Abstract
Insulin resistance is a trait that is expressed early in life and progresses to clinically identifiable states of high cardiometabolic risk, namely prediabetes and metabolic syndrome, and culminates in type 2 diabetes (T2D), cardiovascular disease (CVD) events, or both in individual patients. Lifestyle therapy is highly effective in achieving therapeutic goals to manage cardiometabolic risk, which includes preventing T2D, reducing CVD risk, treating hypertension and dyslipidemia, and improving functionality and quality of life. Lifestyle therapy and weight loss are highly effective in achieving these goals in individuals who are overweight or obese. Patient-focused approaches to lifestyle therapy are described that incorporate evidence-based practices involving diet, physical activity, behavioral interventions, and multidisciplinary care, with demonstrated effectiveness for weight loss. Nutritional therapy for the active phase of weight loss (~first year) is accomplished using any one of several healthy meal plans in a reduced calorie format, selected on the basis of personal and cultural preference. During the chronic phase of weight loss maintenance (years–decades) when patients are in energy balance, the rational choice is to emphasize nutrients shown to enhance insulin sensitivity (monounsaturated fatty acids, fiber, and whole grains; represented in Mediterranean diets) and to minimize or avoid foods that promote insulin resistance (saturated fat, trans-fat, and refined grains; represented in the typical ‘Western diet’). In patients who are overweight or obese and have cardiometabolic risks, lifestyle therapy remains the cornerstone of treatment to optimize outcomes, including those patients treated with weight loss medications or bariatric surgery.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Cardiometabolic risk
- Insulin resistance
- Diabetes prevention
- Hypertension
- Dyslipidemia
- Healthy meal plan
- Exercise
- Weight loss
- Obesity
Introduction
Cardiometabolic risk is a process that begins early in life with relative insulin resistance, progresses to the clinically identifiable states of prediabetes and metabolic syndrome (MetS), and culminates in type-2 diabetes (T2D), cardiovascular disease (CVD) events, or both in single patients [1]. Furthermore, there is a common pathophysiological process responsible for both metabolic and vascular complications that glue together this disease spectrum. Clinical manifestations of insulin resistance include abnormal glucose tolerance, increased blood pressure, and dyslipidemia [2–6]. The relationship between obesity and insulin resistance is complex; nevertheless, weight gain can exacerbate insulin resistance and impel cardiometabolic risk progression. This chapter will focus on the application of lifestyle therapy in the management of cardiometabolic risk prior to the onset of T2D. The principal interventional goals in patients with insulin resistance, prediabetes, and MetS are to prevent progression to T2D and to ameliorate the CVD risk profile, which includes improvement in hypertension and dyslipidemia. In short, lifestyle therapy is highly effective in achieving these goals.
Lifestyle therapy to manage cardiometabolic risk does not involve a universal standard prescription but rather is best implemented using an individualized, patient-centric approach in collaboration with a team of health-care professionals (HCP). In addition to general principles relevant to all patients, lifestyle therapy is designed to achieve and sustain clinically meaningful weight loss as a primary objective in individuals who are overweight or obese. Weight loss is highly effective in preventing progression to T2D, improving CVD risk factors, and treating hypertension and dyslipidemia [7–13]. Clinical algorithms and guidelines advocate diet and physical activity in prediabetes but are largely oriented to indications for glucose-lowering medications [14, 15]. In recent years, randomized clinical trials have not only demonstrated the efficacy of lifestyle therapy and the marked clinical benefits of weight loss but also those components and practices that are effective in producing and sustaining weight loss. Lifestyle therapy remains the cornerstone of weight loss therapy, alone or in combination with weight loss medications or weight loss (bariatric) surgery. Recently approved weight loss medications and refinements in bariatric surgical techniques and patient management have enabled the development of more effective strategies and medical models for management of cardiometabolic risk [16]. For example, the complications-centric approach of the American Association of Clinical Endocrinologists (AACE) emphasizes that the presence and severity of weight-related complications including prediabetes and MetS—rather than body mass index (BMI) per se—should be the primary factor used in clinical decision-making regarding weight loss treatment modality and intensity [17].
Therefore, a reconfigured approach to lifestyle therapy is proposed for patients with cardiometabolic risk, which emphasizes weight loss as a primary therapeutic strategy in patients who are overweight or obese. This approach to lifestyle therapy incorporates evidence-based practices involving diet, physical activity, behavioral change, and multidisciplinary care but also incorporates an emphasis on enhancing insulin sensitivity and managing hypertension and dyslipidemia, as needed, to counteract the underlying pathophysiology.
Cardiometabolic Risk and Prediabetes States
The increasing prevalence of T2D, together with its burden of patient suffering and social costs, underscores the importance of finding effective strategies for both treatment and prevention . Prediabetes and MetS are two clinical constructs that effectively identify individuals at high risk of future T2D [1]. Prediabetes encompasses those with increased glucose levels that are higher than the normal range but do not yet meet criteria for diabetes [18]. Prediabetes can be diagnosed on the basis of impaired fasting glucose (IFG), impaired glucose tolerance (IGT) defined by the 2-h level following as oral glucose challenge (i.e., post-oral glucose tolerance test, OGTT), or by an elevation in hemoglobin A1c (A1C) [18]. Additionally, prediabetes is part of the MetS, a condition defined by a cluster of risk factors mechanistically related to insulin resistance, including abdominal obesity, dyslipidemia , glucose intolerance, elevated blood pressure, and systemic inflammation [19].
T2D and prediabetes are not isolated entities; rather, they are manifestations of a pathophysiological process, with insulin resistance at its core, which is responsible for both metabolic and vascular disease [5, 20, 21]. Insulin sensitivity varies more than fivefold in healthy appearing individuals, and relative insulin resistance is a trait that is expressed early in life. Insulin-resistant individuals will tend to develop the MetS, which confers risk for both diabetes and CVD (e.g., myocardial infarction, stroke, and peripheral vascular disease) yielding a state of cardiometabolic risk . Hypertension and dyslipidemia are also integral manifestations of insulin resistance. Predisposition to insulin resistance and the progression of cardiometabolic risk factors to overt T2D and CVD events involves the convergence of genetic factors, behavior, and the environmental milieu, including poor diet and sedentary lifestyle. The pathophysiological process underlying cardiometabolic risk involves the accumulation of intra-abdominal fat, dysregulated secretion of adipocytokines, and systemic inflammation [22, 23]. These aspects of pathogenesis point to dysfunctional adipocytes which are insulin resistant and exhibit a diminished ability to store lipid. This causes a redistribution of fat to the intra-abdominal compartment and the accumulation of lipid within muscle cells and hepatocytes, which further exacerbates insulin resistance at the level of these organs and contributes to abnormal glucose tolerance. Generalized obesity can exacerbate insulin resistance by augmenting lipid accumulation in muscle, liver, and the visceral compartment and thus further impel progression of the cardiometabolic pathophysiological process towards the end-stage manifestations of overt T2D and CVD [24, 25]. Obesity alone, however, is not a prerequisite nor a sufficient cardiometabolic risk factor since even lean individuals can be insulin resistant and individuals with obesity can be insulin sensitive with no manifestations of MetS [1]. Nevertheless, weight loss in overweight/obese individuals with insulin resistance and cardiometabolic risk represents highly effective therapy. These principles and the spectrum of cardiometabolic risk are illustrated in Fig. 23.1.
The pathophysiology of cardiometabolic risk. Insulin resistance represents the initial lesion beginning early in life. This includes insulin resistance in adipocytes and defective capability for lipid storage, with accumulation of lipid in muscle and liver cells and in the intra-abdominal depot. There is the eventual transition to the clinically identifiable high-risk states of prediabetes and metabolic syndrome. Hypertension and dyslipidemia are common, and these individuals are then at high risk for developing type-2 diabetes, cardiovascular disease events, or both. Thus, the operant pathophysiological mechanisms give rise to both metabolic and vascular disease components. Generalized obesity is neither necessary nor sufficient as a cause for cardiometabolic disease since lean individuals can be afflicted and obese individuals can be insulin sensitive. Nevertheless, obesity can exacerbate insulin resistance and impel disease progression, and weight loss therapy represents highly effective treatment for both the prevention of diabetes and cardiovascular risk factor reduction
The most common diagnostic criteria for the MetS are those advocated by the Adult Treatment Panel III of the National Cholesterol Program; other criteria have been established by the International Diabetes Federation (IDF) and the World Health Organization (WHO), as shown in Table 23.1. One of the traits used to identify MetS is IFG; thus, patients can meet criteria for both MetS and prediabetes. Patients found to exhibit MetS traits together with prediabetes on the basis of IFG and/or IGT are at particularly high risk of future T2D and should therefore be targeted for aggressive lifestyle interventions and perhaps diabetes oral agents (e.g., metformin), according to consensus statements by the American Diabetes Association (ADA) [14] and the AACE [15].
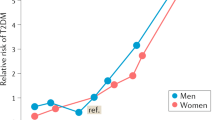
Insulin resistance is manifested by elevated fasting or postprandial insulin levels while glucose values remain normal (not decreased) or elevated. However, highly accurate measures of insulin resistance , such as the hyperinsulinemic euglycemic clamp procedure, are rarely assessed outside of clinical research settings and are not commonly ascertained by primary care physicians. This presents a challenge for the identification of individuals who are insulin resistant in clinical practice and to assess the relative risk for progression to future diabetes. However, insulin resistance and risk of T2D can be clinically identified by evaluating patients for the MetS traits delineated in Table 23.1. The Cardiometabolic Disease Staging (CMDS), illustrated in Fig. 23.2, was developed and validated as a tool to assist in the clinical stratification of individuals for diabetes risk [1]. Using information readily available to the clinician, the CMDS system can be used to identify patients at greatest risk for future T2D and CVD who may benefit from more aggressive weight loss therapy [1]. The prevalence of overweight and obesity approximates 70 % of the population in the USA, and not all patients with obesity are insulin resistant with cardiometabolic risk. The presence of overweight or obesity in subjects with no MetS risk factors (termed the ‘metabolically healthy obese’) has been well documented; these individuals exhibit lower rates of future diabetes, CVD events, and mortality [1, 26–29].
Cardiometabolic Disease Staging (CMDS) quantitatively stratifies risk for future type-2 diabetes using available clinical information. The system can be used to guide aggressiveness of weight loss therapy and optimize benefit/risk ratio for interventions. HDL-C high-density lipoprotein cholesterol, IFG impaired fasting glucose, IGT Impaired glucose tolerance. (Data were generated from the CARDIA Study cohort. From [1])
The diagnostic criteria [18] for prediabetes and T2D are shown in Table 23.2. These diagnoses have traditionally involved glucose determinations under fasting conditions, during OGTT, or random measurements. However, a criterion for the diagnostic use of HbA1C has been added, primarily to identify patients who have diabetes on the basis of elevated 2-h OGTT glucose levels who may have gone undiagnosed due to the failure of health-care professionals to perform OGTTs on a more widespread basis. The diagnosis of T2D is based on measurements of blood glucose at levels of hyperglycemia that have been shown to place patients at risk for vascular complications. The diagnostic criteria for prediabetes are generally considered to be above normal but not high enough to qualify for T2D. Even at this level of hyperglycemia, some patients with prediabetes develop microvascular disease complications, such as background retinopathy and neuropathy [30, 31]. The use of HbA1C to diagnose prediabetes is problematic since it has acceptable specificity but low sensitivity based on fasting and 2-h glucose [32]. Furthermore, the proportion of prediabetes due to IGT rises as a function of age and the sole use of HbA1C will fail to identify many patients [33]. Thus, normal HbA1C values will not effectively exclude prediabetes, and direct measurements of fasting and 2-h glucose should be considered in high-risk individuals.
Lifestyle Therapy: Treatment Goals
Lifestyle therapy can be used to effectively achieve treatment goals in patients with cardiometabolic risk . As shown in Table 23.3, a principal goal for patients with manifestations of insulin resistance and high cardiometabolic risk (i.e., prediabetes and MetS) is to prevent progression to overt T2D. Lifestyle therapy is highly effective for this purpose, and this is critically important given the rising rates of diabetes and associated morbidity, mortality, and social costs. In the Diabetes Prevention Program, it was evident that even individuals with prediabetes can develop microvascular complications, including 10 % with retinopathy and 5–10 % with neuropathy [30, 31]. Therefore, another treatment goal in prediabetes is to normalize glycemia in order to prevent microvascular complications. Lifestyle therapy can also be used to treat hypertension and dyslipidemia, thus improving the cardiovascular risk profile and increase functionality and quality of life.
Benefits of Lifestyle Therapy and Weight Loss in Patients with Cardiometabolic Risk
Lifestyle therapy improves clinical outcomes in both lean and overweight/obese patients with cardiometabolic risk. In lean individuals, physical activity and a healthy meal plan with appropriate macronutrient composition can be used to achieve treatment goals. In patients who are overweight or obese, optimal lifestyle therapy should be designed to promote clinically meaningful weight loss and maintain that weight loss over time. Unless HCP have been trained in weight loss therapy and advocate this to patients as a key therapeutic strategy in its own right, it is unlikely that the patients will experience clinically significant weight loss. Over the past decade, research has identified effective lifestyle interventions that greatly augment both treatment options and therapeutic efficacy for weight loss.
Prevention of T2D
In patients who are overweight or obese, weight loss is highly effective in preventing or delaying progression to T2D, particularly in high-risk patients with prediabetes [7–9] or MetS [12, 34, 35]. A risk-staging system, such as CMDS shown in Fig. 23.2, can be used to identify patients at greatest risk for future T2D and CVD in order to target more aggressive weight loss therapy to those individuals who will receive the greatest benefit [1]. Three major randomized clinical trials, the Diabetes Prevention Program [9, 10, 36], the Finnish Diabetes Study [8, 11, 37], and the Da Qing Study [7, 38], all demonstrated the impressive efficacy of lifestyle/behavioral therapy to prevent T2D. At the same time, weight loss also ameliorated insulin sensitivity and reduced CVD risk factors, including improvements in blood pressure, lipids, and markers of inflammation. In these studies, lifestyle modifications generally involved reductions in caloric intake (by 500–1000 cal/day), behavioral interventions, and increases in physical activity. The Diabetes Prevention Program study randomized subjects with IGT to control, metformin, and lifestyle intervention subgroups, and after 4 years, lifestyle modification reduced progression to T2D by 58 % and metformin by 31 %, compared with placebo. Subjects achieved approximately 6 % mean weight loss at 2 years and 4 % weight loss at 4 years in the lifestyle intervention arm, and in post hoc analysis, a progressive 16 % reduction in T2D risk was seen with every kilogram of weight loss [9, 10]. With observational follow-up after termination of the study, there was still a significant reduction in the cumulative incidence of T2D in the lifestyle treatment group at 10 years, despite the fact that BMI levels had equalized among the three treatment arms [36]. In addition to the reductions in T2D, there was also evidence in the Da Qing Study that CVD events and mortality were reduced after 23 years when comparing the combined subgroups treated with diet and exercise with the control subgroups [38].
Weight loss through lifestyle changes alone can be difficult to maintain [39]. Therefore, interventions such as pharmacotherapy or surgery, employed as an adjunct to lifestyle therapy, may be necessary in some patients and have also been shown to be highly effective in preventing or delaying progression to T2D. When used in combination with lifestyle therapy, orlistat [13] and phentermine/topiramate extended release (ER) [12, 40] produced greater weight loss and more profound reductions in incident diabetes when compared with lifestyle alone. Furthermore, treatment with lifestyle therapy plus phentermine/topiramate ER achieved 12.1 % weight loss after 2 years (compared with 2.5 % weight loss in lifestyle alone) as well as a 79 % reduction in the annualized T2D incidence rate in patients with MetS or prediabetes at baseline [12]. Rates of incident diabetes were reduced in patients treated with a variety of bariatric surgical procedures [41–46], which vary in their efficacy for weight loss. When the clinical decision is made to employ weight loss medications or bariatric surgery, lifestyle therapy remains a critical component of therapy for achieving and maintaining greater degrees of weight loss and for optimizing outcomes.
While lifestyle interventions, pharmacotherapy, and bariatric surgery can all produce weight loss sufficient to prevent progression to T2D, it is important to consider how much weight loss is needed for maximal efficacy in this regard. The ability to prevent T2D has been shown to be dependent on the magnitude of weight loss; however, is there a threshold for the degree of weight loss above which there is no additional benefit? In the Diabetes Prevention Program, maximal prevention of diabetes was observed at about 10 % weight loss [9, 10]. This is consistent with the study employing phentermine/topiramate ER where weight loss of 10 % reduced incident diabetes by 79 % and any further weight loss to ≥ 15 % did not lead to additional prevention [12]. The bariatric surgery studies produced greater weight loss than observed following lifestyle and pharmacotherapy interventions, yet, in two studies, there was a maximum of 76–80 % reduction in diabetes rates [44, 46] similar to that observed in the phentermine/topiramate ER intervention despite the lesser weight loss. These combined data suggest that 10 % weight loss will reduce the risk of future T2D by ~ 80 % and represent a threshold above which further weight loss will not result in additional preventive benefits. This suggests that there is residual risk for T2D that cannot be eliminated by lifestyle therapy or weight loss. T2D is a heterogeneous disease, and some individuals may have a heavy burden of gene–environment interactions that lead inexorably to T2D regardless of weight loss. Lean individuals who are insulin resistant also develop T2D at an increased rate and are not candidates for weight loss. In any event, in high-risk patients with prediabetes and/or MetS, who are overweight or obese, a therapeutic plan producing 10 % weight loss is recommended.
Management of Hypertension
Lifestyle therapy for hypertension primarily involves weight loss, reductions in dietary sodium, and exercise.
Sodium
Epidemiologic studies have suggested that populations with reduced sodium intake have lower blood pressures on average and generally tend to have less increase in blood pressure with age [47]. These populations are typically found in rural or less developed countries where much of the food supply is unprocessed. In most developed nations, a large percentage of dietary sodium is obtained from processed foods; in the USA, more than three fourths of dietary sodium intake is from processed foods [48]. The current Dietary Guidelines for Americans (DGA) suggest limiting sodium intake to less than 2300/day, or about one teaspoonful of salt [49]. Furthermore, these guidelines advocate that some groups of people, including adults 51 years and older, all African-Americans, and those with T2D, hypertension, or chronic kidney disease , limit their sodium intake to 1500 mg/day. These groups add up to about half of the US population and the majority of adults. With mean sodium intake estimated to be more than 3500 mg/day for the US population, it is not surprising that 32.6 % of the population is estimated to have hypertension [50].
Because of the ubiquity of sodium in the diet and the observed relationship between sodium and blood pressure, reduction of dietary sodium intake has been widely promoted as one of the primary strategies to lower blood pressure and prevent hypertension [48]. The efficacy of sodium reduction for lowering blood pressure has been demonstrated in several well-controlled trials. One such example was the Dietary Approaches to Stop Hypertension diet (DASH)-Sodium trial that included feeding study participants fixed diets for 30-day periods at varying levels of sodium intake [51]. When sodium intake was reduced from the highest level (142 m mol/d or 3337 mg) to the intermediate level (107 m mol/d or 2438 mg), blood pressure decreased by 2.1/1.1 mmHg (systolic/diastolic) [52, 53]. Further reduction in blood pressure of 4.6/2.4 mmHg occurred when sodium was decreased to the lower level (65 m mol/d or 1495 mg). In total, reducing sodium intake from the highest level to the lower level decreased blood pressure by 6.7/3.5 mmHg.
However, challenges do exist in reducing dietary sodium. Because of its presence in the food supply, many patients will have difficulty avoiding sodium without making major changes in the way they procure and prepare food. From a practical perspective, the lower level of sodium in the DASH-Sodium trial at approximately 1500 mg is equal to less than 3/4 teaspoon of salt—a relatively small amount of salt that many Americans consume in one meal. Many fast food sandwiches contain nearly two thirds of that total amount of sodium alone. Successful implementation of dietary sodium reduction typically calls for some proficiency at label reading to identify sodium content in packaged foods and limiting restaurant meals and convenience foods. Individuals must also be able to access alternatives for higher sodium products, such as no-salt added or low-sodium versions of breads, soups, canned vegetables, and sauces or condiments. One reasonable approach to recommending sodium reduction is based on the recent Lifestyle Recommendations to Reduce Cardiovascular Risk: Report of the Lifestyle Workgroup, 2013 [54]. This workgroup recommended advising patients with elevated blood pressure to consume no more than 2400 mg/day and that further blood pressure reduction can be achieved by lowering to 1500 mg/day. Even if achievement of these lower levels of sodium intake is out of reach for the individual, the workgroup recommends that blood pressure reduction can be expected if sodium intake is reduced by 1000 mg/day from the patient’s baseline intake level.
DASH Dietary Pattern
The DASH dietary pattern was originally developed for blood pressure reduction in 1999 [55]. This pattern consists of a diet rich in fruits, vegetables, and low-fat dairy foods while being low in fat content (saturated fat, total fat, and cholesterol), red meat, sweets, and sugar-containing beverages. In the original DASH trial, study participants were provided the DASH dietary pattern in daily meals, and this resulted in an average blood pressure reduction of 5.5/3 mmHg at 8 weeks. Individuals who were hypertensive at baseline and/or self-identified as African-American had greater blood pressure responses to the dietary pattern. These improvements in blood pressure occurred without change in weight or sodium reduction; weight was held stable by adjusting calorie intake, and sodium was consistent with typical American intake at 3000 mg/day.
While the DASH dietary pattern is effective alone as a strategy for blood pressure reduction, it can be easily combined with other strategies to further enhance blood pressure reduction. For example, the DASH dietary pattern can be the basis of a calorie-restricted weight reduction diet. In the nonrandomized phase 1 portion of the Lifestyle Interventions and Independence for Elders (LIFE) study, all study participants were instructed to adopt the DASH dietary pattern with a 500-kcal restriction, along with increasing physical activity by more than 180 min per week over a 26-week period [56]. The mean weight loss in this trial was 6.3 kg with 60 % of the participants losing at least 4.5 kg. Similarly, the PREMIER clinical trial, which utilized the DASH dietary pattern as part of a behavioral lifestyle intervention, had weight loss of ~ 5 kg over a 6-month period [57]. The DASH dietary pattern can also be combined with a reduced sodium intake, resulting in greater blood pressure reduction than either strategy alone. In the DASH-Sodium trial, combining the DASH dietary pattern with 2400-mg sodium intake resulted in a blood pressure reduction of 7/4 mmHg; reducing sodium to 1500 mg while consuming the DASH dietary pattern led to blood pressure reduction of 9/5 mmHg.
Potassium
In contrast to sodium, the content of potassium in foods diminishes with food processing. In most countries, the intake of potassium is low because of frequent consumption of processed foods in conjunction with a diet low in fresh fruits and vegetables. Even though the DGA recommend a potassium intake of 120 m mol/d (4700 mg) [49], the average intake in the USA is only around 65 m mol/d (2640 mg) [58]. Fruits and vegetables contribute about 20 % of total potassium intake in the typical American diet [58].
Several meta-analyses concluded that individuals with high potassium intake have lower blood pressure [59–61]. In one meta-analysis, the effect size for increased potassium intake approximated reductions of 3.5 mmHg for systolic and 2 mmHg for diastolic blood pressure [62]. The blood-pressure-lowering effect was greater for those with hypertension, with no effect found in individuals without hypertension. Aburto et al. [62] increased potassium intake to the level recommended in the DGA (up to 120 m mol/d; 4700 mg) and observed reductions in blood pressure of 7/4 mmHg. This amount of potassium intake was found to be optimal; consumption above this level did not provide additional benefit [62]. While there are no reports of adverse events resulting from high potassium intake, caution must be exercised in people with renal impairment to avoid hyperkalemia [63].
Alcohol Intake
Alcohol has a known pressor effect and increases blood pressure in a dose-dependent fashion [64]. Blood pressure begins to increase once consumption exceeds two drinks per day (a standard drink is defined as 14 g of ethanol: 12 oz of beer, 5 oz of table wine, or 1.5 oz of distilled spirits) [65]. Previous studies have shown that intake of > 210 g of alcohol per week is an independent risk factor for incident hypertension [66]. As a corollary, a decrease in alcohol consumption results in lower blood pressure. In one study, when alcohol was decreased from 350 to 70 mL/week, there was a decrease in systolic blood pressure (BP) of 3.1 mmHg, independent of changes in weight that resulted from lower caloric intake [67]. In general, men should be counseled to consume ≤ 2 drinks per day and women ≤ 1 drink per day to lower blood pressure [68]. At the same time, it is important to consider that alcohol consumption is associated with morbidity and mortality (motor vehicle accidents, absenteeism from work, disrupted family, etc.).
Weight Reduction
Elevated blood pressure is an established consequence of overweight and obesity. It is therefore not surprising that one of the associated benefits of weight reduction is lowering of blood pressure. A meta-analysis of eight studies including more than 2100 participants who were randomized to either a weight-reducing diet or a control intervention demonstrated that weight loss was consistently associated with blood pressure reductions [69]. Weight loss diets led to decrements in blood pressure of 4.5/3.2 mmHg together with a 4.0 kg decrease in body weight compared with the control groups after follow-up of 6–36 months. The results of this meta-analysis are consistent with earlier analyses suggesting that blood pressure decreased by 1.2/1.0 mmHg for every kilogram of weight lost [70]. Ultimately, a weight-reducing diet based on the DASH dietary pattern with a lower sodium intake and moderate or no alcohol intake is one of the most comprehensive strategies for producing non-pharmacologic blood pressure reduction. For the motivated patient, combining these strategies can lead to synergies of treatment and pleiotropic effects that are most effectively accomplished with lifestyle therapy techniques.
Physical Activity
Physical activity is a cornerstone of the treatment of hypertension using lifestyle therapy. Many major health organizations, including the American Heart Association (AHA), the American College of Cardiology, and the Centers for Disease Control, emphasize the importance of physical activity training for lowering resting blood pressure in hypertensive and prehypertensive individuals [71]. Aerobic-based activities, such as walking, cycling, and swimming, are prescribed with the goal of achieving 30–60 min of continuous or intermittent aerobic exercise on most days of the week at 40–60 % of heart rate reserve or maximal oxygen uptake [72]. The guidelines from the American College of Sports Medicine (ACSM) also promote supplementing aerobic exercise with resistance training for 2–3 days a week with at least one set of 8–12 repetitions at 60–80 % of the one-repetition maximum (1-RM) targeting the major muscle groups [72]. In examining data from more than 5000 individuals in a meta-analysis, endurance training reduced blood pressures in hypertensive individuals by 8.3/5.2 mmHg (systolic/diastolic) [73]. The values were less for prehypertensive individuals at 4.2/1.7 mmHg. These conclusions are consistent with other studies testing similar physical activity interventions [74]. Several studies also suggest that the rate of developing hypertension in prehypertensive individuals is reduced in individuals engaged in more physical activity leading to greater fitness [74–76].
The modalities and intensity of the physical activity prescription should accommodate the personal preferences and capabilities of the patient, even though the ideal intensity of exercise will not be possible. Nevertheless, lower amounts of exercise can still be beneficial. Incorporating 10-min bouts of exercise at least three times a day for 5 days a week is also efficacious for blood pressure lowering [77]. This pattern of activity is associated with high adherence and is more practical in the normal daily routine of many individuals. Dynamic resistance exercise training also provides reductions in blood pressure, although the changes are smaller than with endurance exercise [78, 79]. Participating in walking groups also confers health benefits, including reducing blood pressures by 3.7/3.1 mmHg [80]. These studies demonstrate the benefits that can be achieved with less traditional exercise programs and importantly, in activities that have high adherence rates.
Treatment of Dyslipidemia
The dyslipidemia associated with insulin resistance and cardiometabolic risk is characterized by elevated triglyceride levels, as a result of an excess of large triglyceride-laden very low-density lipoprotein particles (VLDL), as well as decreased concentrations of high-density lipoprotein cholesterol (HDL-C) [81]. Levels of low-density lipoprotein cholesterol (LDL-C) may not be primarily affected; however, the cholesterol is packaged into smaller denser low-density lipoprotein (LDL) particles [81], which are more atherogenic [82–85]. High triglycerides and low HDL-C constitute two of the five diagnostic criteria for the MetS, which is associated with increased risk of CVD. While there is accumulating evidence that elevated triglycerides constitute a direct risk factor for CVD, it is uncertain whether the associations are due to indirect effects or links to other lipoprotein abnormalities and risk factors. This applies to the elevated concentrations of small dense LDL particles that confer increased risk of CVD events independent of overall LDL-C levels [83–85]. High levels of LDL-C represent a major risk factor for CVD and can occur in patients with or without insulin resistance and cardiometabolic risk. Therefore, LDL-C should be brought to recommended targets in all individuals, particularly in those patients with cardiometabolic risk who are at additional risk for CVD [86–88] .
Expert panels and professional organizations have established evidence-based treatment targets for lipids and lipoproteins based on prevention of CVD [86–88]. Lifestyle therapy can effectively help achieve these therapeutic targets; however, the approaches to dietary therapy require modification based on etiology. Specifically, the macronutrient composition of the diet should be modified based on the degree of hypertriglyceridemia and whether the primary abnormality being treated is elevated LDL-C [87–89].
Dyslipidemia of Insulin Resistance
The dyslipidemia of insulin resistance is responsive to lifestyle therapy including alterations in dietary macronutrient composition, weight loss in patients with overweight or obesity, physical activity, restriction of alcohol, and limited intake of sugars and refined carbohydrates. Healthy meal plans (Table 23.4) can be used effectively to treat dyslipidemia under energy-balanced conditions in patients who are normal weight, or in reduced calorie format for weight loss in patients who are overweight or obese. However, not all healthy meal patterns are appropriate for all patients with dyslipidemia. The dietary prescription will be different depending on the degree of elevation in fasting serum triglyceride [90], which reflects differences in pathophysiology as illustrated in Table 23.5.
Patients with Triglyceride Levels Below 500 mg/dL
Patients with triglyceride levels below 500 mg/dL have borderline-high or high degree of hypertriglyceridemia. These triglyceride levels typically characterize patients with insulin resistance, cardiometabolic risk , MetS, and prediabetes and are largely due to excess production of large triglyceride-enriched VLDL particles by the liver. Since carbohydrates can drive hepatic VLDL production, dietary carbohydrates, particularly sugars and refined carbohydrates, should be reduced and replaced with unsaturated fats and protein [54, 91–95]. Alcohol can also stimulate VLDL production and all patients should restrict alcohol intake (≤ 1 drink per day). Triglyceride levels can be markedly elevated in some patients following alcohol ingestion, and these individuals should refrain from alcohol entirely if this pattern is established.
Regarding the selection of healthy meal plans , low-fat diets should be used cautiously and modified to severely limit simple sugars, refined carbohydrates, and any foods or meals that produce a substantial hyperglycemic response. Under energy-balanced or weight-stable conditions, progressive substitution of carbohydrates by fat will produce further reductions in triglycerides and increases in HDL-C in patients with fasting triglycerides < 500 mg/dL [96]. In particular, dietary intake of sugar, white flour products, fruit juices, and non-diet sodas can dramatically increase triglycerides, while restricting simple carbohydrates and increasing dietary fiber can be important adjuncts that lower triglycerides. On the other hand, low-carbohydrate diets should be modified to limit saturated fats and avoid trans-fat in favor of monounsaturated and polyunsaturated fat . Mediterranean diets are well suited to accommodate an optimal macronutrient composition [97–100], as can dietary prescriptions based on the DASH [55] and other meal plans, which are modified to limit refined carbohydrates and emphasize high fiber and unsaturated dietary fat.
Patients with Triglyceride Levels at 500 mg/dL or Higher
Patients with triglycerides ≥ 500 mg/dL have very high or severe hypertriglyceridemia. In these patients, clearance mechanisms for triglyceride-enriched lipoproteins are saturated and chylomicronemia is likely or can be rapidly induced upon consumption of fatty meals. Abnormal clearance of triglyceride-enriched lipoproteins can result from defective hydrolysis of triglycerides by lipoprotein lipase, abnormalities in hepatic uptake of chylomicron and VLDL remnants, or abnormalities in apolipoproteins regulating VLDL metabolism (apoC-II, apoC-III, and apoE). These patients are at risk of pancreatitis when triglyceride levels approach 1000 mg/dL and, at higher levels, can experience eruptive xanthoma and lipemia retinalis. These patients should be placed on a low-fat diet, less that 15–25 % of total calories, to reduce the release of new chylomicron particles from the gut into the circulation [101, 102]. Therefore, low-carbohydrate diets should generally be avoided since these diets cannot often accommodate the required reductions in dietary fat. Refined carbohydrates and simple sugars should also be avoided in such cases since these nutrients can accelerate hepatic production of VLDL. Thus, the Mediterranean, DASH, low-fat, volumetric, and vegetarian healthy meal plans can serve as the basis for an optimal macronutrient composition.
Omega-3 polyunsaturated fatty acids (PUFAs), derived mainly from fatty fish and some plant products (flax seed), have a unique impact to decrease triglycerides. In large amounts (2–6g/day), these fatty acids can lower triglycerides 40 % or more. These doses are difficult to achieve in the diet, and purified capsules are usually necessary. Fish that contain the highest levels of omega-3 fatty acids are sardines, herring, and mackerel, and daily servings of 0.5–1 lb or more may be necessary to achieve intake levels required to predictably reduce triglycerides. In patients with very high or severe hypertriglyceridemia, it is imperative to keep triglyceride levels below 500 mg/dL to minimize the risk of pancreatitis. In fact, lifestyle therapy will often need to be combined with triglyceride-lowering medications to achieve this biochemical target.
Patients with hypertriglyceridemia should be evaluated for secondary causes. These can include pregnancy, endocrine disorders (e.g., hypothyroidism and hypercortisolism), nephrotic syndrome, lipodystrophy, and drug-induced hyperlipidemia (e.g., estrogens, alcohol, thiazide diuretics, beta-blockers, bile acid sequestrants, antihuman immunodeficiency virus medications, antipsychotics, and antidepressants). Patients with hypertriglyceridemia may have genetic defects in lipid metabolism (e.g., familial hypertriglyceridemia, familial combined hyperlipidemia, and dysbetalipoproteinemia).
Regardless of the degree of hypertriglyceridemia, weight loss is advocated for patients who are overweight or obese [94, 95]. The initial weight loss target should be 5–10 % of body weight. However, greater degrees of weight loss can achieve progressive improvements in dyslipidemia . Hence, weight loss programs should be intensified when initial efforts do not achieve therapeutic targets. Healthy meal plans appropriate for patients with any degree of triglyceride elevation can be employed in a reduced calorie format. In the range of 5–10 % weight loss has been shown to amplify the benefits of changes in macronutrient composition with further reductions in triglycerides, increments in HDL-C, and modest decreases in LDL-C in many studies [102, 103]. Furthermore, there are beneficial effects of weight loss on LDL subclasses characterized by reductions in small dense LDL particle concentrations and an increase in medium and large LDL particles, coupled to a mean increase in LDL particle size and reductions in total LDL particle concentration [104–108]. In a study by Richard et al. [109], a Mediterranean diet without weight loss lowered LDL-C, apoB-100, and the percentage of small dense LDL particle associated with an increase in the fractional clearance of LDL and VLDL; additionally, lipoprotein values were further improved when this Mediterranean diet was combined with weight loss. Thus, the effects of weight loss on dyslipidemia represent a very favorable profile regarding a reduction in CVD risk.
Exercise is an integral component of lifestyle therapy independent of weight loss. The exercise prescription should be sufficient to promote cardiometabolic health (Table 23.6). The toning of large muscles groups (abdomen, back, legs, and arms) and exercise-induced improvements in insulin sensitivity augment clearance of triglyceride-rich lipoproteins via induction of lipoprotein lipase and therefore lower triglycerides [110–113]. In addition, when used together with weight loss, exercise leads to substantial and disproportionate increments in HDL-C [106].
Elevated LDL
For LDL-C lowering, the AHA recommends reductions in saturated fat intake to < 7 % of calories and elimination of trans-fat together with a healthy meal plan that emphasizes whole grains, vegetables, fruits, poultry and fish, low-fat dairy products, legumes, nuts, and nontropical vegetable oils with limited intake of red meats, sweets, and sugar-sweetened beverages [54]. The latest DGA have withdrawn the previously recommended limits on cholesterol (i.e., < 300 mg/day) due to lack of evidence that consumption of dietary cholesterol can affect serum cholesterol [114]. Nevertheless, it is prudent to avoid excessive cholesterol intake in patients with high LDL-C and CVD risk. These dietary recommendations can be adapted to meet personal and cultural food preferences in the context of healthy meal plans such as the DASH, low-fat, Mediterranean, and vegetarian diets, among others. Moderate to vigorous physical activity occurring over 3–4 sessions per week and totaling at least 150 min per week can also result in LDL-C lowering. In patients with overweight or obesity, weight loss of 5–15 % will lead to modest reductions in LDL-C; however, importantly, weight loss will also decrease the percentage of small dense LDL and overall LDL particle concentration [105–109]. Dietary adjuncts for cholesterol lowering include plant sterols and stanols (2–3 g/d), as well as viscous fibers (5–10 g/d). Dietary and other lifestyle recommendations should be reinforced in the context of a structured lifestyle intervention and referrals to a registered dietitian (RD) and exercise specialist are advisable for many patients. Given the proven cardioprotective effects of statin therapy, high-risk patients with MetS, prediabetes, hypertension, and/or dyslipidemia should be strongly considered for statin therapy in addition to lifestyle therapy, particularly if the LDL-C is ≥ 100 mg/dL [86–88]. The Jupiter study demonstrated reductions in CVD events in patients with elevated C-reactive protein, most of whom had MetS, with statin-induced lowering of LDL-C to below 70 mg/dL [115].
The dietary prescription can sometimes be a double-edged sword when treating patients with mixed hypertriglyceridemia (i.e., elevated triglycerides and LDL-C). When triglycerides are markedly elevated (> 500 mg/dL), indicative of defective clearance of triglyceride-enriched lipoproteins, or when treating high LDL-C, the recommended low-fat diet will decrease the appearance of chylomicrons, circulating triglyceride concentrations, and LDL cholesterol. However, in the setting of stable weight and moderately elevated triglycerides, a low-fat diet with a de facto greater proportion of carbohydrate calories will stimulate hepatic production of VLDL, thereby increasing triglycerides and decreasing HDL-C. Therefore, in mixed hyperlipidemia, diets primarily designed to reduce LDL-C and chylomicrons can also increase triglycerides and decrease HDL-C. In such cases, the prescribed macronutrient composition may require a balanced or intermediate approach. Furthermore, a diet emphasizing healthy fat (i.e., monounsaturated and polyunsaturated fat) can be beneficial since this can promote lowering of triglycerides and increasing of HDL-C, without increments or even modest decreases in LDL-C [97–100].
Lifestyle Therapy: An Approach Emphasizing Weight Loss
In considering the diet component of lifestyle therapy with an emphasis on weight loss, both the macronutrient composition of the diet and daily calories can be individualized to achieve weight loss and the overall goals delineated in Table 23.3. There is a relative wealth of data addressing diet during the initial active phase of weight loss. Most of these clinical trials are conducted over 1 year or less with a few studies lasting 2 years. During the initial phase of active weight loss, patients are hypocaloric. Over time, the weight equilibrates at a new lower level, and patients convert to a chronic phase consuming an energy-balanced diet in an effort to maintain weight loss. Furthermore, the chronic phase extends over most of the lifetime of the patient. Patients with cardiometabolic risk require lifelong therapy, and most of the time patients will be in energy balance while maintaining a reasonably stable body weight. This is true, of course, in patients with normal body weight, as well as in patients with overweight or obesity who are post weight loss. Unfortunately, there is a dearth of rigorous data to guide diet during the chronic phase of weight loss maintenance, particularly with respect to clinical outcomes. Some of the best data to inform the chronic diet plan examine the effects of isocaloric substitution or enrichment of various macronutrients on insulin sensitivity and cardiometabolic risk factors [116]. Therefore, diets will be discussed in the context of both the initial phase of active weight loss (e.g., the first year) and the chronic phase of maintenance of weight loss over years to decades when patients are largely in energy balance.
Diet During the Initial Phase of Weight Loss (First Year)
Macronutrient Composition and Healthy Meal Plans
The notion that changes in macronutrient composition can be used to promote weight loss and enhance insulin sensitivity, independent of overall calorie ingestion, has received a great deal of attention in the popular press. Various low-carbohydrate (Atkin’s Diet), ‘right’ carbohydrate (The Zone diet, the South Beach diet), and low-fat diets (Ornish Diet) have been promulgated by best-selling books and have gained devotees. There must exist a caloric deficit for weight loss to occur, and randomized trials do not show that any one of these diets is more effective than the other in promoting long-term weight loss. Rather, success depends on the degree to which patients adhere with the meal plan based on personal and cultural food preferences [117]. Regarding treatment of insulin resistance and cardiometabolic risk, there are multiple healthy meal plans that can be delivered in a reduced calorie format while assuring adequate intake of required nutrients as shown in Table 23.4. Healthy meal plans include low-carbohydrate, low-fat, Mediterranean, volumetrics (e.g., EatRight), low-glycemic index (GI), DASH, and vegetarian diets. Any of these meal plans can generally be employed in the initial weight loss phase and will often require the participation of a dietitian, and, in some patients, monitoring of electrolytes, blood pressure, fasting glucose, and lipids.
Of the diets with variable macronutrient composition, the question remains as to which is most effective in the initial phase of weight loss. All diets can safely be used to achieve weight loss. In randomized head-to-head comparison studies, after 1 year, differences in weight loss among individual diets with varying macronutrient composition are minimal [117]. As an example, in some studies, individuals with higher initial weights, randomized to a low-carb diet, had greater weight loss at 6 months, compared with low-fat or Mediterranean diets but similar weight loss at 1 year. What is clear is that the patients who lose the most weight are those who maintain adherence with the prescribed meal plan [117]. Therefore, personal and cultural food preferences should be discussed with each patient to guide an optimal and more personalized healthy meal plan for a durable effect. Macronutrient composition can also be adjusted to include foods that match these personal and cultural preferences to assure adequate intake of required nutrients.
Low-Carb Versus Low-Fat Diets
Low-carbohydrate (low-carb) diets can also be termed high-fat diets since it is impractical to make up the carbohydrate caloric deficit with dietary protein. Low-carb high-fat diets were first described by William Banting in 1863 and were used extensively prior to the discovery of insulin by Frederick Allen and others to treat type 1 diabetes. Nevertheless, it is clear that low-carb diets can be used safely without negative effects and often with improvements in insulin sensitivity, glycemia, lipid status, blood pressure, and body weight. However, two considerations are important. First, relevant studies have generally not been extended passed 1 or 2 years such that we have little or no data on long-term outcomes. Second, these studies often ignore the composition of dietary fat, which can be clinically important.
Two landmark studies are illustrative regarding patient outcomes on a low-carb diet. Foster et al. [123] compared a low-carb ‘Atkins’ diet against a conventional low-fat (25 % of calories) reduced-calorie diet in otherwise healthy obese subjects. The low-carb diet produced a greater weight loss than the low-fat diet after six months (6.7 versus 2.7 kg) but at 1 year the amount of weight loss was not significantly different between the two groups. Of note, about 40 % of the 63 randomized subjects did not finish the study. Insulin sensitivity was assessed using the quantitative insulin sensitivity check index based on fasting glucose and insulin concentrations; this showed an increase in insulin sensitivity at 6 months but no change from baseline at 1 year in both dietary subgroups, with no significant differences between the subgroups. LDL-C and total cholesterol were lower at 3 months in the low-fat diet subgroup, while HDL-C was higher and triglycerides lower at 1 year in the high-fat diet subgroup. In the second study, Samaha et al. [124] compared the effects of a low-carb versus a low-fat (≤ 30 g/day) National Heart Lung and Blood Institute diet designed to create a caloric deficit of 500 kcal/day. Their subjects were severely obese (mean BMI 43 = kg/m2) and most were African-Americans, hypertensive, and characterized by the presence of either T2D or the MetS. In this 6-month study, subjects on the low-carb diet lost more weight than those on the low-fat diet; however, the amount of weight loss was low and the drop-out rate was again very high, particularly in the low-carb group (47 versus 33 % in the low-fat diet group), indicative of greater nonadherence. LDL-C and HDL-C were not affected by the diets although triglycerides were lowered in the high-fat diet group. The authors also emphasized that the low-carb diet led to greater improvements in insulin sensitivity than the low-fat diet group, but these effects were minimal and the authors again used a suboptimal index based on fasting glucose and insulin levels as a measure of insulin sensitivity.
The studies by Foster et al. [123] and Samaha et al. [124] did not control for the types or composition of fat or carbohydrates in the diets, which could have affected study end points. For example, Lovejoy et al. [125] used the clamp technique to show that a 3-week high-fat diet (50 % fat, 35 % carbohydrate, and 15 % protein) did induce relative insulin resistance compared with an isocaloric low-fat diet (20 % fat, 55 % carbohydrate, and 15 % protein); however, this could be explained by a higher proportion of saturated fatty acids in the high-fat diet. As discussed below, variations in the types of fats in the low-carb diets (e.g., amount of monounsaturated fatty acids, MUFAs) or types of carbohydrate in the low-fat diets (e.g., fiber, starch, and sugar), or other unknown factors, may have influenced study parameters and contributed to inconsistent results with respect to weight loss, insulin sensitivity, and lipid levels.
Some low-fat diets emphasize ad libitum intake of foods with low caloric density and with high fiber and water content [126]. This approach can also be used effectively to promote weight loss and benefit patients with cardiometabolic risk . As discussed above, the DASH diet is relatively enriched in carbohydrates and reduced in fat . Another example is the EatRight® program employed at the University of Alabama at Birmingham [119–121]. This program emphasizes the ingestion of large quantities of high bulk, low-energy-density foods (primarily vegetables, fruits, high-fiber grains, and cereals) and moderation in high-energy-density foods (meats, cheeses, sugars, and fats). This approach produces equal satiety at reduced energy intake compared with a high-fat diet comprising energy-dense foods. EatRight participants loose an average of 6.3–8.2 kg by the end of the 12-week program, and overall, 53 % of participants maintain their reduced weight or continue to lose weight 2 years later, while only 23 % regain all their lost weight [120].
Alterations in Dietary Carbohydrate and the GI
Dietary carbohydrate composition and distribution, as opposed to total dietary caloric content, can influence body weight and insulin sensitivity. The GI has been established to physiologically classify carbohydrates based on post-meal glycemic responses and is a measure of the degree to which a carbohydrate-containing food raises blood glucose in relationship to a reference food such as white bread or glucose. The South Beach and Zone diets advocate the ‘right kind’ of carbohydrates characterized by a low GI. The originators of these diets purport that high GI responses are central to mechanisms promoting weight accretion; however, the data are equivocal as to whether high-GI diets promote weight gain [127]. Short-term studies indicate that consumption of high-GI carbohydrates has less of an effect to suppress appetite and a diminished ability to induce satiation and satiety than foods with lower GI [128, 129]. However, long-term controlled clinical trials assessing effects of low- versus high- GI diets on body weight are lacking. Furthermore, because multiple dietary and physiological factors affect GI, its validity as a meaningful way to characterize food has been questioned and its implementation in nutritional recommendations is problematic [130]. A recent evidence-based report from the WHO found that the only convincing dietary factor protecting against weight gain and obesity was a high dietary fiber intake [131]. Fiber has consistently been shown to improve insulin sensitivity and lipid levels in studies comparing low and high fiber intakes [132, 133]. Patients should be encouraged to consume 25–30 g fiber/day with an emphasis on soluble fiber (7–13 g) for improving cardiometabolic risk factors .
Meal Replacements
Meal replacements can be recommended for weight loss as an option that provides structure for reducing calorie consumption [134]. These products can enhance adherence for many patients due to the known caloric content that eliminates guesswork, provision of required nutrients, and convenience. Optimal products in prediabetes are characterized by high protein, fiber, complex carbohydrates or modified slowly digesting carbohydrates with no refined sugars, low saturated fat, limited sodium, and no trans-fat . Meal replacements usually contain 175–250 kcal per serving and can be employed during the active phase of weight loss and during chronic weight loss maintenance. During active weight loss, meal replacements can be employed in very low-calorie diets (VLCD) or in low-calorie and reduced-calorie diets to comprise one or two meals/day with a third meal of portioned-controlled food. Several studies have demonstrated greater weight loss with incorporation of meal replacements when compared with reduced-calorie diets of conventional foods or with programs using portion-controlled servings of conventional foods or provision of detailed menus.
The Caloric Prescription and Desired Degree of Weight Loss
A caloric deficit is the essential component and a sine qua non of weight loss. During the active phase of weight loss, a reduced-calorie diet where the caloric deficit is ~ 500 cal/day is generally recommended. However, the HCP can opt for greater degrees of caloric reduction, including VLCD defined by total daily calories of 800 or less. One strategy for developing a caloric prescription that will more predictably achieve the desired amount of weight loss is to estimate the basal metabolic rate (kcal/day) using equations based on height, weight, gender, and age [135–138] or using an indirect calorimeter. The caloric deficit is subtracted from the resting metabolic rate to determine total daily calories and can be individualized to achieve the desired rate and extent of weight loss. In patients with cardiometabolic risk, the goals include the prevention of T2D and improvements in hypertension and dyslipidemia (Table 23.3). Most guidelines for obesity recommend weight loss of 5–10 % since this is sufficient to improve multiple weight-related complications. However, as discussed above, maximal prevention of T2D was observed at 10 % weight loss which reduced incident diabetes by ~ 80 %, regardless of whether this was achieved via lifestyle therapy [9, 10], weight loss medications [12, 13], or bariatric surgery [41–43]. In contrast, no thresholds for maximal benefits were observed with the progressive weight loss from 5 to > 15 % in lowering systolic and diastolic blood pressure, increasing HDL-C, and decreasing triglycerides in the LookAHEAD study [139]. For improvements in dyslipidemia and hypertension, therefore, greater weight loss provides for additional clinical benefits up to and beyond 15 % weight loss.
Diet During the Chronic Maintenance Phase of Weight Loss (Years to Decades)
A Healthy Meal Plan for the Long Term
After active weight loss, patients will need an energy-balanced prescription to maintain the new lower body weight and avoid weight regain. This can be problematic since energy expenditure decreases following weight loss. Therefore, resting energy equations based on height and weight will predictably overestimate the number of calories needed for weight stabilization. For this reason, it is wise to reduce daily calories by 100 kcal/day below the calculated value and then to follow the patient making further reductions in the caloric prescription based on changes in body weight. Indirect calorimetry can be helpful at this stage to provide a more accurate estimate.
Following the active weight loss (~ 1 year), patients will equilibrate at a lower body weight, and it is incumbent upon the patient and health-care team to maintain the weight loss. At this point, the patient will essentially be in energy balance, and the macronutrient composition might have different effects in cardiometabolic risk and T2D than during hypocaloric feeding. Various healthy meal plans have been relatively well studied during the active phase of weight loss; however, unfortunately, little long-term data exist beyond 1 or 2 years on these diets. In particular, the effects on long-term clinical outcomes, such as the progression to T2D and CVD disease events, as well as the impact of the various diets on cardiometabolic pathophysiology and disease biomarkers , are very important but largely unknown. The question regarding optimal diet is also relevant to normal-weight patients with cardiometabolic risk who do not require weight loss.
If there is a lack of data addressing long-term outcomes, what evidence can be used to guide the dietary prescription? One consideration was highlighted in selecting the diet for active weight loss, namely, the diet that could best accommodate personal and cultural preferences resulting in greater rates of compliance. This remains an important consideration during chronic weight maintenance. However, the second consideration is a large body of data indicating that isocaloric substitution of macronutrients can influence insulin sensitivity and CVD risk factors [116]. Since insulin resistance is key to the pathophysiology and progression of cardiometabolic risk, it is reasonable to augment macronutrients that enhance insulin sensitivity and reduce macronutrients that promote insulin resistance, as summarized in Table 23.7.
Saturated Versus Polyunsaturated Fat
The composition of dietary fatty acids can modulate insulin sensitivity and CVD risk factors independent of total fat or total calorie intake [140, 141]. With respect to saturated fat, epidemiological studies show that high intake of total and saturated fat intake is associated with insulin resistance [141]. Multiple cross-sectional studies have similarly found that intake of both saturated and trans-fatty acids is associated with hyperinsulinemia and risk of T2D, independent of body adiposity [142, 143]. High intake of PUFAs does not appear to have the same adverse effects and may even result in an increase in insulin sensitivity [144]. For example, Summers et al. [145] studied the effect of substituting dietary saturated fat with PUFA on insulin sensitivity in healthy, obese subjects with T2D. Their findings demonstrated that an isocaloric diet enriched in PUFA resulted in both an increase in insulin sensitivity and a lowering of LDL-C, when compared with a diet rich in saturated fatty acids. However, it was not possible in this study to conclude whether it was the increase in dietary PUFA or the decrease in saturated fat that produced the relative benefits in the PUFA diet subgroup. Diets enriched in PUFA have not consistently been shown to improve insulin sensitivity [146] and long-term intervention trials have not been conducted. Discrepancies in the short-term studies are often attributable to the failure to control for dietary fatty acid and carbohydrate composition (e.g., MUFA), total calories, physical activity, and population characteristics such as age, gender, and adiposity.
Omega-6 fatty acids and omega-3 fatty acids are the two important types of dietary PUFA. While evidence suggests that omega-3 fatty acids, namely eicosapentaenoic acid, docosahexaenoic acid, and α-linolenic acid, from fish or fish oil dietary supplements may help prevent CVD [147], the effects of omega-3 and omega-6 fatty acids on glucose homeostasis are inconsistent [143, 144, 148]. However, while omega-3 fatty acids may not influence insulin sensitivity, doses of 2–6 g/day are effective in lowering circulating triglyceride levels. People are encouraged to consume whole food sources of omega-3 fatty acids, specifically fatty fish at least twice a week. Fatty fish include salmon, mackerel, sardines, tuna, trout, and herring.
Monounsaturated Fatty Acids
Beneficial effects of a high-MUFA diet on glycemic control in T2D have been demonstrated in a meta-analysis of randomized trials using isoenergetic high-MUFA diets [149]. These trials show that isocaloric substitution of MUFA for saturated fat [150], or even substituting MUFA for carbohydrates, can have positive effects on insulin sensitivity, lipids, and cardiometabolic health [151]. Accordingly, the ADA essentially places no restrictions on dietary MUFAs within the limits of the caloric prescription in diabetes.
Fiber
On balance, available data suggest that dietary fiber, rather than carbohydrate quantity or dietary GI per se, is directly responsible for any effects of carbohydrates on insulin sensitivity. In a randomized crossover study comparing isocaloric high- versus low-GI diets, there was no observed benefit of the low-GI diet on insulin sensitivity [152]. However, a low-GI diet with a greater amount of fiber and whole-grain products seemed to improve glycemic and insulin responses and lowered the risk of T2D [133], indicating that the fiber content in low-GI foods may play a metabolic role. In support of this contention, studies on the effects of dietary intake of fiber, particularly whole-grain foods, have been fairly consistent in demonstrating an effect to enhance insulin sensitivity [153–155].Isocaloric substitution experiments indicate that diets enriched in MUFAs, PUFAs, whole grains, and high fiber result in an increase in insulin sensitivity and improvements in lipids, while enrichment in saturated and trans-fats, refined grains, and reduced fiber promote insulin resistance and dyslipidemia (Table 23.7). These data are relevant in the selection of a healthy meal plan during isocaloric periods in patients with cardiometabolic risk. If a low-carbohydrate diet is to be used for chronic weight loss maintenance, it would be important to minimize saturated fat in favor of MUFA, and this can be challenging given the amount of total fat consumed under energy-balanced conditions. Due to the limited number of foods highly enriched in MUFA (e.g., olive oil, avocados, and nuts), a concerted effort working with a dietitian is recommended in order to maintain a high MUFA to saturated fat ratio (≥ 2:1) and at the same time assure a wide range of diet choices. Furthermore, lipid panels should be followed closely for changes in LDL-C, HDL-C, and triglycerides since there is lack of data on the long-term effects of a low-carbohydrate diet under isocaloric conditions. On the other hand, low-fat diets, including volumetrics, vegetarian, and DASH diets, are relatively high in carbohydrates, which could have the effect of worsening glycemia in patients with prediabetes. Complex carbohydrates, high fiber intake, and low-GI meals should be emphasized.
Mediterranean Diets
One meal plan that can be effective in patients with cardiometabolic risk is represented by the Mediterranean diet, characterized by a reliance on olive oil as a fat source, which contains the MUFA oleic acid as ~ 75 % of fatty acids. There are variations in the Mediterranean diet as consumed in various regions and countries; however, they are discussed here in terms of commonalities relevant to cardiometabolic risk reduction. In addition to olive oil, these diets consistently feature a high intake of vegetables, legumes, nuts, and fruits; a low intake of saturated fat; low-to-moderate consumption of dairy products; low intake of meat and poultry and relatively high intake of seafood; and regular consumption of red wine at meals in most Mediterranean cultures. This diet consists entirely of unprocessed foods and is rich in fiber, antioxidant polyphenols, vitamins and minerals, and phytochemicals. Furthermore, Mediterranean diets have been shown to have favorable clinical effects in patients with cardiometabolic risk and insulin resistance, including long-term outcome studies demonstrating prevention of T2D and primary and secondary prevention of CVD [97–99, 156–164]. Epidemiologically, Mediterranean diets have been known to be associated with reduced CVD and mortality when compared with diets consumed in northern European countries. The Lyon Diet Heart Study is a clinical trial that assessed the efficacy of Mediterranean diets for the secondary prevention of CVD events. Patients who have had a previous myocardial infarction were randomized to a Mediterranean diet or a diet typically consumed in northern countries, such as the UK [157, 158]. After 4 years follow-up, the Mediterranean diet group had reduced rates of re-infarction and mortality. Mediterranean diets have also been shown to prevent MetS and reduce rates of progression to T2D [160–164]. Thus, Mediterranean diets are a highly rationale choice as the dietary component of long-term lifestyle therapy in patients with cardiometabolic risk.
Physical Activity
Increased physical activity is an important component of lifestyle therapy in cardiometabolic risk. Regular exercise by itself [165, 166] or as part of a comprehensive lifestyle plan [7–11] can prevent progression to T2D in high-risk individuals. Structured exercise improves fitness , muscle strength, and insulin sensitivity [167–169]. In the context of an overall lifestyle intervention, regular exercise can contribute to weight loss and prevention of weight regain, and improve CVD risk factors such as lipids and blood pressure [7–11]. Studies have demonstrated beneficial effects of both aerobic and resistance exercise and additive benefits when both forms of exercise are combined [170–172]. For cardiometabolic conditioning, the guidelines proposed by the ADA, AHA, and the ACSM are well aligned [54, 173] and are summarized in Table 23.6. Lifestyle therapy should include increased physical activity even though the patient is unable to engage in optimal physical activity. For example, studies have consistently shown that a walking program is associated with reductions in diabetes incidence [174–176]. Elderly patients or persons with disabilities should try to approach levels of activity in the guidelines to the extent possible; however, even reduced activity regimens should be encouraged. Reductions in sedentary behavior can also be helpful (e.g., duration of sedentary periods lasting less than 90 min and interrupted by periods of activity) [177]. Clearly, the HCP and the patient should together establish the exercise prescription with the goal for long-term compliance. Screening for coronary artery disease should also be performed in patients at risk [178]. Table 23.6 describes options for the exercise prescription as well as general principles and behavioral strategies to promote compliance.
Lifestyle Therapy in Patients Treated with Weight Loss Medications or Bariatric Surgery
Lifestyle therapy is also a critical component of care in combination with weight loss medications and bariatric surgery in the treatment of patients with cardiometabolic risk and obesity. Lifestyle therapy alone does not result in sustained weight loss in many patients due to pathophysiological mechanisms operative in obesity as a disease [179–185]. Weight loss medications [13, 186–189] when used as adjunctive therapy to lifestyle interventions provide for greater weight loss that might be required for optimal prevention of T2D and for improvements in hypertension and dyslipidemia [12, 13, 16]. Lifestyle therapy is also critical in bariatric surgery patients both pre- and postoperatively for optimal clinical outcomes and for preventing weight regain following the procedures. This approach must be balanced against the inherent risks of surgical complications and mortality, as well as potential nutritional deficiencies, weight regain in some patients, and the need for lifelong lifestyle support and medical monitoring [190]. Nutrition therapy in these postoperative patients must guard against nutritional deficiencies and include supplementation of micronutrients including iron, calcium, vitamin D and other fat-soluble vitamins, B vitamins (to include thiamine, folic acid, and B12), and minerals (copper, zinc, selenium) [190].
Final Summary Recommendations
-
1.
Cardiometabolic risk is represented by a spectrum of disease findings and markers with common pathophysiological mechanisms, beginning early in life with relative insulin resistance, progressing to clinically identifiable states of high risk, namely prediabetes and MetS, and culminating in T2D, CVD disease events, or both in single patients.
-
2.
Lifestyle therapy is highly effective in achieving therapeutic goals for cardiometabolic risk: (i) prevent progression to T2D, (ii) control glycemia to prevent microvascular complications in prediabetes, (iii) improve the CVD risk factor profile and treat hypertension and dyslipidemia, and (iv) improve functionality and quality of life.
-
3.
A new reconfigured approach to lifestyle therapy is proposed for overweight/obese patients with cardiometabolic risk, which emphasizes weight loss as a primary therapeutic strategy for prevention and treatment. This approach to lifestyle therapy incorporates evidence-based practices involving diet, physical activity, behavioral interventions, and multidisciplinary care, with demonstrated effectiveness for weight loss.
-
4.
Weight loss in overweight/obese individuals is highly effective in preventing progression to T2D and in the treatment of hypertension and dyslipidemia. Weight loss of 10 % is optimal for the prevention of T2D in high-risk patients with prediabetes or MetS.
-
5.
Nutritional therapy for the active phase of weight loss (~first year) is accomplished using any one of several healthy meal plans , selected on the basis of personal and cultural preference, and delivered as a very low-calorie , low-calorie, or reduced-calorie diet.
-
6.
The lifestyle therapy includes physical activity that optimally encompasses both aerobic and resistance exercise and a reduction in sedentary behavior . However, the prescription for physical activity must be tailored to the preferences and capabilities of patients with T2D and take into account the presence of diabetes-related complications.
-
7.
During the chronic phase of weight loss maintenance (years–decades) when patients are in energy balance , there are little data indicating which macronutrient composition may be optimal with regard to long-term safety and clinical outcomes. Given the central role of insulin resistance in cardiometabolic risk, the rational choice is to emphasize nutrients shown to enhance insulin sensitivity in isocaloric substitution studies (e.g., MUFA, fiber, whole grains, and components of Mediterranean diets), and to minimize or avoid foods that promote insulin resistance (e.g., saturated fat, trans-fat, refined grains, and components of Western diets).
-
8.
In overweight/obese patients with cardiometabolic risk, lifestyle therapy remains the cornerstone of treatment to optimize outcomes in patients treated with weight loss medications or bariatric surgery.
Case Report
A 48-year-old European-American female was referred to you by her family doctor for high fasting blood glucose. However, the patient offers the following as the chief complaint: ‘I need help with my weight. Nothing I do seems to help. I want to be a role model for my teenage daughter who also seems to be gaining weight. The whole thing makes me depressed.’
Medical History
-
1.
Gestational diabetes with birth of only child 16 years ago
-
2.
Depression, symptoms waxing and waning over the past 10 years treated with paroxetine 40 mg/day
Social and Family History
The patient is trained as a certified public accountant (CPA) and oversees accounts of two small companies largely working from her home office. She divorced her husband 5 years ago and is a single mother of one 16-year-old daughter. She leads a sedentary lifestyle but belongs to YMCA and tries to get to the gym three times a week but averages once a week. At the gym she uses weights and walks on the treadmill. She likes a cocktail early evening and has a negative smoking history . Her family history is positive only for T2D in her mother.
Exam
BMI 36 kg/m2; waist circumference 40 in.; blood pressure 148/92; trace edema in legs with varicose veins
Laboratory
Fasting glucose 114 mg/dL; HbA1C 6.0 %; lipid panel (mg/dL) shows total cholesterol 199, LDL-C 114, HDL-C 44, and TG 177; transaminases 1.5 times upper limits of normal; and calculated non-HDL cholesterol 155 mg/dL. Complete blood count (CBC), creatinine, and electrolytes are normal.
Weight History
She had a ‘normal body weight’ until her late twenties when she started to gain weight after ‘problems’ began in her marriage. After the birth of her child at the age of 32, she went on several diet plans (South Beach and then Atkins) and did lose weight temporarily but had trouble staying on diet and experienced weight regain. She enrolled in Weight Watchers and the weight loss program at the YMCA in the past, but again weight loss was followed by weight regain. She has also tried Garcinia Cambogia and Sensa without benefit. ‘I need help because I get so hungry and I can’t stay on diet for long. It makes me feel better to eat and less depressed in the short term but when I see my weight increasing I get even more depressed.’
Assessment
The patient clearly has cardiometabolic risk factors as evidenced by the fact that she meets criteria for both prediabetes due to IFG (114 mg/dL) and MetS (elevated waist circumference, low HDL-C, high triglycerides, high fasting glucose, and high blood pressures). Risk stratification using the Cardiometabolic Disease Staging System (CMDS) [1] indicates that she is in the highest risk category for future T2D and CVD mortality. The positive family history for T2D and gestational diabetes during her pregnancy 16 years ago further compound the risk for progression to overt diabetes. Based on the single, sitting blood pressure in your office you conclude that she likely has hypertension, another cardiometabolic risk factor, which you will confirm on a subsequent visit. She also displays the dyslipidemia associated with insulin resistance and cardiometabolic risk with elevated triglycerides and low HDL levels for a female. The non-HDL cholesterol is 155 mg/dL (treatment goal should be < 130 mg/dL). The fact that the non-HDL cholesterol is greater than 30 units above the level of LDL-C indicates that she has high concentrations of small dense LDL particles. Finally, her insulin resistance and obesity put her at risk of nonalcoholic fatty liver disease, and this is suspected as the explanation for the elevated transaminases.
In summary, this patient has multiple manifestations of cardiometabolic risk and is at particularly high risk of future diabetes and CVD. You could recommend medications for IGT, hypertension, and dyslipidemia, but you elect to discuss lifestyle therapy with an emphasis on weight loss with the patient since this will result in improvements in glycemia, blood pressure, and lipids.
Plan
The patient has dietary preferences for fish, poultry, and salads and tends to cook with olive oil. At home, while working as a CPA, she does snack frequently between meals, sometimes with chips and popcorn. You place her on a Mediterranean diet healthy meal plan , with 500 kcal/day energy deficit diet. You ask her to avoid between-meal snacks except that you recommend celery or cucumbers if she gets hungry between meals. You refer her to a dietitian for instructions, implementation, and follow-up. Because the patient has experienced weight regain on several dietary interventions in the past, you discuss the addition of a weight loss medication to help her adhere to the reduced-calorie meal plan and because you want to assure the achievement and maintenance of at least 10 % weight loss, which will maximize your efforts to prevent diabetes in this high-risk patient. For physical activity, you recommend taking a break at lunch and going to the YMCA three times a week and once on weekends for 40 min of brisk walking on the treadmill and support her suggestion to engage a trainer at the facility. You place her on atorvastatin 40 mg/day. You schedule her for return visit in 2 weeks.
Additional Testing
Two-hour OGTT glucose value 182 mg/dL indicative of IGT; electrocardiogram (ECG) normal; apoB-100 value of 110 mg/dL consistent with an elevated LDL particle concentration; spot urine showing normal albumin to creatinine ratio
Two Weeks Later
Patient has lost 3 lb and is excited about the meal plan, the physical activity prescription, and contact with the dietitian. Her daughter wants to join her for ‘work-outs’ at the YMCA on Saturdays. Blood pressure remains elevated at 145/92 mmHg. You add an oral weight loss medication known to suppress appetite as an adjunct to lifestyle therapy. You encourage the patient and discuss the plan to follow fasting glucose, hepatic transaminases, blood pressure, and lipids as the indicators of success for lifestyle therapy . You schedule monthly visits for the next 3 months alternating every 2 weeks with monthly visits to the dietitian.
Abbreviations
- AACE:
-
American Association of Clinical Endocrinologists
- ACSM:
-
American College of Sports Medicine
- ADA:
-
American Diabetes Association
- AHA:
-
American Heart Association
- BP:
-
Blood pressure
- BMI:
-
Body Mass Index
- CBC:
-
Complete blood count
- CMDS:
-
Cardiometabolic Disease Staging
- CPA:
-
Certified public accountant
- CVD:
-
Cardiovascular disease
- DASH:
-
Dietary Approaches to Stop Hypertension diet
- DGA:
-
Dietary Guidelines for Americans
- ECG:
-
Electrocardiogram
- ER:
-
Extended release
- HCP:
-
Health-care professionals
- HDL-C:
-
High-density lipoprotein cholesterol
- IFG:
-
Impaired fasting glucose
- IGT:
-
Impaired glucose tolerance
- IDF:
-
International Diabetes Federation
- LDL:
-
Low-density lipoprotein
- LDL-C:
-
Low-density lipoprotein cholesterol
- MetS:
-
Metabolic syndrome
- PUFAs:
-
Polyunsaturated fatty acids
- RD:
-
Registered dietitian
- VLCD:
-
Very low-calorie diets
- VLDL:
-
Very low-density lipoprotein particles
- WHO:
-
World Health Organization
References
Guo F, Moellering DR, Garvey WT. The progression of cardiometabolic disease: validation of a new cardiometabolic disease staging system applicable to obesity. Obesity. 2014;22:110–8.
Reaven GM. Pathophysiology of insulin resistance in human disease. Physiol Rev. 1995;75:473–86.
Liao Y, Kwon S, Shaughnessy S, Wallace P, Hutto A, Jenkins AJ, Klein RL, Garvey WT. Critical evaluation of adult treatment panel III criteria in identifying insulin resistance with dyslipidemia. Diabetes Care. 2004;27:978–83.
Reaven GM. Insulin resistance: the link between obesity and cardiovascular disease. Med Clin North Am. 2011;95:875–92.
Eckel RH, Grundy SM, Zimmet PZ. The metabolic syndrome. Lancet. 2005;365:1415–28.
Lorenzo C, Okoloise M, Williams K, Stern MP, Haffner SM, San Antonio Heart Study. The metabolic syndrome as predictor of type 2 diabetes: the San Antonio heart study. Diabetes Care. 2003;26:3153–9.
Pan XR, Li GW, Hu YH, et al. Effects of diet and exercise in preventing NIDDM in people with impaired glucose tolerance. The Da Qing IGT and Diabetes Study. Diabetes Care. 1997;20:537–44.
Tuomilehto J, Lindstrom J, Eriksson JG, et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med. 2001;344:1343–50.
Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393–403.
Hamman RF, Wing RR, Edelstein SL, et al. Effect of weight loss with lifestyle intervention on risk of diabetes. Diabetes Care. 2006;29:2102–7.
Laaksonen DE, Lindstrom J, Lakka TA, et al. Physical activity in the prevention of type 2 diabetes: the Finnish diabetes prevention study. Diabetes. 2005;54:158–65.
Garvey WT, Ryan DH, Henry R, Bohannon NJ, Toplak H, Schwiers M, et al. Prevention of type 2 diabetes in subjects with prediabetes and metabolic syndrome treated with phentermine and topiramate extended release. Diabetes Care. 2014;37:912–21.
Torgerson JS, Hauptman J, Boldrin MN, Sjostrom L. XENical in the prevention of diabetes in obese subjects (XENDOS) study: a randomized study of orlistat as an adjunct to lifestyle changes for the prevention of type 2 diabetes in obese patients. Diabetes Care. 2004;27:155–61. Erratum in Diabetes Care. 2004;27:856.
Nathan DM, Davidson MB, DeFronzo RA, et al. Impaired fasting glucose and impaired glucose tolerance: implications for care. Diabetes Care. 2007;30:753–9.
Garber AJ, Handelsman Y, Einhorn D, Bergman DA, Bloomgarden ZT, Fonseca V, Garvey WT, Gavin JR 3rd, Grunberger G, Horton ES, Jellinger PS, Jones KL, Lebovitz H, Levy P, McGuire DK, Moghissi ES, Nesto RW. Diagnosis and management of prediabetes in the continuum of hyperglycemia: when do the risks of diabetes begin? A consensus statement from the American College of Endocrinology and the American Association of Clinical Endocrinologists. Endocr Pract. 2008;14:933–46.
Garvey WT. New tools for weight loss therapy enable a more robust medical model for obesity treatment: rationale for a complications-centric approach. Endocr Pract. 2013;19:864–74.
Garvey WT, Garber AJ, Mechanick JI, Bray GA, Dagogo-Jack S, Einhorn D, Grunberger G, Handelsman Y, Hennekens CH, Hurley DL, McGill J, Palumbo P, Umpierrez G. On behalf of the AACE Obesity Scientific Committee. American Association of Clinical Endocrinologists and American College of Endocrinology position statement on the 2014 advanced framework for a new diagnosis of obesity as a chronic disease. Endocr Pract. 2014;20:977–89.
American Diabetes Association. Standards of medical care in diabetes—2015. Diabetes Care. 2015;38 Suppl 1:S8–16.
Grundy SM, Brewer Jr HB, Cleeman JI, American Heart A. Definition of metabolic syndrome: report of the National Heart, Lung, and Blood Institute/American Heart Association conference on scientific issues related to definition. Circulation. 2004;109:433–8.
Milicevic Z, Raz J, Beattie SD, et al. Natural history of cardiovascular disease in patients with diabetes: role of hyperglycemia. Diabetes Care. 2008;31(2):155–60.
Van Gaal LF, Mentens IL, De Block CE. Mechanisms linking obesity with cardiovascular disease. Nature. 2006;444:875–80.
Nigro J, Osman N, Dart AM, Little PJ. Insulin resistance and atherosclerosis. Endocr Rev. 2006;27:242–59.
Olefsky JM, Glass CK. Macrophages, inflammation, and insulin resistance. Annu Rev Physiol. 2010;72:219–46.
Després J-P, Lemieux I. Abdominal obesity and metabolic syndrome. Nature. 2006;444:881–7.
Lara-Castro C, Garvey WT. Intracellular lipid accumulation in liver and muscle and the insulin resistance syndrome. Endocrinol Metab Clin North Am. 2008;37:841–56.
Stefan N, Kantartzis K, Machann J, et al. Identification and characterization of metabolically benign obesity in humans. Arch Intern Med. 2008;168:1609–16.
Wildman RP, Muntner P, Reynolds K, et al. The obese without cardiometabolic risk factor clustering and the normal weight with cardiometabolic risk factor clustering: prevalence and correlates of 2 phenotypes among the US population (NHANES 1999–2004). Arch Intern Med. 2008;1 68:1617–24.
Meigs JB, Wilson PW, Fox CS, et al. Body mass index, metabolic syndrome, and risk of type 2 diabetes or cardiovascular disease. J Clin Endocrinol Metab. 2006;91:2906–12.
Yusuf S, Hawken S, Ounpuu S, et al. Obesity and the risk of myocardial infarction in 27,000 participants from 52 countries: a case-control study. Lancet. 2005;366:1640–9.
Ratner R, Goldberg R, Haffner S, et al. Diabetes Prevention Program Research Group. Impact of intensive lifestyle and metformin therapy on cardiovascular disease risk factors in the diabetes prevention program. Diabetes Care. 2005;28:888–94.
Carnethon MR, Prineas RJ, Temprosa M, et al. Diabetes Prevention Program Research Group. The association among autonomic nervous system function, incident diabetes, and intervention arm in the Diabetes Prevention Program. Diabetes Care. 2006;29:914–9.
Guo F, Moellering DR, Garvey WT. Use of HbA1c for diagnoses of diabetes and prediabetes: comparison with diagnoses based on fasting and 2-hour glucose values and effects of gender, race, and age. Metab Syndr Relat Disord. 2014;12:258–68.
DECODE Study Group. Age- and sex-specific prevalences of diabetes and impaired glucose regulation in 13 European cohorts. Diabetes Care. 2003;26(1):61–9.
Deedwania PC, Volkova N. Current treatment options for the metabolic syndrome. Curr Treat Options Cardiovasc Med. 2005;7:61–74.
Grundy SM, Cleeman JI, Daniels SR, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005;112:2735–52.
Diabetes Prevention Program Research Group, Knowler WC, Fowler SE, Hamman RF, et al. 10-year follow-up of diabetes incidence and weight loss in the Diabetes Prevention Program Outcomes Study. Lancet. 2009;374:1677–86.
Lindström J, Ilanne-Parikka P, Peltonen M, et al. Finnish Diabetes Prevention Study Group. Sustained reduction in the incidence of type 2 diabetes by lifestyle intervention: follow-up of the Finnish Diabetes Prevention Study. Lancet. 2006;368:1673–9.
Li G, Zhang P, Wang J, et al. Cardiovascular mortality, all-cause mortality, and diabetes incidence after lifestyle intervention for people with impaired glucose tolerance in the Da Qing Diabetes Prevention Study: a 23-year follow-up study. Lancet Diabetes Endocrinol. 2014;2:474–80.
Barte JC, ter Bogt NC, Bogers RP, et al. Maintenance of weight loss after lifestyle interventions for overweight and obesity, a systematic review. Obes Rev. 2010;11:899–906.
Garvey WT, Ryan DH, Look M, et al. Two-year sustained weight loss and metabolic benefits with controlled-release phentermine/topiramate in obese and overweight adults (SEQUEL): a randomized, placebo-controlled, phase 3 extension study. Am J Clin Nutr. 2012;95:297–308.
Wentworth JM, Hensman T, Playfair J, et al. Laparoscopic adjustable gastric banding and progression from impaired fasting glucose to diabetes. Diabetologia. 2014;57:463–8.
Sjöholm K, Anveden A, Peltonen M, et al. Evaluation of current eligibility criteria for bariatric surgery: diabetes prevention and risk factor changes in the Swedish obese subjects (SOS) study. Diabetes Care. 2013;36:1335–40.
Carlsson LM, Peltonen M, Ahlin S, et al. Bariatric surgery and prevention of type 2 diabetes in Swedish obese subjects. N Engl J Med. 2012;367:695–704.
Magliano DJ, Barr EL, Zimmet PZ, et al. Glucose indices, health behaviors, and incidence of diabetes in Australia: the Australian Diabetes, Obesity and Lifestyle Study. Diabetes Care. 2008;31:267–72.
Sjöström L, Peltonen M, Jacobson P, et al. Bariatric surgery and long-term cardiovascular events. J Amer Med Assoc. 2012;307:56–65.
Booth H, Khan O, Prevost T, et al. Incidence of type 2 diabetes after bariatric surgery: population-based matched cohort study. Lancet Diabetes Endocrinol. 2014;2:963–8.
Institute of Medicine (U.S.). Committee on the Consequences of Sodium Reduction in Populations, et al. Sodium intake in populations: assessment of evidence. xiv. Washington, DC: National Academies Press; 2013. 209 p.
Institute of Medicine (U.S.). Committee on Strategies to Reduce Sodium Intake, et al. Strategies to reduce sodium intake in the United States. xii. Washington, DC: National Academies Press; 2010. 493 p.
Report of the Dietary Guidelines Advisory Committee on the Dietary Guidelines for Americans. U.D.o.H.a.H.S. U.S. Department of Agriculture, Editors. Washington, DC: U.S. Department of Agriculture, US Department of Health and Human Services; 2010.
Mozaffarian D, et al. Heart disease and stroke statistics-2015 update: a report from the American Heart Association. Circulation. 2015;131(4):e29–322.
Svetkey LP, et al. The DASH diet, sodium intake and blood pressure trial (DASH-sodium): rationale and design. DASH-Sodium Collaborative Research Group. J Am Diet Assoc. 1999;99(8 Suppl):S96–104.
Vollmer WM, et al. Effects of diet and sodium intake on blood pressure: subgroup analysis of the DASH-sodium trial. Ann Intern Med. 2001;135(12):1019–28.
Sacks FM, et al. Effects on blood pressure of reduced dietary sodium and the dietary approaches to stop hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N Engl J Med. 2001;344(1):3–10.
Eckel RH, et al. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(25 Suppl 2):S76–99.
Svetkey LP, et al. Effects of dietary patterns on blood pressure: subgroup analysis of the dietary approaches to stop hypertension (DASH) randomized clinical trial. Arch Intern Med. 1999;159(3):285–93.
Elder CR, et al. Impact of sleep, screen time, depression and stress on weight change in the intensive weight loss phase of the LIFE study. Int J Obes. 2012;36(1):86–92.
Appel LJ, et al. Effects of comprehensive lifestyle modification on blood pressure control: main results of the PREMIER clinical trial. JAMA. 2003;289(16):2083–93.
Hoy MK, Goldman JD. Potassium intake of the US population: what we eat in America, NHANES 2009–1010. Food Surveys Research Group Dietary Data Brief No. 10; 2012. 10.
Cappuccio FP, MacGregor GA. Does potassium supplementation lower blood pressure? A meta-analysis of published trials. J Hypertens. 1991;9(5):465–73.
Geleijnse JM, Kok FJ, Grobbee DE. Blood pressure response to changes in sodium and potassium intake: a metaregression analysis of randomised trials. J Hum Hypertens. 2003;17(7):471–80.
Whelton PK, et al. Effects of oral potassium on blood pressure. Meta-analysis of randomized controlled clinical trials. JAMA. 1997;277(20):1624–32.
Aburto NJ, et al. Effect of increased potassium intake on cardiovascular risk factors and disease: systematic review and meta-analyses. BMJ. 2013;346:f1378.
Medicine, I.o., Dietary Reference Intakes for Water, Potassium, Sodium, Chloride, and Sulfate. 2005: National Academies Press.
Puddey IB, Vandongen R, Beilin LJ. Pressor effect of alcohol. Lancet. 1985;2(8464):1119–20.
Klatsky AL, et al. Alcohol consumption and blood pressure Kaiser-Permanente multiphasic health examination data. N Engl J Med. 1977;296(21):1194–200.
Fuchs FD, et al. Alcohol consumption and the incidence of hypertension: The Atherosclerosis Risk in Communities Study. Hypertension. 2001;37(5):1242–50.
Puddey IB, et al. A randomized controlled trial of the effect of alcohol consumption on blood pressure. Clin Exp Pharmacol Physiol. 1985;12(3):257–61.
Chobanian AV, et al. The seventh report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA. 2003;289(19):2560–72.
Siebenhofer A, et al. Long-term effects of weight-reducing diets in hypertensive patients. Cochrane Database Syst Rev. 2011;(9):CD008274.
Staessen J, Fagard R, Amery A. The relationship between body weight and blood pressure. J Hum Hypertens. 1988;2(4):207–17.
Bushman B. Promoting exercise as medicine for prediabetes and prehypertension. Curr Sports Med Rep. 2014;13(4):233–9.
Medicine, A.C.o.S., ACSM’s Guidelines for Exercise Testing and Prescription. 9th ed. 2014, Philadelphia: Lippincott Williams and Wilkins.
Cornelissen VA, Smart NA. Exercise training for blood pressure: a systematic review and meta-analysis. J Am Heart Assoc. 2013;2(1):e004473.
Kokkinos P. Cardiorespiratory fitness, exercise, and blood pressure. Hypertension. 2014;64(6):1160–4.
Barlow CE, et al. Cardiorespiratory fitness is an independent predictor of hypertension incidence among initially normotensive healthy women. Am J Epidemiol. 2006;163(2):142–50.
Huai P, et al. Physical activity and risk of hypertension: a meta-analysis of prospective cohort studies. Hypertension. 2013;62(6):1021–6.
Staffileno BA, et al. Blood pressure responses to lifestyle physical activity among young, hypertension-prone African-American women. J Cardiovasc Nurs. 2007;22(2):107–17.
Cornelissen VA, Buys R, Smart NA. Endurance exercise beneficially affects ambulatory blood pressure: a systematic review and meta-analysis. J Hypertens. 2013;31(4):639–48.
Cornelissen VA, et al. Impact of resistance training on blood pressure and other cardiovascular risk factors: a meta-analysis of randomized, controlled trials. Hypertension. 2011;58(5):950–8.
Hanson S, Jones A. Is there evidence that walking groups have health benefits? A systematic review and meta-analysis. Br J Sports Med, 2015.
Garvey WT, Kwon S, Zheng D, Shaughnessy S, Wallace P, Pugh K, Jenkins AJ, Klein RL, Liao Y. The effects of insulin resistance and type 2 diabetes mellitus on lipoprotein subclass particle size and concentration determined by nuclear magnetic resonance. Diabetes. 2003;52:453–62.
Zambon A, Hokanson JE, Brown BG, Brunzell JD. Evidence for a new pathophysiological mechanism for coronary artery regression: hepatic lipase-mediated changes in LDL density. Circulation. 1999;99:1959–64.
St-Pierre AC, Cantin B, Dagenais GR, Mauriege P, Bernard PM, Despres JP, Lamarche B. Low density lipoprotein subfractions and the long term risk of ischemic heart disease in men: 13-year follow up data from the Quebec Cardiovascular Study. Arterioscler Thronmb Vasc Biol. 2005;25:553–9.
Ip S, Lichtenstein AH, Chung M, Lau J, Balk EM. Systematic review: Association of low-density lipoprotein subfractions with cardiovascular outcomes. Ann Intern Med. 2009;150:474–84.
Mora S, Szklo M, Otvos JD, Greenland P, Psaty BM, Goff JDC, O’Leary DH, Saad MF, Tsai MY, Sharrett AR. LDL particle subclasses, LDL particle size, and carotid atherosclerosis in the Multi-Ethnic Study of Atherosclerosis (MESA). Atherosclerosis. 2007;192:211–7.
Jellinger PS, Smith DA, Mehta AE, Ganda O, Handelsman Y, Rodbard HW, Shepherd MD, Seibel JA. AACE Task Force for Management of Dyslipidemia and Prevention of Atherosclerosis. American Association of Clinical Endocrinologists’ Guidelines for Management of Dyslipidemia and Prevention of Atherosclerosis. Endocr Pract. 2012;18 Suppl 1:1–78.
Garber AJ, Abrahamson MJ, Barzilay JI, Blonde L, Bloomgarden ZT, Bush MA, Dagogo-Jack S, Davidson MB, Einhorn D, Garber JR, Garvey WT, Grunberger G, Handelsman Y, Hirsch IB, Jellinger PS, McGill JB, Mechanick JI, Rosenblit PD, Umpierrez G, Davidson MH. Aace/ace comprehensive diabetes management algorithm 2015. Endocr Pract. 2015;21(4):438–47.
Jacobson TA, Ito MK, Maki KC, et al. National Lipid Association recommendations for patient-centered management of dyslipidemia: part 1-executive summary. J Clin Lipidol. 2014;8(5):473–88.
Ewald N, Hardt PD, Kloer HU. Severe hypertriglyceridemia and pancreatitis: presentation and management. Curr Opin Lipidol. 2009; 20:497–504.
National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002. 17; 106(25):3143–3421.
Johnson RK, Appel LJ, Brands M, Howard BV, Lefevre M, Lustig RH, Sacks F, Steffen LM, Wylie-Rosett J, American Heart Association Nutrition Committee of the Council on Nutrition, Physical Activity, and Metabolism and the Council on Epidemiology and Prevention. Dietary sugars intake and cardiovascular health: a scientific statement from the American Heart Association. Circulation. 2009;120(11):1011–20.
Appel LJ, Sacks FM, Carey VJ, Obarzanek E, Swain JF, Miller ER 3rd, Conlin PR, Erlinger TP, Rosner BA, Laranjo NM, Charleston J, McCarron P, Bishop LM, OmniHeart Collaborative Research Group. Effects of protein, monounsaturated fat, and carbohydrate intake on blood pressure and serum lipids: results of the OmniHeart randomized trial. JAMA. 2005;294(19):2455–64.
de Souza RJ, Swain JF, Appel LJ, Sacks FM. Alternatives for macronutrient intake and chronic disease: a comparison of the OmniHeart diets with popular diets and with dietary recommendations. Am J Clin Nutr. 2008;88(1):1–11.
Miller M, Stone NJ, Ballantyne C, et al., American Heart Association Clinical Lipidology, Thrombosis, and Prevention Committee of the Council on Nutrition, Physical Activity, and Metabolism; Council on Arteriosclerosis, Thrombosis and Vascular Biology; Council on Cardiovascular Nursing; Council on the Kidney in Cardiovascular Disease. Triglycerides and cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2011;123:2292–333.
Bays HE, Toth PP, Kris-Etherton PM, et al. Obesity, adiposity, and dyslipidemia: a consensus statement from the National Lipid Association. J Clin Lipidol. 2013;7:304–83.
Mensink RP, Zock PL, Kester AD, Katan MB. Effects of dietary fatty acids and carbohydrates on the ratio of serum total to HDL cholesterol and on serum lipids and apolipoproteins: a meta-analysis of 60 controlled trials. Am J Clin Nutr. 2003;77:1146–55.
Itsiopoulos C, Brazionis L, Kaimakamis M, et al. Can the Mediterranean diet lower HbA1c in type 2 diabetes? Results from a randomized cross-over study. Nutr Metab Cardiovasc Dis. 2011;21:740–7.
Estruch R, Ros E, Salas-Savado J, et al. PREDIMED Study Investigators. Primary prevention of cardiovascular disease with a Mediterranean diet. N Engl J Med. 2013;368:1279–90.
Elhayany A, Lustman A, Abel R, Attal-Singer J, Vinker S. A low carbohydrate Mediterranean diet improves cardiovascular risk factors and diabetes control among overweight patients with type 2 diabetes mellitus: a 1-year prospective randomized intervention study. Diabetes Obes Metab. 2010;12:204–9.
Shai I, Schwarzfuchs D, Henkin Y, et al., Dietary Intervention Randomized Controlled Trial (DIRECT) Group. Weight loss with a low-carbohydrate, Mediterranean, or low-fat diet. N Engl J Med. 2009;359:229–41.
Kjems L, Filozof C, Wright M, Keefe D. Association between fasting triglycerides and presence of fasting chylomicrons in patients with severe hypertriglyceridemia. J Clin Lipidol. 2014;8:312. (Abstract 121).
Viljoen A, Wierzbicki AS. Diagnosis and treatment of severe hypertriglyceridemia. Expert Rev Cardiovasc Ther. 2012;10:505–14.
Nordmann AJ, Nordmann A, Briel M, Keller U, Yancy WS Jr, Brehm BJ, Bucher HC. Effects of low-carbohydrate vs low-fat diets on weight loss and cardiovascular risk factors: a meta-analysis of randomized controlled trials. JAMA Intern Med. 2006;166(3):285–93. Erratum in: JAMA Intern Med. 2006;166(8):932.
Morgan LM, Griffin BA, Millward DJ, DeLooy A, Fox KR, Baic S, Bonham MP, Wallace JM, MacDonald I, Taylor MA, Truby H. Comparison of the effects of four commercially available weight-loss programmes on lipid-based cardiovascular risk factors. Public Health Nutr. 2009;12(6):799–807.
Varady KA, Bhutani S, Klempel MC, Lamarche B. Improvements in LDL particle size and distribution by short-term alternate day modified fasting in obese adults. Br J Nutr. 2011;105(4):580–3.
Varady KA, Bhutani S, Klempel MC, Kroeger CM. Comparison of effects of diet versus exercise weight loss regimens on LDL and HDL particle size in obese adults. Lipids Health Dis. 2011;10:119.
Krauss RM, Blanche PJ, Rawlings RS, Fernstrom HS, Williams PT. Separate effects of reduced carbohydrate intake and weight loss on atherogenic dyslipidemia. Am J Clin Nutr. 2006;83(5):1025–31.
Wood RJ, Volek JS, Liu Y, Shachter NS, Contois JH, Fernandez ML. Carbohydrate restriction alters lipoprotein metabolism by modifying VLDL, LDL, and HDL subfraction distribution and size in overweight men. J Nutr. 2006;136(2):384–9.
Richard C, Couture P, Ooi EM, Tremblay AJ, Desroches S, Charest A, Lichtenstein AH, Lamarche B. Effect of Mediterranean diet with and without weight loss on apolipoprotein B100 metabolism in men with metabolic syndrome. Arterioscler Thromb Vasc Biol. 2014;34(2):433–8.
Graham TE. Exercise, postprandial triacylglyceridemia, and cardiovascular disease risk. Can J Appl Physiol. 2004;29:781–99.
Dekker MJ, Graham TE, Ooi TC, Robinson LE. Exercise prior to fat ingestion lowers fasting and postprandial VLDL and decreases adipose tissue IL-6 and GIP receptor mRNA in hypertriacylglycerolemic men. J Nutr Biochem. 2010;21(10):983–90.
Tambalis K, Panagiotakos DB, Kavouras SA, Sidossis LS. Responses of blood lipids to aerobic, resistance, and combined aerobic with resistance exercise training: a systematic review of current evidence. Angiology. 2009;60(5):614–32.
Pitsavos C, Panagiotakos DB, Tambalis KD, Chrysohoou C, Sidossis LS, Skoumas J, Stefanadis C. Resistance exercise plus to aerobic activities is associated with better lipids’ profile among healthy individuals: the ATTICA study. Q J Med. 2009;102(9):609–16.
http://www.health.gov/dietaryguidelines/2015-scientific-report/PDFs/Scientific-Report-of-the-2015-Dietary-Guidelines-Advisory-Committee.pdf/dietaryguidelines/2015-scientific-report/PDFs/Scientific-Report-of-the-2015-Dietary-Guidelines-Advisory-Committee.pdf.
Ridker PM, Danielson E, Fonseca FA, Genest J, Gotto AM Jr, Kastelein JJ, Koenig W, Libby P, Lorenzatti AJ, MacFadyen JG, Nordestgaard BG, Shepherd J, Willerson JT, Glynn RJ, JUPITER Study Group. Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. N Engl J Med. 2008;359(21):2195–207.
Lara-Castro C, Garvey WT. Diet, insulin resistance, and obesity: zoning in on data for Atkins dieters living in South Beach. J Clin Endocrinol Metab. 2004;89:4197–205.
Dansinger ML, Gleason JA, Griffith JL, Selker HP, Schaefer EJ. Comparison of the Atkins, Ornish, Weight Watchers, and Zone diets for weight loss and heart disease risk reduction: a randomized trial. J Amer Med Assoc. 2005;293(1):43–53.
Stern L, Iqbal N, Seshadri P, et al. The effects of low-carbohydrate versus conventional weight loss diets in severely obese adults: one-year follow-up of a randomized trial. Ann Intern Med. 2004;140:778–85.
Weinsier RL, Wilson NP, Morgan SL, Cornwell AR, Craig CB. EatRight lose weight: seven simple steps. Birmingham: Oxmoor House; 1997.
Greene LF, Malpede CZ, Henson CS, Hubbert KA, Heimburger DC, Ard JD. Weight maintenance 2 years after participation in a weight loss program promoting low-energy density foods. Obesity. 2006;10:1795–801.
Ard JD, Cox TL, Zunker C, Wingo BC, Jefferson WK, Brakhage C. A study of a culturally enhanced EatRight dietary intervention in a predominately African American workplace. J Public Health Manag Pract. 2010;16(6):E1–8.
Turner-McGrievy GM, Barnard ND, Cohen J, Jenkins DJA, Gloede L, Green AA. Changes in nutrient intake and dietary quality among participants with type 2 diabetes following a lowfat vegan diet or a conventional diabetes diet for 22 weeks. J Am Diet Assoc. 2008;108:1636–45.
Foster GD, Wyatt HR, Hill JO, McGuckin BG, Brill C, Mohammed BS, Szapary PO, Rader DJ, Edman JS, Klein S. A randomized trial of a low-carbohydrate diet for obesity. N Engl J Med. 2003;348:2082–90.
Samaha FF, Iqbal N, Seshadri P, Chicano KL, Daily DA, McGrory J, Williams T, Williams M, Gracely EJ, Stern L. A low-carbohydrate as compared with a low-fat diet in severe obesity. N Engl J Med. 2003;348:2074–81.
Lovejoy JC, Windhauser MM, Rood JC, de la Bretonne JA. Effect of a controlled high-fat versus low-fat diet on insulin sensitivity and leptin levels in African-American and Caucasian women. Metabolism. 1998;47:1520–4.
Astrup A, Astrup A, Buemann B, Flint A, Raben A. Low-fat diets and energy balance: how does the evidence stand in 2002? Proc Nutr Soc. 2002;61:299–309.
Schwartz MW, Figlewicz DP, Baskin DG, Woods SC, Porte D Jr. Insulin in the brain: a hormonal regulator of energy balance. Endocr Rev. 1992;13:387–414.
Ludwig DS. Dietary glycemic index and obesity. J Nutr. 2000;130:280S–3.
Roberts SB. High-glycemic index foods, hunger, and obesity: is there a connection? Nutr Rev. 2000;58:163–9.
Pi-Sunyer FX. Glycemic index and disease. Am J Clin Nutr. 2002;76:290S–8.
World Health Organization. Diet, nutrition and the prevention of chronic diseases. 916. Geneva: WHO Technical Report Series; 2003.
Pereira MA, Jacobs DR Jr, Pins JJ, Raatz SK, Gross MD, Slavin JL, Seaquist ER. Effect of whole grains on insulin sensitivity in overweight hyperinsulinemic adults. Am J Clin Nutr. 2002;75:848–55.
Hu FB, van Dam RM, Liu S. Diet and risk of type II diabetes: the role of types of fat and carbohydrate. Diabetologia. 2001;44(7):805–17.
Heymsfield SB, van Mierlo CA, van der Knaap HC, Heo M, Frier HI. Weight management using a meal replacement strategy: meta and pooling analysis from six studies. Int J Obes Relat Metab Disord. 2003;27:537–49.
Harris JA, Benedict FG. A biometric study of basal metabolism in man. Washington, DC: Carnegie Institute of Washington; 1919 (publ. no. 279).
Mifflin MD, St. Jeor ST, Hill LA, Scott BJ, Daugherty SA, Koh YO. A new predictive equation for resting energy expenditure in healthy individuals. Am J Clin Nutr. 1990;51:251–7.
Martin K, Wallace P, Rust PF, Garvey WT. Estimation of resting energy expenditure considering effects of race and diabetes status. Diabetes Care. 2004;27:1405–11.
Hipskind P, Glass C, Charlton D, Nowak D, Dasarathy S. Do handheld calorimeters have a role in assessment of nutrition needs in hospitalized patients? A systematic review of literature. Nutr Clin Pract. 2011;26(4):426–33.
Wing RR, Lang W, Wadden TA, et al. The Look AHEAD Research Group. Benefits of modest weight loss in improving cardiovascular risk factors in overweight and obese individuals with type 2 diabetes. Diabetes Care. 2011;34:1481–6.
Rivellese AA, De Natale C, Lilli S. Type of dietary fat and insulin resistance. Ann N Y Acad Sci. 2002;967:329–35.
Mayer-Davis EJ, Monaco JH, Hoen HM, Carmichael S, Vitolins MZ, Rewers MJ, Haffner SM, Ayad MF, Bergman RN, Karter AJ. Dietary fat and insulin sensitivity in a triethnic population: the role of obesity. The Insulin Resistance Atherosclerosis Study (IRAS). Am J Clin Nutr. 1997;65:79–87.
Maron DJ, Fair JM, Haskell WL. Saturated fat intake and insulin resistance in men with coronary artery disease. The Stanford Coronary Risk Intervention Project Investigators and Staff. Circulation. 1991;84:2020–7.
Marshall JA, Bessesen DH, Hamman RF. High saturated fat and low starch and fibre are associated with hyperinsulinaemia in a non-diabetic population: the San Luis Valley Diabetes Study. Diabetologia. 1997;40:430–8.
Salmeron J, Hu FB, Manson JE, Stampfer MJ, Colditz GA, Rimm EB, Willett WC. Dietary fat intake and risk of Type 2 Diabetes in women. Am J Clin Nutr. 2001;73:1019–26.
Summers LK, Fielding BA, Bradshaw HA, Ilic V, Beysen C, Clark ML, Moore NR, Frayn KN. Substituting dietary saturated fat with polyunsaturated fat changes abdominal fat distribution and improves insulin sensitivity. Diabetologia. 2002;45:369–77.
Mayer EJ, Newman B, Quesenberry CP Jr, Selby JV. Usual dietary fat intake and insulin concentrations in healthy women twins. Diabetes Care. 1993;16:1459–69.
Simopoulos AP. Omega-3 fatty acids in the prevention-management of cardiovascular disease. Can J Physiol Pharmacol. 1997;75:234–9.
Vessby B, Aro A, Skarfors E, Berglund L, Salminen I, Lithell H. The risk to develop NIDDM is related to the fatty acid composition of the serum cholesterol esters. Diabetes. 1994;43:1353–7.
Garg A. High-monounsaturated-fat diets for patients with diabetes mellitus: a meta-analysis. Am J Clin Nutr. 1998;67:577S–82.
Perez-Jimenez F, Lopez-Miranda J, Pinillos MD, Gomez P, Paz-Rojas E, Montilla P, Marin C, Velasco MJ, Blanco-Molina A, Jimenez Pereperez JA, Ordovas JM. A Mediterranean and a high-carbohydrate diet improve glucose metabolism in healthy young persons. Diabetologia. 2001;44:2038–43.
Thomsen C, Rasmussen O, Christiansen C, Pedersen E, Vesterlund M, Storm H, Ingerslev J, Hermansen K. Comparison of the effects of a monounsaturated fat diet and a high carbohydrate diet on cardiovascular risk factors in first degree relatives to Type-2 diabetic subjects. Eur J Clin Nutr. 1999;53:818–23.
Kiens B, Richter EA. Types of carbohydrate in an ordinary diet affect insulin action and muscle substrates in humans. Am J Clin Nutr. 1996;63:47–53.
Liese AD, Roach AK, Sparks KC, Marquart L, D’Agostino RB Jr, Mayer-Davis EJ. Whole-grain intake and insulin sensitivity: the Insulin Resistance Atherosclerosis Study. Am J Clin Nutr. 2003;78:965–71.
McKeown NM, Meigs JB, Liu S, Saltzman E, Wilson PW, Jacques PF. Carbohydrate nutrition, insulin resistance, and the prevalence of the metabolic syndrome in the Framingham Offspring Cohort. Diabetes Care. 2004;27:538–46.
Pereira MA, Jacobs DR Jr, Pins JJ, Raatz SK, Gross MD, Slavin JL, Seaquist ER. Effect of whole grains on insulin sensitivity in overweight hyperinsulinemic adults. Am J Clin Nutr. 2002;75:848–55.
Shai I, Schwarzfuchs D, Henkin Y, et al. Dietary Intervention Randomized Controlled Trial (DIRECT) Group. Weight loss with a low-carbohydrate, Mediterranean, or low-fat diet. N Engl J Med. 2009;359:229–41.
de Lorgeril M, Salen P, Martin JL, Monjaud I, Delaye J, Mamelle N. Mediterranean diet, traditional risk factors, and the rate of cardiovascular complications after myocardial infarction: final report of the Lyon Diet Heart Study. Circulation. 1999;99(6):779–85.
Martinez-Gonzalez MA, Bes-Rastrollo M. Dietary patterns, Mediterranean diet, and cardiovascular disease. Curr Opin Lipidol. 2014;25(1):20–6.
Hoevenaar-Blom MP, Nooyens AC, Kromhout D, Spijkerman AM, Beulens JW, van der Schouw YT, Bueno-de-Mesquita B, Verschuren WM. Mediterranean style diet and 12-year incidence of cardiovascular diseases: the EPIC-NL cohort study. PLoS ONE. 2012;7(9):e45458.
Kastorini CM, Milionis HJ, Esposito K, Giugliano D, Goudevenos JA, Panagiotakos DB. The effect of Mediterranean diet on metabolic syndrome and its components: a meta-analysis of 50 studies and 534,906 individuals. J Am Coll Cardiol. 2011;57:1299–313.
Esposito K, Maiorino MI, Ceriello A, Giugliano D. Prevention and control of type 2 diabetes by Mediterranean diet: a systematic review. Diabetes Res Clin Pract. 2010;89:97–102.
Salas-Salvadó J, Bulló M, Babio N, et al. Reduction in the incidence of type 2 diabetes with the Mediterranean diet: results of the PREDIMED-Reus nutrition intervention randomized trial. Diabetes Care. 2011;34:14–9.
Martínez-González MA, de la Fuente-Arrillaga C, Nuñez-Córdoba JM, et al. Adherence to Mediterranean diet and risk of developing diabetes: prospective cohort study. Brit Med J. 2008;336:1348–51.
Salas-Salvadó J, Fernández-Ballart J, Ros E, et al. Effect of a Mediterranean diet supplemented with nuts on metabolic syndrome status: one-year results of the PREDIMED randomized trial. Arch Intern Med. 2008;168:2449–58.
Jeon CY, Lokken RP, Hu FB, van Dam RM. Physical activity of moderate intensity and risk of type 2 diabetes: a systematic review. Diabetes Care. 2007;30(3):744–52.
Duncan GE, Perri MG, Theriaque DW, Hutson AD, Eckel RH, Stacpoole PW. Exercise training, without weight loss, increases insulin sensitivity and postheparin plasma lipase activity in previously sedentary adults. Diabetes Care. 2003;26(3):557–62.
Houmard JA, Tanner CJ, Slentz CA, Duscha BD, McCartney JS, Kraus WE. Effect of the volume and intensity of exercise training on insulin sensitivity. J Appl Physiol. 2004;96(1):101–6.
Bajpeyi S, Tanner CJ, Slentz CA, et al. Effect of exercise intensity and volume on persistence of insulin sensitivity during training cessation. J Appl Physiol. 2009;106(4):1079–85.
Myers VH, McVay MA, Brashear MM, Johannsen NM, Swift DL, Kramer K, Harris MN, Johnson WD, Earnest CP, Church TS. Exercise training and quality of life in individuals with type 2 diabetes: a randomized controlled trial. Diabetes Care. 2013;36(7):1884–90.
Johannsen NM, Swift DL, Lavie CJ, Earnest CP, Blair SN, Church TS. Categorical analysis of the impact of aerobic and resistance exercise training, alone and in combination, on cardiorespiratory fitness levels in patients with type 2 diabetes: results from the HART-D study. Diabetes Care. 2013;36(10):3305–12.
Snowling NJ, Hopkins WG. Effects of different modes of exercise training on glucose control and risk factors for complications in type 2 diabetic patients: a meta-analysis. Diabetes Care. 2006;29(11):2518–27.
Sigal RJ, Kenny GP, Boule NG, Wells GA, Prud’homme D, Fortier M, et al. Effects of aerobic training, resistance training, or both on glycemic control in type 2 diabetes: a randomized trial. Ann Intern Med. 2007;147:357–69.
American College of Sports Medicine and the American Diabetes Association. Joint position statement: exercise and type 2 diabetes. Med Sci Sports Exerc. 2010;42:2282–303.
Katzmarzyk PT, Church TS, Craig CL, Bouchard C. Sitting time and mortality from all causes, cardiovascular disease, and cancer. Med Sci Sports Exerc. 2009;41(5):998–1005.
Helmrich SP, Ragland DR, Leung RW, Paffenbarger RS Jr. Physical activity and reduced occurrence of non-insulin-dependent diabetes mellitus. N Engl J Med. 1991;325(3):147–52.
Hu FB, Sigal RJ, Rich-Edwards JW, et al. Walking compared with vigorous physical activity and risk of type 2 diabetes in women: a prospective study. JAMA. 1999;282(15):1433–9.
Manson JE, Rimm EB, Stampfer MJ, et al. Physical activity and incidence of non-insulin-dependent diabetes mellitus in women. Lancet. 1991;338(8770):774–8.
Bax JJ, Young LH, Frye RL, Bonow RO, Steinberg HO, Barrett EJ. Screening for coronary artery disease in patients with diabetes. Diabetes Care. 2007;30:2729–36.
Maclean PS, Bergouignan A, Cornier MA, Jackman MR. Biology’s response to dieting: the impetus for weight regain. Am J Physiol Regul Integr Comp Physiol. 2011;301:R581–R600.
Leibel RL, Rosenbaum M, Hirsch J. Changes in energy expenditure resulting from altered body weight. N Engl J Med. 1995;332:621–8.
Ebbeling CB, Swain JF, Feldman HA, et al. Effects of dietary composition on energy expenditure during weight-loss maintenance. JAMA. 2012;307:2627–34.
Sumithran P, Prendergast LA, Delbridge E, et al. Long-term persistence of hormonal adaptations to weight loss. N Engl J Med. 2011;365:1597–604.
Sumithran P, Proietto J. The defence of body weight: a physiological basis for weight regain after weight loss. Clin Sci. 2013;124:231–41.
Doucet E, Imbeault P, St-Pierre S, et al. Appetite after weight loss by energy restriction and a low-fat diet-exercise follow-up. Int J Obes Relat Metab Disord. 2000;24:906–14.
Ochner CN, Barrios DM, Lee CD, Pi-Sunyer FX. Biological mechanisms that promote weight regain following weight loss in obese humans. Physiol Behav. 2013;120:106–13.
Fidler MC, Sanchez M, Raether B, et al. A one-year randomized trial of lorcaserin for weight loss in obese and overweight adults: the BLOSSOM trial. J Clin Endocrinol Metab. 2011;96:3067–77.
Wadden TA, Foreyt JP, Foster GD, et al. Weight loss with naltrexone SR/bupropion SR combination therapy as an adjunct to behavior modification: the COR-BMOD trial. Obesity. 2011;19:110–20.
Wadden TA, Hollander P, Klein S, et al. Weight maintenance and additional weight loss with liraglutide after low-calorie-diet-induced weight loss: the SCALE Maintenance randomized study. Int J Obes. 2013;37:1514.
Wadden TA, Berkowitz RI, Sarwer DB, Prus-Wisniewski R, Steinberg C. Benefits of lifestyle modification in the pharmacologic treatment of obesity: a randomized trial. Arch Intern Med. 2001;161(2):218–27.
Mechanick JI, Youdim A, Jones DB, et al. Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient-2013 update: cosponsored by American Association of Clinical Endocrinologists, the Obesity Society, and American Society for Metabolic & Bariatric Surgery. Endocr Pract. 2013;19:337–72.
Acknowledgments
We acknowledge the support of the Diabetes Research Center at the University of Alabama at Birmingham funded by an award from the National Institutes of Health (DK-079626).
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Garvey, W., Arathuzik, G., Miller, G., Ard, J. (2016). Lifestyle Therapy in the Management of Cardiometabolic Risk: Diabetes Prevention, Hypertension, and Dyslipidemia. In: Mechanick, J., Kushner, R. (eds) Lifestyle Medicine. Springer, Cham. https://doi.org/10.1007/978-3-319-24687-1_23
Download citation
DOI: https://doi.org/10.1007/978-3-319-24687-1_23
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-24685-7
Online ISBN: 978-3-319-24687-1
eBook Packages: MedicineMedicine (R0)