Abstract
Human semen is a complex mixture of motile and immotile sperm, precursor germ cells, cellular debris, and leukocytes. For assisted reproductive technology (ART) procedures, development of efficient sperm preparation protocols capable of separating motile spermatozoa from cellular debris and seminal plasma is essential. Once sperm is separated from seminal plasma, it can undergo capacitation which is the prerequisite for fertilization. Routine sperm separation protocols vary from simple wash and centrifugation to swim-up or separation on double density gradient. From this list, double density gradient separation is most common in routine sperm preparation and better than other protocols in terms of total recovery and motility. Developments of sperm separation protocols based on the electrostatic charges on sperm surface have been successful in obtaining spermatozoa with reduced apoptotic marker proteins and in trials which showed better outcomes. Since the development of intracytoplasmic sperm injection (ICSI), specific sperm selection protocols were developed to successfully obtain sperm from severely oligozoospermic semen samples, retrograde ejaculation, and from testicular or epididymal sources. Some other sperm selection processes using microfluidic system, magnetic cell sorter using Annexin V columns, and hyaluron binding of spermatozoa have shown improved clinical outcomes.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Developing an efficient method of sperm separation technique is essential for the successful fertilization using assisted reproductive technologies. Human semen sample is a complex mixture of variable amount of cellular debris, germ cells, and leukocytes and does not have the capacity to fertilize the oocyte instantly after ejaculation. It has to acquire the capacity to be acrosome reacted and fertilize the oocytes in the female genital tract by undergoing a series of complex physiological and biochemical changes termed capacitation [1–2]. It involves the removal of sterols (e.g., cholesterol) and non-covalently bound glycoproteins from sperm cell surfaces. This renders the sperm cell surface receptors to be accessible with an increase in the fluidity of sperm membrane and permeability of Ca++. Due to increased permeability of Ca++, there is an increase in intracellular cAMP which aids sperm to undergo hyperactivation [1,2,3,4]. In vivo sperm undergoes the process of capacitation after ejaculation by swimming out from seminal plasma into cervical mucus, but in vitro, to acquire capacitation, sperm has to be removed from seminal plasma by washing it out using different protocols as described in this chapter. It has been shown that prolonged exposure of sperm to seminal plasma (>60 min) is detrimental and hampers the fertilization potential [5] and traces of seminal plasma present in the re-suspended sperm in the media can be harmful [6].
Therefore, when sperm sample has to be used for clinical purposes, like intrauterine insemination (IUI), therapeutic donor insemination (TDI), in vitro fertilization (IVF), or intracytoplasmic sperm injection (ICSI), it is important to remove the semen from the seminal plasma as soon as sample liquefies using different washing protocols with an effort to put least trauma to the sample during preparation. Processed sperm sample has to be re-suspended in a suitable culture medium which is capable of sustaining capacitation.
1 Simple Wash Procedure
This is one of the earliest methods to prepare sperm, where semen samples are diluted with Hepes-HTF medium containing 5 mg/ml of human serum albumin (HSA) using centrifugation.
Procedure
-
1.
Mix the semen sample well.
-
2.
Dilute the entire semen sample (1:2) with Hepes-HTF medium with serum to dilute seminal plasma.
-
3.
Transfer diluted sample into more tubes, if total volume is more than 3 ml. There should not be more than 3 ml of sample per tube.
-
4.
Centrifuge at 300–500 × g for 5–10 min.
-
5.
Carefully aspirate and discard the supernatants.
-
6.
Re-suspend the combined sperm pellets if more than one tube was used into one tube in approximately 1 ml of medium by gentle pipetting.
-
7.
Centrifuge again at 300–500 × g for 3–5 min.
-
8.
Carefully aspirate and discard the supernatant.
-
9.
Resulting pellet can be re-suspended in 0.3–0.50 ml of medium depending upon the pellet size.
Although this procedure tends to have a good recovery, other cells, dead spermatozoa, and leucocytes can also accumulate and generate copious amount of reactive oxygen species [7] that can compromise sperm function and DNA integrity. It is therefore not a method of choice. However, where recovery of a few motile sperm is required for achieving fertilization using intracytoplasmic sperm injection (ICSI), it can be useful.
2 Direct Swim-Up Method
This method is devised based on the motile sperm’s ability to swim out of seminal plasma into the sperm wash buffer, typically Hepes-buffered HTF with 5 mg/ml HSA. Liquefied sample can be washed once by diluting it with sperm wash buffer, and resultant pellet can be layered under medium in a culture tube or medium can be gently layered over the pellet and left for 30–45 min, so that motile sperm can swim into the medium. However, wash and centrifugation prior to swim-up is not recommended due to the possibility of peroxidative damage to the sperm membranes and due to accumulation of leukocytes and cellular debris in the resultant pellet after centrifugation [8]. Therefore, a direct swim-up method using liquefied semen is recommended [9, 10]. We describe here the direct swim-up technique:
-
1.
Put 2.5 ml of Hepes-HTF medium with 5 mg/ml HSA in three to four 12 × 75 mm 5 ml sterile tubes.
-
2.
Place approx. 0.5 ml aliquots of liquefied semen into the bottom of these tubes. Semen with normal to high counts may require several tubes.
-
3.
Mark the meniscus on the surface of the tube where semen sample meets with the media with a permanent marker.
-
4.
Place caps tightly on the tubes, and incubate for 60 min at 37 °C in an incubator. Tube should be tilted at 45°. This helps in good recovery of motile sperm.
-
5.
Time of incubation should be varied between 30 and 90 min due to the initial count and motility of the specimen, i.e., normal specimens usually only require 30 min to achieve a good concentration in the media layer.
-
6.
Remove the upper layer of media above the meniscus—take care not to aspirate any semen into the pipette. Place the aspirate into a sterile 15 ml conical tube. Repeat for all tubes. Put approximately 4 ml of Hepes-HTF medium with 5 mg/ml HSA.
-
7.
Centrifuge 300–500 × g for 10 min. Remove the supernatant using a sterile Pasteur pipette. Gently dislodge the pellet by tapping. Add 3 ml of medium and centrifuge again for 5 min at 300–500 × g.
-
8.
Re-suspend final pellet to 0.2–0.5 ml with media and assess count and motility.
There is a simple variant of this method where organ culture dish (OCD) can be used successfully and duration of the swim-up can be reduced to 15 min [11]. 0.7 ml of unwashed liquefied semen was transferred under the 2.5 ml of Hepes-HTF medium with HSA in the center well of organ culture dish and incubated at 37 °C for 15 min. Approximately 2 ml of the medium containing motile sperm was removed by a fine tip pipette directed against the edge of the center well. The aspirated medium is centrifuged at 300 × g for 7 min, and the resulting pellet was re-suspended in 1 ml of media and washed again for 5 min at 300 × g, and pellet is reconstituted in 0.5 ml, and then count and motility are assessed. This method works well with good recovery and with frozen sperm as well. It is less time-consuming as compared to multiple tube incubation.
Direct swim-up technique yields good recovery of motile sperm if sperm count and motility are adequate and semen sample is free from cellular contaminants and leukocytes and is successfully used for sperm preparation for IVF and IUI.
3 Sperm Preparation Using Discontinuous Density Gradients
This method is most popular and widely used in ART laboratories. It provides best and clean separation of spermatozoa from other cellular debris and contaminants of semen. It is easy to standardize and results are consistent. This method separates spermatozoa based on the density and specific gravity. Mature and morphologically normal spermatozoa have a density of >1.12 g/ml, whereas immature and morphologically abnormal spermatozoa density varies between 1.06 and 1.09 g/ml. Several years ago a commercially available gradient Percoll which was available from Pharmacia Biotech, Uppsala, Sweden, was extensively used for sperm preparation. Percoll is colloidal silica coated with polyvinylpyrrolidone, and 80% (v/v) of it is about 1.10 g/ml. Due to this density, only highly mature spermatozoon could penetrate through the 80% layer which allowed the separation of most mature and morphologically normal spermatozoa. However, Percoll is not recommended anymore for clinical use, and since then various commercial gradients are available now that can be safely and successfully used. Some of the most popular name brands are Isolate from Irvine Scientific (Santa Ana, CA) and PureSperm from Nidacon International, Göteborg, Sweden. These products are tested and found to be as good as Percoll [12]. Here we describe the method of sperm separation using this method [10]:
-
1.
Perform sperm count and motility assessment on the semen sample after 30 min after liquefaction.
-
2.
Transfer 2 ml of 80% PureSperm gradient in a Falcon polystyrene (#2095) 15 ml tube. Do not use polypropylene tube as it may be toxic to sperm.
-
3.
On top of it, layer 2 ml of 40% gradient gently.
-
4.
Pipette same volume of liquefied semen on top of the gradients by touching the semen pipette tip to the top of the 40% gradient. If semen volume is more than 2 ml, make another tube with 80%:40% gradient.
-
5.
Centrifuge at 400 × g for 15 min using a swinging bucket rotor.
-
6.
Aspirate the gradient part without disturbing the pellet. Remove the pellet using a wide bore sterile pipette to a clean tube containing 4 ml of sperm wash buffer, and centrifuge it for 10 min at 200 × g.
-
7.
Remove the supernatant using a fine tip aspiration pipette. Add 2 ml of sperm wash buffer and repeat the centrifugation at 200 × g for 5 min.
-
8.
Re-suspend the washed pellet with 500–1000 μl of sperm wash buffer.
For viscous sample it is difficult to obtain good yield of motile spermatozoa. It is recommended therefore to take few measures to reduce the viscosity before proceeding to sperm preparation. Specimen viscosity can be reduced to some extent by diluting the sample with an equal volume of sperm wash buffer and mixing it using sterile pipette. Let the sample to sit for 5–10 min, and remove the settled debris from the bottom using a sterile Pasteur pipette. Any viscous mass that is still floating in the medium can be carefully removed using a fine bore Pasteur pipette.
In recent years growing attentions are directed to apoptotic markers as indicators of sperm integrity [12,13,14,15,16,17]. Some studies have compared apoptosis in prepared sperm by swim-up and density gradient centrifugation [18]. Hence, there is a quest to develop sperm preparation protocols that involve minimum trauma because the shearing forces inflicted due to centrifugation stimulate ROS generation in human sperm samples [8, 19].
4 Sperm Selection Based on Electrostatic Charges
Some novel methods of sperm selection were developed utilizing the electrokinetic properties of sperm surface membrane. Mature sperm typically exhibit a net negative charge of −16 to −20 mv [20]. This high negative charge on the sperm surface is due to high levels of sialic acid residues which play a role in sperm capacitation and the formation of binding bridges between sperm membrane proteins and oocytes [21]. A procedure of sperm selection based on this property of net negative charge on sperm surface membrane will result in the isolation of more mature, viable, motile, and morphologically normal sperm which are free of DNA damage [22, 23]. Based on these characteristics, two methods have been developed for sperm separation. A simple version is Zeta method [24,25,26] and a more complex method that separates sperm electrophoretically [27, 28].
5 Zeta Method of Sperm Selection
This method is described in detail in [26]. It is recommended that this method should be carried out immediately after semen liquefaction because as more time progresses sperm starts to lose its electrostatic charges. In order to perform this, use polystyrene 15 ml centrifuge tube. It will be better if tubes are checked before to have adequate positive charge and volt meter read 204 kv per square inch. Sperm should be washed using a double density gradient method. Put 0.1 ml of prepared sperm into the tube, and dilute it with 5 ml Hepes-HTF medium without serum. Hold the tube using the cap (never touch anywhere else), and put inside a latex glove with the cap part exposed only. Rotate the tube two to three times gently by holding the cap in clockwise direction, and then let it incubate for a minute which will allow the charged sperm to adhere on the wall of the tube. After the incubation slowly invert the tube to drain off all non-adherent sperm. Centrifuge the tube at 300 × g for 5 min, and then place the tube upside down on a tissue paper to blot off the excess liquid at the mouth of the tube. Put 0.2 ml of Hepes-HTF medium containing 3% or more of serum slowly so that it can trickle down at the bottom detaching the adherent sperm. Pour the medium again on the side wall using a fine tip pipette, and collect the medium at the bottom which has detached sperm. Estimate the count and motility. Sperm selection using zeta methods has increased higher probability in fertilization, implantation, and pregnancy [29, 30].
6 Electrophoretic Sperm Separation
Sperm is separated based on the size and charge using electrophoresis [27]. A special device consisting of four chambers is used. There are two inner and two outer chambers. Two polyacrylamide membranes with a pore size of 15 kDA separate the inner and outer chambers. Although free flow of water, small molecules, and ions can occur between the inner and outer chambers, the cell suspension is retained within the inner chamber. A platinum-coated titanium mesh electrode is present in the outer chambers. Two 12 v pumps in each electrode chamber circulate the buffer at 1.6 l/min. Each inner chamber has a capacity of 400 μl. One is an inoculation chamber into which semen is deposited, and the other is a collection chamber containing only the buffer. The two inner chambers are separated by a 5 μM polycarbonate membrane. The pore size allows movement of sperm but not the larger leukocyte and precursor germ cells that are commonly present in the semen sample.
Semen sample and buffer are loaded in the two reservoirs and allowed to equilibrate for 5 min before the electric field is applied. The separation and electrode buffer is comprised of 10 mM Hepes, 30 mM Nacl, and 0.2 M sucrose. pH of the buffer was adjusted to 7.4 with an osmolarity of 310 osm/l. The samples were run at the constant applied current of 75 mA and a variable voltage of between 18 and 21 V at room temperature. Purified sample is collected and count, motility, and progression are estimated. Isolated sample collected after this method contained motile, morphologically normal sample and exhibited reduced level of DNA damage. It is also free from contaminating leukocytes and germ cells. This is a quick method that does not require any centrifugation and recovery which is similar to commonly applied methods like density gradient separation or swim-up.
7 Sperm Separation Using Microfluidic Sperm Sorter
In recent years microfluidic sperm sorters (MFSSs) are developed that can be used to separate motile sperm from immotile sperm and from other cellular debris based on fluid dynamics [31,32,33]. This device has sample inlets, outlets, and sorting channels and a novel passively driven pumping system that provides a steady flow of liquids. These well-designed two parallel laminar flow channels separate motile spermatozoa from immotile spermatozoa. It has been shown that sperm motility and morphology can be increased twofold using this method [32]. It requires no external power or controls. This system does not require any centrifugation and can sort out motile sperm without DNA damage [34].
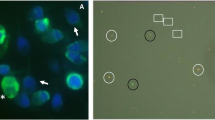
8 Sperm Preparation Using Magnetic-Activated Cell Sorting
The principle behind this method is to bind sperm showing apoptotic marker proteins using Annexin V. Consequently, sperm prepared by this method show reduced level of apoptotic marker proteins, e.g., Fas, phosphatidylserine, Bcl-XL, p53, etc., as compared to routine sperm preparation protocols that require centrifugation [35, 36]. Density gradient-separated sperm is incubated with Annexin V-conjugated microbeads (Miltenyi Biotec, Auburn, CA) for 15 min at room temperature (100 μl microbeads for every ten million sperm) to form a suspension. The suspension is then loaded on a separation column containing a coated-cell matrix containing iron balls which are in turn fitted in a magnet (MiniMACS, Miltenyi Biotec). The spermatozoa with apoptotic markers get retained in the separation column (Annexin-positive fraction), and those with intact membranes are eluted through the column (Annexin-negative). Fluorescence-labeled dye and flow cytometry have confirmed that these sperm have significantly reduced levels of apoptotic markers [37]. It is suggestive therefore that with the use of this method, there is high probability of increase in fertilization potential as revealed in some trials [38, 39].
9 Sperm Selection Using Hyaluron Binding
Sperm selection based on its ability to bind hyaluron has shown improved implantation [40] and clinical pregnancy [41]. This technique is based on the concept that spermatozoa bind to hyaluron has completed spermatogenesis. During the process of spermiogenesis, there are alterations in plasma membrane and appearance of hyaluron binding sites. Human sperm that bind to hyaluron appeared to have low DNA fragmentation and normal morphology and exhibit least aneuploidies and are compared to the sperm that bind to zona pellucida which is important for successful fertilization [42]. This sperm selection method can be successfully performed in conjunction with ICSI in specially designed dishes with hyaluron droplets. Sperm head can bind to the hyaluron dots and can be easily picked up for injection in the oocytes.
10 Retrograde Ejaculation Sperm Processing
Azoospermia with severely reduced semen volume can be associated with retrograde ejaculation, which is a condition where the sperm are pushed into the bladder (retrograde ejaculation), rather than out through the urethra (antegrade ejaculation). If large numbers of sperm pass into the bladder, then the sperm can be harvested from the urine and used for ART procedures [10]. Patient should abstain from ejaculation for 2–3 days.
-
1.
For 2 days prior, patient should start taking sodium bicarbonate (Alka Seltzer) 650 mg by mouth four times per day and pseudoephedrine (Sudafed) 60 mg by mouth two times per day with an 8 oz of glass before collection of specimen. No alcohol or other drugs (other than those that are necessary) should be taken.
-
2.
On morning of test, patient should urinate, and then take two sodium bicarbonate tablets, and drink one to two glasses of water.
-
3.
The bladder should be emptied approximately 1 h prior to collecting the specimens.
The patient should use masturbation to produce an antegrade semen specimen (if possible). Within 5 min after orgasm, the patient should urinate into another specimen cup(s). Both the antegrade ejaculate (if any) and the post-ejaculatory urine should be presented to the lab. These patients should collect all specimens at the laboratory, so that the sperm can be isolated from the urine quickly.
-
1.
Aliquot all urine into 15 ml sterile conical tubes—approximately 10–15 ml per tube.
-
2.
Record total volume of urine specimen.
-
3.
Centrifuge tubes at 550 × g for 10 min. Discard supernatant.
-
4.
Re-suspend pellets in sperm wash buffer approximately 1–2 ml per tube, depending upon the size of pellet (large pellet, 2–3 ml). Consolidate all aliquots into one 15 ml conical centrifuge tube. If motility is adequate, it can be processed using density gradient. Remove 10 μl and do a sperm count, and assess the motility and progression following semen analysis method.
If an antegrade specimen is obtained, 10 μl of the semen specimen is assessed for count, motility, and progression as per standard semen analysis protocol.
11 Sperm Preparation from Epididymal Aspirates and Testicular Biopsies
Since the advent of ICSI, it is now possible to obtain sperm from men using epididymal sperm aspiration or testicular biopsy, if there is no sperm in the ejaculate due to obstructive or nonobstructive azoospermia. Epididymal aspirates are the suspension of cells usually obtained with fine needles from the epididymis. If epididymal aspirates contain some motile spermatozoa, it can be processed using double density gradient successfully [43]. However, if majority of spermatozoa in the epididymal aspirates are immotile, density gradient separation will be inefficient, and then a simple wash technique will be useful. Often these samples have very poor motility, and incubating sperm with pentoxifylline (2 mg/ml) in sperm wash buffer is quite helpful.
12 Sperm Preparation from Testicular Biopsies
Testicular biopsies should be transported to laboratory in a sterile container containing sufficient amount of sperm wash buffer (Hepes-HTF with 5 mg/ml HSA).
-
1.
The biopsy is removed from the container it comes in, using sterile forceps, thoroughly rinsed in sperm wash buffer to remove the blood, placed on the lid of a 60 mm dish in a small drop of sperm wash buffer, and thoroughly minced with a pair of disposable scalpels. Sometimes using a pair of 26 gauge needles bent to an angle of 90° attached with 1 ml disposable syringe is very helpful in finely teasing the seminiferous tubules [10, 44]. Once the tissue is thoroughly minced, use the bottom portion of the 60 mm dish, and place it over the minced tissue, and using fingers inside the lid, press it over at several places to squeeze out the sperm from the tubules. A twisting motion should not be used, as this may break the sperm head from the tail.
-
2.
Once the tissue is well squashed, the lid is rinsed with sperm wash buffer; the sample is collected into a 15 ml centrifuge tube and centrifuged at 800 × g for 5 min.
-
3.
The supernatant is removed and discarded and the sample is suspended in 0.5–1 ml of sperm wash buffer depending on sample size. Vortex the suspension for 20–30 seconds to dislodge spermatozoa from the cells. Take an aliquot (5–10 μl), and put it in 20–30 μl of pentoxifylline solution (2 mg/ml in Hepes-HTF + HSA) in a dish lid covered with oil and kept at 37 °C. Thoroughly examine the droplet under inverted microscope under high power for the presence of a motile sperm. If motile sperm is seen, then sperm preparation can be successfully used. It is always recommended to cryopreserve the sample for future use.
13 Conclusions
Routine sperm separation protocols have evolved from simple wash to gradient separation over the years, and the general consensus is that both swim-up and gradient protocols work equally well, although gradient protocol is preferable due to efficient separation of motile sperm even from suboptimal samples [45, 46]; nevertheless, a Cochrane database system review has not found any difference on the clinical outcome by different sperm preparation protocols [47]. There have been several advances made in sperm separation utilizing electrostatic potential and some novel microfluidic procedures with sperm showing significantly reduced apoptotic markers. However, these technologies are still not in routine use. In future, knowledge gleaned from varying DNA methylation patterns of spermatozoa that affect embryo development [48] and sperm RNA analysis [49] may be helpful in devising specific protocols that may help in selecting spermatozoa for better clinical outcome.
References
De Jonge C. Biological basis for human capacitation. Hum Reprod Update. 2005;11:205–14.
Ikawa M, Inoue N, Benham AM, Okabe M. Fertilization: a sperm’s journey to and interaction with the oocyte. J Clin Invest. 2010;120:984–94.
Austin CR, Braden AW. Passage of the sperm and the penetration of the egg in mammals. Nature. 1952;170:919–21.
Yanagimachi R. Mammalian sperm reaction: where does it begin before fertilization? Biol Reprod. 2011;85:4–5.
Rogers BJ, Perrault SD, Bentwood BJ, McCarville C, Hale RW, Soderdahl DW. Variability in the human-hamster in vitro assay for fertility evaluation. Fertil Steril. 1983;39:204–11.
Kanwar KC, Yanagimachi R, Lopata A. Effects of human seminal plasma on fertilizing capacity of human spermatozoa. Fertil Steril. 1979;31:321–7.
Aitken RJ, Bukingham DW, Bridle J, Gomez E, Baker HW, Irvine DS. Analysis of sperm movement in relation to the oxidative stress created by leukocytes in washed sperm preparation and seminal plasma. Hum Reprod. 1995;10:2061–71.
Aitken RJ, Clarkson JS. Significance of reactive oxygen species and antioxidants in defining the efficacy of sperm preparation techniques. J Androl. 1988;9:367–76.
Mortimer D. Sperm recovery techniques to maximize fertilizing capacity. Reprod Fertil Dev. 1994;6:25–31.
WHO. Laboratory Manual for the examination and processing of human semen. 5th ed. Geneva: World Health Organization, Department of Reproductive Health and Research; 2010.
Yin HZ, Srivastava RK, Bar-Ami S, Seibel MM. An unwashed sperm rise method for preparing fresh or frozen sperm using organ culture dishes. Fertil Steril. 1997;68(Suppl 1):S56–7.
Centola GM, Herko R, Andolina E, Weisensel S. Comparison of sperm separation methods: effect on recovery, motility, motion parameters, and hyperactivation. Fertil Steril. 1998;70:1173–5.
Sakkas D, Mariethoz E, St John JC. Abnormal sperm parameters in humans are indicative of an abortive apoptotic mechanism linked to the fas-mediated pathway. Exp Cell Res. 1999;251:350–5.
Ricci G, Perticarari S, Fragonas E, Giolo E, Canova S, Pozzobon C, et al. Apoptosis in human sperm: its correlation with semen quality and the presence of leukocytes. Hum Reprod. 2002;17:2665–72.
Sakkas D, Seli E, Bizzaro D, Tarozzi N, Manicardi GC. Abnormal spermatozoa in ejaculate: abortive apoptosis and faulty nuclear remodeling during spermatogenesis. Reprod Biomed Online. 2003;7:428–32.
Oehninger S, Morshedi M, Weng SL, Taylor S, Duran H, Beebe S. Presence and significance of somatic cell apoptosis markers in human ejaculated spermatozoa. Reprod Biomed Online. 2003;7:469–76.
Agarwal A, Saleh RA, Bedaiwy MA. Role of reactive oxygen species in the pathophysiology of human reproduction. Fertile Steril. 2003;79:829–43.
Ricci G, Perticarari S, Boscolo R, Montico M, Guaschino S, Presani G. Semen preparation methods and sperm apoptosis: swim-up versus gradient-density centrifugation technique. Fertil Steril. 2009;91:632–8.
Shekarriz M, Thomas AJ Jr, Agarwal A. Effects of time and sperm concentration on reactive oxygen species formation in human semen. Arch Androl. 1995;34:69–75.
Isijima SA, Okuno M, Mohri H. Zeta potential of human X- and Y-bearing sperm. Int J Androl. 1991;14:340–7.
Calzada L, Salazar EL, Pedron N. Presence and chemical composition of glycoproteic layer on human spermatozoa. Arch Androl. 1994;33:87–92.
Aitken RJ, Hanson AR, Kuczera L. Electrophoretic sperm isolation; optimization of electrophoresis conditions and impact on oxidative stress. Hum Reprod. 2011;26:1955–64.
Ainsworth C, Nixon B, Aitken RJ. The electrophoretic separation of spermatozoa: an analysis of genotype, surface carbohydrate composition and potential for capacitation. Int J Androl. 2011;34(5 Pt 2):e422–34.
Chan PJ, Jacobson JD, Corselli JU, Patton WC. A simple zeta method for sperm selection based on membrane charge. Fertil Steril. 2006;85:481–6.
Kam TL, Jacobson JD, Patton WC, Corselli JU, Chan PJ. Retention of membrane charge attributes by cryopreserved-thawed sperm and zeta selection. J Assist Reprod Genet. 2007;24:429–34.
Simon L, Ge SQ, Carrell DT. Sperm selection based on electrostatic charge. Methods Mol Biol. 2013;927:269–78.
Ainsworth C, Nixon B, Aitken RJ. Development of a novel electrophoretic system for the isolation of human spermatozoa. Hum Reprod. 2005;20:2261–70.
Ainsworth C, Nixon B, Jansen RP, Aitken RJ. First recorded pregnancy and normal birth after ICSI using electrophoretically isolated spermatozoa. Hum Reprod. 2007;22:197–200.
Kheirollahi-Kouhestani M, Razavi S, Tavaleee M, Deemeh MR, Mardani M, Moshtaghian J, Nasar-Esfahani MH. Selection of sperm based on combined density gradient and zeta method may improve ICSI outcome. Hum Reprod. 2009;24:2409–16.
Deemeh MR, et al. The first report of successful pregnancy after ICSI with combined DGC/Zeta sperm selection procedure in a couple with eleven repeated fail IVF/ICSI cycles. Int J Fertil Steril. 2010;4:41–3.
Cho BS, Schuster TG, Zhu X, Chang D, Smith GD, Takayama S. Passively driven integrated microfluidic system for separation of spermatozoa. Anal Chem. 2003;75:1671–5.
Schuster TG, Cho B, Keller LM, Takayama S, Smith GD. Isolation of motile spermatozoa from semen samples using microfluidics. Reprod Biomed Online. 2003;7:75–81.
Wu JM, Chung Y, Belford KJ, Smith GD, Takayama S, Lahann J. A surface modified sperm sorting device with long-term stability. Biomed Microdevices. 2006;8:99–107.
Shirota K, Yotsumoto F, Itoh H, Obama H, Hidaka N, Nakajima K, et al. Separation efficiency of a microfluidic sperm sorter to minimize sperm DNA damage. Fertil Steril. 2016;105:315–21.
Sakkas D, Moffatt O, Manicardi GC, Mariethoz E, Tarozzi N, Bizzaro D. Nature of DNA damage in ejaculated human spermatozoa and the possible involvement of apoptosis. Biol Reprod. 2002;66:1061–7.
Cayli S, Sakkas D, Vigue L, Demir R, Huszar G. Cellular maturity and apoptosis in human sperm: creatine kinase, caspase-3 and Bcl-XL levels in mature and diminished maturity sperm. Mol Hum Reprod. 2004;10:365–72.
Lee TH, Liu CH, Shih YT, Tsao HM, Huang CC, Chen HH, et al. Magnetic-activated cell sorting for sperm preparation reduces spermatozoa with apoptotic markers and improves the acrosome reaction in couples with unexplained infertility. Hum Reprod. 2010;25:839–46.
de Polak FE, Denaday F. Single and twin ongoing pregnancies in two cases of previous ART failures after ICSI performed with sperm sorted using annexin V microbeads. Fertil Steril. 2010;94:351–8.
Rawe VY, Boudri HU, Alvarez SC, Carro M, Papier S, Nodar F. Healthy baby born after reduction of sperm DNA fragmentation using cell sorting before ICSI. Reprod Biomed Online. 2010;20:320–3.
Parmegiani L, Cognigni GE, Ciampaglia W, Pocognoli P, Marchi F, Filicori M. Efficiency of hyaluronic acid (HA) sperm selection. J Assist Reprod Genet. 2010;27:13–6.
Worrilow KC, Eid S, Woodhouse D, Perloe M, Smith S, Witmyer J, et al. Use of hyaluron in the selection of sperm for intracytoplasmic sperm injection (ICSI): significant improvement in clinical outcomes-multicenter, double-blinded and randomized control trial. Hum Reporod. 2013;28:306–14.
Huszar Z, Jakab A, Sakkas D, Ozenci CC, Cayli S, Delpiano E, et al. Fertility testing and ICSI sperm selection by hyaluronic acid binding: clinical and genetic aspects. Reprod Biomed Online. 2007;14:650–63.
Ord T, Marcello E, Patrizio P, Balmaceda JP, Silber SJ, Asch RH. The role of the laboratory in the handling of epididymal sperm for assisted reproductive technologies. Fertil Steril. 1992;57:1103–6.
Muller CH, Pagel ER. Recovery, isolation, identification, and preparation of spermatozoa from human testis. Methods Mol Biol. 2013;927:227–40.
Carrell DT, Kuneck PH, Peterson CM, Hataska HH, Jones KP, Campbell BF. A randomized, prospective analysis of five sperm preparation techniques before intrauterine insemination of husband sperm. Fertil Steril. 1998;69:122–6.
Facio CL, Previato LF, Machado-Paula LA, Matheus PC, Araujo EF. Comparison of two sperm processing techniques for low complexity assisted fertilization: sperm washing followed by swim-up and discontinuous density gradient centrifugation. JBRA Assist Reprod. 2016;20:206–11.
Boomsma CM, Heineman MJ, Cohlen BJ, Farquhar C. Semen preparation techniques for intrauterine insemination. Cochrane Database Syst Rev. 2007;4:CD004507.
Hammoud SS, Nix DA, Zhang H, Purwar J, Carrell DT, Cairns BR. Distinctive chromatin in human sperm package genes for embryo development. Nature. 2009;460:473–8.
Ostermeier GC, Goodrich RJ, Diamond MP, Duix DZJ, Krawetz SA. Towards using stable spermatozoal RNAs for prognostic assessment of male factor fertility. Fertil Steril. 2005;83:1687–94.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Srivastava, R.K. (2020). Sperm Separation Protocols. In: Allahbadia, G.N., Ata, B., Lindheim, S.R., Woodward, B.J., Bhagavath, B. (eds) Textbook of Assisted Reproduction. Springer, Singapore. https://doi.org/10.1007/978-981-15-2377-9_90
Download citation
DOI: https://doi.org/10.1007/978-981-15-2377-9_90
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-15-2376-2
Online ISBN: 978-981-15-2377-9
eBook Packages: MedicineMedicine (R0)