Abstract
Establishing an accurate medical cause of death is a policy requirement in the United Kingdom. It is also important for social and ethical reasons and for health care practice and planning. This leads to England and Wales having one of the highest autopsy rates in the world [1]. These autopsies are often performed for sudden and unexpected but natural deaths and therefore have a very different demographic from the cases undergoing investigation after traumatic or potentially homicidal deaths.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Postmortem computed tomography angiography (PMCTA)
- Targeted PMCTA
- Postmortem coronary angiography
- Coronary artery disease
- Cause of death
- PMCT methods
1 Introduction
Establishing an accurate medical cause of death is a policy requirement in the United Kingdom. It is also important for social and ethical reasons and for health care practice and planning. This leads to England and Wales having one of the highest autopsy rates in the world [1]. These autopsies are often performed for sudden and unexpected but natural deaths and therefore have a very different demographic from the cases undergoing investigation after traumatic or potentially homicidal deaths.
In light of growing religious, cultural, and humanitarian concerns regarding invasive postmortem examinations, an alternative means of determining the cause of death is desirable [2]. Postmortem computed tomography (PMCT) is becoming a standard investigation for the investigation of death, both as an adjunct and as a possible replacement for autopsy [3–5]. However, the use of non–contrast enhanced PMCT is limited, particularly for disease or trauma affecting blood vessels [6–8], although in many cases of unexplained sudden natural death a cardiac cause of death may still be predicted [9, 10]. This problem has been overcome to a large extent by the development of PMCT angiography (PMCTA), the subject of this atlas. We have developed an alternative to the different techniques of whole-body PMCTA such as multiphase postmortem computed tomography angiography (MPMCTA) consisting of a targeted coronary angiography system, using a catheter passed from the carotid artery into the ascending aorta [11, 12]. Injecting contrast media to study the coronary arteries has shown correlation with coronary artery disease identified at autopsy [12–14]. One situation this technique has been developed for is to select cases of sudden and unexpected natural death when autopsy is not required, in order to issue a medical cause of death (based on “the balance of probabilities,” the evidence required by Her Majesty’s Coroner [15]). These cases have a high incidence of death caused by coronary vascular disease, making a targeted coronary angiography technique faster and cheaper than whole body techniques. This method is therefore suitable for the large number of cases that could potentially go through this process.
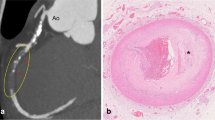
Our experience has shown that luminal examination of the coronary arteries with PMCTA can be equivalent to traditional autopsy; however, it highlights the inability of PMCTA to provide diagnostic intraplaque pathology such as plaque hemorrhage. However, autopsy can fail to identify some pathology detectable by PMCTA. One specific finding in our comparison of targeted coronary PMCTA with autopsy relates to cases in which PMCTA showed luminal patency at sites where autopsy and histologic examination reported severe stenosis in regions of calcification [13]. This is likely to be because the vessels were examined under pressure using the technique of PMCTA, thereby more closely mimicking clinical conditions [16]. The benefits of examining vessels under pressure at autopsy are well recognized but rarely performed in standard pathologic practice [17].
2 Method for Targeted Coronary PMCTA
2.1 Inserting the Angiography Catheter
The method for raising the carotid artery was adapted from a standard embalming technique and uses standard mortuary equipment to access the left carotid artery and insert a balloon catheter [11] (Fig. 8.1).
For cannulation we raise the body on a mortuary block placed under the middle of the shoulders, with the head turned facing right. This assists in the dissection of the neck, exposure of the left carotid artery, and insertion of the catheter. The incision should be just above the medial left clavicle head. Care should be taken during the dissection to avoid engorged veins, especially in the area of the clavicle, because blood loss may make arterial cannulation difficult. Enlarged lymph nodes may be identified at this point, alerting the operator to the possibility of tuberculosis.
The mortuary block is then removed prior to catheter insertion; otherwise the catheter may proceed down the descending aorta. The aim is to place the catheter tip into the ascending aorta just above the aortic valve and adjacent to the coronary ostia. During insertion the operator aims the tip of the catheter toward the right axilla. It is possible to insert the catheter in the mortuary by “feel” (haptic feedback). Any obstruction to catheter advancement between 5 and 10 cm is likely because of contact with the inferior wall of the arch of the aorta, and the catheter can be manipulated to advance into the ascending aorta. If no resistance is felt by 20 cm, then it is likely that the catheter has advanced down the descending aorta, and repositioning is required. When the catheter advances correctly down the ascending aorta, it “bounces” at about 10–15 cm on the leaflets of the aortic valve and can then be pulled back slightly. The balloon is then inflated above the ostia in the ascending aorta to prevent the flow of contrast agent up the ascending aorta. The left common carotid artery is used, as in our experience this side achieves a higher direct success rate than from the right (Fig. 8.2).
We have utilized many catheters for this purpose and have reported the use of a standard 14 Fr urinary catheter with a equal to or greater than 30 mL balloon size [11, 18]. However, in order to improve cannulation success rate and to be able to access the coronary ostia with other catheters, we have designed a dedicated targeted PMCTA catheter (the Cadatheter patent [PCT/GB2012/050359]). This design aims to achieve an ideal combination of rigidity, length, balloon size and characteristics, tip and marker configuration, and ability for repetitive use.
A guidewire may help stiffen the catheter in difficult cases. The balloon is inflated with dilute water-soluble radiographic contrast (1 in 50 dilution of Urografin, Madrid, Spain and Berkshire, UK) to help ascertain the position of the balloon in the aorta on initial scans and reposition it if required (Fig. 8.3).
(a) Incision made above the clavicle on the lateral side of the neck. Following blunt dissection, the left common carotid artery is elevated by means of an aneurysm hook prior to incision of the anterior arterial wall of the carotid artery. (b), A suitable PMCTA catheter is inserted into the carotid artery. Lengths of string are used to tie off the superior aspect of the artery and act as a marker for the inferior aspect
2.1.1 Contrast Agent Injection
Initially, we targeted PMCTA using a manual injection method. However, it has been recognized in ex vivo coronary angiography studies that coronary artery stenosis may be better assessed under physiologic conditions that mimic arterial pressure [17]. Furthermore, because of the rapid dispersal of water-soluble iodinated contrast media from the vascular to the interstitial space, it is recognized in clinical practice that scanning is best performed dynamically during the injection to gain optimal arterial contrast. To achieve this dynamic scanning manual injection is difficult because it involves radiation exposure to the operator and the injection pressure is variable. We therefore now use a pump injector and scan dynamically during pressure injection [16] (Fig. 8.4).
The sequence involves five runs, three after air injection and two after positive water-soluble iodinated contrast injection. The pump injector is used to inject 300 mL of air at 6 mL/s, twice in the supine position and then once in the right lateral decubitus position. Positive contrast medium (Urografin, 150 mg/mL, Bayer HealthCare plc; Berkshire, UK) diluted 1:10 is then injected (150 mL at 3 mL per second), first in the right lateral decubitus position and then in the supine position. Imaging is performed to run concurrently with the end of the injection so that images are acquired while the arteries are under pressure (43 s delay from start of injection to start of imaging).
We use the right lateral decubitus position to facilitate air passage into the left coronary arteries and positive contrast material into the right coronary artery (Fig. 8.5). Multiple injections are useful to assist complete coronary artery opacification and to confirm whether any filling defects or apparent stenoses are consistent.
We have found that this contrast medium and injection protocol does not affect subsequent toxicology and DNA analysis [19, 20].
2.1.2 Differences Between Targeted PMCTA and Whole-Body PMCTA Techniques
Low molecular weight water-soluble iodinated contrast agents have rapid dispersal from the vascular to the extravascular space in comparison to higher molecular weight hydrophobic compounds such as oil-based contrast media or contrast in a viscous carrier such as polyethylene glycol (PEG). This may lead to (1) alterations in cellular structure, (2) diminution of contrast, and (3) contrast material leak in areas of postmortem tissue breakdown such as the stomach [21, 22]. Thus different contrast media will have different perfusion patterns with different pathophysiologic implications.
We have found that our targeted approach does not cause these problems owing to dynamic rapid scanning before contrast dispersal and the relatively small quantity of contrast injected. The dispersal of contrast medium is also useful in that it allows assessment of tissue perfusion (Fig. 8.6). It has been proposed that assessing cardiac tissue for perfusion may be useful in diagnosing cardiac ischemia [12]. In our daily work we look for this sign but treat it with caution because perfusion defects can also be caused by technical or postmortem changes in normal hearts; in addition, in clinical practice myocardial ischemia can cause paradoxically increased enhancement for a number of complex reasons [23].
3 Interpretation of Coronary Artery Angiography
3.1 PMCTA for the Coronary Arteries
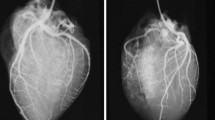
Our standard approach is to assess the precontrast (native) images and all five contrast-enhanced runs to assess the best views for each artery. If an abnormality is detected in any location, other views are also checked to make sure the abnormality is constant.
The optimum run is variable, but we often find that the first or second air run is optimal for the right coronary artery and either the right lateral decubitus air run or the supine contrast run is best for the left-sided arteries. Review is performed first using the axial scans, which can quickly determine the overall state of the coronary arteries in terms of calcification and grossly normal or abnormal. More detailed review then uses a curved multiplane projection (cMPR) approach. The vessel is generally manually identified (seeded), since automatic seeding programs do not work as well as in clinical practice because of the presence of air/contrast interfaces. This approach allows the entire coronary artery to be followed and displayed in a single reconstruction (Fig. 8.7). Image analysis workstations should also allow both a longitudinal and perpendicular (axial) image of the artery to be studied. This is important for the assessment of stenosis (Fig. 8.8).
Filling is generally good in healthy arteries, and it is generally easy to follow even if there are both air and positive contrast material in the same coronary artery. Failure to fill an artery may be caused by disease but also by technical failure such as failure to achieve injection pressures in the ascending aorta (e.g., as a result of a ruptured balloon). Postmortem clots and fluid may also cause apparent filling defects. This will often move between images and therefore will not be a consistent sign. We have found that filling defects with biconcave borders is not associated with macroscopic or histologic abnormalities [13] (Fig. 8.9).
PMCTA generally has good correlation with pathology studies and autopsy, particularly when assessing the whole vessel or heart for the presence of critical stenosis. It is important to assess all runs to get a complete picture and make sure any stenosis is consistent (Fig. 8.10). However, there are clear weaknesses of PMCTA compared with macroscopic and histologic studies of the vessels: the vessel is seen poorly distal to a critical stenosis, and it is difficult to state whether a stenosis is chronic or caused by acute plaque hemorrhage or rupture. PMCTA, however, does have some clear advantages over autopsy, particularly in calcified vessels where cutting the vessel may damage it, giving the impression of critical stenosis (Fig. 8.11).
When a coronary artery stenosis is observed and is shown to be consistent on all images, other factors may also be used to assess its significance. For example a perfusion deficit and lack of calcification may indicate an acute soft plaque rupture in the presence of a convincing medical history (Fig. 8.12). Alternatively, the use of air as a contrast medium as it enters the left ventricle allows assessment of the myocardium, and thinning or scarring of the left ventricular (LV) wall suggests chronicity or an old cardiac event (Fig. 8.13).
PMCTA can also pick up potentially serious anatomic anomalies of the coronary artery [24] (Figs. 8.14 and 8.15). Other clinical variants also need to be recognized. Identifying previous coronary bypass grafts is important because some of these may not be filled by contrast material (such as internal mammary artery grafts), and the chronic stenosis in the native arteries may be overinterpreted as a clinically important stenosis. Furthermore, coronary artery stents may actually be difficult to see in areas of significant calcification (as in clinical practice) and should be carefully looked for (Fig. 8.16).
This study shows air (a) and positive contrast (b) cMPR images of the same left anterior descending artery. The filling defect (open arrows) with biconcave margins is consistent with postmortem fluid or clot and was not present on the positive contrast run of the same vessel or associated with pathology on autopsy. The other narrowing (closed arrow) was consistent on all images and was associated with a 50 % stenosis on autopsy
Curved MPR (cMPR) images from two air runs (a, b) and a positive contrast run (c). A consistent stenosis is seen in the proximal right coronary artery (RCA) confirmed at autopsy (open arrows). The apparent left anterior descending (LAD) artery stenosis seen on the first air run (a, closed arrows) is not consistent on other runs and was not seen at autopsy
Curved (a) and standard (b) MPR images of the LAD artery and (c) a cross- sectional view of the myocardium in a 56-year-old man with recent increasing chest pain on exertion and then sudden collapse and death. The images show a stenosis with visible noncalcified plaque (arrows) and a large myocardial perfusion deficit (*). Autopsy showed plaque rupture causing myocardial infarction relating to the abnormality seen on PMCTA
Anomalous origin of the RCA shown in serial images (a–d). The normal origin (large arrow) and anomalous origin (small arrow) are shown (a). (b–d), The anomalous artery is shown (small arrows) passing between the air-filled aorta and the pulmonary trunk (*). Although this is a recognized lethal anomaly, it was not the cause of death in this case, and caution should be taken before interpreting congenital abnormalities as a cause of death in adults
Three-dimensional reconstructions (a, c) and MPR images (b) showing different cases with coronary artery stents (open arrows). These can be difficult to discern from calcification and may be missed if their characteristic shape and distinct margins are not recognized. The closed arrow (c) shows a significant stenosis in a nonstented region causing critical myocardial ischemia
3.1.1 PMCTA for the Myocardium and Valves
As already mentioned, PMCTA, particularly when using air as the contrast medium, is also useful for assessing the myocardium and valves because air passes into the ventricles and atria. This helps us assess for left ventricular hypertrophy (LVH) (Fig. 8.17). However, one should be cautious when using LV thickness as the only sign of LVH because of the inconsistent effects of rigor mortis. Patent and stenosed aortic and mitral valves can also be assessed, and this may be useful when considering LV thickness (Fig. 8.18). Both air and positive contrast material can also be useful for identifying and assessing ventricular aneurysms and rupture (Figs. 8.19 and 8.20).
Short (a) and long (b) axis views of the myocardium with air contrast studies of the left descending (c) and circumflex (d) arteries. There was independent agreement from PMCTA and autopsy that both ventricular hypertrophy (double arrow heads), probably due to hypertension and myocardial ischemia due to critical arterial stenosis (single arrow) led to death
Different cases showing the aortic valve (*). In (a) there is mild aortic valve calcification with normal valve diameter and normal myocardial thickness (double arrow); (b) shows left ventricular hypertrophy (LVH) (double arrow) with normal aortic valve diameter; (c, d) are pre- and postcontrast images showing calcified aortic valve stenosis and LVH
Precontrast long (a) and short (b) axis views and postcontrast long (c) and short (d) axis views of the left ventricle (LV), showing a left ventricular rupture. This is suspected on the precontrast views due to the hemopericardium (*). However, contrast is required to demonstrate the actual rupture site (arrows)
4 Identifying the Cause of Death: the Balance of Probabilities
When assessing sudden unexplained but probably natural death in the elderly, potentially lethal conditions such as coronary artery stenosis, LVH, and respiratory disease are quite common. So unless there are clear signs of acute deterioration in the pathology, such as indications of acute pneumonia, hemorrhage, or arterial plaque dissection, it may be impossible to state with certainty what the actual cause of death was. In our experience this is equally a problem for PMCT and for invasive autopsy. We have experience of many cases where both tests have been reported independently as part of research and despite both tests having shown the same pathologies, different conclusions were reached because of a different emphasis on each abnormality. For cases referred by Her Majesty’s Coroner in England and Wales, the balance of probabilities is required; therefore, it is acceptable to state the probable cause of death rather than to prove the cause (Fig. 8.21). A different approach would clearly be required in a case where criminal law is involved, and therefore we would advocate that the gold standard is both invasive autopsy and PMCTA in these cases.
Targeted coronary angiography and pulmonary ventilation (VPMCTA) was used in this case. Air (a) and positive (b) contrast images of the arteries (RCA right coronary artery, LAD left anterior descending artery), postventilation lung (c) and postcontrast myocardial (d) images are shown (RV right ventricle, LV left ventricle). VPMCTA independently showed agreement with autopsy findings, with pathology in the lung (emphysema and super added infection) and in the heart (moderate coronary vascular disease). However, on a balance of probabilities, the primary cause of death at VPMCTA was attributed to the coronary arteries, whereas at autopsy it was attributed to the lung pathology. Both reporters recognized that either primary cause could be correct
5 Conclusion
The technique of targeted coronary PMCTA has been developed to provide a rapid and relatively inexpensive method for investigation of causes of death. However, the decision of what angiography method to use, if any, depends on the questions to be answered in each case. Many of our cases are part of postmortem investigation as requested by HM Coroners for the investigation of adult sudden death in order to replace the need for invasive autopsy. The main purpose of the investigation is to confirm that death has occurred naturally and to give a medical cause on the “balance of probabilities.” For these cases the most common finding is related to the heart and coronary artery disease. For this purpose targeted coronary PMCTA can replace the need for autopsy in many HM Coroner investigations. For other types of investigation, such as those performed for the purpose of criminal examination, PMCT is often performed as an adjunct to the autopsy. In these cases we may use PMCT alone, PMCTA with pulmonary ventilation (VPMCTA), targeted coronary PMCTA, or whole body PMCTA techniques.
References
Luce T. Coroners and death certification law reform: the coroners and justice act 2009 and its aftermath. Med Sci Law. 2010;50:171–8.
Rutty GN, Rutty JE. Perceptions of near virtual autopsies. J Forensic Leg Med. 2011;18:306–9.
Dirnhofer R, Jackowski C, Vock P, Potter K, Thali MJ. VIRTOPSY: minimally invasive, imaging-guided virtual autopsy. Radiographics. 2006;26:1305–33.
Rutty GN, Morgan B, O’Donnell C, Leth PM, Thali M. Forensic institutes across the world place CT or MRI scanners or both into their mortuaries. J Trauma. 2008;65:493–4.
Okuda T, Shiotani S, Sakamoto N, Kobayashi T. Background and current status of postmortem imaging in Japan: short history of “autopsy imaging (ai)”. Forensic Sci Int. 2013;225:3–8.
Roberts IS, Benamore RE, Benbow EW, Lee SH, Harris JN, Jackson A, et al. Post-mortem imaging as an alternative to autopsy in the diagnosis of adult deaths: a validation study. Lancet. 2012;379:136–42.
Wichmann D, Obbelode F, Vogel H, et al. Virtual autopsy as an alternative to traditional medical autopsy in the intensive care unit: a prospective cohort study. Ann Intern Med. 2012;156:123–30.
Kasahara S, Makino Y, Hayakawa M, Yajima D, Ito H, Iwase H. Diagnosable and non-diagnosable causes of death by postmortem computed tomography: a review of 339 forensic cases. Leg Med (Tokyo). 2012;14:239–45.
Biggs MJ, Brown LJ, Rutty GN. Can cause of death be predicted from the pre-necropsy information provided in coroners’ cases? J Clin Pathol. 2008;61:124–6.
Rutty GN, Duerden RM, Carter N, Clark JC. Are coroners’ necropsies necessary? A prospective study examining whether a “view and grant” system of death certification could be introduced into England and Wales. J Clin Pathol. 2001;54:279–84.
Saunders SL, Morgan B, Raj V, Robinson CE, Rutty GN. Targeted post-mortem computed tomography cardiac angiography: proof of concept. Int J Legal Med. 2011;125:609–16.
Roberts IS, Traill ZC. Minimally invasive autopsy employing post-mortem CT and targeted coronary angiography: evaluation of its application to a routine coronal service. Histopathology. 2014;64:211–7.
Morgan B, Biggs MJ, Barber J, Raj V, Amoroso J, Hollingbury FE, et al. Accuracy of targeted post-mortem computed tomography coronary angiography compared to assessment of serial histological sections. Int J Legal Med. 2013;127:809–17.
Michaud K, Grabherr S, Doenz F, Mangin P. Evaluation of postmortem MDCT and MDCT-angiography for the investigation of sudden cardiac death related to atherosclerotic coronary artery disease. Int J Cardiovasc Imaging. 2012;28:1807–22.
Dorries C. Coroners’ courts: a guide to law and practice. 2nd ed. Oxford: Oxford University Press; 2004.
Robinson C, Barber J, Amoroso J, Morgan B, Rutty G. Pump injector system applied to targeted post-mortem coronary artery angiography. Int J Legal Med. 2013;127:661–6.
Coghill SB, Nicoll SM, McKimmie A, Houston I, Matthew BM. Revitalising postmortem coronary angiography. J Clin Pathol. 1983;36:1406–9.
Roberts IS, Benamore RE, Peebles C, Roobottom C, Traill ZC. Technical report: diagnosis of coronary artery disease using minimally invasive autopsy: evaluation of a novel method of post-mortem coronary CT angiography. Clin Radiol. 2011;66:645–50.
Rutty GN, Barber J, Amoroso J, Morgan B, Graham EA. The effect on cadaver blood DNA identification by the use of targeted and whole body post-mortem computed tomography angiography. Forensic Sci Med Pathol. 2013;9:489–95.
Rutty GN, Smith P, Visser T, Barber J, Amorosa J, Morgan B. The effect on toxicology, biochemistry and immunology investigations by the use of targeted post-mortem computed tomography angiography. Forensic Sci Int. 2013;225:42–7.
Jackowski C, Bolliger S, Aghayev E, et al. Reduction of postmortem angiography-induced tissue edema by using polyethylene glycol as a contrast agent dissolver. J Forensic Sci. 2006;51:1134–7.
Grabherr S, Djonov V, Friess A, et al. Postmortem angiography after vascular perfusion with diesel oil and a lipophilic contrast agent. Am J Roentgenol. 2006;187:W515–23.
Kim RJ, Fieno DS, Parrish TB, Thali MJ, Ranner G, Vock P, Dirnhofer R. Relationship of MRI delayed contrast enhancement to irreversible injury, infarct age, and contractile function. Circulation. 1999;100:1992–2002.
Rahalkar AM, Rahalkar MD. Pictorial essay: coronary artery variants and anomalies. In J Radiol Imaging. 2009;19:49–53.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Morgan, B., Robinson, C., Rutty, G.N. (2016). Targeted Coronary Postmortem Computed Tomography Angiography. In: Grabherr, S., Grimm, J., Heinemann, A. (eds) Atlas of Postmortem Angiography. Springer, Cham. https://doi.org/10.1007/978-3-319-28537-5_8
Download citation
DOI: https://doi.org/10.1007/978-3-319-28537-5_8
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-28535-1
Online ISBN: 978-3-319-28537-5
eBook Packages: MedicineMedicine (R0)