Abstract
Sperm washing is performed to remove seminal plasma and increase sperm density prior to intrauterine insemination (IUI). Gradient sperm washing is highly effective at isolating motile sperm from the ejaculate of most men. IUI may be indicated in cases of poor postcoital testing due to hostile or absent cervical mucus, oligospermia, or the presence of sperm antibodies. It may be used in conjunction with artificial insemination or IVF procedures.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Sperm washing is performed to remove seminal plasma and increase sperm density prior to intrauterine insemination (IUI) [1]. Gradient sperm washing is highly effective at isolating motile sperm from the ejaculate of most men. IUI may be indicated in cases of poor postcoital testing due to hostile or absent cervical mucus, oligospermia, or the presence of sperm antibodies [2]. It may be used in conjunction with artificial insemination or IVF procedures.
2 Specimen Collection
The patient is instructed on how to collect the specimen (see “Semen Collection and Labeling Procedure”). The patient collects the specimen into a sterile container and brings it to the laboratory. The patient, or partner, is told to return in ~1 h to pick up the washed specimen.
3 Equipment and Materials
-
A.
Components of the sperm separation kit—sterile colloidal suspension of silica particles stabilized with covalently bound hydrophilic silane supplied with HEPES-buffered human tubal fluid (HTF):
-
1.
Lower phase (80 %)
-
2.
Upper phase (40 %)
-
1.
-
B.
Sperm washing media (modified HTF with 5 % human serum albumin and gentamicin
-
C.
Disposable sterile 15 mL polystyrene conical centrifuge tube(s) with cap(s)
-
D.
Centrifuge
-
E.
37 °C incubator
-
F.
Sterile graduated serological pipettes (2 mL)
-
G.
Computer-assisted semen analyzer (CASA)
-
H.
Long stemmed (9”) pasteure pipette
-
I.
Disposable 20 μm sperm counting chamber
-
J.
Makler counting chamber
-
K.
Dilution cups 2-mL
-
L.
Brown paper bags
-
M.
Disposable sterile transfer pipettes
-
N.
Viscosity treatment system (when applicable)-5 mg chymotrypsin
4 Quality Control
-
A.
Sperm recovery and percent motility are checked and recorded semiannually on all IUI samples.
Criteria: None defined.
-
B.
Daily Precision:
A patient specimen should be selected at random and run through CASA. A manual count and motility reading should be performed simultaneously.
Criteria: All manual results should be within 20 % of CASA value.
Response: If results are not within the defined percentage difference, the sample must be repeated. If it is still out-of-range, inform supervisor or director.
-
C.
Technologists review patient results to check for technical and clerical errors prior to release of specimen for insemination.
5 Procedure
5.1 Prepare Reagents
-
1.
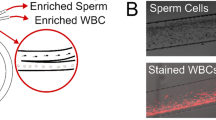
Bring the upper and lower phase, HTF, and semen sample to 37 °C by incubating for 20 min (Fig. 14.1).
-
2.
Transfer 2 mL of the lower phase into a sterile disposable 15 mL conical centrifuge tube.
-
3.
Layer 2 mL of the upper phase on top of the 2 mL lower phase using a sterile pipette. Slowly dispense the upper phase lifting the pipette up the side of the tube as the level of the upper phase rises.
Note: A distinct line separating the two layers should be observed. This two-layer gradient is stable for up to 2 h.
5.2 Prepare Paperwork/Accept Patient Specimen
-
1.
Make sure the specimen container is labeled with two identifiers. Acceptable identifiers are either the patient name and date of birth or the patient name and medical record number (or SSN).
Note: If all of the patient information on the specimen cup is not present, the container should be labeled in front of the patient.
-
2.
Have the “Sperm Wash Worksheet,” “Artificial Insemination by Husband,” “Specimen Drop-off/Pick-up Form,” and two IUI labels prefilled before the patient arrives with all pertinent information.
-
3.
Label a 15 mL centrifuge tube with the patient’s and partner’s name, medical record numbers, and date. The tube should also be labeled with color-coded tape* as an extra identifier.
*Note: Color-coded labeling tape should be used for all tubes, media, and paperwork and should be specific (of the same color) for each patient.
-
4.
Have the person delivering the specimen sign the “Specimen Drop-off/Pick-up Form.” They must at this time present an acceptable ID card (e.g., driver’s license, employee badge). The technologist accepting the specimen must record on the sheet the type of identification presented and the appropriate ID number.
-
5.
Label a 2 mL conical cup for the post-wash analysis. Remove the warm tube of sperm wash media (HTF with 5 % HSA) from the 37 °C incubator and label it with the patient’s name and colored labeling tape* (same color as used above).
5.3 Wash/Analyze Specimen
Note: Always use sterile technique during specimen processing.
-
1.
Allow the semen specimen to liquefy completely for ~20 min in a 37 °C incubator before processing.
Note: Occasionally, samples do not liquefy properly and remain too viscous to pass through the gradient. Add 5 mg of chymotrypsin to the viscous sample ~5–10 min before layering to increase motile sperm yields.
-
2.
Using a sterile transfer pipette, place a few drops of the patient’s semen sample into a conical cup. Place ~5 μL of the sample onto a sperm counting chamber and microscopically verify that there is motile sperm before proceeding with the wash (this sample can also be used for the prewash analysis).
-
3.
Measure the total semen volume using a sterile 2 mL serological pipette.
-
4.
Gently layer no more than 3 mL* of liquefied semen onto the upper phase.
*Note: If the sample volume is greater than 3 mL, it is necessary to split the specimen into two tubes for processing. Process the second tube using the same procedure that was used for the first tube. Combine the second tube with the first tube during step #11 after adding HTF media.
-
5.
Centrifuge for 20 min at 1600 rpm (Fig. 14.1).
-
6.
While the specimen is in the centrifuge, perform a prewash CASA analysis. Perform CASA analysis according to the “Routine Semen Analysis” protocol and record the results on the worksheet.
Note: While examining the specimen, pay particular attention to any extraneous round cells, debris, and bacteria that are present. If round cells are greater than or equal to 1.00 M/mL, perform an Endtz test immediately. A positive Endtz test should be reported to the appropriate medical personnel as soon as possible. The Endtz result should also be written on the tube’s outer label at the end of the wash procedure before handing the specimen to the patient.
-
7.
After the specimen has centrifuged, remove the supernatant without disturbing the pellet. Using a sterile long pasteure pipette carefully remove the seminal plasma, upper interphase (raft “a”), upper (40%) colloid layer, and the lower interphase “raft b”). Leave the majority of the 80% colloid layer in place and discard the aspirated material.
-
8.
Using another clean pasteure pipette remove the soft pellet by direct aspiration (maximum 0.5 mL) from the bottom of the tube beneath the lower (80%) colloid layer into the soft. Avoid contaminating the pasteure tip aperture with the residual seminal plasma/raft material.
-
9.
Transfer the pellet to a clean 15 mL conical tube.
-
10.
Using a serological pipette, add 2 mL of HTF media and resuspend the pellet by pipetting the sample gently up and down until the sperm pellet is properly mixed into the sample.
-
11.
Centrifuge the resuspended sample for 7 min at 1600 rpm (Fig. 14.2).
-
12.
Repeat step 7 above (Fig. 14.3).
-
13.
Resuspend the final pellet (Fig. 14.4) using 0.5 mL of HTF media with a 2 mL serological pipette. Note the volume of the sample. Leave a small droplet (~20 μL) in a labeled conical cup for the post-wash analysis. Subtract this volume from the volume noted above and record on the patient worksheet (Fig. 14.5).
Fig. 14.4 -
14.
Seal the tube using tamper-evident tape, label it with the premade label, and place it in the incubator until the patient arrives. Show the color-coded tube to the patient and have the patient verify the couple’s names, medical record numbers, and date. Place the sample in a brown paper bag and hand it to the patient. Be sure the patient signs the specimen pick-up form and presents appropriate identification. The patient should carry the specimen to gynecologist for the insemination. The gynecologist determines whether or not the sperm count and motility are sufficient for insemination. If no motile sperm are found on the post-wash specimen, page the gynecology nurse prior to releasing specimen.
Note: Always look at the post-wash specimen on a sperm counting chamber before releasing it to the patient. Notify the inseminator immediately if bacteria are present. If there is a positive Endtz test, report the result to the nurse as soon as possible and write it on the outside label of the tube before handing it to the patient. If the prewash Endtz is positive and the post-wash round cell count is less than 1 M/mL, note the round cell count on the outside label of the tube.
-
13.
Perform a post-wash CASA analysis according to the “Routine Semen Analysis” protocol and record the results on the patient worksheet. Page the nurse with the patient name, clinic number, total motile sperm, Endtz value (if necessary), and any other pertinent information.
-
14.
Record appropriate information (below) on the “Artificial Insemination by Husband” form:
-
(a)
MRN
-
(b)
Date of insemination
-
(c)
Total motile post-wash sperm
-
(d)
Wash type (e.g., gradient)
-
(e)
Insemination performed (Gyn nurse)
-
(f)
Comments (e.g., positive Endtz, agglutination, high viscosity)
-
(g)
Tech initials
-
(a)
-
15.
After checking for technical and clerical errors, enter the results and print the final report. Check the final report to ensure the accuracy of the final results.
Note: Immediately correct any inaccurate results.
6 Procedural Notes
-
A.
It is important to use sterile plasticware and glassware during the sperm wash procedure.
-
B.
Each patient specimen should be kept in a separate specimen rack during the time of processing.
-
C.
Processing of patient specimen(s) should be started and completed by a single technologist. In rare cases, when a second technologist is called to help during the processing, the patient’s paperwork should be reverified by the assisting technologist.
7 Tips on How to Maximize the Yield from Density Gradient
-
A.
Make sure you have all components of the gradient brought to 37 °C temperature before use. Besides avoiding a “cold shock” to the spermatozoa, condensation on the media bottles disappears allowing for better inspection of the bottles for contamination. Any bottle whose contents appear in any way cloudy or hazy should not be used.
-
B.
Do not use the same pipette in more than one bottle of media.
-
C.
Density gradient components are air-buffered. Prolonged exposure to a 5 % CO2 environment will alter the pH of these products, which may in turn affect their nature and performance.
-
D.
For highly viscous semen add 5 mg of chymotrypsin to the ejaculate 10 min before it is placed on top of the gradient increases motile sperm yields without any measurable damage to the motile sperm.
-
E.
Do not overload the gradient. The volume of semen in this case is less important than the absolute number of sperm placed on the gradient. Usually, a maximum number should be around 120 million cells. Overloading the gradient will result in a phenomenon called “rafting”—this aggregation of desirable, as well as undesirable, components of the semen will be created and will be present in the post-centrifugation pellet.
-
F.
Always use the gradient within 1 h after creating it—eventually the two phases over time blend into each other and a sharp interface will not exist.
-
G.
To optimize the number of motile sperm, avoid contamination with the seminal plasma raft “a” or raft “b”, or the upper and lower layers.
-
H.
Use a long stem preferably a 9” Pasteure pipette to carefully aspirate the soft pellet at the bottom of the tube beneath the 80% layer.
-
I.
Transfer the final soft pellet into a fresh 15 mL conical tube for second step of centrifugation.
References
Beydola T, Sharma RK, Lee W, Agarwal A. Sperm preparation and selection techniques. In: Rizk B, Aziz N, Agarwal A, Sabanegh E, editors. Male infertility practice. New Delhi: Jaypee Brothers Medical Publishers; 2012.
Agarwal A, Allamaneni S. Artificial insemination. Section 6: infertility and recurrent pregnancy loss. Clinical reproductive medicine and surgery: Tommaso Falcone and William Hurd. Elsevier publishers.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Cleveland Clinic
Cleveland Clinic

Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Agarwal, A., Gupta, S., Sharma, R. (2016). Sperm Preparation for Intrauterine Insemination Using Density Gradient Separation. In: Agarwal, A., Gupta, S., Sharma, R. (eds) Andrological Evaluation of Male Infertility. Springer, Cham. https://doi.org/10.1007/978-3-319-26797-5_14
Download citation
DOI: https://doi.org/10.1007/978-3-319-26797-5_14
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-26795-1
Online ISBN: 978-3-319-26797-5
eBook Packages: MedicineMedicine (R0)