, Cofield RH, Kreofsky CR, Sanchez-Sotelo J. Revision of an unstable hemiarthroplasty or anatomical total shoulder replacement using a reverse design prosthesis. Bone Joint J. 2013;95-B(5):668–72.
Wirth MA, Rockwood Jr CA. Complications of total shoulder-replacement arthroplasty. J Bone Joint Surg Am. 1996;78(4):603–16.
Namba RS, Thornhill TS. Posterior capsulorrhaphy in total shoulder arthroplasty. A case report. Clin Orthop Relat Res. 1995;313:135–9.
Ahrens P, Boileau P, Walch G. Posterior instability after unconstrained shoulder arthroplasty in: 2000 shoulder prostheses…two to ten year follow up. Montpellier: Sauramps Medical; 2001.
Flury MP, Frey P, Goldhahn J, Schwyzer HK, Simmen BR. Reverse shoulder arthroplasty as a salvage procedure for failed conventional shoulder replacement due to cuff failure – midterm results. Int Orthop. 2011;35(1):53–60.
Walker M, Willis MP, Brooks JP, Pupello D, Mulieri PJ, Frankle MA. The use of the reverse shoulder arthroplasty for treatment of failed total shoulder arthroplasty. J Shoulder Elbow Surg. 2012;21(4):514–22.
Melis B, Bonnevialle N, Neyton L, Levigne C, Favard L, Walcg G, Boileau P. Glenoid loosening and failure in anatomical total shoulder arthroplasty: is revision with a reverse shoulder arthroplasty a reliable option? J Should Elb Surg. 2012;21(3):342–9.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Lawrence, T., Pennington, N., Sperling, J. (2016). Revision Total Shoulder Arthroplasty. In: Armstrong, A., Murthi, A. (eds) Anatomic Shoulder Arthroplasty. Springer, Cham. https://doi.org/10.1007/978-3-319-29164-2_10
Download citation
DOI: https://doi.org/10.1007/978-3-319-29164-2_10
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-29162-8
Online ISBN: 978-3-319-29164-2
eBook Packages: MedicineMedicine (R0)