Abstract
Introduction
Several studies have been performed to assess the efficacy of postmortem computed tomography angiography (PMCTA) in solving cases of sudden cardiac death, even in comparison with the traditional autopsy. However, the results were often inconsistent and inconclusive. Therefore, a global discussion on the subject through a systematic review of the literature and a meta-analysis is necessary.
Methods
A systematic search of PubMed was performed up to April 23, 2018. Studies exploring the role of PMCTA in cases of sudden cardiac death and the accuracy of this method in diagnosing the cause of death compared to traditional autopsy were included.
Results
The overall sensitivity and specificity of the seven included studies, using conventional autopsy as a reference standard, were 92% and 95%, respectively. The positive and negative likelihood ratios were, respectively, 20.76 (95% CI 1.16–370.2) and 0.08 (95% CI 0.03–0.17), showing that PMCTA represents a strong indicator of the posttest probability of disease. The diagnostic odds ratio and the area under the curve were, respectively, 261.54 (95% CI 1.87–5760.53) and 0.93 (95% CI 0.90–0.95), indicating a high diagnostic power of the test.
Conclusion
PMCTA demonstrated a high accuracy in the diagnosis of parietal and luminal coronary changes but was less effective in detecting myocardial ischemia and necrosis. Therefore, the only radiological investigation is often insufficient to determine the cause of sudden death and the conventional autopsy remains the gold standard. However, PMCTA can improve the performance of the autopsy, serving as an aid and guide in the sampling phase for histopathological investigations.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Sudden cardiac death (SCD) has been defined as “a natural, unexpected fatal event occurring within 1 h from the onset of symptoms in an apparently healthy subject or in one whose disease was not so severe as to predict an abrupt outcome.” The incidence of SCD increases with age, in line with the increase in the incidence of the coronary artery disease which, according to numerous studies, represents the pathology most frequently involved in the determinism of sudden death (sudden coronary death) [1, 2].
Postmortem examination and autopsy represent reliable methods for determining the causes of SCD [3, 4]. However, due to ethical, religious, cultural, economic and organizational reasons, the number of autopsies performed is decreasing worldwide and the use of minimally invasive ancillary methods is considered preferable in some circumstances.
In view of these circumstances, postmortem cardiac imaging is assuming increasing importance in the study of myocardium and coronary arteries as an aid and guide in the execution of conventional autopsy and, sometimes, as an alternative [5, 6].
Currently, postmortem computed tomography (PMCT), postmortem computed tomography angiography (PMCTA), postmortem magnetic resonance (PMMR) and postmortem magnetic resonance angiography (PMMRA) have become established methods due to numerous studies that have documented the undeniable advantages in terms of acquisition times, costs and possibility to review the data acquired at any time [7,8,9,10,11,12,13].
A series of studies have been performed over the years to assess the efficacy of PMCTA in solving cases of sudden cardiac death, even in comparison with the traditional autopsy. However, the results are often inconsistent and inconclusive. Therefore, a global discussion on the subject through a systematic review of the literature and a meta-analysis is necessary.
This paper aims at analyzing the diagnostic accuracy of PMCTA in sudden cardiac death cases as well as evaluating the possibility to use this method as an alternative to postmortem examination and conventional autopsy in such cases.
Methods
The systematic review and the meta-analysis were conducted following the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement’s criteria [14, 15].
Searching strategy
The study was performed using Boolean operators, MeSH terms and free-text terms to expand research and not to exclude potentially relevant articles.
Studies focusing on the role of PMCTA and traditional autopsy in cases of sudden cardiac death due to coronary artery disease were initially searched using PubMed, with the terms “((((((coronary artery disease[MeSH Terms]) OR cardiac death[MeSH Terms]) OR sudden cardiac death[MeSH Terms]))) AND (((((postmortem imaging) OR PMCTA) OR postmortem CTA) OR postmortem computed tomography angiography) OR non-invasive autopsy) OR minimally invasive autopsy) AND ((((conventional autopsy) OR traditional autopsy) OR autopsy) AND full text[sb] AND Humans[Mesh]).”
“Full-text,” “Humans” and “English” filters have been applied. No time restrictions have been applied. The last research was carried out on April 23, 2018. The PubMed section “similar articles” and the references of the selected articles were used to expand the research.
Inclusion and exclusion criteria
Studies were included if they met the following criteria: (1) population consisting of persons who died of suspected sudden cardiac death; (2) evaluation of the accuracy of PMCTA in diagnosing the cause of death and in detecting major or minor diagnostic findings; (3) comparison of the efficacy of PMCTA with the gold standard, the conventional autopsy; (4) availability of the entire panel of true positives (TP), false positives (FP), false negatives (FN) and true negatives (TN), or sufficient data to calculate them. Meanwhile, studies were excluded if they were: (1) case reports; (2) not original research, such as review articles; (3) studies conducted on fetuses.
Data extraction and assessment
Data from each included study were extracted using Microsoft Excel spreadsheets, including information on authors, journal, publishing years, nation, population selection criteria, sample size, gender, age, diagnostic technique under examination, reference standards, as well as results in terms of TP, FP, FN and TN.
The quality of the individual studies was determined through the QUADAS-2 (Quality Assessment of Diagnostic Accuracy Study) tool, structured in four key domains: (1) patient selection; (2) index test; (3) reference standard; and (4) flow and timing. The risk of bias for each domain was considered low, high or unclear in cases where it was not deductible. The studies were considered at low risk of bias if the population selection criterion was clear, if the radiologist and forensic pathologist operated in double-blind, if they both had access to the same information about the case and if the interval between performing the imaging exam and the autopsy was less than 72 h. The studies were considered at moderate risk of bias in the presence of at least one of the following conditions: (1) unclear selection, (2) knowledge by the radiologist or the forensic pathologist of the other test results, (3) latency time between the two investigations exceeding 72 h. The studies were considered at high risk of bias in the presence of two or more of the previously indicated conditions.
Statistical analysis
The meta-analysis was conducted using Stata 13.0 (Stata Corporation, College Station, Texas, USA) [16,17,18,19]. The results in terms of TP, FP, FN and TN were used to calculate the sensitivity and specificity in each of the primary studies. The sensitivity and specificity values of the individual studies were graphically represented in a forest plot using the Meta-DiSc software (Unit of Clinical Biostatistics, Ramón y Cajal Hospital, Madrid, Spain). The heterogeneity between the primary studies was evaluated through the Cochran Q test (Chi-square test) and the Higgins index (I2). For the synthesis of the results on the PMCTA performances, two random effect models were used: the bivariate model and the HSROC (Hierarchical Summary Receiver Operating Characteristic) model.
Results
Included studies
By applying the search strategy mentioned above, we found a total of 793 studies in PubMed. A total of 767 articles were removed due to irrelevant titles or abstracts; most of them were researches regarding perinatal autopsy and postmortem MRI. After this elimination, 26 papers were eligible for full-text review. Finally, 7 studies were included in the meta-analysis, [20,21,22,23,24,25,26] while the others were excluded as they did not meet the eligibility criteria. The process of study inclusion is illustrated in Fig. 1.
The sample size ranged between 5 and 38 with a total of 127 subjects; the publication time was from 2010 to 2014. Three studies evaluated the diagnostic capacity of the PMCTA total body, associated with PMCT and/or biopsy. Four studies, on the other hand, investigated the role of selective coronary PMCTA. The reference standard was represented in all cases by conventional autopsy. The main characteristics of the seven included studies are listed in Table 1.
Risk of bias assessment
The quality of the studies was determined with the QUADAS-2 tool. The risk of bias was globally low or unclear in the four domains except for the reference standard; the latter was at high risk in two studies because the autopsy was performed by a pathologist aware of the results of radiological investigations. Therefore, four studies were considered at low risk of bias, one at low/undefined risk and two at moderate/undefined risk (Table 2).
Qualitative analysis (systematic review)
Bolliger et al. [20] evaluated the diagnostic accuracy of a minimally invasive approach (PMCT, PMCTA, CT-guided biopsy) in 20 cases of apparently natural death of which 11 of sudden coronary death. PMCTA and traditional investigations have agreed in all cases on the cause of death. In only one case, the minimally invasive approach underestimated the severity of ischemic heart disease because, despite the visualization of a coronary thrombotic occlusion, the necrotic area of interest had not been detected.
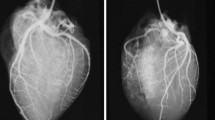
Roberts et al. [21] compared the diagnostic accuracy of selective coronary PMCTA and autopsy in 10 cases of sudden death. In 8 cases, there was complete agreement between the data obtained from the two tests, while in one case radiological investigations had overestimated the severity of a stenosis that was considered nonsignificant to autopsy. Finally, in one case there was a discrepancy between the two techniques, with a diagnosis of coronary stenosis and ischemic cardiopathy at PMCTA and a diagnosis of hypertensive heart disease and asthma at autopsy.
Ross et al. [22] have shown a concordance between conventional autopsy and PMCTA associated with CT-guided biopsy in 20 cases of sudden death after chest pain. In 8 of the 9 cases of sudden coronary death, the PMCTA had been able to highlight the alterations responsible for the death, while in one case, early myocardial infarction of the papillary muscles had been missed.
Michaud et al. [23] compared the results obtained with PMCT, PMCTA and conventional autopsy in 23 cases of sudden death associated with ischemic heart disease. PMCTA allowed an excellent visualization of the coronary arteries and a better evaluation of stenosis and occlusions. However, PMCTA has not been able to identify early-stage necrosis areas. Furthermore, a postmortem clot had been visualized as a complete perfusion defect resulting in a false positive.
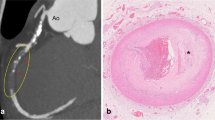
Morgan et al. [24] investigated the sudden death of five subjects with selective coronary PMCTA. Regarding the detection of coronary disease, PMCTA and autopsy showed complete concordance in identifying at least one area of critical stenosis in each case; however, 18 discrepancies were recorded, including 5 major and 13 minor. PMCTA demonstrated poor accuracy in the evaluation of areas downstream of a critical stenosis, while it showed a greater diagnostic accuracy in the detection of coronary calcifications. Finally, PMCTA was unable to identify findings such as intraplaque hemorrhage and dissection with recanalization; however, the unidentified findings did not invalidate the judgment on the cause of death as they were at the level of correctly identified critical stenosis.
Inokuchi et al. [25] compared autopsy findings with those of selective coronary PMCTA in 38 cases of death apparently associated with ischemic heart disease. In 18 cases, both the autopsy and the PMCTA showed coronary lesions that only in 11 cases were causally related to death. In 2 cases, selective coronary PMCTA failed to detect the presence of a critical stenosis. In the remaining 18 cases, both methods did not show coronary disease.
Polacco et al. [26] investigated 11 cases of suspected SCD identifying 7 cases in which the cause of death was attributed to myocardial infarction; in 6 of these cases, the selective coronary PMCTA detected the ischemic area as an area of extravasation of the contrast medium. In 2 cases, the death was attributed to calcific aortic valve stenosis, while in the other two cases toxicological investigations were positive for lethal intoxication.
Statistical analysis (meta-analysis)
Sensitivity was homogeneously high in all studies with values ranging from 86 to 100% (mean value of 92%; CI 95% 0.84–0.97) and absent heterogeneity (p 0.67 at Cochran test; I2 0%) (Fig. 2).
Specificity showed a wide variability ranging from 0 to 100% (mean value of 94%; CI 95% 0.83–0.99) and high heterogeneity (p 0.01 at the Cochran test; I2 62.2%) (Fig. 3).
The summary point determined by the HSROC model showed values of 92% (CI 95% 0.84–0.96) for sensitivity and 95% (CI 95% 0.51–0.98) for specificity (Fig. 4). LR+ and LR− were, respectively, 20.76 (95% CI 1.16–370.2) and 0.08 (CI 95% 0.04–0.17); the dOR had a value of 261.54 (CI 95% 1.87–5760.53) (Table 3).
The area under the curve, analyzed using the bivariate model, showed a value of 0.93 (95% CI 0.90–0.95) (Fig. 5).
Discussion
Sudden cardiac death in adults is attributed in most cases to coronary artery disease and its complications, while non-ischemic cardiomyopathies or arrhythmic syndromes in the absence of coronary pathology are responsible for a minority of cases.
In conventional postmortem investigations, the diagnosis of coronary artery disease or ischemic heart disease is obtained after a complete autopsy followed by a gross examination of the heart and a microscopic examination with histological and immunohistochemical staining. Nevertheless, such investigations require the experience of the pathologist and the application of a rigorous methodological approach to the complex task represented by sudden cardiac death.
Postmortem imaging provides a decisive contribution to forensic pathology, its importance is widely recognized, and its use is increasingly common in forensic practice [27]. This consideration assumes remarkable significance in light of the importance of imaging methods in the approach to cases of sudden cardiac death [28, 29].
Computed tomography (CT) is the most widely used method in modern forensic radiology. Despite the extensive use of this type of investigation, the method presents two major limitations consisting of the low density of soft tissues and the poor visualization of vascular structures. In fact, in the included primary studies that required the execution of a scan without contrast medium before PMCTA, PMCT did not prove useful in the diagnosis of coronary heart disease, being able only to highlight findings such as cardiac tamponade or calcifications of coronary arteries.
Post-Mortem CT Angiography (PMCTA), on the other hand, is a minimally invasive procedure, able to show direct (coronary stenosis or occlusions) and indirect (contrastographic enhancement of the myocardium as a sign of ischemic necrosis) evidence of coronary artery disease with a much higher diagnostic accuracy than unenhanced PMCT [30, 31].
The main advantage of PMCTA is the possibility of visualizing myocardial bridging and alterations of luminal patency without altering the examined vascular structure, as it inevitably occurs during the conventional investigation. In fact, PMCTA studies the vessels throughout their course allowing to identify even small areas of critical stenosis that could be missed by the sections carried out during the autopsy. In addition, PMCTA has shown to be superior to autopsy in investigating the patency of coronary vessels as it is able to demonstrate through perfusion pressure the patency of calcific vessels that had been described as occluded at the autopsy.
Post Mortem CT Angiography also allows the study and three-dimensional evaluation of coronary artery bypass grafts and coronary stents, [32, 33] facilitating the forensic pathologist in the identification of findings difficult to highlight during autopsy due to the adhesion phenomena attributable to the surgical manipulation of the pericardium and heart. The injection of contrast medium finally allows a better assessment of pathological conditions of the myocardium such as traumatic tears or fibrotic areas.
The main limitation of PMCTA is the impossibility of providing data on the functional relevance of a stenosis, being an exclusively morphological imaging technique. The included primary studies have also shown that only a relatively low percentage of ischemic myocardial necrosis was detectable by PMCTA as a contrast enhancement area, documenting a sensitivity limit of this method compared to the histopathological evaluation or other imaging techniques such as PMMR. On the other hand, the tomographic scans are limited by the impossibility of visualizing the vessels downstream of the stenosis and by the difficulty in ascertaining the acute or chronic nature of the stenosis. A further doubt about the diagnostic efficacy of PMCTA could derive from the possibility of a thrombus displacement following coronary artery reperfusion, with consequent failure to visualize coronary occlusion; although the hypothesis cannot be refuted with certainty, several studies have reported as unlikely the possibility that a perfusion pressure lower than the in vivo one can determine the displacement of a thrombus.
The present systematic review and meta-analysis demonstrated the high accuracy of PMCTA in the diagnosis of sudden coronary death. Post Mortem CT Angiography represents a valid tool for the assessment of coronary arteries anatomy, for the detection of stenosis and occlusions, [34] as well as for the guide of sampling for histological examination. At the same time, however, this method has proved less effective in the visualization of myocardial ischemia and necrosis.
There are two major limitations concerning the present study. First, the meta-analysis was performed on a small number of primary studies, many of which had a small population and did not provide enough information to clearly determine the quality of the study. Second, there is a moderate heterogeneity between studies, probably due to the protocol used to perform PMCTA and to the population examined. Therefore, even if an HSROC model was used for data analysis, the results should be interpreted carefully.
For these reasons, to date, autopsy followed by histological examination remains the gold standard for the diagnosis of sudden coronary death. The current trend must be to combine PMCTA with a conventional autopsy to implement the diagnostic quality of postmortem investigations [35]. In fact, PMCTA is extremely useful in cases where a minimally invasive approach is required for several reasons or in cases where a guide to myocardial and coronary sampling is required during the autopsy.
In conclusion, in the field of cardiac pathology, postmortem coronary imaging is still insufficient to establish with certainty the cause of death and autopsy remains the gold standard. Currently, in fact, no radiological technique can replace the histological examination.
The value of this study is in the combination of data from several studies resulting in the evaluation of a larger cohort of subjects as well as in obtaining data more applicable to forensic practice. Nevertheless, further studies are still required to offer better evidence on the use of PMCTA as a routine investigation or as an aid to conventional autopsy.
The role of PMCTA in cases of sudden cardiac death is that of guidance and aid to traditional autopsy. In particular, this investigation can determine an increase in diagnostic performance and ensure a better evaluation of the coronary arteries as well as a more accurate coronary and myocardial sampling [36,37,38,39,40].
For these reasons, postmortem computed tomography angiography must be considered an ancillary method in determining the cause of sudden cardiac death, rather than an alternative to conventional investigations [41, 42].
References
Priori SG, Aliot E, Blomstrom-Lundqvist C, Bossaert L, Breithardt G, Brugada P, Camm AJ, Cappato R, Cobbe SM, Di Mario C, Maron BJ, McKenna WJ, Pedersen AK, Ravens U, Schwartz PJ, Trusz-Gluza M, Vardas P, Wellens HJ, Zipes DP (2001) Task force on sudden cardiac death of the European Society of Cardiology. Eur Heart J 22:1374–1450
Hayashi M, Shimizu W, Albert C (2015) The spectrum of epidemiology underlying sudden cardiac death. Circ Res 116(12):1887–1906
Basso C, Aguilera B, Banner J, Cohle S, d’Amati G, de Gouveia RH, di Gioia C, Fabre A, Gallagher PJ, Leone O, Lucena J, Mitrofanova L, Molina P, Parsons S, Rizzo S, Sheppard MN, Mier MPS, Kim Suvarna S, Thiene G, van der Wal A, Vink A, Michaud K (2017) Guidelines for autopsy investigation of sudden cardiac death: 2017 update from the Association for European Cardiovascular Pathology. Virchows Arch 6:691–705
Burton JL, Underwood J (2007) Clinical, educational, and epidemiological value of autopsy. Lancet 369:1471–1480
Bolliger SA, Thali MJ, Ross S, Buck U, Naether S, Vock P (2008) Virtual autopsy using imaging: bridging radiologic and forensic sciences. A review of the virtopsy and similar projects. Eur Radiol 18(2):273–282
Westphal SE, Apitzsch JC, Penzkofer T, Kuhl CK, Mahnken AH, Knüchel R (2014) Contrast-enhanced postmortem computed tomography in clinical pathology: enhanced value of 20 clinical autopsies. Hum Pathol 45(9):1813–1823
Vullo A, Panebianco V, Cannavale G, Aromatario M, Cipolloni L, Frati P, Santurro A, Vullo F, Catalano C, Fineschi V (2016) Post-mortem magnetic resonance foetal imaging: a study of morphological correlation with conventional autopsy and histopathological findings. Radiol Med 121(11):847–856
Lundström C, Persson A, Ross S, Ljung P, Lindholm S, Gyllensvärd F, Ynnerman A (2012) State-of-the-art of visualization in post-mortem imaging. APMIS 120:316–326
Bolliger SA, Thali MJ (2015) Imaging and virtual autopsy: looking back and forward. Philos Trans R Soc Lond B Biol Sci 370:1674
Pomara C, Fineschi V, Scalzo G, Guglielmi G (2009) Virtopsy versus digital autopsy: virtuous autopsy. Radiol Med 114:1367–1382
De Marco E, Vacchiano G, Frati P, La Russa R, Santurro A, Scopetti M, Guglielmi G, Fineschi V (2018) Evolution of post-mortem coronary imaging: from selective coronary arteriography to post-mortem CT-angiography and beyond. Radiol Med 123(5):351–358
Saunders SL, Morgan B, Raj V, Rutty GN (2011) Post-mortem computed tomography angiography: past, present and future. Forensic Sci Med Pathol 7:271–277
Dirnhofer R, Jackowski C, Vock P, Potter K, Thali MJ (2006) Virtopsy: minimally invasive, imaging-guided virtual autopsy. Radiographics 26:1305–1333
Moher D, Liberati A, Tetzlaff J, Altman D (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Plos Med 6(7):e.1000097
Liberati A (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann Intern Med 151(4):W65–W94
Leeflang M (2014) Systematic reviews and meta-analyses of diagnostic test accuracy. Clin Microbiol Infect 20(2):105–113
Kim K, Lee J, Choi S, Huh J, Park S (2015) Systematic review and meta-analysis of studies evaluating diagnostic test accuracy: a practical review for clinical researchers-part I. General guidance and tips. Korean J Radiol 16(6):1175
Lee J, Kim K, Choi S, Huh J, Park S (2015) Systematic review and meta-analysis of studies evaluating diagnostic test accuracy: a practical review for clinical researchers-part II. Statistical methods of meta-analysis. Korean J Radiol 16(6):1188
Liu Z, Yao Z, Li C, Liu X, Chen H, Gao C (2013) A step-by-step guide to the systematic review and meta-analysis of diagnostic and prognostic test accuracy evaluations. Br J Cancer 108(11):2299–2303
Bolliger S, Filograna L, Spendlove D, Thali M, Dirnhofer S, Ross S (2010) Postmortem imaging-guided biopsy as an adjuvant to minimally invasive autopsy with CT and postmortem angiography: a feasibility study. Am J Roentgenol 195(5):1051–1056
Roberts IS, Benamore RE, Peebles C, Roobottom C, Traill ZC (2011) Diagnosis of coronary artery disease using minimally invasive autopsy: evaluation of a novel method of post-mortem coronary CT angiography. Clin Radiol 66:645–650
Ross SG, Thali MJ, Bolliger S, Germerott T, Ruder TD, Flach PM (2012) Sudden death after chest pain: feasibility of virtual autopsy with postmortem CT angiography and biopsy. Radiology 264:250–259
Michaud K, Grabherr S, Doenz F, Mangin P (2012) Evaluation of postmortem MDCT and MDCT-angiography for the investigation of sudden cardiac death related to atherosclerotic coronary artery disease. Int J Cardiovasc Imaging 28:1807–1822
Morgan B, Biggs M, Barber J, Raj V, Amoroso J, Hollingbury F, Robinson C, Rutty G (2012) Accuracy of targeted post-mortem computed tomography coronary angiography compared to assessment of serial histological sections. Int J Legal Med 127(4):809–817
Inokuchi G, Yajima D, Hayakawa M, Motomura A, Chiba F, Torimitsu S, Makino Y, Iwase H (2013) The utility of postmortem computed tomography selective coronary angiography in parallel with autopsy. Forensic Sci Med Pathol 9(4):506–514
Polacco M, Sedati P, Arena V, Pascali VL, Zobel BB, Oliva A, Rossi R (2014) Visualization of myocardial infarction by post-mortem single-organ coronary computed tomography: a feasibility study. Int J Legal Med 129(3):517–524
Grabherr S, Grimm J, Dominguez A, Vanhaebost J, Mangin P (2014) Advances in post-mortem CT-angiography. Br J Radiol 87(1036):20130488
Turillazzi E, Frati P, Pascale N, Pomara C, Grilli G, Viola RV, Fineschi V (2016) Multi-phase post-mortem CT-angiography: a pathologic correlation study on cardiovascular sudden death. J Geriatr Cardiol 13:855–865
Guidi B, Aquaro GD, Gesi M, Emdin M, Di Paolo M (2018) Postmortem cardiac magnetic resonance in sudden cardiac death. Heart Fail Rev. https://doi.org/10.1007/s10741-018-9705-0
Heinemann A, Vogel H, Heller M, Tzikas A, Püschel K (2015) Investigation of medical intervention with fatal outcome: the impact of post-mortem CT and CT angiography. Radiol Med 120(9):835–845
Takei H, Sano R, Takahashi Y, Takahashi K, Kominato Y, Tokue H, Shimada T, Awata S, Hirasawa S, Ohta N (2018) Usefulness of coronary postmortem computed tomography angiography to detect lesions in the coronary artery and myocardium in cases of sudden death. Leg Med (Tokyo) 30:46–51
Vogel B, Heinemann A, Tzikas A, Poodendaen C, Gulbins H, Reichenspurner H, Püschel K, Vogel H (2013) Post mortem computed tomography (PMCT) and PMCT-angiography after cardiac surgery Possibilities and limits. Arch Med Sad Kryminol 63(3):155–171
Vogel B, Heinemann A, Gehl A, Hasegawa I, Höpker WW, Poodendaen C, Tzikas A, Gulbins H, Reichenspurner H, Püschel K, Vogel H (2013) Post-mortem computed tomography (PMCT) and PMCT-angiography after transvascular cardiac interventions. Arch Med Sad Kryminol 63(3):255–266
Lee H, Park H, Cha JG, Lee S, Yang K (2015) Myocardial contrast defect associated with thrombotic coronary occlusion: pre-autopsy diagnosis of a cardiac death with post-mortem CT angiography. Korean J Radiol 16:1024–1028
O’Donnell C (2010) An image of sudden death: utility of routine postmortem computed tomography scanning in medico-legal autopsy practice. Diagn Histopathol 16:552–555
Rüegger CM, Bartsch C, Martinez RM, Ross S, Bolliger SA, Koller B, Held L, Bruder E, Bode PK, Caduff R, Frey B, Schäffer L, Bucher HU (2014) Minimally invasive, imaging guided virtual autopsy compared to conventional autopsy in foetal, newborn and infant cases: study protocol for the paediatric virtual autopsy trial. BMC Pediatr 14:15
Aghayev E, Thali MJ, Sonnenschein M, Jackowski C, Dirnhofer R, Vock P (2007) Post-mortem tissue sampling using computed tomography guidance. Forensic Sci Int 166:199–203
Ebert LC, Ptacek W, Naether S, Fürst M, Ross S, Buck U, Weber S, Thali M (2010) Virtobot–a multi-functional robotic system for 3D surface scanning and automatic post mortem biopsy. Int J Med Robot 6:18–27
Busardò FP, Frati P, Santurro A, Zaami S, Fineschi V (2015) Errors and malpractice lawsuits in radiology: what the radiologist needs to know. Radiol Med 120(9):779–784
Grabherr S, Heinemann A, Vogel H, Rutty G, Morgan B, Woźniak K, Dedouit F, Fischer F, Lochner S, Wittig H, Guglielmi G, Eplinius F, Michaud K, Palmiere C, Chevallier C, Mangin P, Grimm JM (2018) Postmortem CT angiography compared with autopsy: a forensic multicenter study. Radiology 1:170559
Poulsen K, Simonsen J (2007) Computed tomography as routine in connection with medico-legal autopsies. For Sci Int 171(2–3):190–197
Flach PM, Thali MJ, Germerott T (2014) Times have changed! Forensic radiology-a new challenge for radiology and forensic pathology. Am J Roentgenol 202(4):W325–W334
Author information
Authors and Affiliations
Contributions
All authors contributed to manuscript drafting and critical discussion and approved the definitive version.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standards
This article does not contain any studies with human participants or animals performed by any of the authors. All accepted principles of ethical and professional conduct have been followed.
Rights and permissions
About this article
Cite this article
La Russa, R., Catalano, C., Di Sanzo, M. et al. Postmortem computed tomography angiography (PMCTA) and traditional autopsy in cases of sudden cardiac death due to coronary artery disease: a systematic review and meta-analysis. Radiol med 124, 109–117 (2019). https://doi.org/10.1007/s11547-018-0943-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-018-0943-y