Abstract
Central venous catheters are the most ubiquitously placed device in the critical care environment. With an estimated 500,000 catheters placed per year in the United States alone, this procedure is an integral part of the practice of the competent critical care clinician. With known complications such as bleeding, vascular injury, or pneumothorax, there has been a push in recent times to more safely conduct placement of central venous catheters in an expeditious manner. Procedural ultrasound is a key modality in clinical practice which has mitigated these risks and improved quality of care. In this chapter, we explore the history of the central venous catheter, indications, complications, and the use of ultrasound in clinical applications.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Overview
Central venous catheter (CVC) placement is the most commonly performed procedure in the ICU with over 5 million CVC lines being placed each year in the USA alone. CVC lines first began utilization in early 1966 [1]. Their use and implementation are ubiquitous in the ICU, and routine placement has become a part of many care bundles, including early goal-directed therapy (EGDT) for sepsis . Moreover, CVC lines have become an integral part in the management of the critically ill, with CVP monitoring being a significant factor for placement [2]. They are required for a number of vasopressors, inotropic agents, antibiotics, and medications which may pose a risk of extravasation. The first reported use of ultrasound (US) technology to aid in the cannulation was in 1984. Although initially there was a lack of adoption of this vital technology, a recent survey among resident physicians has found a utilization rate of 90 % in the internal jugular site with US guidance becoming the sine qua non for CVC placement [3, 4]. Prior to the widespread adoption of US technology, clinicians had a significant failure rate using traditional anatomic landmarks with some authors citing a failure rate of 19.4 % [5]. Lastly, even in highly experienced operators, reliance on traditional landmark techniques may result in a sixfold increase in complication rate when more than three attempts are made at vascular access in a given site (Subclavian, Internal Jugular) [6].
2 Review of Ultrasound Technology
Traditional ultrasound techniques include the use of a linear array probe and B-mode (brightness mode) ultrasound. This is in contrast to other types of probes (phased array) and modes (M or motion mode ) used for indications other than CVC placement. The ultrasound machine utilizes a piezoelectric effect to utilize energy along the ultrasound crystal array to create an image of the anatomic structure of interest. Typically frequencies for procedural use operate in the range of 2–15 MHz. Variables that may be controlled include the depth and gain to create a clearer image for CVC placement. Additionally, the views utilized may consist of short axis views, long axis views, or a combination (biplanar) approach [7]. There has been some debate over the superiority of the short axis approach as opposed to the long axis approach for vessel cannulation. However, a prospective randomized study showed that success rates in the short axis group, while higher, were not statistically significant [8]. Although there is less of a difference in short axis vs. long axis techniques , success rates for US vs. traditional landmark techniques are drastically different with one author citing success rates of 93.9 % with US in comparison to 78.5 % using landmarks alone. Further techniques to provide for a more optimal US image of the needle include placing the bevel side down so as to be in the plane of the US transducer and the use of commercially available echogenic needle tips. Lastly, commercial needle guides may be available for utilization to facilitate optimal needle placement with an incidence angle of 30–45°.
3 Indications
Owing to its ubiquitous use in the critical care environment, there are a multitude of indications for the placement of a CVC catheter [9]. Hemodynamic monitoring is one of the most frequent reasons. Interestingly, some complications in SC CVC placement may actually be lower than PICC catheters. One study found that rates of thrombophlebitis were lower in SC CVC catheters when the reason for placement was TPN administration [10]. Common indications for CVC placement are outlined as follows in Table 12.1:
4 Contraindications
Common contraindications for CVC placement are outlined as follows in Table 12.2:
5 Anatomic Locations for Catheterization and Procedure Without US Guidance
Typical anatomic locations for CVC placement include the internal jugular vein, subclavian vein, and femoral vein . Although other sites may be utilized for the placement of peripherally inserted central catheters (PICCs) , their discussion is outside of the purview of this chapter and is discussed elsewhere.
Internal Jugular Site
The internal jugular vein may be found beneath the digastric belly of the sternocleidomastoid muscle . The classic landmarks which delineate the borders of the carotid triangle include the sternocleidomastoid, trapezius, and the clavicle inferiorly. Traditionally, in a nonultrasound approach of the right internal jugular vein, the clinician may palpate the carotid pulse medially with their nondominant hand and insert a smaller finder needle laterally and aim at a 45° needle, inserting it in the direction of the ipsilateral nipple . It is important to initially start higher on the neck for a number of reasons. First, the internal jugular vein courses from a lateral position to the carotid to more of an anterior relationship to the vein as the internal jugular approaches the base of the neck. This relationship predisposes to possible inadvertent cannulation of the carotid artery or hematoma if posterior wall puncture (PWP) occurs. The avoidance of PWP is of tantamount importance in the placement of large bore hemodialysis CVC catheters in this site, owing to the larger dilators that are employed [11–13]. Secondly, the risk of pneumothorax increases as the insertion site moves further toward the base of the neck as the longer cannulation needle may actually penetrate the apex of the lung, which may be extended to the space above the clavicle. Relative advantages of the internal jugular vein for CVC placement include ease of access and readily visible landmarks. Relative disadvantages for CVC placement in this location include pooling of oropharyngeal secretions in intubated patients, difficulty in placing an occlusive dressing, and potential for airway compromise in the event of carotid hematoma. Failure and complication rates for traditional placement techniques in experienced vs. inexperienced operators have been listed as 11.7 % and 17.6 %, respectively [14]. In an observational study conducted in the ED setting, US in the IJ site was still safer in inexperienced operators as opposed to the SC site with a failure rate of 10 %. In that same study, complication rates of hematomas and arterial punctures were listed as 7 % and 2 %, respectively [15, 16]. Moreover, the use of ultrasound has been associated with a higher success rate (93.9 % vs. 78.5 %) and a reduced time for placement when compared with the traditional landmark technique [17–19].
Subclavian Site
The subclavian vein may be found beneath the clavicle at the transition point between the proximal and middle third at the clavicle at the midclavicular line. Of note, the clinician may palpate this site and feel a firmness which signifies the ligament of Halsted. The optimal site of cannulation of the subclavian vein is laterally and inferiorly to this location on the clavicle (Fig. 12.1). After appropriate cleansing, anesthetic placement, and draping, the clinician may enter the skin with the needle at a thirty degree angle. With the nonneedle hand, once the needle is in the skin, the clinician then provides gentle downward pressure over the needle with their thumb and slowly advances toward the sternal notch and the contralateral shoulder. Gentle aspiration is performed until a venous flash occurs. In the event that the clinician directs the needle more caudally, they may encounter a bright red arterial flash. Additionally, great care should be taken as the risk of pneumothorax is significantly higher in this anatomic site. Loss of negative pressure on the syringe may signify entry into the pleural space and subsequent pneumothorax. For patients who are intubated, clinical signs of tension pneumothorax include an increase in peak inspiratory pressures, loss of tidal volumes, or an increase in respiratory rate. Physical examination may reveal jugular venous distention or loss of breath sounds. As with the internal jugular site, failure and complication rates for traditional placement techniques in experienced vs. inexperienced operators with the subclavian site have been listed as 7.5 % and 15 %, respectively [20]. A more detailed study of the subclavian site showed a pneumothorax rate of 2.5 % and an overall complication rate of 5.5 % [21]. Complications listed included tip misplacement, arterial puncture, inability to locate the vessel, and hemothorax. Interestingly, US guidance using either SA or LA approaches in the SC site has failed to show any meaningful reduction in complication rates [22, 23].
Femoral Site
The femoral vein may be located medial to the femoral artery and below the inguinal ligament. Traditionally the clinician thoroughly cleanses the groin, drapes the patient, and anesthetizes the soft tissue. Palpating the femoral pulse, the clinician inserts the needle and syringe medially, in contradistinction to the internal jugular vein which is lateral to the pulse. Of note, it is important to cannulate the vessel below the inguinal crease, as placement above the crease may cause the needle to be inserted inadvertently into the peritoneum. Moreover, placement in an extreme medial position may cause for entry into the extralymphatic or lymphatic space. The femoral site is traditionally a site of last resort, owing to the high likelihood of contamination, vis-à-vis the groin. Instances in which the femoral site is advantageous include patients who may be coagulopathic. Although there have been few studies that specifically review the femoral vein as a primary cannulation site of choice, one study exploring US-guided cannulation in this site did show a significantly reduced number of venipuncture attempts (2.3 vs. 5.0; P = 0.0057) and rate of complications (0 % vs. 20 %; P = 0.025) [7]. Recall that subclavian sites may be dangerous in this case as inadvertent puncture of the subclavian artery may lead to massive hemothorax, owing to the non-compressibility of the subclavian artery. Lastly, in the event that femoral cannulation is required, it is the personal experience of the author that these femoral central venous catheters remain in place for no more than 24 h, until a definitive CVC is placed in an alternate location. Traditionally, femoral vein CVC placement is a location of last resort.
6 Implementation of US Guidance for CVC Placement
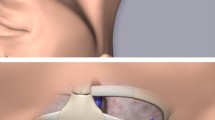
Ultrasound has found an expansion in utilization owing to its relatively inexpensive cost, lack of ionizing radiation, and excellent safety profile. Moreover, in its procedural implementation, there is no need for contrast. Due to this widespread adoption, many medical schools have begun implementing formal didactics and training throughout the 4-year allopathic educational model [24]. Web-based models have found widespread success in the adoption of US CVC guidance techniques for physicians in training and have improved the base of knowledge for procedural competence [25, 26]. Techniques that may be employed include either static or dynamic techniques. Static techniques are employed by operators that may not be facile in the use of probe or when a sterile probe cover is not available. By definition, static techniques rely on the operator using the probe to gain orientation to the structure of interest, marking the skin over the vein and placing the probe aside. Static techniques are less optimal as the operator may still hit the artery or penetrate the posterior wall of the vein. In contrast, dynamic techniques are superior with regard to avoiding complications [27]. However, they may be more challenging for junior operators to master. In the dynamic technique, the operator maintains the probe in the field at all times so that the needle may be visualized in the area of interest throughout the duration of vessel cannulation. This provides for a safer procedure, as inadvertent puncture of the nearby artery or the posterior wall is avoided. The author utilizes a technique where in right-sided IJ placement via US, the thenar aspect of the left hand is lightly steadied on the patient’s jaw. This enables the operator to maintain the probe in an optimal perpendicular plane. A good view will reveal the IJV to be circular, whereas an off-axis view will provide an oblong appearing IJV. At this point, the operator should test for compressibility of the IJ. See Fig. 12.2 to the left.
Utilizing the dynamic technique with a short axis view, the operator then slowly advances the needle at a 30–45° angle with the bevel down, looking for a “V” indentation on the anterior aspect of the IJV. The needle is advanced until a dark red venous flash is obtained. It should be cautioned to not advance if the flash is lost, as this may signify penetration of the posterior wall of the vessel. See Fig. 12.3 for an image of the needle being introduced into the vein.
This may occur even in dynamic US placement as the angle of approach may take the needle out of the plane of the US transducer at the distal end of the vessel. Besides US, additional means of confirming the needle in the vein include utilizing a sterile length of IV tubing to transduce central venous pressure. In the case of arterial puncture, blood flow will not cease and will climb the entire length of tubing. In venous puncture , the blood flow may rise to a certain point and then cease. Significant respiratory variation of venous flow in the transducer tubing may signify hypovolemia or pneumothorax . It should be noted that IJV CVC placement still carries a significant risk of pneumothorax, particularly if the placement occurs on the lower third of the neck. A significant review of the literature revealed a paucity of information on the use of US in the SC site. Traditionally, operators may switch to a long axis (LA) view . See Fig. 12.4.
However one prospective, randomized crossover trial failed to show an attendant increase in the success rate in US-guided SC CVC placement [28]. This is likely due to a number of reasons, among them being the fact that anatomically the SC vein courses beneath the clavicle.
7 Complications
A number of factors may impact complication rates in the placement of CVC lines. In research conducted at Johns Hopkins, it was noted that although operator experience of less than 25 CVC lines did not impact success rates, complication rates were higher in inexperienced operators [29]. In a comprehensive review, a number of risk factors have been elucidated, with some of the more prominent being inexperience, number of needle passes (sixfold increase in complication risk with > three needle passes), BMI > 30 or < 20, large catheter size (i.e., hemodialysis access catheter ), or prior operation and/or radiation exposure in the area of interest [6, 30]. Rare complications may include guidewire fraying, retention, or perforation of the vena cava. These complications, although rare, may require either median sternotomy or IR-guided retrieval of the retained wire [31]. Common complications for CVC placement are outlined as follows in Table 12.3:
8 Process of CVC Insertion
The process of CVC insertion is best performed in a controlled environment. Clinicians are encouraged to use a pre-procedure checklist which facilitates safety and quality assurance. This provider’s direct experience has been to perform the procedure with a minimum of assistance from other providers, who may be encumbered with other patient care activities.
The process is as follows for ultrasound-assisted placement of a CVC in the right internal jugular vein:
-
1.
Obtain informed consent and discuss the risks and benefits of the procedure, as well as any potential complications. Ensure that the consent has the correct date and time. Also, if a phone consent is obtained, clearly print the name and telephone number of the consenting party. Document the type of relationship and have a witness verify and attest that you have thoroughly addressed the informed consent process.
-
2.
Verify two forms of identification, typically patient name and date of birth. If the patient is intubated, verify with a second provider at the bedside. Also verify any allergies. Conduct a formal time-out process with the bedside nurse in attendance.
-
3.
Gather necessary equipment including a mask and cap for each person remaining in the room during the procedure. Also gather the CVC kit, a gown, two pairs of sterile gloves, a sterile dressing kit, and sterile flushes.
-
4.
Additionally, the ultrasound machine should be powered on, plugged in, have the correct vascular access probe connected, and should have correct settings entered for depth and gain. A sterile probe cover should be obtained. At this point, it is prudent to inform the patient of the fact that you may be resting your hand on their jaw and that a drape will cover their face during the procedure. The author simulates this motion with the patient so that they understand their optimal body positioning throughout the procedure. A baseline ultrasound view is obtained of the internal jugular vein.
-
5.
The bed is then placed in Trendelenburg position. If the patient has respiratory distress, this step can be deferred until after the draping process to minimize time in this position.
-
6.
Using a skin marker, the operator marks their initials on the side of the body on which the CVC line will be placed.
-
7.
The operator should thoroughly wash their hands for 60 s.
-
8.
At this point the operator opens the sterile equipment and dons the gown, along with two pairs of sterile gloves. The author proposes the cover glove system as it allows for more independent preparations. The outer gloves are typically one half size larger and may be shed after draping has taken place and after the ultrasound probe has been placed in the sterile probe cover.
-
9.
Using chlorhexidine or betadine, cleanse the area in widening concentric circles and allow the cleansed area to dry. After drying, cleanse a second time, this time with a scrubbing motion. Ensure that not only the neck, but the landmarks which encompass the subclavian site are cleansed and draped so that the SC site may be used as a secondary insertion point should IJ insertion fail.
-
10.
Drape the patient with a sterile sheet. Most commercially available kits contain a sterile drape with a clear area for patient visibility and a circular fenestration. Place this fenestration over the IJ site, ensuring that you do not drag any contaminated patient care bed linens into the sterile field which also encompasses the upper chest.
-
11.
If assistance is available, have your assistant hold the ultrasound probe above the opening for the sterile probe cover, and using gravity, have them gently lower the probe into the probe cover. If no assistant is available, the operator may perform this piece independently and shed the outer cover glove after carefully placing the sterile probe cover/probe assembly on the field.
-
12.
Draw up 5 cc of 1 % lidocaine and infiltrate the soft tissues of the neck after gently aspirating the syringe.
-
13.
At this point, organize the equipment on a sterile tray table in the order that it is used in the procedure. This ensures consistency of placement and assures an expeditious CVC placement. For junior operators, this assists them in acting as a type of prompt for the next step in the line placement process.
-
14.
Using the provided sterile flushes included in the CVC kit, flush out all air from any attached claves, central line ports, or tubing.
-
15.
Gently place the left hand with the probe perpendicular to the vessel in a short axis view. Steady the thenar aspect of the hand on the patient’s jaw. Ensure the view with the probe matches with the anatomic positioning of the vessels, with the carotid on the medial side and the internal jugular vein on the lateral side. Gently compress the vessel and center the vein in the middle of the screen.
-
16.
With the bevel side down, position the right hand to bring the syringe into an acute angle. Maintain the needle into the plane of the ultrasound window. While steadily advancing the needle, look for a “V” indentation on the anterior wall of the vessel while continuing to gently aspirate. Continue to keep the needle in view of the ultrasound window. If the needle bevel disappears, stop advancing with the right hand and slowly slide the left probe hand toward the base of the neck until the needle comes back into view. Once the needle is in the center of the vessel, continue to gently aspirate and drop the angle of the right hand to a shallower angle (approximately 30–45°).
-
17.
Gently detach the syringe. If a sterile length of IV tubing is available in the kit, transduce and check blood flow.
-
18.
Remove the tubing and introduce the guidewire. Monitor both length of guidewire and check for any dysrhythmias. Ensure that the guidewire is not put down at any time. Throughout the procedure, the operator may have to switch hands, but at no time should they put the wire down. Using ultrasound, verify the position of the guidewire in the vessel.
-
19.
With the needle still in place over the guidewire, gently nick the skin with the number 11 blade, with the blade side up. It is important to nick the skin with the needle covering the guidewire so that the wire is not inadvertently frayed by the blade.
-
20.
Remove the needle and advance the vessel dilator via Seldinger technique. Verify the dilator via ultrasound.
-
21.
Remove the dilator and advance the catheter over the guidewire. Remove the guidewire and recover it into the guidewire sheath. This is in the event that the vessel needs to be recannulated for any reason. Additionally, the guidewire may potentially contaminate the field if left out.
-
22.
Suture the catheter in position and flush all three ports with sterile saline.
-
23.
Place a sterile dressing and mark the date and time on the dressing. Verify the needle and sharp counts with the bedside nurse.
-
24.
Place an order for a postprocedure chest X-ray to verify the CVC line position.
-
25.
Provide the patient/bedside nurse with education on CLABSI prevention. The CDC FAQ sheet may be found online at: http://www.cdc.gov/hai/pdfs/bsi/BSI_tagged.pdf [35].
-
26.
Document the procedure note and document any medications given, number of attempts, complications, and results of postprocedure chest X-ray. Write an order allowing the nurse to use the CVC line and maintain a relevant operator procedure log which documents site, side, number of attempts, and complications.
9 Conclusions
CVC placement is a procedure which is conducted ubiquitously in a variety of critical care settings. US guidance greatly increases the likelihood of operator success. That being said, complication rates in junior operators with less than 25 line placements may still be common. Operators with <25 prior insertions cause more complications (25.2 % vs. 13.6 %, P = 0.04), require the assistance of a senior operator more frequently, and have more completely failed attempts [32]. Best practices and good judgment should be utilized in the placement of CVC catheters, and junior operators doing 25–50 line placements have higher success rates (90 % vs. 75 %) when supervised by a more experienced operator, with a lower interim complication rate using US. Senior operators responsible for the training of individuals should utilize a number of strategies including web-based didactics, simulation, physical supervision, and frequent review of procedural logs [24–26, 32]. Although success with US guidance may be site dependent and higher in the IJ position, the long axis view utilizing a dynamic technique has a reduced likelihood of PWP [23]. With experienced operators, in the event that no US machine is available, the subclavian position may still be a safe alternative [22]. Although many studies have addressed the difference in complication rates among learners of various experience levels, some data with regard to physician assistants vs. physicians show that well-trained physician assistants have comparable complication rates when conducting invasive procedures [33, 34].
References
Hermosura BVL. Measurement of pressure during intravenous therapy. JAMA. 1966;195:181.
Gourlay D. Central venous cannulation. Br J Nurs. 1996;5(1):8–15.
Legler D, Nugent M. Doppler localization of the internal jugular vein facilitates central venous catheterization. Anesthesiology. 1984;60:481–2.
Nomura J, Sierzenski P. Cross sectional survey of ultrasound use for central venous catheter insertion among resident physicians. Del Med J. 2007;80(7):255–9.
Denys B, Uretsky B. Ultrasound-assisted cannulation of the internal jugular vein. A prospective comparison to the external landmark-guided technique. Circulation. 1993;87(5):1557–62.
Schummer W, Schummer C, Rose N, et al. Mechanical complications and malpositions of central venous cannulations by experienced operators: a prospective study of 1794 catheterizations in critically ill patients. Intensive Care Med. 2007;33:1055–9.
Gibbs F, Murphy M. Ultrasound guidance for central venous catheter placement. Hosp Physician. 2006;42(3):23–31.
Mahler S, Wang H. Short vs. long-axis approach to ultrasound guided peripheral intravenous access: a prospective randomized study. Am J Emerg Med. 2011;29:1194–7.
Karakitsos D, Labropoulos N. Real -time ultrasound-guided catheterisation of the internal jugular vein: a prospective comparison with the landmark technique in critical care patients. Crit Care. 2006;10(6):1–8.
Cowl C, Weinstock J. Complications and cost associated with parenteral nutrition delivered to hospitalized patients through either subclavian or peripherally-inserted central catheters. Clin Nutr. 2000;19(4):237–43.
Yeum C, Kim SW. Percutaneous catheterization of the internal jugular vein for hemodialysis. Korean J Intern Med. 2001;16(4):243–6.
Geddes C, Walbaum J. Insertion of internal jugular temporary hemodialysis cannulae by direct ultrasound guidance-a prospective comparison of experienced and inexperienced operators. Clin Nephrol. 1998;50(5):320–5.
Pervez A, Abreo K. Central vein cannulation for hemodialysis. Semin Dial. 2007;20(6):621–5.
Leung J, Duffy M. Real-time ultrasonagraphically-guided internal jugular vein catheterization in the emergency department increases success rates and reduces complications: a randomized, prospective study. Ann Emerg Med. 2006;84(5):540–7.
Theodoro D, Bausano B. A descriptive comparison of ultrasound-guided central venous cannulation of the internal jugular vein to landmark-based subclavian vein cannulation. Acad Emerg Med. 2010;17(4):416–22.
Lampert M, Cortelazzi P. An outcome study on complications using routine ultrasound assistance for internal jugular vein cannulation. Acta Anaesthesiol Scand. 2007;51:1327–30.
Leung J, Duffy M. Real-time ultrasonagraphically-guided internal jugular vein catheterization in the emergency department increases success rates and reduces complications: a randomized, prospective study. Ann Emerg Med. 2006;48(5):540–7.
Shrestha BR, Gautam B. Ultrasound versus the landmark technique: a prospective randomized comparative study of the internal jugular vein cannulation in an intensive care unit. JNMA J Nepal Med Assoc. 2011;51(182):56–61.
Slama M, Novara A. Improvement of internal jugular vein cannulation using an ultrasound-guided technique. Intensive Care Med. 1997;23:916–9.
Sznajder J, Zveibil F. Central vein catherization. Failure and complication rates by three percutaneous approaches. Arch Intern Med. 1986;146:259–61.
Crozier J, McKee R. Is the landmark technique safe for the insertion of subclavian venous lines? Surgeon. 2005;3(4):277–9.
Mansfield P, Hohn D. Complications and failures of subclavian-vein cannulation. N Engl J Med. 1994;331(26):1735–8.
Vogel J, Haukoos J. Is long-axis view superior to short axis view in ultrasound-guided central venous catheterization? Crit Care Med. 2015;43(4):832–9.
Baltarowich O, DiSalvo D. National ultrasound curriculum for medical students. Ultrasound Q. 2014;30(1):13–9.
Grover S, Currier P. Improving residents’ knowledge of arterial and central line placement with a web-based curriculum. J Grad Med Educ. 2010;2(4):548–54.
Mosier J, Malo J. Critical care ultrasound training: a survey of US fellowship directors. J Crit Care. 2014;29:645–9.
Scott L, Wax J. Use of ultrasound to guide vascular access procedures-AIUM practice guideline. American Institute of Ultrasound in Medicine. 2012:1–23
Bold R, Winchester D. Prospective, randomized trial of doppler-assisted subclavian vein cannulation. Arch Surg. 1998;133:1089–93.
Bo-Linn G, Anderson D. Percutaneous central venous catheterization performed by medical house officers: a prospective study. Cathet Cardiovasc Diagn. 1982;8:23–9.
Kusminsky R. Complications of central venous catheterization. J Am Coll Surg. 2007;204(4):681–96.
Phy M, Neilson R. Guidewire complication with central line placement. Hosp Physician. 2004;June:41–43.
Lennon M, Zaw N. Procedural complications of central venous catheter insertion. Minerva Anestesiol. 2012;78(11):1234–40.
Cox T, Parish T. A study of pneumothorax rates for physician assistants inserting central venous catheters at a large urban hospital. Internet J Allied Health Sci Pract. 2005;3(3):1–4.
Benham J, Culp C. Complication rate of venous access procedures performed by a radiology practitioner assistant compared with interventional radiology physicians and supervised trainees. J Vasc Interv Radiol. 2007;18:1001–04.
FAQs about Central Line Associated Bloodstream Infections [Internet]; 2010 [updated 2012 May 10; cited 2015 Mar 30]. Available from: http://www.cdc.gov/HAI/bsi/bsi.html. Accessed 25 Nov 2010.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
O’Gowan, R. (2016). Central Venous Catheterization With and Without Ultrasound Guidance. In: Taylor, D., Sherry, S., Sing, R. (eds) Interventional Critical Care. Springer, Cham. https://doi.org/10.1007/978-3-319-25286-5_12
Download citation
DOI: https://doi.org/10.1007/978-3-319-25286-5_12
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-25284-1
Online ISBN: 978-3-319-25286-5
eBook Packages: MedicineMedicine (R0)