Abstract
Central venous access is an essential skill for critical care providers. More than 5 million central venous catheters are inserted annually in the United States, with an overall complication rate of 15%. Use of ultrasound guidance increases success and reduces complications. The use of ultrasound guidance for central venous access has been recommended by multiple medical societies and supported by several studies in the literature. The use of ultrasound guidance for central venous catheterization has significantly increased in recent years, and it has become standard of care in current clinical practice. This chapter will review the basic principles of this technique, indications, contraindications, preparation, and procedural steps for ultrasound-guided central venous catheter (CVC) placement in the internal jugular, femoral, subclavian, and axillary veins.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Ultrasound
- Ultrasonography
- Central venous access
- Central venous catheter
- Central venous catheterization
- Internal jugular vein
- Femoral vein
- Subclavian vein
- Axillary vein
Introduction
Central venous access is a commonly performed procedure in a variety of acute care settings. The use of real-time ultrasound guidance for cannulation has been shown to improve success rates and decrease mechanical complications when compared to traditional landmark-based techniques. Multiple studies have demonstrated the benefits of using ultrasound guidance for central venous access in internal jugular and subclavian veins. Real-time needle visualization results in fewer needle pass attempts, increased first-pass success, and decreased complications. Understanding sonographic anatomy and basic principles of needle guidance is crucial to successfully perform central venous cannulation using ultrasound guidance. Ultrasound-guided needle placement can be performed in an “in-plane” or “out-of-plane” or “oblique” technique. Once the guidewire is inserted, ultrasound can be used to ensure the correct placement of the wire. It is critical to confirm wire location prior to dilation and central line placement. The diameter of the typical introducer needle and guidewire ensures minimal complications in the case of arterial penetration in comparison to dilation and cannulation with a central line catheter. Following catheter placement, ultrasound can be used to confirm catheter position using a saline flush test in combination with cardiac sonography.
Advantages of Ultrasound Guidance
Ultrasound provides real-time visualization of the needle and needle tip in relation to the target vessel and other surrounding vital anatomic structures leading to improvements in success rates and decreases in complications over traditional landmark techniques. The benefit of ultrasound has been extensively demonstrated for placement of CVCs in the internal jugular vein. A recent Cochrane review found a 71% reduction in complications and a 57% increase in first-stick success when using ultrasound guidance for internal jugular CVC placement compared to anatomic landmark techniques [1]. Another similar review also showed a reduction in complications with ultrasound-guided subclavian CVC placement and an improved success rate for femoral vein CVC placement [2]. Ultrasound guidance for internal jugular venous access is currently recommended by multiple organizations including the Agency for Healthcare Research and Quality [3].
Another advantage to ultrasound is the ability to evaluate the patency of a vein prior to cannulation. The operator can ensure the vein distends adequately without evidence of stenosis, thrombus, or variant anatomy. After cannulating the vessel, ultrasound can visualize guidewire entry and confirm successful catheter placement.
Anatomy
The internal jugular and subclavian veins are commonly used for ultrasound-guided central venous access. The internal jugular vein exits the skull via jugular foramen; then descends down the neck, lateral to the carotid artery within the carotid sheath; and eventually joins the subclavian vein. It is the most superficial in the upper part of the neck and lies underneath the sternocleidomastoid muscle at the level of the thyroid cartilage. At the level of the sternoclavicular joint, the internal jugular vein joins the subclavian vein to form the brachiocephalic vein. Since it is not concealed by bone, it is an ideal vein to visualize using ultrasound. The subclavian vein is a continuation of the axillary vein, lying anterior to the subclavian artery and runs from the lateral border of the first rib to the medial border of the anterior scalene muscle. It joins the internal jugular vein posterior to the sternoclavicular joint and forms the brachiocephalic vein. Since the subclavian vein runs for a significant distance under the clavicle which generates an acoustic shadow on ultrasound, it is technically challenging to perform ultrasound-guided cannulation compared to internal jugular vein cannulation. The common femoral vein is found medial to the common femoral artery below the inguinal ligament. In the proximal thigh, the femoral and deep femoral veins join to form the common femoral vein. Below the inguinal ligament, the greater saphenous vein joins the common femoral vein anteromedially. The common femoral vein becomes the external iliac vein as it ascends posterior to the inguinal ligament.
It is crucial to distinguish the sonographic appearance of veins from arteries to perform ultrasound-guided central venous access. Veins and arteries are typically identified by their size, shape, ability to be compressed with pressure, color Doppler characteristics, and spectral Doppler waveforms. Both structures have an anechoic lumen, while the artery is round in appearance, has a thick hyperechoic wall, and demonstrates visible pulsations. Veins have relatively thin hypoechoic wall, are oval in appearance, are easily compressible with pressure, and demonstrate phasic flow (Figs. 6.1, 6.2, 6.3, and 6.4). Pulsed-wave Doppler is the only reliable method of confirming vessel identify in almost all conceivable situations as various combinations of conditions can lead to confusion between artery and vein when relying solely on compression and color Doppler assessment.
Indications
-
Providing medications that are caustic to smaller vessels, i.e., vasopressors, certain antibiotics, and long-term electrolyte replacement
-
Large volume resuscitation (Cordis line)
-
Hemodynamic monitoring
-
Transvenous cardiac pacing
-
Hemodialysis/plasmapheresis
-
Difficult venous access
Contraindications
A CVC should not be placed in an area with overlying cellulitis or where it will be difficult to maintain site sterility. A CVC should not be placed in a clotted or stenotic vein or if there is known or suspected venous injury. Coagulopathic and obese patients should be approached with great care as there is an increased risk of complications. If a patient is in need of dialysis or is to have an arteriovenous (AV) fistula placed, the central line should not be placed in the vein that the AV fistula or temporary catheter will be placed.
Equipment and Probe Selection
Probe Selection
A high-frequency linear probe (Fig. 6.5) should be used as it provides the best resolution for superficial structures such as the veins that require cannulation as well as the needle tip. Typical modern broadband transducers now range from approximately 15–6 MHz, but exact frequencies and bandwidth can vary widely. While attempting a supraclavicular subclavian line, the endocavitary probe (Fig. 6.6) or other small footprint high-frequency probe can be used as this provides better access to the supraclavicular fossa.
Equipment
-
Antiseptic (chlorhexidine gluconate, betadine, etc.)
-
Local anesthetic (1% lidocaine)
-
Gauze
-
25 gauge needle for anesthetic infiltration
-
18 gauge introducer needle
-
Syringes (3 cc, 10 cc)
-
Needles for anesthetic (18 gauge, 25 gauge)
-
Sterile drapes, gown, gloves, mask, and hat
-
Sterile ultrasound probe cover
-
J-shaped guidewire
-
Dilator
-
11 blade scalpel
-
Large Tegaderm
-
Biopatch
-
Catheter
Preparation and Preprocedure Evaluation
The site and choice of catheter depends on the clinical scenario. The subclavian or internal jugular veins are typically preferred because of lower infection rates and thrombosis, but a femoral CVC is appropriate in many situations. For certain procedures or when large volume resuscitation is required, a large bore 8.5 french (2.8 mm) introducer (Cordis) (Fig. 6.7) may be required. When central access is required to give specific medications or provide central venous pressure monitoring, a multilumen CVC (Fig. 6.8) may be more appropriate. (It is important to note that a multilumen CVC is typically inferior to large bore peripheral IV access for rapid volume resuscitation due to the resistance to flow caused by the longer catheter length.) Informed consent should be obtained and the benefits and risks explained. In emergent settings, if the patient or a next of kin is unable to provide timely consent, implied consent may be necessary.
Prior to setup, anatomic landmarks should be assessed by ultrasound. First note the location of the target vein and its corresponding artery. Veins will appear to have thin walls versus the thicker walled and pulsatile artery. Note that the artery should not be easily compressible, while the vein should compress with gentle probe pressure. The use of color Doppler may also demonstrate the pulsatile flow of the artery and the steady flow of the vein. Scan up and down to visualize the course of the vein, while also taking note of surrounding structures. It is important to identify surrounding vessels, nerves, lymphatics, or evidence of lung tissue as these structures should be avoided while placing the line.
There are two ways that ultrasound can be utilized to guide the placement of CVCs. The static approach describes when ultrasound is used to confirm the location of the target vein and its trajectory and to assess the surrounding anatomy, but is not used during the procedure itself. The site of needle insertion over the vein must be marked on the skin prior to sterilization. The dynamic approach is when ultrasound is used to provide real-time visualization during needle insertion and help guide needle advancement into the target vessel. It has been found that the static approach has superior first-attempt success rates than the landmark technique (also known as the “blind” technique) alone. It can be done quickly if the practitioner is unable to place the line with the ultrasound probe remaining stable or if a sterile cover is not available. However, the same study found the dynamic approach to be superior to both static and landmark techniques [4]. The dynamic approach is strongly recommended as there is potential for the alignment and orientation of vessels to change with movement (particularly for the internal jugular vein with head and neck movements).
After scanning the vessel, the room should be set up appropriately with ultrasound machine and equipment in locations that permit the operator to easily access equipment and visualize the screen. The patient should be prepared and draped in normal sterile fashion. Clean the patient’s skin with chlorhexidine gluconate or a comparable antiseptic solution. The operator should gown and then drape the patient. It is important to have an assistant to aid the operator in handling equipment and the ultrasound probe.
When using a dynamic approach, the ultrasound probe must be placed in a sterile sleeve. A sheath of at least 6 feet in length is important to cover enough cable length to avoid contaminating the sterile field with uncovered cable. However, some radiology procedural sterile sheaths can be so long as to be unmanageable when it comes to dressing a standard ultrasound transducer. Sterile ultrasound sleeves are typically packaged with sterile ultrasound gel. A copious amount of gel should be placed directly in the sleeve prior to inserting the probe to ensure that the entire footprint of the ultrasound probe is covered. The ultrasound probe can then be lowered into the sleeve by the assistant (Fig. 6.9). Rubber bands provided are used to keep the sterile sleeve in place. When applying the rubber band, try to make sure there is a layer of gel in between the transducer footprint and the sterile sleeve free of air bubbles.
In the event that an assistant is not available, a single-operator technique can be used to cover the probe. The probe should be placed in a holder on the ultrasound cart, and gel should be applied prior to the operator gowning. After the operator has put on sterile gloves and gown, the operator will place his hand inside the sterile ultrasound cover sleeve and grasp the nonsterile probe as demonstrated in Fig. 6.10. The operator can then grab the corner of the sleeve and pull the cover over the probe and cord as shown in Fig. 6.11.
All equipment should be inventoried and inspected prior to starting the procedure. When using a multilumen CVC, the lumens should be instilled with normal saline to assess for integrity and/or malfunction.
Procedure
The previously determined site of needle entry should be anesthetized using local anesthesia. Always make sure to aspirate prior to instilling the lidocaine to ensure the needle is not inside a vessel. The dynamic approach for ultrasound guidance can be performed using three different needle visualization techniques: in-plane, out-of-plane, and oblique (Table 6.1).
Out-of-Plane Approach
In the out-of-plane approach , the ultrasound beam is insinuated perpendicular to the target vessel causing it to appear as a circle. Once the needle is inserted through the skin, the practitioner should translate the ultrasound probe both proximally and distally to identify the location of the needle tip. The needle tip is seen as a bright, hyperechoic dot with reverberation artifact (Fig. 6.12). Because the needle will also be perpendicular to the ultrasound beam, or “out-of-plane,” the practitioner must actively translate the ultrasound probe as the needle is advanced to maintain constant needle tip visualization . If the needle tip is not adequately visualized, the operator can move the needle side to side to create a jiggling effect of the needle tip to aid in its identification. The needle should be slowly advanced toward the vessel while relocating the tip after each manipulation until the needle tip indents and punctures the anterior wall of the target vein. Once the needle tip is properly positioned within the vein, it should appear as a target sign. Again, the ultrasound probe should be moved distally to ensure that the needle does not pass through the back wall of the vein. Once you see the “target sign” fan the probe distally the “target sign” should disappear, and when you fan the probe back proximally the “target sign” should reappear. This indicates the needle tip is in the vessel and is known as the “vanishing target sign” [5].
An advantage of the out-of-plane approach is it allows for simultaneous visualization of the vessel and surrounding structures (artery, nerves, etc.). A common drawback is for the operator to mistake the shaft of the needle for the needle tip, which can result in advancing the needle too far and potentially puncturing the posterior wall of the vein or other nearby structures.
In-Plane Technique
In the in-plane approach , the beam is parallel to the long axis of the target vessel causing the vessel to appear as a rectangle on the screen. The needle is inserted and advanced toward the vessel in this same plane (also known as an “in-plane” approach). The benefit of the “in-plane” technique is the operator does not need to move the probe as the needle is advanced; the needle tip will always be visible so long as the needle remains in the plane of the beam. This minimizes the chances of advancing the needle tip past the posterior wall of the target vessel. Figure 6.13 shows an example of a needle in the vessel in long axis. A disadvantage of the in-plane approach is it requires that the sonographer be able to maintain alignment of the vessel and needle in the beam of the ultrasound probe, which may be difficult in some patients. If the operator swings the syringe either left or right, the needle may move out of plane and become only partially visualized. If the operator accidentally translates or fans the probe, the beam will go from cutting through the main sagittal portion of the vessel to a parasagittal portion which may prevent successful cannulation. This latter issue is often termed the cylinder tangential effect.
Oblique Approach
The oblique approach is a hybrid of the long-axis and short-axis approaches. Starting with an out-of-plane approach, the ultrasound probe is rotated so the vein is visualized midway between its short and long axis. With this technique, the needle is advanced in plane with the ultrasound probe. This allows for both visualization of the full length of the needle and assessment of anatomy around the vein (Fig. 6.14) [6, 7].
One alternate technique is to use the out-of-plane approach when puncturing the skin to make sure the needle enters directly above the vessel and then switches to an in-plane approach to visualize advancement of the needle. Alternatively, the oblique view may be utilized. Upon successful needle placement into the vessel, blood should be able to be aspirated in the syringe. At this point, the syringe can be removed, and dark, non-pulsatile blood should flow out of the needle. The guidewire should be inserted into the needle and advanced into the vein. Ultrasound can be used to visualize the guidewire as it is inserted into the vein (Fig. 6.15).
Guidewires typically have 5 cm hash markings to let the operator know how much guidewire has been inserted. The operator should not insert more than 10–15 cm of guidewire. If ectopy is noted on cardiac monitoring, the guidewire should be pulled back. The operator should never let go of the guidewire as the negative pressure generated by a deep inspiration can cause catheter embolization. A small incision should be made adjacent to the needle just large enough to pass the dilator. The needle can be removed and the dilator inserted while always maintaining control of the guidewire. After the skin and tissue are dilated, the catheter can then be thread over the guidewire using the Seldinger technique. Feed the wire back through the catheter until it comes out at the back end of the catheter (typically the brown port of a triple lumen). Grab the wire coming out at the back end of the catheter, and then advance the catheter into the vein. At this point, the guidewire should be completely removed, and blood should be withdrawn from the ports. The amount of catheter to be inserted into the patient depends on the location (right internal jugular, 14 cm; left internal jugular or right subclavian, 16 cm; left subclavian, 18 cm). Test each line using the normal saline in the syringe you have prepped making sure that each port is free of any air bubbles prior to flushing. A biopatch should be placed at the skin around the CVC. The CVC should be secured using sutures or specially made clips. The site should finally be cleaned and covered with a Tegaderm™.
When placing a Cordis , the dilator is already within the CVC (Fig. 6.7). Once the blade is used to make an incision in the skin and the needle is removed with the guidewire in place in the vessel, place the Cordis over the guidewire, and push the catheter into place making sure to keep the wire in your hands at all times. Remove the dilator with the wire and place the tubing to the end of the Cordis and flush the line. The line will similarly be sewn into place and covered with a large Tegaderm™.
Internal Jugular Vein Cannulation
Ultrasound-guided internal jugular vein catheterization is often the first choice for many practitioners due to its relative ease of access with ultrasound compared to the subclavian vein, physician familiarity, and a lower rate of catheter-related infections when compared to femoral lines [8]. Accessing the internal jugular vein may be difficult in patients that are unable to lay flat and severely dehydrated (resulting in collapse of the IJ) or who have neck trauma resulting in the need for a cervical collar. Potential complications associated with placement of an internal jugular venous catheter include pneumothorax, bleeding, hematoma formation, arterial cannulation, and laceration of the thoracic duct (left side cannulation) [6]. Ultrasound guidance can decrease the risk of these complications.
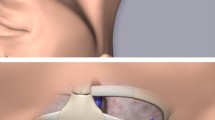
When prepping for internal jugular cannulation, the patient should be placed in Trendelenburg position (head of bed down) with the patient’s head slightly rotated away from the procedural site (Fig. 6.16). With the practitioner standing at the patient’s head, the ultrasound should be positioned next to the patient with the screen in line with the practitioner. The right internal jugular is preferred as it provides a straight course to the superior vena cava. As with the landmark technique, locate the anterior triangle of the neck with the two bellies of the sternocleidomastoid muscle and the clavicle as the inferior portion of the triangle (Fig. 6.17). When scanning this region, the internal jugular vein can be visualized lateral and superficial to the carotid artery (Fig. 6.18). Figures 6.19 and 6.20 illustrate needle puncturing internal jugular vein in in-plane and out-of-plane approaches. It is important to note that rotating the patient’s head may cause the carotid artery to be displaced posterior to the internal jugular vein, increasing the potential for inadvertent arterial puncture. The internal jugular vein should be imaged along its course to assess for its relative position to the carotid artery, vessel depth, and site of maximal diameter. After the catheter is secured, a chest x-ray should be obtained to assess placement. The tip of the line should terminate within the superior vena cava or just above the cavoatrial junction.
Common Femoral Vein Cannulation
The common femoral vein (CFV) is another option for central venous access, although it has been shown to have higher rates of catheter-related infections than both the internal jugular and subclavian vein. These lines are often placed as temporary central access in emergency situations as they can be placed while the patient is being intubated and during chest compressions or procedures to the chest including thoracentesis or thoracotomy.
The CFV is optimally visualized when the leg is abducted and externally rotated (frog leg position). The operator should be positioned on the side of cannulation with the ultrasound screen in line with the practitioner (Fig. 6.21). The CFV is found just below the inguinal ligament where it travels medial to the common femoral artery and femoral nerve. It is important to make sure the femoral artery is not overlying the femoral vein prior to attempting cannulation (Fig. 6.22).
The line should be placed as noted above. Successful catheter placement can be confirmed with ultrasound by visualizing the catheter within the femoral vein and seeing that the catheter flushes and draws venous blood.
Subclavian and Axillary Vein Cannulation
Since 2011, the CDC has recommended that a subclavian or axillary line should be placed over an internal jugular or femoral line to reduce the risk of infection when placing a nontunneled catheter [9]. The lower infection risk of subclavian and axillary venous catheters is sometimes offset by the high risk of pneumothorax – a complication often associated with physician inexperience [6]. Ultrasound guidance can be used to help avoid this risk.
The axillary vein arises from the brachial vein in the axilla and travels across the chest toward the first rib where it becomes the subclavian vein. The axillary vein can be cannulated under ultrasound guidance using the infraclavicular approach. The subclavian vein can be cannulated under ultrasound guidance using the supraclavicular approach. For both approaches, the patient should be placed in Trendelenburg position to minimize the risk of air embolism.
For the supraclavicular approach, the operator should stand at the patient’s head with the ultrasound next to the patient and the screen of the ultrasound in line with the practitioner. The linear probe can be used for this approach (Fig. 6.23); however, an endocavitary probe may provide better access to this region given its small footprint (Fig. 6.24). To identify the subclavian vein, first locate the internal jugular vein and track it proximally. The subclavian vein will be seen uniting with the internal jugular vein in the supraclavicular fossa (Figs. 6.25 and 6.26). The vessel can be cannulated using an in-plane technique. If available substitute a neonatal-type, high-frequency micro-convex array probe for the endocavitary probe as it will be easier to wield when attempting vascular access while still providing good access to this site.
For the infraclavicular approach, the practitioner usually stands on the patient’s side with the ultrasound machine near the patient’s head. Sonographic visualization of the axillary vein is improved when the patient’s arm is abducted and externally rotated. The axillary vein can be visualized by placing the transducer on the lateral position of the chest wall (Fig. 6.27). The axillary vein can be followed as it travels inferior to the deltopectoral groove of the clavicle and becomes the subclavian vein as it crosses the first rib (Fig. 6.28). You may be able to see lung sliding deep to the axillary vein. The axillary vein can be cannulated using either an in-plane or out-of-plane approach as previously described.
An axillary CVC is more easily placed with ultrasound guidance than a subclavian CVC since the clavicle does not obscure the vessel. It has also been demonstrated that the axillary vein tracts away from both its corresponding artery and the rib cage as it courses distally, suggesting less risk of arterial puncture and pneumothorax [10].
Confirming Placement
X-ray has previously been the study of choice to assess for proper placement of upper extremity CVCs. The catheter should be seen coursing along the path of the vein with its tip terminating near the superior vena cava/right atrial junction. A large downside to x-ray confirmation is the time and resources it requires to obtain the image and process it for review. Alternatively, bedside ultrasound can be used to rapidly assess for proper catheter placement using agitated saline. Agitated saline can be made at the bedside with two 5 ml syringes and a three-way stopcock. One syringe should be filled with normal saline and the other empty. Place the two syringes on the stopcock, and close the third end so that the syringes are flowing into one another. “Agitate” the saline by quickly moving the saline between the two syringes. Once this is complete (10–30 seconds of agitation) (Fig. 6.29), instill the saline into the central line while using ultrasound to visualize the right atrium and ventricle. If the catheter is correctly placed, agitated normal saline bubbles (Fig. 6.30) will be seen within the right atrium and right ventricle [11]. Subclavian CVC placement sometimes results in cannulation of the ipsilateral internal jugular vein. A technique to detect this complication is to flush normal saline into the CVC while placing the palm of your hand on the patient’s neck. If a thrill is palpated when fluid is instilled, the line should be reattempted [12].
Complications
Pneumothoraces
This is a risk when placing subclavian and internal jugular CVCs. Ultrasound can evaluate for a pneumothorax after line placement more quickly and accurately than portable chest x-ray [13]. With the patient lying supine, the linear probe is placed in the midclavicular line with the probe marker toward the patient’s head. The pleural line can be identified as a hyperechoic line between the inferior aspects of the ribs (Fig. 6.31). As the patient breaths, the sonographer should note sliding or “shimmering” of the lung pleura. In the case of a pneumothorax, this will be absent. Occasionally, comet tails may be seen which is an indication of normal lung tissue and rules out a pneumothorax in this region. The sonographer should scan between multiple rib spaces to ensure that the patient does not have a small or focal pneumothorax. Use of M-mode may also help the sonographer. In the event of a pneumothorax and absent lung sliding, there will be no motion detected, and the “barcode” sign (Fig. 6.32) will be seen. Alternatively, when lung sliding is present, one will see the “seashore” sign (Fig. 6.33) [11].
Infections
Nontunneled CVCs are at the highest risk for central line-associated bloodstream infections (CLABSI) with femoral lines yielding the highest infection rate. Intrinsic or non-modifiable risk factors for infection are patient age, underlying disease or conditions, and patient gender (increased risk in males and the elderly). Extrinsic or modifiable risk factors include prolonged hospitalization before CVC insertion, multiple CVCs, parenteral nutrition, femoral or internal jugular access site, heavy microbial colonization at insertion site, multilumen CVCs, lack of maximal sterile barriers for CVC insertion, and CVC insertion in an intensive care unit or emergency department [14]. Using ultrasound guidance for CVC insertions helps decrease the risk of associated infections by decreasing the number of cannulation attempts. Adherence to full barrier precaution technique throughout the procedure is also vital in reducing infection rates. Additionally, the continued need for central access should be frequently reassessed to minimize the duration that CVCs are in place.
Other Complications
Other potential complications of CVC placement include arterial puncture, hematoma formation, arteriovenous fistula formation, intraluminal dissection, venous air embolism, retroperitoneal bleeding, pseudoaneurysm, a lost wire which may cause an atrial wall rupture, thrombus formation, nerve injury, anaphylaxis from an antibiotic impregnated catheter, thoracic duct injury (with left-sided cannulation), or catheter malposition [6].
Pearls and Pitfalls
-
A common pitfall in the out-of-plane approach is to mistake the shaft of the needle for the tip resulting in advancing the needle too far which can lead to posterior wall, artery, or lung perforation.
-
When using the out-of-plane approach, the transducer must be constantly repositioned to maintain visualization of the needle tip. Slightly jiggling the needle can also help localize the tip.
-
Taking time to set up the room appropriately making both CVC materials and ultrasound equipment easily accessible will improve overall success of the procedure.
-
Visualize the target vessel in both the long and short axis prior to starting the procedure to ensure there is no variant anatomy or barriers to line placement (clot, stenosis).
-
A useful approach is to start in the out-of-plane approach to make sure the needle entry is directly over the vessel and then switch to an in-plane approach to advance the needle into the vein.
-
Consider the subclavian or axillary vein when the internal jugular vein is completely collapsed due to dehydration as there is a high likelihood of posterior wall puncture.
Integration into Clinical Practice
Ultrasound decreases complications and improves success when placing CVCs. Ultrasound guidance for internal jugular cannulation is recommended by multiple organizations. Ultrasound guidance should be routinely used for CVC placement to enhance patient safety. Use of ultrasound guidance is considered as standard of practice in current clinical practice.
Evidence
-
2015 Cochrane review on ultrasonography for internal jugular line placement found that use of ultrasound when compared to the landmark technique reduced arterial punctures, number of attempts, and time to successful cannulation [1].
-
2013 meta-analysis found decreased risks of cannulation failure, arterial puncture, hematoma, and hemothorax in adult patients for which ultrasound guidance was used for CVC placement [15].
-
First-pass success is significantly increased by use of ultrasound guidance in internal jugular vein cannulation [16].
-
Use of ultrasound for subclavian cannulation is associated with better outcomes and, in at least one study, a zero incidence of pneumothorax [17].
Key Points
-
Ultrasound guidance improves success and reduces the risk of complications when placing CVCs.
-
Ultrasound can be used for placement of internal jugular, subclavian/axillary, and femoral lines.
References
Brass P, Hellmich M, Kolodziej L, Schick G, Smith AF. Ultrasound guidance versus anatomical landmarks for internal jugular vein catheterization. Cochrane Database Syst Rev. 2015;1:CD006962.
Brass P, Hellmich M, Kolodziej L, Schick G, Smith AF. Ultrasound guidance versus anatomical landmarks for subclavian or femoral vein catheterization. Cochrane Database Syst Rev. 2015;1:CD011447.
Shekelle P, Dallas P. Use of real-time ultrasound guidance during central line insertion: brief update review. In: Agency For Health Research and Quality (US), editor. The New England Journal of Medicine: AHRQ; Boston, MA 2013. p. 172–7.
Milling TJ Jr, Rose J, Briggs WM, Birkhahn R, Gaeta TJ, Bove JJ, et al. Randomized, controlled clinical trial of point-of-care limited ultrasonography assistance of central venous cannulation: the Third Sonography Outcomes Assessment Program (SOAP-3) Trial. Crit Care Med. 2005;33(8):1764–9.
Thomas S, Moore CL. The vanishing target sign: confirmation of intraluminal needle position for ultrasound guided vascular access. Acad Emerg Med. 2013;20(10):e17–8.
Troianos CA, Hartman GS, Glas KE, Skubas NJ, Eberhardt RT, Walker JD, et al. Guidelines for performing ultrasound guided vascular cannulation: recommendations of the American Society of Echocardiography and the Society of Cardiovascular Anesthesiologists. J Am Soc Echocardiogr. 2011;24(12):1291–318.
Phelan M, Hagerty D. The oblique view: an alternative approach for ultrasound-guided central line placement. J Emerg Med. Elsevier. 2009;37(4):403–8.
McGee DC, Gould MK. Preventing complications of central venous catheterization. N Engl J Med. 2003;348(12):1123–33.
O’Grady NP, Alexander M, Burns LA, Dellinger EP, Garland J, Heard SO, et al. Summary of recommendations: guidelines for the prevention of intravascular catheter-related infections. Clin Infect Dis. 2011;52(9):1087–99.
Galloway S, Bodenham A. Ultrasound imaging of the axillary vein—anatomical basis for central venous access. Br J Anaesth. 2003;90(5):589–95.
Duran-Gehring PE, Guirgis FW, McKee KC, Goggans S, Tran H, Kalynych CJ, et al. The bubble study: ultrasound confirmation of central venous catheter placement. Am J Emerg Med [Internet]. 2014.; Available from: https://doi.org/10.1016/j.ajem.2014.10.010.
Rath GP, Bithal PK, Toshniwal GR, Prabhakar H, Dash HH. Saline flush test for bedside detection of misplaced subclavian vein catheter into ipsilateral internal jugular vein†. Br J Anaesth. 2009;102(4):499–502.
Nagarsheth K, Kurek S. Ultrasound detection of pneumothorax compared with chest X-ray and computed tomography scan. Am Surg. 2011;77(4):480–4.
Commission J, Others. Preventing central line--associated bloodstream infections: a global challenge, a global perspective. Oak Brook: Joint Commission Resources; 2012.
Wu S-Y, Ling Q, Cao L-H, Wang J, Xu M-X, Zeng W-A. Real-time two-dimensional ultrasound guidance for central venous cannulation: a meta-analysis. Anesthesiology. 2013;118(2):361–75.
Augoustides JG, Horak J, Ochroch AE, Vernick WJ, Gambone AJ, Weiner J, et al. A randomized controlled clinical trial of real-time needle-guided ultrasound for internal jugular venous cannulation in a large university anesthesia department. J Cardiothorac Vasc Anesth. 2005;19(3):310–5.
Kilbourne MJ, Bochicchio GV, Scalea T, Xiao Y. Avoiding common technical errors in subclavian central venous catheter placement. J Am Coll Surg. 2009;208(1):104–9.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Tajani, A., Au, A., Fields, J.M. (2020). Ultrasound-Guided Central Venous Access. In: Adhikari, S., Blaivas, M. (eds) The Ultimate Guide to Point-of-Care Ultrasound-Guided Procedures . Springer, Cham. https://doi.org/10.1007/978-3-030-28267-7_6
Download citation
DOI: https://doi.org/10.1007/978-3-030-28267-7_6
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-28265-3
Online ISBN: 978-3-030-28267-7
eBook Packages: MedicineMedicine (R0)