Abstract
The modern era of correction of pectus excavatum (PE) started in 1949 by Ravitch. Since several modifications to the technique were published, but it was the standard way to correct PE for long time. Prof Nuss’s minimally technique changed the strategy for correction and seems now to be the standard technique for surgeons who correct PE. The optimal age for surgery is discussed. Most surgeons prefer that the patient is in the beginning of the puberty so the bar system is in situ through the growth spurt. It looks like that this decreases the recurrence rate. At this age the patients are also aware of the restrictions which are in the beginning of the treatment. But recently it has been offered to patient up to 40 years of age. Bar removal is done 3 years after correction and is a day surgery project. In most cases it is only necessary to open the incision where you have the stabilizer if you use the short bar technique. The complication are few in experienced hands. Most of the patients get a very beautiful result and are very satisfied with the operation.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
The modern era of correction of pectus excavatum (PE) started in 1949 where Ravitch published the his first paper [1]. Since several modifications to the technique were published, but it was the standard way to correct PE until Nuss orally presented his first work in 1997 and published it in 1998 [2]. This minimally technique changed the strategy for correction and seems now to be the standard technique for surgeons who correct PE. This paper dealed with 45 patients who were corrected through a 10-years course. The age group was from 1 to 15 years and at that time it was thought that the technique could only be used in children and adolescents because the rigidity of the chest in adults was too high. With the growing experience of the technique it has been shown that even patients in the fifties and sixties might be corrected by the Nuss-procedure [3, 4]. The original technique prescribed that the bar length should be from the mid axillary line on each side. The first operations were done without scope assistance but to make the intervention safer using of the thoracoscope is now mandatory. One of the problems with the technique was the risk of rotation of the bar. This was reduced by first adding a stabilizer, then fixing the stabilizer to the bar and finally using several circumcostal sutures around the bar and rib on the opposite site of the stabilizer. These reduced the risk from around 15 to 1 % [5]. Later the use of a shorter bar has been published and this change has shown the same low risk of rotation [6, 7]. Using the shorter bar is easier, using shorter time in the OR, gives the same good cosmetic result and is as stable as using the long original bar.
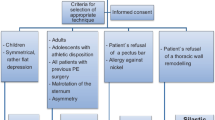
Indication for Surgery
In most published papers the indication for surgery is cosmetic complaints from the patient [8]. It has been known for many years that the patients too have several physiological symptoms [9] and recent studies have shown that correction without increasing the patients quality of life significantly [10–16] also means better movement of the chest [17, 18] and better cardiac performance [19, 20]. Some surgeons prefer to measure the Haller index, which should normally be bigger than 3.25 to indicate surgery, but the problem with the Haller index is that it is also depending of the chest shape, if it is flat or barrel shaped.
Surgery
The optimal age for surgery is discussed. Most surgeons prefer that the patient is in the beginning of the puberty so the bar system is in situ through the growth spurt. It looks like that this decreases the recurrence rate. At this age the patients are also aware of the restrictions which are in the beginning of the treatment. In girls I prefer that the there is some demarcation of the breasts so the incisions might be placed in the sulcus.
The surgery is done in general anaesthesia and prior to surgery an epidural catheter is placed to facilitate the postoperative pain treatment. Position of the patient is on the back either with the arms abducted or the arm along the body with a pillow behind the back [21] or in my mind better with the right arm elevated in front of the head to allow free movement of the scope. The deepest point is defined and the points for penetration of the chest wall are marked on the skin. These points should be just medially to the highest areas. The length of the bar should be so the right end covers two ribs and the left end is long enough to carry the stabilizer, so the stabilizer is placed very close to the hinge point. This gives a very stable system with a very limited risk of rotation. This means that the bar is placed asymmetric in the patient. The tunnel under the sternum is done guided by the scope which normally is only used from the right side. It is very important that the introducer is in close contact with the backside of the chest, if this is not true so you have to use an introducer with a longer tip. A template is bended to the expected shape of the chest after correction with some overcorrection 1–2 cm because the pressure from the sternum will cause some debending of the bar. The bar might be guided through the chest by a normal suture or a tape. The bar is inserted as an U and turned 180°. In most cases it might be done with the use of only one flipper.
Most of the patients only need one bar, which normally should support the sternum under the deepest point. The number of bars is depended on the length of the PE, the deepness and the rigidity of the chest wall. Around 30 % needs more than one bar. In many cases two bars might be inserted through the same incisions. In some cases an oblique bar gives a better cosmetic result. All bars are normally stabilized on the left side with a stabilizer, which is fixed either by a steel wire around the bar or an additional bending of the end.
The lung is expanded at the end of the operation by using a chest tube under water seal and is removed at the end of the operation.
An x-ray is done the second postoperative day before discharge. X-ray just after surgery is normally not required [22].
Pain Treatment
The pain treatment is a combination of epidural analgesia and perorally treatment. The epidural catheter is closed the second postoperative day in the morning. The day of the operation the patient have morphine and bupivacaine and the next day it is changed to pure bupivacaine. The first postoperative day the patient starts NSAID, Ibuprofen and often oxycodone. The oxycodone is stopped after 10–14 days, Ibuprofen and NSAID are normally stopped after 4 and 5 weeks postoperatively, respectively.
Postoperative Restrictions
The first 6 weeks the patients are not allowed to carry more than 2 kg in front of the body and 5 kg on the their back. They must not bike, not rotate the upper body more than 15° and should sleep on the back. Sleeping on the back is often the most difficult issue, giving the patient serious backpain, but most of the patients start spontaneously to turn in the bed after 5–7 weeks and then the backpain problems disappear.
In all 3 years heavy contact sport such as American football, rugby, icehockey and self-defence sports should be avoided.
Postoperative Follow-Up
The patients are seen in the outpatient clinic after 6 weeks for a clinical examination and an x-ray to see the position of the bar system. After this the patient is called 3 years later for bar removal. Should there be any problems in the mean time they may call the department.
Results
Most of the patients get a very beautiful result and are very satisfied with the operation. The complication are few in experienced hands.
References
Ravitch MM. The operative treatment of pectus excavatum. Ann Surg. 1949;129:429–44.
Nuss D, Kelly Jr RE, Croitoru DP, Katz ME. A 10-year review of a minimally invasive technique for the correction of pectus excavatum. J Pediatr Surg. 1998;33:545–52.
Pilegaard HK, Licht PB. Routine use of minimally invasive surgery for pectus excavatum in adults. Ann Thorac Surg. 2008;86:952–6.
Pilegaard HK. Extending the use of Nuss procedure in patients older than 30 years. Eur J Cardiothorac Surg. 2011;40:334–7.
Nuss D. Recent experiences with minimally invasive pectus excavatum repair “Nuss procedure”. Jpn J Thorac Cardiovasc Surg. 2005;53:338–44.
Pilegaard HK, Licht PB. Early results following the Nuss operation for pectus excavatum – a single-institution experience of 383 patients. Interact Cardiovasc Thorac Surg. 2008;7:54–7.
Pilegaard HK, Licht PB. Can absorbable stabilizers be used routinely in the Nuss procedure? Eur J Cardiothorac Surg. 2009;35:561–4.
Krasopoulos G, Goldstraw P. Minimally invasive repair of pectus excavatum deformity. Eur J Cardiothorac Surg. 2010.
Kelly Jr RE. Pectus excavatum: historical background, clinical picture, preoperative evaluation and criteria for operation. Semin Pediatr Surg. 2008;17:181–93.
Roberts J, Hayashi A, Anderson JO, Martin JM, Maxwell LL. Quality of life of patients who have undergone the Nuss procedure for pectus excavatum: preliminary findings. J Pediatr Surg. 2003;38:779–83.
Lawson ML, Cash TF, Akers R, Vasser E, Burke B, Tabangin M, Welch C, Croitoru DP, Goretsky MJ, Nuss D, Kelly Jr RE. A pilot study of the impact of surgical repair on disease-specific quality of life among patients with pectus excavatum. J Pediatr Surg. 2003;38:916–8.
Krasopoulos G, Dusmet M, Ladas G, Goldstraw P. Nuss procedure improves the quality of life in young male adults with pectus excavatum deformity. Eur J Cardiothorac Surg. 2006;29:1–5.
Metzelder ML, Kuebler JF, Leonhardt J, Ure BM, Petersen C. Self and parental assessment after minimally invasive repair of pectus excavatum: lasting satisfaction after bar removal. Ann Thorac Surg. 2007;83:1844–9.
Kelly Jr RE, Cash TF, Shamberger RC, Mitchell KK, Mellins RB, Lawson ML, Oldham K, Azizkhan RG, Hebra AV, Nuss D, Goretsky MJ, Sharp RJ, Holcomb 3rd GW, Shim WK, Megison SM, Moss RL, Fecteau AH, Colombani PM, Bagley T, Quinn A, Moskowitz AB. Surgical repair of pectus excavatum markedly improves body image and perceived ability for physical activity: multicenter study. Pediatrics. 2008;122:1218–22.
Lam MW, Klassen AF, Montgomery CJ, LeBlanc JG, Skarsgard ED. Quality-of-life outcomes after surgical correction of pectus excavatum: a comparison of the Ravitch and Nuss procedures. J Pediatr Surg. 2008;43:819–25.
Jacobsen EB, Thastum M, Jeppesen JH, Pilegaard HK. Health-related quality of life in children and adolescents undergoing surgery for pectus excavatum. Eur J Pediatr Surg. 2010;20:85–91.
Redlinger Jr RE, Kelly RE, Nuss D, Goretsky M, Kuhn MA, Sullivan K, Wootton AE, Ebel A, Obermeyer RJ. Regional chest wall motion dysfunction in patients with pectus excavatum demonstrated via optoelectronic plethysmography. J Pediatr Surg. 2011;46:1172–6.
Redlinger Jr RE, Wootton A, Kelly RE, Nuss D, Goretsky M, Kuhn MA, Obermeyer RJ. Optoelectronic plethysmography demonstrates abrogation of regional chest wall motion dysfunction in patients with pectus excavatum after Nuss repair. J Pediatr Surg. 2012;47:160–4.
Lesbo M, Tang M, Nielsen HH, Frokiaer J, Lundorf E, Pilegaard HK, Hjortdal VE. Compromised cardiac function in exercising teenagers with pectus excavatum. Interact Cardiovasc Thorac Surg. 2011;13:377–80.
Maagaard M, Tang M, Ringgaard S, Nielsen HH, Frokiaer J, Haubuf M, Pilegaard HK, Hjortdal VE. Normalized cardiopulmonary exercise function in patients with pectus excavatum three years after operation. Ann Thorac Surg. 2013;96:272–8.
de Campos JR, Fonseca MH, Werebe Ede C, Velhote MC, Jatene FB. Technical modification of the Nuss operation for the correction of pectus excavatum. Clinics (Sao Paulo). 2006;61:185–6.
Knudsen MR, Nyboe C, Hjortdal VE, Pilegaard HK. Routine postoperative chest X-ray is unnecessary following the Nuss procedure for pectus excavatum. Interact Cardiovasc Thorac Surg. 2013;16:830–3.
Nyboe C, Knudsen MR, Pilegaard HK. Elective pectus bar removal following Nuss procedure for pectus excavatum: a single-institution experience. Eur J Cardiothorac Surg. 2011;39:1040–2.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Pilegaard, H.K. (2016). Minimal Invasive Repair of Pectus Excavatum. In: Kolvekar, S., Pilegaard, H. (eds) Chest Wall Deformities and Corrective Procedures. Springer, Cham. https://doi.org/10.1007/978-3-319-23968-2_9
Download citation
DOI: https://doi.org/10.1007/978-3-319-23968-2_9
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-23966-8
Online ISBN: 978-3-319-23968-2
eBook Packages: MedicineMedicine (R0)